Abstract
The effect of metabolic syndrome (MetS) and clusters of its components on central blood pressure (CBP) has not been well characterized. We aimed to describe the effect of MetS and clusters of its components on CBP in a large population and to identify whether this effect differs in men and women. We studied 15,609 volunteers (43% women) from 10 cohorts worldwide who participated in the Metabolic syndrome and Artery REsearch Consortium. MetS was defined according to the NCEP-ATP III criteria (GHTBW, glucose, high-density lipoprotein cholesterol, triglyceride, blood pressure, waist circumference). CBP was measured noninvasively and acquired from pulse wave analysis by applanation tonometry. MetS was associated with a 50% greater odds of having higher CSBP. After controlling for age, male sex, non HDL cholesterol, diabetes mellitus, and mean arterial pressure, only specific clusters of MetS components were associated with a higher CSBP; and some of them were significant in women but not in men. We identified “risky clusters” of MetS variables associated with high CSBP. Future studies are needed to confirm they identify subjects at high risk of accelerated arterial aging and, thus, need more intensive clinical management.
Similar content being viewed by others
Introduction
Brachial blood pressure measurement is the most widely used approach in managing hypertension in daily clinical practice. Many epidemiological and interventional studies showed an undeniable beneficial effect of lowering brachial blood pressure for cardiovascular (CV) and renal outcomes1. However, the accuracy of peripheral systolic and diastolic blood pressure in reflecting central blood pressure has been questioned since 20072. This challenge has paralleled the increasing attention to large arteries. Indeed, recent research has focused on accelerated to healthy/supernormal vascular aging3,4,5 and the possible role of vascular geometry6; aortic stiffness as an independent predictor of cardiovascular morbidity7 and its association with the progression of cognitive impairment8 and multiple organ damage9,10,11; the definition of a “normality threshold” for clinical purposes12 and the role of arterial aging in response to treatment13; and the issue of central blood pressure in routine clinical practice14.
Whereas mean arterial pressure (MBP) and diastolic blood pressure (DBP) are relatively constant along the arterial tree, the height of the pressure pulse is amplified from the aorta toward peripheral arteries15. Therefore, brachial SBP is higher than central systolic blood pressure (CSBP). These differences decreases with advancing age and are affected by sex, body height, and cardiovascular risk factors (e.g., dyslipidemia, diabetes, and smoking)16.
As peripheral tissues to central (aortic) rather than brachial pressures, CBP has shown a stronger association with left ventricular hypertrophy, intima-media thickness, and pulse wave velocity17. And CBP was a stronger predictor of CV events than brachial BP18,19,20. Moreover, interventional studies showed that specific antihypertensive drug treatment differentially impacts on brachial and CSBP21,22.
Metabolic syndrome (MetS) is a complex construct encompassing several clusters of five components (low HDL cholesterol, increased fasting glucose, increased triglyceride, elevated waist circumference, and elevated peripheral blood pressure). The effects of Mets and the selected cluster of MetS components on large artery stiffness and thickness have been described in a previous report from the MARE Consortium23. However, the effect of MetS and clusters of MetS components on CBP has not yet been described in large populations.
The present cross-sectional, observational study aims to describe the association between MetS and selected clusters of its components on CBP in a large global population and identify possible sex differences in this association.
Subjects and methods
The MARE consortium
The original MARE (Metabolic Syndrome and Artery Research) Consortium aimed to identify diverse metabolic syndrome clusters and their association with vascular aging, gene-lifestyle interactions, and cardiovascular risk among ten cohort studies worldwide and to develop novel cardiovascular prevention methods based on lifestyle modification. The detailed methodology is published elsewhere23. The MARE Consortium is open to additional participating cohorts if data on the MetS components and arterial properties become available for the recruited subjects. The affiliates providing data for the present study are described in Appendix 1 and include subjects from Belgium, Portugal, Greece, Taiwan, Lithuania, Sweden, Russia, the Netherlands, and Italy. All participating countries provided approval for this study.
The ethical committee approved this international multicenter study of Ghent University Hospital and the University of Pennsylvania Institutional Review Board; the Committee of ethics of research with the medicine of the health area of Salamanca; the Ethics committee for the health of Guimaraes; the Ethics Committee of the Athens Medical School; Yu-li Veterans Hospital Ethics Committee; the Vilnius Regional Bioethics Committee of Clinical Research; the Ethical Committee at the Lund University; The ethics committee of the National Research Centre for Preventive Medicine in Moscow; The Medical Ethics Committee of Erasmus University; Bro Taf Local Research Ethics Committee in Cardiff; by the institutional Ethical Committee on human research of the University of Brescia (details provided in Appendix 1).
Each subject gave informed consent.
The MARE Consortium was performed in line with the principles of the Declaration of Helsinki and Title 45, U.S. Code of Federal Regulations, Part 46, Protection of Human Subjects, Revised November 13, 2001, effective December 13, 2001. All methods of this study were performed following the relevant guidelines and regulations stated in the Declaration of Helsinki.
Definition of the metabolic syndrome
MetS was defined according to The Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (NCEP ATP III)24 criteria, where the metabolic syndrome is diagnosed if three or more of the following five components are present:
-
(1)
Elevated fasting glucose (G) (≥ 110 mg/dl) or the presence of drug treatment for increased glucose;
-
(2)
Low HDL cholesterol (H) (< 40 mg/dl in men and < 50 mg/dl in women) or the presence of a specific treatment for lipid abnormalities;
-
(3)
High triglycerides (T) (≥ 150 mg/dl) or the presence of a particular treatment for lipid abnormalities;
-
(4)
Elevated blood pressure (systolic or diastolic, ≥ 130 or ≥ 85 mmHg) (B) or presence of antihypertensive treatment;
-
(5)
Abdominal obesity (W) with a waist circumference of more than 102 cm in men and more than 88 cm in women.
Since at least three components define metabolic syndrome, the study subjects could have had 16 different MetS component combinations.
Brachial and central blood pressure measurements
Brachial blood pressure (BP) was measured according to European Society of Hypertension recommendations25. Pulse pressure (PP) was determined as systolic BP minus diastolic BP in mmHg. Mean arterial pressure (MBP) calculated as diastolic BP + 1/3 (PP).
After resting for 10 min in the supine position, central blood pressure was measured noninvasively and acquired from pulse wave analysis by applanation tonometry (SphygmoCor, AtCor Medical Pty Ltd, Sydney, Australia) at the femoral artery or common carotid artery. The heart rate was monitored using three-lead electrocardiography. All measurements were performed by a trained operator three times in a row; the goal operator index was considered greater than 80%. Only measurements that fulfilled these requirements were analyzed. Elevated central systolic BP was defined as higher than or equal to 140 mmHg.
The gold standard method for CBP is invasive measurement. According to the previous reports26, the applanation tonometry derived CBP overestimates the invasively measured CBP by 0.3 ± 1.0 mmHg.
Statistical analysis
All analyses were performed using the SAS package for Windows (9.1 Version Cary, NC, US). ANOVA followed by the Bonferroni test was adopted to compare means among subgroups of subjects. Least square means (± standard error, SEM) were calculated with ANCOVA analysis to compare CSBP, CPP, and pulse pressure amplification (PPA) values and to compare CSBP values across clusters of MetS components after controlling for covariates (age, sex, non HDL cholesterol (nonHDL-C) levels, MBP, presence of diabetes mellitus). To test for possible age- or sex-specific differences in CSBP and CPP across MetS clusters, interaction terms for sex, age, and MetS clusters were alternatively introduced into separate models.
Multivariable logistic regression models were constructed to identify potential clusters of MetS components associated with high CSBP (= > 140 mmHg).
A two-sided p-value < 0.05 indicated statistical significance.
Results
The characteristics of the 15,609 participants (43% women) from cohorts participating in the MARE consortium are illustrated in Table 1. CPP, but not CSBP, was significantly greater in women than in men (51 ± 18 vs. 49 ± 17 mmHg, p < 0.001).
Effects of specific clusters of MetS components on CSBP
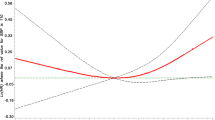
Both CSBP and CPP levels progressively increased with the number of altered MetS components (Fig. 1).
Central systolic blood pressure and pulse pressure values according to the number of altered MetS components. Men—black bars, women—gray bars. Numbers from 0 to 5 indicate the numbers of MetS components. Significant sex-specific differences in CSBP (p < 0.001) and in CPP (p < 0.001). Three components or more are considered typical of MetS.
In the model including age, sex, brachial SBP and DBP, and use of antihypertensive medications, MetS was associated with a 50% greater odds of having high CSB (OR 1.50; 95% CI: 1.38–1.63, p < 0.001).
Then we tried to identify specific clusters of MetS components associated with higher CSBP, as previously illustrated for large artery stiffness and thickness. As expected, a cluster of MetS components with elevated brachial BP had higher CSBP and CPP levels (data not shown) than those MetS clusters without elevated BP levels. Therefore, to account for differences in brachial BP levels, glucose, and lipid levels according to the cluster of MetS components, multivariable logistic regression models were constructed, including non HDL-C, MBP, and presence of diabetes mellitus—together with age and sex—as covariates; and controlling for age, male sex, nonHDL-C, MBP, and presence of diabetes mellitus.
Except for low HDL-C-hypertriglyceridemia-abdominal obesity (HTW), the other combinations of MetS components were accompanied by a 1.3 to a 4.0 fold greater odds of presenting high CSBP (Fig. 2). Of note, in addition to HTW, HBW and GHBW MetS clusters were not associated with greater CSBP levels in men but not in women (Fig. 2 bottom panels).
Clusters of MetS components as determinants of high CSBP—controlling for age, diabetes mellitus, nonHDL-C, and mean blood pressure. Odds ratio (OR) with 95% confidence interval for specific MetS clusters of components in the whole population (upper panel), in men (central panel), and women (lower panel). We evaluated all the possible combinations of MetS components, but only specific clusters are described here. Abbreviations: All other MetS comb., all different combinations of metabolic syndrome components not depicted in the picture; MetS, metabolic syndrome; W, abdominal obesity; H, low HDL cholesterol; B, high blood pressure; T, triglycerides; G, glucose; MAP, mean arterial pressure. Not significant clusters in men: HTW, HBW, GHBW; in women: HTW; in the whole population: HTW.
Secondary analyses, run after excluding participants using antihypertensive medications, showed that the cluster of MetS components TBW (OR 1.52, 05% CI 1.05–2.20), HTB (OR 1.85, 95% CI 1.15 -2.97), and GHTBW (OR 3.40, 95% CI 1.99–5,81) were associated with higher CSBP after controlling for age, sex, diabetes, non HDL cholesterol, and MBP levels.
Discussion
The present cross-sectional, observational study showed that MetS was associated with greater odds of having higher CSBP, independent of age, sex, and brachial blood pressure levels. However, not all the clusters of MetS components defining “the metabolic syndrome” were associated with high CSBP, and sex-differences were observed in the specific MetS clusters associated with high CSBP.
Large arteries are heterogeneous, and their functional and structural properties are poorly correlated with each other27,28. Measures of large artery structure and function as markers of vascular aging have emerged as independent predictors of CV morbidity and related disability29.
Notably, specific clusters of MetS components—namely HBW, TBW, and GBW—have been constantly associated with greater odds not only of high CSBP but also of stiffer23 and thicker29 arteries.
Given the cross sectional-nature of the MARE Consortium, including large population studies, we can only speculate about potential pathophysiological mechanisms underlying our findings.
The first interpretation—identifying a bias rather than a finding—may suggest that MetS clusters, including the “elevated (brachial) blood pressure” (B) component, carried greater odds of having high CSBP simply because of the high correlation between brachial and central SBP levels.
Though we cannot rule out this interpretation, it does not seem to represent the most accurate explanation. When subjects receiving antihypertensive treatment were excluded, not all the MetS clusters, including the “elevated (brachial) blood pressure” (B) component, were associated with significantly greater odds of having high CSBP.
Additionally, in men, specific MetS clusters, including elevated brachial blood pressure (HBW and GHBW), were not associated with greater odds of having high CSBP.
Furthermore, a significant association between HTW and high CSBP had been expected, but it has not been observed in the present study. In fact, visceral adiposity has been associated with a fivefold higher risk of hypertension30. Recently, the adipose tissue has emerged as an endocrine organ, secreting adipokines (adiponectin, pectin, etc.) with a systemic impact on the cardiac and vascular system. Lower adiponectin levels were observed in the presence of higher ambulatory 24-h blood pressure in the Porto Alegre cohort31. Lower adiponectin levels have been associated with stiffer arteries independently of MetS components in the SardiNIA Study32 and hypertensive subjects with MetS33. Adipose tissue also expresses mineralocorticoid receptors, modulating vascular remodeling, development of glucose tolerance, and obesity34.
A relevant unanswered question remains whether these clusters recognize a common altered pathway of pathophysiological relevance—with or without a genetic basis—remains speculative to date. However, these MetS clusters likely identify subjects with accelerated arterial aging, at greater risk of CV mortality and disability, and, thus, need a more intensive management.
Despite ongoing research collaborations and activities in gender-related science, further research is needed to analyze the sex-specific interplay between MetS and central hemodynamics. Two decades ago35, different large artery properties showed elevated CBP in men younger than 40 years compared to women. The Bogalusa Heart Study36 observed a more pronounced discrepancy between peripheral and central blood pressure in women than in men. The SardiNIA Study reported a stronger association of visceral obesity with arterial stiffness in women than in men37. Gender differences have also been reported for genetic markers of visceral adiposity38. We also report a steeper CSBP slope with age in women than in men, with a turning point at 50 years of age, after which the difference disappears. Our study observed higher CPP in women not dependent on MetS components such as elevated brachial blood pressure and abdominal obesity.
Yet, the sex-specific differences in central hemodynamics in the context of MetS still need clarification.
One limitation of this study is represented by its cross-sectional design. Additionally, no information on antihypertensive drug classes was universally coded and available for participants from all MARE Consortium cohorts.
This multicenter, multiethnic observational study confirms that the greater odds of having high CSBP associated with the presence of MetS hides a constellation of phenotypes that are not equally risky of arterial aging, whether indexed as central BP, large artery stiffness, or thickness.
Identification of “risky clusters” in the whole population and specific to sex may contribute to a more personalized management of CV risk and lead to the identification of novel pathways accelerating arterial aging.
Further studies are needed to elucidate the sex-specific interplay between MetS components and the pathophysiology of vascular aging.
References
Xie, X. et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: Updated systematic review and meta-analysis. Lancet 387, 435–443 (2016).
Mancia, G. et al. 2007 Guidelines for the management of arterial hypertension. Eur. Heart J. 28, 1462–1536 (2007).
Calimport, S. R. G. et al. To help aging populations, classify organismal senescence. Science 1979(366), 576–578 (2019).
Nilsson, P. M. et al. Characteristics of healthy vascular ageing in pooled population-based cohort studies: The global metabolic syndrome and artery research consortium. J. Hypertens. 36, 2340–2349 (2018).
Cunha, P. G. et al. Pulse wave velocity distribution in a cohort study: Fromarterial stiffness to early vascular aging. J. Hypertens. 33, 1438–1445 (2015).
Scuteri, A. et al. Functional correlates of central arterial geometric phenotypes. in Hypertension vol. 38 1471–1475 (Lippincott Williams and Wilkins, 2001).
Vlachopoulos, C., Aznaouridis, K. & Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 55, 1318–1327 (2010).
Scuteri, A. & Wang, H. Pulse wave velocity as a marker of cognitive impairment in the elderly. J. Alzheimer’s Dis. 42, S401–S410 (2014).
Scuteri, A. et al. Arterial stiffness and multiple organ damage: A longitudinal study in population. Aging Clin. Exp. Res. https://doi.org/10.1007/s40520-019-01260-0 (2019).
Scuteri, A. et al. An operational definition of SHATS (Systemic Hemodynamic Atherosclerotic Syndrome): Role of arterial stiffness and blood pressure variability in elderly hypertensive subjects. Int. J. Cardiol. 263, 132–137 (2018).
Scuteri, A. et al. Routine assessment of cognitive function in older patients with hypertension seen by primary care physicians: Why and how-a decision-making support from the working group on “hypertension and the brain” of the European Society of Hypertension and from the European Geriatric Medicine Society. J Hypertens 39, 90–100 (2021).
Mattace-Raso, F. U. S. et al. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘Establishing normal and reference values’. Eur. Heart J. 31, 2338–2350 (2010).
Lakatta, E. G. et al. Impact of Stiffer Arteries on the Response to Antihypertensive Treatment: A Longitudinal Study of the SardiNIA Cohort. J. Am. Med Dir Assoc 21, 720–725 (2020).
Sharman, J. E. et al. Lancet Commission on Hypertension group position statement on the global improvement of accuracy standards for devices that measure blood pressure. J. Hypertens. 38, 21–29 (2020).
Pauca, A. L., Wallenhaupt, S. L., Kon, N. D. & Tucker, W. Y. Does radial artery pressure accurately reflect aortic pressure?. Chest 102, 1193–1198 (1992).
Herbert, A., Cruickshank, J. K., Laurent, S. & Boutouyrie, P. Reference Values for Arterial Measurements Collaboration: Establishing reference values for central blood pressure and its amplification in a general healthy population and according to cardiovascular risk factors. Eur. Heart J. 35, 3122–3133 (2014).
Kollias, A., Lagou, S., Zeniodi, M. E., Boubouchairopoulou, N. & Stergiou, G. S. Association of central versus brachial blood pressure with target-organ damage: Systematic review and meta-analysis. Hypertension 67, 183–190 (2016).
Roman, M. J. et al. Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: The Strong Heart Study. Hypertension 50, 197–203 (2007).
Pini, R. et al. Central but not brachial blood pressure predicts cardiovascular events in an unselected geriatric population: the ICARe Dicomano Study. J. Am. Coll. Cardiol. 51, 2432–2439 (2008).
Wang, K. L. et al. Central or peripheral systolic or pulse pressure: Which best relates to target organs and future mortality?. J Hypertens. 27, 461–467 (2009).
Williams, B., et al.; CAFE Investigators; Anglo-Scandinavian Cardiac Outcomes Trial Investigators; CAFE Steering Committee and Writing Committee. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: Principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 113, 1213–1225 (2006).
Boutouyrie, P., Achouba, A., Trunet, P., Laurent, S., & EXPLOR Trialist Group. Amlodipine-valsartan combination decreases central systolic blood pressure more effectively than the amlodipine-atenolol combination: The EXPLOR study. Hypertension. 55, 1314–1322 (2010)
Scuteri, A. et al. Arterial stiffness and influences of the metabolic syndrome: A cross-countries study. Atherosclerosis 233, 654–660 (2014).
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA: J. Am. Med. Assoc. 285, 2486–2497 (2001).
O’Brien, E. et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J. Hypertens. 21(5), 821–848 (2003).
Kang, J. H. et al. A comparison between central blood pressure values obtained by the Gaon system and the SphygmoCor system. Hypertens Res 35, 329–333 (2012).
Prado, C. M. & Rossi, M. A. Circumferential wall tension due to hypertension plays a pivotal role in aorta remodeling. Int. J. Exp. Pathol. 87, 425–436 (2006).
Carallo, C. et al. Evaluation of common carotid hemodynamic forces: Relations with wall thickening. Hypertension 34, 217–221 (1999).
Scuteri, A. et al. The relationship between the metabolic syndrome and arterial wall thickness: A mosaic still to be interpreted. Atherosclerosis 255, 11–16 (2016).
Hayashi, T. et al. Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann. Intern Med. 140, 1 (2004).
von Frankenberg, A. D. et al. Major components of metabolic syndrome and adiponectin levels: A cross-sectional study. Diabetol. Metab. Syndr. 6, 1 (2014).
Scuteri, A. et al. Independent and additive effects of cytokine patterns and the metabolic syndrome on arterial aging in the SardiNIA Study. Atherosclerosis 215(2), 459–464 (2011).
Chen, M. C. et al. Low serum adiponectin level is associated with metabolic syndrome and is an independent marker of peripheral arterial stiffness in hypertensive patients. Diabetol. Metab. Syndr. 9, 49 (2017).
Feraco, A. et al. Mineralocorticoid receptors in metabolic syndrome: From physiology to disease. Trends Endocrinol. Metab. 31(3), 205–217 (2020).
Hayward, C. S. & Kelly, R. P. Gender-related differences in the central arterial pressure waveform. J. Am. Coll. Cardiol. 30, 1863–1871 (1997).
Chester, R. et al. Women have significantly greater difference between central and peripheral arterial pressure compared with men: The Bogalusa Heart Study. J. Am. Soc. Hypertens. 7, 379–385 (2013).
Scuteri, A. et al. Associations of large artery structure and function with adiposity: Effects of age, gender, and hypertension. The SardiNIA Study. Atherosclerosis 221(1), 189–197 (2012).
Fox, C. S. et al. Genome-wide association for abdominal subcutaneous and visceral adipose reveals a novel locus for visceral fat in women. PLoS Genet 8(5), e1002695 (2012).
Acknowledgements
We thank all the participants in the cohorts for contributing data to the MARE consortium and the funding agencies supporting these cohorts.
Funding
Open access funding provided by Lund University. The Asklepios Study is supported by the Fund for Scientific Research—Flanders (FWO research grants G042703 and G083810N). The Rotterdam Study is supported by the Erasmus Medical Center and Erasmus University Rotterdam; the Netherlands Organization for Scientific Research; the Netherlands Organization for Health Research and Development (ZonMw); the Research Institute for Diseases in the Elderly (RIDE); the Netherlands Heart Foundation; the Ministry of Education, Culture and Science; the Ministry of Health Welfare and Sports; the European Commission; and the Municipality of Rotterdam. The SardiNIA team was supported by Contract NO1-AG-1-2109 from the NIA. This research was partly supported by the Intramural Research Program of the NIH, National Institute on Aging (USA). The LitHiR program was reimbursed from the Statutory Health Insurance Fund (Lithuania). The Malmö Diet and Cancer Study (MDCS) has been supported by a Lund University Infrastructure grant “Malmö population-based cohorts” (STYR 2019/2046). The SMART study was funded initially by Takeda. The Vobarno Study is supported by grants from the European Community Network of Excellence (InGenious HyperCare, 2006 to 2010); Italian University and Research Ministry, Regione Lombardia, and Fondazione della Comunità Bresciana Onlus.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design. A.L.-C. and A.S. analyzed the data. A.L.-C. and A.S. drafted the manuscript. All authors critically revised the manuscript and read and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laucyte-Cibulskiene, A., Chen, CH., Cockroft, J. et al. Clusters of risk factors in metabolic syndrome and their influence on central blood pressure in a global study. Sci Rep 12, 14409 (2022). https://doi.org/10.1038/s41598-022-18094-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18094-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.