Abstract
Dupuytren’s disease is a chronic, progressive fibroproliferative condition of the hand fascia which results in digital contraction. So far, treatments do not directly interfere with the (myo)fibroblasts that are responsible for the formation of the collagen-rich cords and its contraction. Here we investigated whether verteporfin (VP) is able to inhibit the activation and subsequent differentiation of DD nodular fibroblasts into myofibroblasts. Fibroblasts were isolated from nodules of 7 Dupuytren patients. Cells are treated (1) for 48 h with 5 ng/ml transforming growth factor β1 (TGF-β1) followed by 48 h with/without 250 nM VP in the absence of TGF-β1, or treated (2) for 48 h with TGF-β1 followed by 48 h with/without VP in the presence of TGF-β1. mRNA levels were measured by means of Real-Time PCR, and proteins were visualized by means of Western blotting and/or immunofluorescence. Quantitative data were statistically analyzed with GraphPad Prism using the paired t-test. We found that fibroblasts activated for 48 h with TGF-β1 show a decrease in mRNA levels of COL1A1, COL3A1, COL4A1, PLOD2, FN1EDA, CCN2 and SERPINE1 when exposed for another 48 h with VP, whereas no decrease is seen for ACTA2, YAP1, SMAD2 and SMAD3 mRNA levels. Cells exposed for an additional 48 h with TGF-β1, but now in the presence of VP, are not further activated anymore, whereas in the absence of VP the cells continue to differentiate into myofibroblasts. Collagen type I, fibronectin-extra domain A, α-smooth muscle actin, YAP1, Smad2 and Smad3 protein levels were attenuated by both VP treatments. We conclude that VP has strong anti-fibrotic properties: it is able to halt the differentiation of fibroblasts into myofibroblasts, and is also able to reverse the activation status of fibroblasts. The decreased protein levels of YAP1, Smad2 and Smad3 in the presence of VP explain in part the strong anti-fibrotic properties of VP. Verteporfin is clinically used as a photosensitizer for photodynamic therapy to eliminate abnormal blood vessels in the eye to attenuate macular degeneration. The antifibrotic properties of VP do not rely on photo-activation, as we used the molecule in its non-photoinduced state.
Similar content being viewed by others
Introduction
Dupuytren’s disease (DD) is a fibroproliferative condition of the hand fascia that affects mainly adults of Northern European ascent1,2. The etiology of the disease is unclear, but genetic predisposition plays an important role. Studies in twin siblings show heritability up to 80%3 and genome-wide association studies show specific genomic regions that give rise to DD4,5,6. Moreover, several non-genetic factors are reported to contribute to the development of the disease, such as smoking, alcohol intake, diabetes, hyperlipidemia and manual labor or exposure to vibrations1,2,6,7.
DD is characterized by the presence of fibrotic lesions that seem to spread along the palmar fascia of the palm and fingers, that may contract thereby impairing their extension, thus affecting hand function and quality of life1,2,6,7. The disease has three different stages, all of which can be present at the same time. The initial proliferative stage is when nodules form, containing numerous myofibroblasts, driving the whole fibrotic response. The proliferative stage is followed by an involutional stage, where myofibroblasts and extracellular matrix (ECM) are aligned along the stress lines of the hand. It ends with the residual stage, where the nodules disappear, leaving behind a mostly acellular fibrotic tendon-like structure (cord) that adheres to the skin and fascia resulting in contracture lesions1,2,6.
Treatment of DD comprises nonsurgical treatments (e.g. physiotherapy, intralesional injected steroids or radiotherapy) which are usually performed in early stages of the disease, but the efficacy of these treatments is not clear1,8,9. A novel treatment approach is the injection of collagenase derived from Clostridium histolyticum. Its efficacy continues to be evaluated10,11,12. The late stage contractures are treated by surgical interventions such as fasciotomy, fasciectomy or dermofasciectomy and skin grafting1,2,6,7,13,14. However, all of the above interventions frequently lead to recurrences15,16,17. Unfortunately, as is the case with fibrosis in general, an effective pharmacological treatment has not been developed yet.
Although DD is a tissue-specific fibrosis, it seems likely that it behaves on a cellular and molecular level in a similar way as other chronic fibrotic processes in different organs of the body. These processes are the result of many different biochemical and biophysical cues. These cues are sensed by fibroblasts, which subsequently are triggered to differentiate into myofibroblasts. The latter cells express α-smooth muscle actin (α-SMA), resulting in the formation of stress fibers that increase cellular contractibility. Simultaneously, myofibroblasts show increased synthesis of extracellular matrix (ECM) proteins such as collagen types I and III and fibronectin-extra domain A (Fn-EDA). Under fibrotic conditions, the balance between the production and degradation of extracellular matrix proteins becomes impaired. The balance is, apart from the production of ECM itself, also determined by the interplay between matrix metalloproteinases and tissue inhibitors of metalloproteinases6,18.
Several molecular pathways have been associated with the onset of DD. Among them, the transforming growth factor β (TGF-β) pathway is highly relevant, as it is in other fibrotic disorders. The profibrotic cytokine TGF-β is involved in the differentiation of fibroblasts towards myofibroblasts, including the maintenance of the activation status of myofibroblasts through the intracellular downstream Smad signaling cascade. Stimulation of the TGF-β pathway results in the phosphorylation of Smad2 and Smad3, forming a complex that binds to Smad4, a complex that in turn activates the transcription of fibrosis-related genes19,20,21. TGF-β levels are increased in DD fibroblasts compared to control fibroblasts, along with its downstream effectors Smad2 and Smad3. As a consequence, ECM markers are also increased. Stimulation with TGF-β1 in vitro increases myofibroblast proliferation, collagen contraction, as well as synthesis of ECM components22,23,24.
Three important intertwined signal transduction routes, namely the transforming growth factor (TGF)-β, the Wingless/Int (WNT), and the yes-associated protein 1 (YAP)/transcriptional coactivator with PDZ-binding motif (TAZ) pathways, have been linked to the pathophysiology of fibrosis25. GWAS studies have shown that several components of the WNT pathway are linked to DD4,5,6, that TGFβ1 is highly expressed in affected DD tissues22,23,24,25, and more recently that YAP is highly expressed in Dupuytren nodules26.
Several preclinical studies revealed that specifically inhibiting the YAP/TAZ pathway by e.g. siRNA results in a major improvement in the outcome of fibrosis27,28. Unfortunately, translation of preclinical fibrosis models into a clinical therapy has often failed, e.g., due to major species differences. Apart from that, introduction of a new drug into the clinic is an expensive and time-consuming process. However, it was recently found that verteporfin (VP), a FDA-approved benzoporphyrin derivative that is already used in the clinic to inhibit macular degeneration, is capable of inhibiting extracellular matrix deposition in liver, kidney and retinal rodent fibrosis models by interfering with the YAP/TAZ pathway18,29,30,31.
By using mouse and rat fibroblasts under various (fibrotic) conditions, it was found that VP inhibits the production of collagen (the hallmark of fibrosis) as well as that of many other profibrotic molecules29,32,33,34,35 . A few studies also investigated the effect of VP on human cells in the context of fibrosis (retinal Müller cells; ventricular fibroblasts; Peyronie plaque fibroblasts; conjunctival fibroblasts; dermal fibroblasts; systemic sclerosis dermal fibroblasts)31,36,37,38,39. In all cases, a decrease is seen in collagen production, either on mRNA level or protein level. Of these studies, only a single paper investigated the effect of VP in human cells at both the mRNA and protein level39. Here we report the effect of VP on nodular fibroblasts from surgically excised tissue of 7 DD patients, both at the mRNA and protein level. Since the aim of our study is to evaluate the anti-fibrotic potential of VP in both the early and late stage of the disease, we created a profibrotic environment by stimulating DD cells with TGF-β1 for 48 h before VP treatment. This was followed by a comparison between DD fibroblasts treated with VP for another 48 h under continued TGF-β1 stimulation (highly activated fibroblasts) with DD fibroblasts without further TGF-β1 stimulation (i.e., fibroblasts with a lower activation level). Our results show a significant decrease of fibrotic markers, both at the mRNA and protein level in both experimental groups, and conclude that VP has major anti-fibrotic properties.
Methods
Reagents for cell culture
Reagents and final concentrations used in culture medium were as follows: Human recombinant TGF-β1 (5 ng/ml; 100-21C, Peprotech, London, UK); ascorbic acid (0.17 mM; A8960, Sigma-Aldrich, Merck KGaA, Darmstadt, Germany); penicillin/streptomycin (pen/strep) (50 U/L; 15,140,122, Thermo Fisher Scientific, Landsmeer, The Netherlands), verteporfin (250 nM; SML0534, Sigma-Aldrich, The Netherlands). Stock solutions of the drug VP were prepared in dimethyl sulfoxide (DMSO) and stored at − 20 °C; the working solutions were diluted in culture medium with a final solvent concentration of ≤ 1%.
Cell culture
Dupuytren tissue was obtained from 7 patients undergoing primary limited fasciectomy or dermofasciectomy (Caucasians from the northern part of the Netherlands; age range 59–67). Informed written consent was obtained through approval of the local ethics committee. Surgical pieces were macroscopically dissected into nodule and cord. Nodules were separated in pieces of 0.5 cm2, four pieces per well were placed in 6 well plates. Isolation of primary nodule fibroblast was performed by the outgrow method in Minimum Essential Medium – Eagle with Earle's BSS (MEM Eagle EBSS; 12-611F, Lonza) containing 20% fetal bovine serum (FBS). FBS was filtered before use through a SFCA 0.45 μm filter. Before the onset of experiments, Dupuytren nodular fibroblasts were propagated in Dulbecco’s modified Eagle medium (DMEM) (12-604F, Lonza) containing 50 U/L pen/strep) and 10% FBS (Sigma-Aldrich). All cells were tested negative for mycoplasm. At the start of the experiment, cells were trypsinized, reseeded at a density of 15.000 cells/cm2, and starved for 18 h in DMEM containing 50 U/L pen/strep, 0.5% FCS and 0.17 mM ascorbic acid. Experiments were carried out in primary fibroblasts passage 4 to 6 with DMEM containing 50 U/L pen/strep, 0.17 mM ascorbic acid, and 0.5% FBS. Treatments were performed as follows (Fig. 1): for all cells, stimulation with 5 ng/ml TGF-β1 in starvation medium for 48 h. Next, cells were treated for 48 h in starvation medium with or without 5 ng/ml TGF-β1 stimulation in the presence of 1% (v/v) DMSO (= control vehicle) or 250 nM VP. Medium was refreshed every 24 h.
RNA extraction and Real-Time PCR
For gene expression analysis, total RNA was isolated with the Tissue Total RNA mini kit (Favorgen Biotech Corp., Taiwan). RNA quantity and quality were determined by UV spectrophotometry (NanoDrop Technologies, Wilmington, DE). One μg of RNA was reverse transcribed with RevertAid First Strand cDNA Synthesis kit (Thermo Fischer Scientific). Real-time PCR was performed with SYBR green PCR master mix (Roche, Basel, Switzerland) and VIIA7 thermal cycling system (Applied Biosystems, Carlsbad, CA). Thermal cycling conditions were 2 min at 95 °C (enzyme activation), followed by 15 s at 95 °C, 30 s at 60 °C and 30° seconds at 72 °C (40 cycles). Melting curve analysis was performed in order to verify the absence of primer dimers. Primers were designed and optimized to have a calculated 95% to 105% reaction efficiency; the used sequences are shown in Table 1. All data were normalized against the reference gene tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein, zeta isoform (YWHAZ). The following genes were measured: the extracellular matrix proteins collagen type I, III, IV and fibronectin-extra domain A (COL1A1, COL3A1, COL4A1 and FN1EDA, respectively), the collagen modifying enzyme lysyl hydroxylase 2 (PLOD2), the cytoskeletal protein alfa-smooth muscle actin (ACTA2), the matricellular protein connective tissue growth factor (CTGF = CCN2), the serpin family protein plasminogen activator inhibitor-1 (PAI1 = SERPINE1), and three Hippo/TGFβ pathway proteins (YAP1, SMAD2 and SMAD3).
Immunofluorescence
Detection of both intracellular and extracellular collagen type I, α-SMA and fn-EDA isoform was carried out on fixed cells with 4% paraformaldehyde (Sigma-Aldrich) for 10 min. Later they were permeabilized with 0.5% Triton X-100 in phosphate-buffered saline (PBS) for 10 min. For all immunostainings, fixed cells were subsequently incubated with PBS + 0.1% Triton, containing 2.2% bovine serum albumin (BSA, Sanquin Reagents, Amsterdam, The Netherlands) and 5% of specific anti-serum antibody for 60 min at room temperature (RT). The primary antibodies were incubated for 120 min at RT. The secondary antibodies were incubated for 30 min at RT. The binding protein Streptavidin Cy3 in PBS + 1% BSA was incubated in the dark for 20 min at RT. Nuclei were visualized with 4′,6-diamidine-2′-phenylindole dihydrochloride (DAPI) (dilution 1:5000). All wash steps were performed in PBS-Tween. The cells were mounted with Citifluor AF1 (AF1-25, Brunschwig Chemie, Amsterdam, The Netherlands). Microphotographs were acquired in a random blind fashion with the use of a Leica TCS SP8 confocal system microscope (Leica Microsystems, Rijswijk, The Netherlands). Antibodies used are shown in Table 2.
Immunoblotting
Cells were lysed with RIPA buffer (Thermo Fischer Scientific) supplemented with 1% protease inhibitor cocktail (Sigma-Aldrich) and 1% phosphatase inhibitor cocktail (Sigma-Aldrich), and lysates were disrupted with sonication. Protein concentrations were determined with a DC protein assay (Bio-Rad, Hercules, CA), and equal amounts of protein (30 µg/ml) per lane were subjected to SDS gel electrophoresis. Protein transfer to a nitrocellulose membrane was performed with the semidry Transblot Turbo system (Bio-Rad). Membranes were blocked in Tris-buffered saline (TBS) + 0.5% Tween20 (Sigma-Aldrich) that contained 5% milk powder. Primary and secondary antibodies were diluted in TBS-Tween20 that contained 5% milk powder. Membranes were cut prior to incubation with primary and secondary antibodies. Primary antibodies were incubated overnight at 4 °C, secondary antibodies were incubated for 60 min at RT. All washing steps were performed in TBS-Tween20. Protein bands were visualized with chemiluminescence and ChemiDoc imaging system (Bio-Rad). Image analyses were performed with Image Lab™ Software version 6.0.1 (Bio-Rad). Original images of blots from all the replicates are included in the supplementary information, acquisition was performed when the total length of the ladder was visible. The antibodies used are shown in Table 2.
Statistical analysis
All data were analyzed with GraphPad Prism version 8.03 (GraphPad Software, La Jolla, CA) using the paired t-test. Values of p < 0.05 (95% confidence interval) were considered to be statistically significant.
Human ethics statement
All methodology followed research integrity covering rules, regulations and best practices in accordance with relevant guidelines and regulations. Tissue samples were collected after informed written consent and approval of the Medical Ethics Committee (METc) of the University Medical Center Groningen (2007/067).
Ethics approval and consent to participate
Obtained.
Consent for publication
Not applicable.
Results
Dupuytren nodular fibroblasts show upregulation of fibrosis-related genes at mRNA level after TGF-β1 stimulation
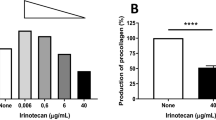
We performed quantitative PCR for COL1A1, COL3A1, COL4A1 and FN1EDA, being a set of extracellular matrix genes that are upregulated in fibrotic pathologies. Other fibrosis-related genes that we measured are SERPINE1 (an inhibitor for plasmin-mediated MMP activation), PLOD2 (an enzyme involved in collagen cross-linking), YAP1 and its downstream target CCN2. Finally, we measured ACTA2, encoding for alfa-smooth muscle actin, that form stress fibers in myofibroblasts. With the exception of YAP1, we observed significant upregulation of all fibrosis-related genes after 96 h TGF-β1 stimulation in comparison with 48 h TGF-β1 stimulation (Fig. 2). Its shows that 48 h of exposure to 5 ng/ml TGF-β1 is not enough to obtain full activation of the fibroblasts. In fact, we observe on average a 3.3-fold increase of mRNA levels of COL1A1 (p = 0.0006), 2.7-fold increase of COL3A1 (p = 0.0013), 11.4-fold increase of COL4A1 (p = < 0.0001), 5.8-fold increase for FN1EDA (p = < 0.0001), 3.7-fold increase for CCN2 (p = 0.0001), 5.1-fold increase for ACTA2 (p = 0.0008), 4.7-fold increase for PLOD2 (p = < 0.0001), 5.2-fold change for SERPINE1 (p = 0.0031). We observed a significant downregulation of the YAP1 gene, showing a 1.4-fold change (p = 0.0082) (Fig. 2). Our results clearly show increased mRNA levels of fibrotic markers in nodule fibroblasts with prolonged TGF-β1 stimulation time. Furthermore, we observed different delta upregulation values after 96 h TGF-β1 exposure between the patients, which seems to indicate a high heterogeneity between patients suffering from DD.
VP treatment decreases gene expression of fibrosis-related genes at mRNA levels in Dupuytren nodular fibroblasts
Next, we investigated the effect of verteporfin in the presence or absence of TGF-β1 on the expression of the genes mentioned in the previous section (COL1A1, COL3A1, COL4A1, FN1EDA, SERPINE1, PLOD2, YAP1, CCN2 and ACTA2) in nodule fibroblasts.
We found that VP decreases significantly the expression levels of the 4 genes encoding for ECM proteins (COL1A1, COL3A1, COL4A1, FN1EDA), both in the presence or absence of TGF-β1. In the group without the presence of TGF-β1, we observed a decrease in 7 of the 9 genes tested (COL1A1, COL3A1, COL4A1, FN1EDA, PLOD2, CCN2, and SERPINE1) with values ranging from 1.4 to 5.5 (Fig. 3). In the group that was exposed to an additional 48 h with TGF-β1, we observed a decrease in 6 of the 9 genes tested (COL1A1, COL3A1, COL4A1, FN1EDA, PLOD2, and SERPINE1) with values ranging from 1. 8 to 3.9 (Fig. 4).
We do not observe a decrease in ACTA2 and YAP1 gene expression when exposed to VP, regardless whether TGF-β1 was present or not. A significant decrease of CCN2 gene expression was seen in the group cultured in the absence of TGF-β1 stimulation. No such significance could be shown in the group cultured in the presence of TGF-β1 stimulation, although a trend in decreasing levels can be observed. Detailed foldchanges in gene expression are presented in Table 3.
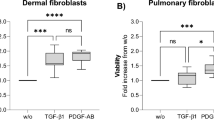
VP affects the translation and morphology of hallmark proteins in fibrosis
Since it is known that there can be a discrepancy between mRNA levels and protein levels, especially in the case of extracellular matrix proteins, we also stained the presence of collagen type I and fibronectin-EDA (fn-EDA) in the cell cultures. Furthermore, we stained the α-SMA stress fibers (the marker of mature myofibroblasts) in the cells themselves. Collagen type I shows a more intense staining with increasing TGF-β1 incubation time (48 vs. 96 h), both intracellularly and as extracellular deposits (Fig. 5a). VP significantly decreased the amount of stained collagen, both in the presence or absence of TGF-β1. Fn-EDA also showed a more intense staining at 96 h TGF-β1 incubation time. As in the case with collagen, the presence of VP decreased the amount of stained fn-EDA (Fig. 5b). In addition, changes in morphology of the deposited fn-EDA are seen. When cells are not stimulated with TGF-β1, a reticular pattern of deposition is observed, which is shifted to a net-like deposition in the presence of TGF-β1. After treatment with VP the reticular pattern is again seen (Fig. 5b). With respect to α-SMA, hardly any α-SMA positive cells were seen at 48 h TGF-β1 stimulation, while clearly increasing numbers were seen at 96 h (Fig. 5c). The presence of VP resulted in a decrease in α-SMA positive cells in a subset of patients only.
Immunofluorescence of hallmark proteins in fibrosis. (a) Synthesis and deposition of collagen type I after 48 and 96 h TGF-β1 stimulation in the presence or absence of VP. Immunofluorescence of intracellular and extracellular collagen type I. (b) Deposition and morphology of Fn-EDA after 48 and 96 h TGF-β1 stimulation in the presence or absence of VP as revealed by immunofluorescence staining. (c) Myofibroblast differentiation after 48 and 96 h TGF-β1 stimulation in the presence or absence of VP as revealed by immunofluorescence staining of α-SMA. Iimages are shown from donors with a high and a low expression (high: patient DDf3 and low: patient DDf7; for mRNA data see Figs. 3 and 4) (magnification 63x, scale-bar = 50 µm).
To strengthen the results as obtained by optical analyses, we next quantified protein levels of collagen type I by Western blot. It is important to note that the protein samples were obtained from cell lysates, so we can only quantify intracellular collagen and not collagen deposited extracellularly, which is the case for collagen type I. As expected, collagen type I levels are rather low when stimulated with TGF-β1 for 48 h only; it became even lower in the presence of VP (Fig. 6). More collagen was observed when cells were stimulated for 96 h, and also here a significant decrease is seen of collagen type I in the presence of VP (Fig. 7). In the case of the myofibroblast marker α-SMA, a major increase is seen with prolonged TGF-β1 incubation times (48 and 96 h), and in both cases α-SMA protein levels were lower in the presence of VP (Fig. 7). This decrease in protein level VP which was not clearly evident by immunostaining of the cells themselves (compare Fig. 5c with Fig. 7).
Western blot analysis and quantification of Col 1a1 and α-SMA in DD nodule-derived fibroblasts after stimulation for 48 h with TGF-β1 followed by 48 h in the presence or absence of VP. Images from donors with high and low expression (high: patient DDf3 and low: patient DDf7). Original blots are presented in Supplementary Fig. 1 (S1).
Western blot analysis and quantification of Col 1a1 and α-SMA in DD nodule-derived fibroblasts after stimulation for 96 h with TGF-β1 but in the last 48 h in the presence or absence of VP. Images from donors with high and low expression (high: patient DDf3 and low: patient DDf7). Original blots are presented in Supplementary Fig. 2 (S2).
VP affects protein levels of YAP, SMAD2 and SMAD3
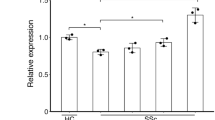
Since we observed that VP downregulates major fibrogenic genes, we further determined the effect of VP on the downstream effectors of the TGF-β and Hippo pathway. We studied gene expression by quantitative PCR and protein levels by Western blot of total YAP1 and SMAD2 and SMAD3. No changes were observed in gene expression levels of YAP1 and SMAD3 by VP, neither with or without the presence of TGF-β1 for 48 or 96 h. In contrast, we observed an upregulation of SMAD2 gene expression after VP treatment in the group under continuous (96 h) TGF-β1 stimulation (Fig. 8).
Effect of VP treatment on TGF-β/Hippo pathway downstream effectors. Relative mRNA expression of YAP1, SMAD2 and SMAD3 after stimulation with TGF-β1 for 48 h followed by 48 h in the presence or absence with VP, or after stimulation with TGF-β1 for 96 h but in the last 48 h in the presence or absence of VP.
On protein expression level, a mild decrease of protein level is seen for all three proteins (YAP1, Smad2 and Smad3) studied as a result of TGF-β1 stimulation. Remarkably, all three proteins become essentially undetectable after VP treatment (Fig. 9).
Effect of VP treatment on TGF-β/Hippo pathway downstream effectors. Western blot analysis and quantification of YAP, Smad2, and Smad3, after stimulation with TGF-β1 for 48 h followed by 48 h in the presence or absence with VP, or after stimulation with TGF-β1 for 96 h but in the last 48 h in the presence or absence of VP. Images are shown from donors with a high and low expression (high: patient DDf3 and low: patient DDf7). Original blots are presented in Supplementary Figs. 3 and 4 (S3 and S4).
Discussion
DD is a chronic, fibroproliferative disorder of the hand fascia, which results in impairment of the extension of fingers and therefore hinders a normal use of the hand. Treatments for DD in early stages unfortunately show lack of effectiveness, while the management of the final stage is invasive and often results in disease recurrence15. Therefore, the need for a treatment that at least prevents the progression of the disease is high. Here we show with in vitro cell cultures of DD nodular fibroblasts that VP is not only able to halt the activation of fibroblasts into myofibroblasts, but is also able to reverse the activation status of the cells.
Differentiation of fibroblasts into myofibroblasts is a relatively slow process. In this study, we first cultured DD nodular fibroblasts in the presence of TGF-β1 for 48 h. After this stimulation period, we subsequently treated the fibroblasts for 48 h with or without verteporfin under two regimes: with or without TGF-β1. In the absence of VP, we observed that in the additional 48 h a further acceleration of the activation status takes place in the presence of TGF-β1. In this additional time period, an increase is seen in mRNA levels of COL1A1, COL3A1, COL4A1, FN1EDA, PLOD2, ACTA2, CCN2 and SERPINE1, which is substantiated by the increased protein levels of collagen type I, fn-EDA and α-SMA. In this experimental setup, one is able to investigate1 whether VP is able to push back the achieved activation status of the first stimulation period (namely the experiment with VP in the absence of TGF-β1), and2 whether VP is able to halt an ongoing activation in cells that are already triggered to become myofibroblasts (namely the experiment with VP in the presence of TGF-β1).
Our experiments show that VP has strong anti-fibrotic properties: it not only pushes back the activation status of fibroblasts that are exposed for 48 h to TGF-β1, but it also halts an ongoing activation of cells that are in the process of becoming myofibroblasts. In both experimental settings mRNA levels of COL1A1, COL3A1, COL4A1, FN1EDA, PLOD2, CCN2 and SERPINE1 are significantly decreased, and this is also observed in the protein levels of collagen type I. We observed in addition changes in the morphology of the deposited fn-EDA, namely from a mesh-like deposition to a reticular network in the presence of VP (the other genes were not investigated with regard to protein levels). Keeping in mind that the hallmark of fibrosis (and DD) is an unwanted accumulation of collagen (especially collagen type I), this is quite promising.
The decrease of COL1A1 gene expression after VP treatment has also been found in in vivo preclinical models of kidney and hepatic fibrosis29,32,35. It has also been observed in rodent and human in vitro models, namely rat hepatic stellate cells, angiotensin II-stimulated primary human ventricular fibroblasts, and TGF-β1 stimulated dermal fibroblasts33,36,39. Moreover, our results correlate with data obtained from myofibroblasts isolated from other pathological tissues, namely plaque tissue from Peyronie’s disease and forearm skin of patients with diffuse subset scleroderma, where expression of COL1A1 is also decreased after VP treatment37,39. As is the case with mRNA, a decrease in protein expression of collagen type I has also been reported18,29,30,31,32,34,]35.
The expression of a variety of profibrotic genes is activated by nuclear YAP and Smad2/318,29,30,]31,32,35,36,38,40. We therefore measured mRNA and protein levels of these three molecules. We found no effect of VP on mRNA levels of these three genes when fibroblasts are stimulated for 48 h with TGF-β1. The same was the case with YAP1 and SMAD3 in fibroblasts stimulated for 96 h with TGF-β1, whereas SMAD2 was slightly upregulated. However, in all cases the protein levels of YAP1, Smad2 and Smad3 were dramatically decreased in the presence of VP, being an explanation why VP is able to attenuate the expression of a large variety of important pro-fibrotic molecules.
The accumulation of collagen in fibrotic diseases (such as in DD) is due to a disbalance between collagen synthesis and collagen degradation. In fibrosis, more collagen is synthesized, and there is less collagenolytic activity. SERPINE1 is an inhibitor for plasmin-mediated MMP activation41,42. VP not only attenuated the synthesis of collagen, it also attenuated SERPINE1 levels, thus facilitating plasmin-mediated MMP activation (and consequently collagen breakdown). PLOD2 encodes for lysyl hydroxylase 2, an enzyme involved in the formation of a specific cross-link type of collagen, making collagen more resistant towards collagenases7,43,44. We found that VP also decreases mRNA levels of PLOD2, thus making the deposited collagen more susceptible towards collagenases.
It is well established, that myofibroblasts are at the heart of fibrosis: these are the cells that produce the collagen that replaces functional tissues into fibrotic tissues. Myofibroblasts are characterized by the presence of α-SMA stress fibers; these fibers are absent in fibroblasts. Interestingly, VP did not affect mRNA levels of ACTA2 (encoding for α-SMA), only modestly affected protein levels (as revealed by Western blotting), and no change was seen in the percentage α-SMA positive cells in some of the patients. Despite this, all subjects showed a major decrease in e.g. collagen levels. Thus, although the cells would still be classified as myofibroblasts based on the presence of α-SMA stress fibers, the overall phenotypical properties of the cells are that of a fibroblast. Although a full inhibition of myofibroblasts can be achieved by e.g. using higher concentrations of VP29,36,45, such concentrations might not be necessary to achieve the desired outcome (i.e. inhibition of extracellular matrix accumulation).
CCN2 (= CTGF) gene expression is induced by TGF-β1 stimulation and is a direct target of the YAP/TAZ-TEAD complex46,47,48. An inhibition of YAP by VP should therefore result in lower mRNA levels of CCN2. Our results show that VP treatment indeed decreases CCN2 gene expression both in non-stimulated and stimulated cells, which is in line with other studies18,29,34,37,39,45.
In our study, VP did not influence the gene expression (mRNA level) of the myofibroblast marker ACTA2 in 48 h or in 96 h stimulated cells. From the five in vitro studies that report a decrease in ACTA2 gene expression, three used higher concentrations of VP29,36,45. We used a concentration of 0.25 µM, while the range of dose of others goes from 0.5 µM up to 1.5 µM. The other two studies18,32 used a lower or the same concentration as used by us. In myofibroblasts isolated from Peyronie’s tissue there is a significant decrease of ACTA2 after the first 24 h of VP treatment, while after 48 h of treatment ACTA2 was not significantly reduced anymore37. This suggests that a 0.25 μM concentration of VP can initially influence the transcription of ACTA2, but that this effect is diminished at longer treatment times. A decrease was also observed in TGF-β1 stimulated (but not unstimulated) rat kidney interstitial myofibroblasts after 24 h of treatment18. Unfortunately, there are no data regarding a longer treatment time to corroborate our hypothesis whether the decrease in mRNA is time-dependent. It should be stressed that although we did not see a decrease in mRNA levels of ACTA2, we do see a significant decrease of the protein on Western blots.
The mechanism of action of VP is not completely understood yet, but recent studies show its ability to inhibit TGF-β1 nuclear accumulation of the YAP/Smad2/3 complex in two unilateral ureter obstruction mouse models of renal fibrogenesis and renal tubulointerstitial fibrosis, as well as in human conjunctival fibroblasts and rat kidney interstitial fibroblasts18,35,38,40. Our results confirm that VP treatment of DD nodule-derived fibroblasts decreases the total protein levels of YAP and Smad2/3 with little influence in gene expression, correlating well with the data from previous studies, further demonstrating that VP targets DD through this mechanism of action. It is important to note that YAP silencing has not shown the same strong results as VP treatment18,26, which suggest the involvement of additional mechanisms of action of VP. Recent studies show that VP has an effect on the Wnt pathway as it decreases levels of β-catenin in TGF-β1 stimulated hepatic stellate cells and in TGF-β2 stimulated conjunctival fibroblasts34,38. Interestingly, GWAS studies revealed the possible association of several components of the WNT pathway with DD, and protein studies revealed that certain elements of the WNT pathway are indeed up- or downregulated in DD5,6,49.
Conclusion
Verteporfin (known under the marketing name Visudyne) is an FDA-approved drug for the treatment of macular degeneration. The route of administration is intravenously, and needs to be photo-activated in the eye by means of a laser, resulting in a selective vaso-occlusive treatment by targeting choroidal vascular abnormalities. The anti-fibrotic properties of verteporfin do not rely on photo-activation, as the molecule inhibits YAP when it is in a non-photoinduced state. It is promising that VP is able to inhibit the expression of a large set of pro-fibrotic genes, in various preclinical fibrosis models (liver, kidney), in various fibroblasts (rat, mouse, human), and in fibroblasts that display various activation states. As shown here, it is even able to reverse the activation level of fibroblasts. Furthermore, it is effective in a concentration (0.25 μM) that is at least a magnitude below its cyctotoxicity level (2 μM; see30). Although further studies are necessary, verteporfin seems to have potential of a broad-spectrum anti-fibrotic drug, as shown here in the context of DD nodular fibroblasts. So far, only Nintedanib and Pirfenidone are marketed as anti-fibrotic drugs, but serious side effects have been reported, and so far, the efficacy of these drugs to prevent the progression of fibrosis is rather limited50,51,52,53,54.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- α-SMA:
-
α-Smooth muscle actin
- BSA:
-
Bovine serum albumin
- DAPI:
-
4′,6-Diamidine-2′-phenylindole dihydrochloride
- DD:
-
Dupuytren’s disease
- DMEM:
-
Dulbecco’s modified Eagle medium
- DMSO:
-
Dimethyl sulfoxide
- ECM:
-
Extracellular matrix
- FBS:
-
Fetal bovine serum
- Fn-EDA:
-
Fibronectin-extra domain A
- GWAS:
-
Genome-wide association study
- PBS:
-
Phosphate-buffered salt
- RT:
-
Room temperature
- TBS:
-
Tris-buffered saline
- TGF-β1:
-
Transforming growth factor β1
- VP:
-
Verteporfin
References
Shih, B. & Bayat, A. Scientific understanding and clinical management of Dupuytren disease. Nat. Rev. Rheumatol. 6(12), 715–726 (2010).
Karkampouna, S. et al. Novel ex vivo culture method for the study of Dupuytren’s disease: Effects of TGFβ type 1 receptor modulation by antisense oligonucleotides. Mol. Ther. Nucl. Acids. 3, e142 (2014).
Larsen, S. et al. Genetic and environmental influences in Dupuytren’s disease: A study of 30,330 Danish twin pairs. J. Hand. Surg. 40(2), 171–176 (2015).
Dolmans, G. H. et al. Wnt signaling and Dupuytren’s disease. N. Engl. J. Med. 365(4), 307–317 (2011).
Becker, K. et al. Meta-analysis of genome-wide association studies and network analysis-based integration with gene expression data identify new suggestive loci and unravel a Wnt-centric network associated with Dupuytren’s disease. PLoS ONE 11(7), e0158101 (2016).
Ng, M. et al. A genome-wide association study of Dupuytren disease reveals 17 additional variants implicated in fibrosis. Am. J. Hum. Genet. 101(3), 417–427 (2017).
Sayadi, L. R. et al. The molecular pathogenesis of Dupuytren disease: Review of the literature and suggested new approaches to treatment. Annals Plast. Surg. 83(5), 594–600 (2019).
Pratt A, Ball C. Dupuytren ’ s disease—The role of hand therapy. In: Living Textbook of Hand Surgery 2015:1–7.
Ball, C., Izadi, D., Verjee, L. S., Chan, J. & Nanchahal, J. Systematic review of non-surgical treatments for early Dupuytren’s disease. BMC Musculoskelet. Disord. 17(1), 345 (2016).
Badalamente, M. A., Hurst, L. C. & Hentz, V. R. Collagen as a clinical target: Nonoperative treatment of Dupuytren’s disease. J. Hand. Surg. Am. 27(5), 788–798 (2002).
Hurst, L. C. et al. Injectable collagenase Clostridium histolyticum for Dupuytren’s ontracture. N. Engl. J. Med. 361(10), 968–979 (2009).
Scherman, P., Jenmalm, P. & Dahlin, L. B. Three-year recurrence of Dupuytren’s contracture after needle fasciotomy and collagenase injection: a two-centre randomized controlled trial. J. Hand. Surg. 43(8), 836–840 (2018).
Black, E. M. & Blazar, P. E. Dupuytren disease: An evolving understanding of an age-old disease. Am. Acad. Orthop. Surg. 19(12), 746–757 (2011).
Rodrigues, J. N. et al. Surgery for Dupuytren’s contracture of the fingers. Cochrane Database Syst. Rev. 12, CD010143 (2015).
Karkampouna, S. et al. Connective tissue degeneration: Mechanisms of palmar fascia degeneration (Dupuytren’s disease). Curr. Mol. Biol. Rep. 2(3), 133–140 (2016).
Karakaplan, M. Percutaneous needle aponeurotomy for the treatment of Dupuytren’s contracture. Jt. Dis. Relat. Surg. 30(1), 53–60 (2019).
Alfonso-Rodríguez, C. A. et al. Identification of histological patterns in clinically affected and unaffected palm regions in Dupuytren’s disease. PLoS ONE 9(11), e112457 (2014).
Szeto, S. G. et al. YAP/TAZ are mechanoregulators of TGF-β-Smad signaling and renal fibrogenesis. J. Am. Soc. Nephrol. 27(10), 3117–3128 (2016).
Carthy, J. M. TGFβ signaling and the control of myofibroblast differentiation: Implications for chronic inflammatory disorders. J. Cell. Physiol. 233(1), 98–106 (2018).
Vallée, A. & Lecarpentier, Y. TGF-β in fibrosis by acting as a conductor for contractile properties of myofibroblasts. Cell Biosci. 9(1), 98 (2019).
Distler, J. H. W. et al. Shared and distinct mechanisms of fibrosis. Nat. Rev. Rheumatol. 15(12), 705–730 (2019).
Krause, C., Kloen, P. & ten Dijke, P. Elevated transforming growth factor β and mitogen-activated protein kinase pathways mediate fibrotic traits of Dupuytren’s disease fibroblasts. Fibrogenesis Tissue Repair. 4(1), 14 (2011).
Badalamente, M. A., Sampson, S. P., Hurst, L. C., Dowd, A. & Miyasaka, K. The role of transforming growth factor beta in Dupuytren’s disease. J. Hand. Surg. Am. 21(2), 210–215 (1996).
Satish, L., Gallo, P. H., Baratz, M. E., Johnson, S. & Kathju, S. Reversal of TGF-β1 stimulation of α-smooth muscle actin and extracellular matrix components by cyclic AMP in Dupuytren’s - derived fibroblasts. BMC Musculoskelet. Disord. 12(1), 113 (2011).
Piersma, B., Bank, R. A. & Boersema, M. Signaling in fibrosis: TGF-β, WNT, and YAP/TAZ converge. Front. Med. 2, 1–14 (2015).
Piersma, B. et al. YAP1 is a driver of myofibroblast differentiation in normal and diseased fibroblasts. Am. J. Pathol. 185(12), 3326–3337 (2015).
Qin, Z., Xia, W., Fisher, G. J., Voorhees, J. J. & Quan, T. YAP/TAZ regulates TGF-β/Smad3 signaling by induction of Smad7 via AP-1 in human skin dermal fibroblasts. Cell Commun. Signal. 16(1), 18 (2018).
Lee, M. J., Byun, M. R., Furutani-Seiki, M., Hong, J. H. & Jung, H. S. YAP and TAZ regulate skin wound healing. J. Invest. Dermatol. 134(2), 518–525 (2014).
Mannaerts, I. et al. The Hippo pathway effector YAP controls mouse hepatic stellate cell activation. J. Hepatol. 63(3), 679–688 (2015).
Liang, M. et al. Yap/Taz deletion in gli+ cell-derived myofibroblasts attenuates fibrosis. J. Am. Soc. Nephrol. 28(11), 3278–3290 (2017).
Zhang, W. & Kong, Y. YAP is essential for TGF-β-induced retinal fibrosis in diabetic rats via promoting the fibrogenic activity of Müller cells. J. Cell Mol. Med. 24(21), 12390–12400 (2020).
Leung, J. Y. et al. Sav1 loss induces senescence and Stat3 activation coinciding with tubulointerstitial fibrosis. Mol. Cell. Biol. 37(12), 1–17 (2017).
Du, K. et al. Hedgehog-YAP signaling pathway regulates glutaminolysis to control activation of hepatic stellate cells. Gastroenterology 154(5), 1465–1479 (2018).
Yu, H. et al. Blockade of YAP alleviates hepatic fibrosis through accelerating apoptosis and reversion of activated hepatic stellate cells. Mol. Immunol. 107, 29–40 (2019).
Jin, J. et al. Inhibition of yes-associated protein by verteporfin ameliorates unilateral ureteral obstruction-induced renal tubulointerstitial inflammation and fibrosis. Int. J. Mol. Sci. 21(21), 8184 (2020).
Francisco, J. et al. Blockade of fibroblast YAP attenuates cardiac fibrosis and dysfunction through MRTF-A inhibition. JACC Basic Transl. Sci. 5(9), 931–945 (2020).
Mohede, D. C. J., de Jong, I. J., Bank, R. A. & van Driel, M. F. Verteporfin as a medical treatment in Peyronie’s disease. Sex Med. 6(4), 302–308 (2018).
Futakuchi, A. et al. YAP/TAZ are essential for TGF-β2–mediated conjunctival fibrosis. Investig. Opthalmol. Vis. Sci. 59(7), 3069 (2018).
Shi-wen, X. et al. Verteporfin inhibits the persistent fibrotic phenotype of lesional scleroderma dermal fibroblasts. J. Cell Commun. Signal 15(1), 71–80 (2021).
Gui, Y. et al. Yap/Taz mediates mTORC2-stimulated fibroblast activation and kidney fibrosis. J. Biol. Chem. 293(42), 16364–16375 (2018).
Kim, K. K., Sheppard, D. & Chapman, H. A. TGF-β1 signaling and tissue fibrosis. Cold Spring Harb. Perspect. Biol. 10(4), a022293 (2018).
Ghosh, A. K. & Vaughan, D. E. PAI-1 in tissue fibrosis. J. Cell Physiol. 227(2), 493–507 (2012).
Gjaltema, R. A. F. & Bank, R. A. Molecular insights into prolyl and lysyl hydroxylation of fibrillar collagens in health and disease. Crit. Rev. Biochem. Mol. Biol. 52(1), 74–95 (2017).
Karsdal, M. A. et al. The good and the bad collagens of fibrosis—Their role in signaling and organ function. Adv. Drug Deliv. Rev. 121, 43–56 (2017).
Fearing, B. V. et al. Verteporfin treatment controls morphology, phenotype, and global gene expression for cells of the human nucleus pulposus. JOR Spine. 3(4), 1–16 (2020).
Kim, C.-L., Choi, S.-H. & Mo, J.-S. Role of the Hippo pathway in fibrosis and cancer. Cells 8(5), 468 (2019).
Noguchi, S., Saito, A. & Nagase, T. YAP/TAZ signaling as a molecular link between fibrosis and cancer. Int. J. Mol. Sci. 19(11), 3674 (2018).
Hinz, B., McCulloch, C. A. & Coelho, N. M. Mechanical regulation of myofibroblast phenoconversion and collagen contraction. Exp. Cell Res. 379(1), 119–128 (2019).
ten Dam, E.-J.P.M., van Beuge, M. M., Bank, R. A. & Werker, P. M. N. Further evidence of the involvement of the Wnt signaling pathway in Dupuytren’s disease. J. Cell Commun. Signal 10(1), 33–40 (2016).
Marcos Ribes, B. et al. Effectiveness and safety of pirfenidone for idiopathic pulmonary fibrosis. Eur. J. Hosp. Pharm. 27(6), 350–354 (2020).
Li, X., Zhu, L., Wang, B., Yuan, M. & Zhu, R. Drugs and targets in fibrosis. Front. Pharmacol. 8, 855 (2017).
Raghu, G. & Selman, M. Nintedanib and pirfenidone. New antifibrotic treatments indicated for idiopathic pulmonary fibrosis offer hopes and raises questions. Am. J. Respir. Crit. Care Med. 191(3), 252–4 (2015).
Hughes, G., Toellner, H., Morris, H., Leonard, C. & Chaudhuri, N. Real world experiences: Pirfenidone and nintedanib are effective and well tolerated treatments for idiopathic pulmonary fibrosis. J. Clin. Med. 5(9), 78 (2016).
Bando, M. et al. Clinical experience of the long-term use of pirfenidone for idiopathic pulmonary fibrosis. Intern Med. 55(5), 443–448 (2016).
Acknowledgements
We thank the patients who participated in this study.
Funding
No external funding was obtained.
Author information
Authors and Affiliations
Contributions
B.P., N.P., P.O., and R.B. conceived the presented idea. B.P., N.P. and R.B. conceived the experimental setup. S.R. and I.H. isolated and cultured cells; S.R. performed part of the experiments and N.P. performed most experiments and analyzed with R.B. and P.O. all data. P.W. contributed with discussion and performed or supervised the surgeries. N.P. and R.B. drafted and wrote the manuscript. P.O., P.W. and R.B. revised and approved the manuscript. All authors contributed to the article and approved the submitted version. Disclosure P.W. was member of SERB for Frida Ltd (Milan) during a phase 1 clinical trial concerning the development of a new collagenase for DD treatment.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Puerta Cavanzo, N., Riesmeijer, S.A., Holt-Kedde, I.L. et al. Verteporfin ameliorates fibrotic aspects of Dupuytren’s disease nodular fibroblasts irrespective the activation state of the cells. Sci Rep 12, 13940 (2022). https://doi.org/10.1038/s41598-022-18116-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18116-9
This article is cited by
-
Deciphering the spatial landscape and plasticity of immunosuppressive fibroblasts in breast cancer
Nature Communications (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.