Abstract
Magnetic resonance imaging (MRI) is a powerful and versatile technique that offers a range of physiological, diagnostic, structural, and functional measurements. One of the most widely used basic contrasts in MRI diagnostics is transverse relaxation time (T2)-weighted imaging, but it provides only qualitative information. Realizing quantitative high-resolution T2 mapping is imperative for the development of personalized medicine, as it can enable the characterization of diseases progression. While ultra-high-field (≥ 7 T) MRI offers the means to gain new insights by increasing the spatial resolution, implementing fast quantitative T2 mapping cannot be achieved without overcoming the increased power deposition and radio frequency (RF) field inhomogeneity at ultra-high-fields. A recent study has demonstrated a new phase-based T2 mapping approach based on fast steady-state acquisitions. We extend this new approach to ultra-high field MRI, achieving quantitative high-resolution 3D T2 mapping at 7 T while addressing RF field inhomogeneity and utilizing low flip angle pulses; overcoming two main ultra-high field challenges. The method is based on controlling the coherent transverse magnetization in a steady-state gradient echo acquisition; achieved by utilizing low flip angles, a specific phase increment for the RF pulses, and short repetition times. This approach simultaneously extracts both T2 and RF field maps from the phase of the signal. Prior to in vivo experiments, the method was assessed using a 3D head-shaped phantom that was designed to model the RF field distribution in the brain. Our approach delivers fast 3D whole brain images with submillimeter resolution without requiring special hardware, such as multi-channel transmit coil, thus promoting high usability of the ultra-high field MRI in clinical practice.
Similar content being viewed by others
Introduction
Non-invasive biomedical imaging provides high-impact medical diagnostics and offers an ideal means of promoting preventative medicine. This is indeed the case when it comes to ultra-high field (≥ 7 T) Magnetic Resonance Imaging (MRI)1,2,3. One high-value diagnostic MRI method is based on estimating the T2 relaxation time of tissues—either T2-weighted4 imaging or quantitative-T2 mapping5,6,7. T2-weighted MRI of the brain is one of the most widely employed routine diagnostic methods in cancer and neurodegenerative diseases. It is essential for the detection of hyperintense lesions pronounced in demyelinating diseases, such as multiple sclerosis8,9,10, and in the monitoring of disease progression9. In multiple sclerosis, improved precision at early stages of lesion formation would allow their clear categorization and aid in developing new tools to delay or eliminate the relapse. Recent studies at 7 T MRI have shown that we can detect smaller lesions than previously possible and so better monitor disease progression8. However, the robust characterization of disease progression with MRI requires quantitative T2 mapping, the use of which in clinics is impeded by its long scan duration. Novel fast methods11,12,13 encounter extra challenges in ultra-high field MRI among which are the severe RF field inhomogeneity14, which reduces the accuracy of the quantification, and the increased power deposition that results in prolonged scan duration. Common T2 methods are especially prone to the above drawbacks since they are spin-echo-based, requiring refocusing pulses that are high in Specific Absorption Rate (SAR)15 and whose effectiveness is sensitive to RF field inhomogeneity.
Recent studies have proposed another solution—called Magnetic Resonance Fingerprinting (MRF)16,17. This method allows parametric MR mapping (including T1 and T2 maps), thus eliminating the dependence on the specific scan parameter or scanner. However, MRF is not easily translated into ultra-high field MRI, since overcoming the RF field inhomogeneity further complicates the acquired dataset17. Designs based on the steady-state gradient echo (GRE) pulse sequences offer a plethora of pathways toward multi-contrast fast acquisitions, among which are simultaneous multi-parametric acquisitions18,19 as well as a design for T1 and T2 weighted images in highly inhomogeneous static magnetic fields20. These include DESPOT221 and phase-cycled balanced steady-state free precession22,23,24 (bSSFP). A method called TESS19,25 shows promising results for T2 mapping without RF field dependence, however, currently it was demonstrated only as a 2D implementation for brain imaging26. Finally, a method analyzing the complex signal of a set of unbalanced GRE scans at 7 T gave T1 and T2 maps18, but included a long total scan duration (16:36 min) and used parallel transmission to mitigate the transmit field inhomogeneity.
Recently, a new method was introduced based on a steady-state spoiled gradient-echo (SGRE) acquisition that utilizes low flip angles and short repetition times (TRs) to obtain T2 maps at 3 T MRI27, assuming a uniform and a priori known flip angle. While most of the GRE-based studies have focused on magnitude images20,21,28, in this study, phase information was highlighted, which offers a new and attractive method for T2 mapping. Building on this work we elucidate the dependence of the phase-based method on the (unknown) excitation flip angle in addition to the RF pulse phase, with an eye to design an approach suited for T2 mapping of the brain at 7 T. This new extension to the steady state method includes both T2 and RF field estimation and is designed to cover the relevant flip angle range arising in the brain due to the RF field inhomogeneity at 7 T MRI (see Fig. 1). The advantage of this approach is its ability to simplify the signal dependencies and reduce the confounding variables. This includes the removal of the static magnetic field (B0) dependence and a reduced dependence on the longitudinal relaxation time (T1).
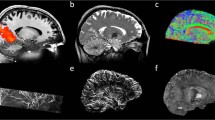
Schematics of the steady state method for T2 and RF field estimation—its design and verification. Starting from simulations, through assessment of the estimation algorithm, via a 3D head-shaped brain-like phantom, to human imaging. Left—a design of a steady-state configuration based on Bloch simulations that provides θ(T2,α) for specific φinc, which was thereafter utilized to generate T2 and α in the 2D space (θ1, θ2). The new space allows to extract T2 and α from θ1 and θ2. Center—the estimation algorithm was assessed via simulations and brain-like phantom measurements. In these measurements, a realistic signal \(S\) was acquired, providing |S| and \(\angle S\), from which the T2 and α (or B1 distribution) were estimated. Right—human imaging at 7 T MRI provided high-resolution whole-brain T2 maps, while coping with the B1 distribution.
Building on the phase-based approach by Wang27,29, which departs from the traditional concepts based on spin-echo, our extension introduces a new T2 mapping solution for ultra-high field MRI. This method can deliver quantitative T2 mapping at 7 T MRI without requiring any additional hardware—such as dielectric pads or multi-channel transmit coil—to reduce the RF field inhomogeneity. Another advantage of this method is that it enables whole-brain imaging with high acceleration factors, as it relies on a 3D k-space acquisition.
Our study comprised three main steps (Fig. 1). First, we conducted Bloch simulations of the generated steady state signal for different scan parameters (such as RF flip angle, RF phase, and TR). Then, we looked for parameter combinations that support the range of flip angles, due to the RF field inhomogeneity, in 7 T brain imaging. Next, we developed and assessed an efficient estimation algorithm. Lastly, we performed human brain imaging on a 7 T MRI scanner. The estimation algorithm was assessed on synthetic signals from the Bloch simulations, as well as on actual measurements, in a realistic setting, via a 3D head-shaped phantom, which was designed to model the RF field distribution in the brain30. For both the head-shaped phantom and the human brain imaging the phase-based method was compared with the gold-standard single-echo spin echo (SE–SE). Furthermore, we used the phase-based method to acquire whole-brain T2 maps with sub-millimeter resolution.
Principles of the modified-SGRE sequence for simultaneous T2 and RF field mapping
The foundation for using phase increments during the RF pulse train was provided by Zur et al. in 198831,32. They showed that an RF pulse train with a quadratic phase φRF(n) = φinc∙(n2 + n)/2 for the n-th pulse—using an appropriate φinc value in conjunction with a spoiling gradient—can achieve incoherent transverse magnetization, an effective spoiling better than simple gradient spoiling (φinc = 0 case). This is commonly called RF spoiling. Recent work by Wang27 at 3 T provided another keystone, in which the authors showed that small φinc values have the opposite effect; they introduce coherent transverse magnetization, where the phase of the signal possess a strong dependence on T2 (Fig. 2a). Figure 2a also shows the dependence of the phase of the signal on the excitation flip angle α. The α dependence curves have an extremum in the vicinity of 15°, i.e., the actual flip angle in that vicinity has a small effect on the phase. As the flip angle in the 3 T implementation was assumed to be given by the scan (due to relatively homogeneous RF field distribution), T2 values could be extracted solely from the phase of the signal.
The phase of the steady-state signal as a function of T2 and the flip angle. (a) θ(T2, α, T1) dependence (Bloch simulation results) for a representative small φinc (φinc = 2°). The dependence on T2, α, and T1 is shown in 1D plots and in 2D. (b) T2 and α distributions in the new (θ1, θ2) 2D space. Two examples are shown: Top—(φinc1 = 2°, αscan1) with (φinc2 = 2°, αscan2 = 2αscan1). Bottom—(φinc1 = 3°, αscan1) with (φinc2 = 1.5°, αscan2 = 2αscan1). In each case, α (θ1, θ2) and T2 (θ1, θ2) are shown with the equi-T2 and equi-α lines.
In our study, however, the combined (T2, α) dependence of the signal’s phase θ was exploited to cope with the RF field inhomogeneity at ultra-high field MRI. Neglecting, for now, the small T1 dependence of the phase—for T1 values relevant to brain tissues at 7 T, see Fig. 2a—the phase θ of the signal depends on the T2 at the voxel and on the actual flip angle α there. This α is the target flip angle of the scan αscan scaled by the RF field ratio at each voxel: α = αscan∙RFratio, where RFratio is the normalized RF field distribution. As the phase θ(T2, α) (see Fig. 2a) is not a one-to-one map of (T2, α) to θ, at least two measurements, θ1 and θ2, are needed; thus defining a 2D space (θ1, θ2). To extract T2 and α from θ(T2,α), we need a convenient 2D space to represent T2 and α in each voxel. Based on the Bloch simulations, such a 2D space can be generated by two scans with two flip angles, αscan1 and αscan2 = RFA∙αscan1 (RFA is a user set multiplication factor; for example, RFA = 2). Furthermore, we found that varying φinc between the two scans—one scan with (φinc1, αscan1) and a second with (φinc2, αscan2 = RFA∙ αscan1)—provides greater flexibility in controlling the 2D (θ1, θ2) space and its mapping to (T2, α). Figure 2b shows that different combinations of phase increment and flip angle pairs can be useful to adjust the range of viable flip angles and the T2 of interest.
The two phase measurements, θ1 for scan parameters (φinc1, αscan1) and θ2 for scan parameters (φinc2, αscan2), are functions of φinc1, φinc2, T2 and the (actual) flip angles, i.e., θ1 = θ(φinc1, α1, T2) and θ2 = θ(φinc2, α2, T2), where α1 and α2 are the actual flip angles. Although α1 and α2 are unknown, their ratio must obey α2/α1 = αscan2/αscan1 \(\equiv\) RFA. Thus, renaming α1 as α, we have θ1 = θ(φinc1, α, T2) and θ2 = θ(φinc2, RFA∙α, T2), or in a shorthand notation θ1 = θ1(α, T2) and θ2 = θ2(α, T2), where the functions θ1() and θ2() contain the known φinc1, φinc2, and RFA parameters. One can now map T2 and α to the new (θ1, θ2) 2D space, written as T2(θ1, θ2) and α(θ1, θ2). Figure 2b shows that equi-T2 and equi-α lines are nearly orthogonal, when we are well inside the “balloon” (the support region), which is an indication of the robust estimation for a given set of (θ1,θ2) there. At the “balloon” edges of low or high α values the solution is ill-posed and can provide more than one solution, thus increasing the variability and bias of the estimation at that region. Having now the simulated (θ1, θ2) 2D space for T2 and for α, one can point with any measured (θ1meas.,θ2meas.) to that space and provide the expected T2 and α values by a simple interpolation. This representation is useful to explore and characterize optimal choices of flip angles and φinc to achieve minimal variability and bias. Figure 2b shows that the set (φinc1 = 3°, αscan1) and (φinc2 = 1.5°, αscan2 = 2αscan1) covers a larger flip-angle range than set (φinc1 = 2°, αscan1) and (φinc2 = 2°, αscan2 = 2αscan1). We performed a detailed analysis to determine the optimal regime for whole-brain imaging, the results of which are summarized in Fig. S1–S4.
Variability and bias evaluation + SAR considerations
We examined the variability and bias of the method in the range of flip angles relevant for brain imaging. To do so, noise was added to the simulated signal and the variability and bias of the method were examined as a function of T2 and α. The noise in the simulations was calibrated so the resulting synthetic signal to noise ratio (SNR) matched the measured SNR in agar tubes for the same α and T2, where the agar T2 was in a range matching white matter (WM) and gray matter (GM) at 7T18. The signal dependence on flip angle and phase increment showed that the phase of the signal is high for low φinc (φinc < 10°) (Fig. S1). It can be seen that the combination (φinc1 = 3°, αscan1) and (φinc2 = 1.5°, αscan2 = 2αscan1) provides a lower variability (i.e., lower std(T2est.)) and a smaller bias (i.e., lower |ave(T2est.) − T2true|) for a larger range of flip angles (Fig. S2). We also examined three criteria (Fig. S3): the average estimation variability for 30 < T2 < 50 ms and 5° < α < 17°, and both the minimal and maximal flip angles that provide std(T2est.) < 5 ms. The result of a combined minimization of the three criteria (shown in Fig. S3d) is a pair of scans with (φinc1 = 3°, αscan1) and (φinc2 = 1.5°, αscan2 = 2αscan1) that provides a good combination of the lowest average std(T2est.) and supports a flip angle range of 3.7–35° (in which std(T2est.) < 5 ms).
Figure S4 shows three additional aspects that were included to establish the final configuration, including the repetition time (TR), the RFA in a realistic experiment and reduction of the cerebrospinal fluid (CSF) signal. Although the combination (φinc1 = 3°, αscan1) and (φinc2 = 1°, αscan2 = 2αscan1) provides a better flip angle range (2.4–35°), in practice, φinc1 = 1° generates a high CSF signal. This can result in an extra signal and a residual artifact in the proximity of the ventricles. To reduce the CSF signal’s effect, it was found worthwhile to use φinc2 = 1.5° (Fig. S4a). As the change in relative variability as a function of TR (Fig. S4b) is insignificant, the choice of TR can be made by balancing between SAR limitations, on the one hand, and scan duration, on the other hand. A TR of 10 ms provided a practical tradeoff. Our examination of the effect of the RFA on the flip angle range showed that the higher the RFA, the better (Fig. S4c). However, to keep SAR within the “Normal” level, it was found that RFA in the range of 1.6–2 (with TR = 10 ms) provides a suitable flip angle range. In case of adopting “First level” SAR limit, one can increase the range of the flip angles.
Global phase corrections
In practice, the phase (\(\angle S\)) of the signal S at a voxel is comprised of the steady-state phase θ(α, T2, T1) plus a global phase θ0. The global phase θ0 arises from several factors, with a dominant contribution from B0. It can be eliminated by repeating the scan twice, once with + φinc and once with -φinc, and setting θ(α, T2, T1) = \(\angle \left({S}_{{+\varphi }_{inc}}\cdot conj\left({S}_{{-\varphi }_{inc}}\right)\right)/2\) (as was shown in Ref.27). The implemented acquisition thus includes four scans: the two scans (φinc1, αscan1) and (φinc2, αscan2) and their repetition with a negative phase increment to remove θ0. Calculating the θ1 and θ2 in this method does not result in phase wrapping, since after the global phase removal, the signals’ phase is in the range of 0° to ~ 50°.
Estimation algorithm
The actual estimation algorithm included two main steps, per voxel, namely the removal of the global phase (θ0) and an estimation of T2 and α from (θ1,θ2) using linear interpolation. An additional step was established for low flip angles because low flip angles result in (θ1,θ2) measurement pairs close to the edges of the “balloon” (Fig. 2b), a region where interpolation is an ill-posed problem. Low flip angles are relevant for whole-brain imaging because despite the flip angle of the first scan being set to αscan1 = 15° , the actual whole-brain RF field distribution results in a flip angle in the range of ~ 4° to 22° (even reaching below 4° for some regions, see a representing distribution in Fig. 1). Brain regions where very low flip angles (~ 4–6°) are typically reached are the cerebellum, midbrain, and brainstem, as well as some regions in the temporal lobe. The added step to handle low flip angles takes advantage of two aspects: i) that α changes slowly in space, and ii) that for small flip angles (α < 20°) the phase \(\theta\) is linear with T2, and that the slope itself is linear with the flip angle α. Detailed description of this step are in the “Materials and methods” section. Figure S5 shows the improvement attained using the second step for the low flip angles. Additional steps were also performed to improve the estimation for the expected low values of (θ1,θ2), which, due to noise, results in negative values (see “Materials and methods”).
T1 corrections
As mentioned, phase dependence on T1 is small, but it can account for ~ 15% of the final T2 estimation. To reduce the error due to T1 in human imaging voxels were classified as either “high” or “low” T1 by empirically thresholding \(\left|{S}_{{\alpha }_{\text{scan2}}}\right|/\left|{S}_{{\alpha }_{\text{scan1}}}\right|\). Separate maps—T2(θ1, θ2) and α(θ1, θ2)—were used for each classification, based on T1 = 1 s (representing WM) and T1 = 2 s (the rest). With this correction, the error was further reduced (shown in Fig. S6). A detailed description of the algorithm is provided in the “Materials and methods” section.
Results
To examine the estimation bias and estimation variability we conducted two imaging experiments with phantoms, one with tubes filled with agarose suspension, the other with a 3D head-shaped phantom. In the first experiment (Fig. 3a), the variability was × 1.4 smaller than with SE–SE (0.5 ms compared to 0.7 ms). The aslope and the relative deviation error (see Eq. 1) calculated between the T2 from this method and the T2 from SE–SE were 1.01 and 0.5%. Thus, the phase-based method provides a small bias and a lower variability compared to SE–SE, while the scan duration is × 2.3 faster.
Assessment of estimation bias and variability in phantoms. (a) Comparison of the T2 obtained with the phase-based method and SE–SE in agar tubes. Top—a central slice of the T2 maps and magnitude images. Bottom—estimated T2 for each tube as a function of T2 with SE–SE; aslope = 1.01, relative deviation error = 0.5%. The average standard deviation was 0.5 ms for the phase-based method, and 0.7 ms for SE–SE. (b–d) Comparisons using a 3D-head-shaped brain-like phantom. (b) T2 and α maps estimated by the phase-based method. (c) T2 map estimated with SE–SE. And (d) α map estimated using the vendor’s RF field mapping scan. Two main cross-sections are shown for all cases, Sagittal and Axial. For comparison, the average T2 and standard deviation was calculated in the same region of interest (marked by a blue contour for the phase-based method and a red contour for SE–SE). The average deviation between the α maps of the phase-based method and of the vendor’s RF mapping was calculated to be 0.56° for the Sagittal plane and 0.84° for the Axial plane.
In the second experiment, a specially designed 3D head-shaped brain-like phantom was used to examine the capability to cope with an RF field distribution similar to that in the brain. The “brain” had a uniform T2, which helped to separate the two parameters we sought to estimate, α and T2. Our results show low variability in T2 (std(T2 phase-based-method )/std(T2 SE–SE) = 0.46) and an RF field map estimation with little bias (a 4% average deviation from the map acquired with the vendor’s pulse sequence), see Fig. 3b. Even low flip angles, in the ill-posed area of the “balloon”, were well determined using the implemented estimation algorithm (Fig. S8).
The contribution of the B1 correction to the T2 estimate can be seen in Fig. 4. It compares T2 maps extracted from a set of four scans (two pairs) to T2 maps extracted from a single pair—as in Ref.27—using either of the pairs (either pair 1: φinc1 = 3° and φinc1 = − 3°, with αscan1; or pair 2: φinc2 = 1.5° and φinc2 = − 1.5°, with αscan2). It can be seen that for both phase increments the RF field inhomogeneity results in either underestimated or overestimated T2 values, depending on the actual flip angle in each voxel (see Fig. 2a for phase dependence on flip angle). The 4-scans result, which combines both phase increments, provides a uniform T2 map of the “brain” tissue in the 3D-head shaped phantom, as expected by the design.
Comparison of T2 maps extracted with (a) 4-scans, (b) single pair with (φinc1, αscan1) and (c) single pair with (φinc2, αscan2). (d) For each case a plot for a line shown in the Sagittal and Axial scans. The images show 3D-head shaped phantom (left) and human imaging (right). The human axial plane image in (a) shows the regions that were examined and summarized in Table 1.
Figure 4 also shows the estimated T2 maps, for human imaging, based on either 4-scans or a single scan-pair. Although more challenging to observe, due to the heterogeneous T2 distribution in the brain and to the very high T2 values in the CSF regions, it can also be seen that T2, estimated from a single pair, is either underestimated or overestimated compared to 4-scans. This can be observed, for example, in regions such as the cerebellum and the temporal lobes. Table 1 summarizes the results by giving sample T2 values in white matter, grey matter and CSF. For each tissue 2 sampled regions were chosen as shown in Fig. 4—WM1 and WM2 in white matter tissue, GM1 and GM2 in the grey matter tissue and CSF1, CSF2 in the CSF. The table also shows T2 values reported in Ref. 18. Note: the CSF values are underestimated with the current method, as further elaborated in the Discussion section.
Continuing with human imaging, Fig. 5 compares the phase-based method with 1.5 mm isotropic voxels to the gold standard SE–SE, for a T2 mapping comparison, and to the vendor RF mapping, for an RF field mapping comparison. The α map in Fig. 5c was smoothed by 3 × 3 filter to reduce the effect of local CSF signals (see Fig. S13 for original high resolution B1 map). The RF field map extracted with the phase-based approach shows a distribution similar to the separately acquired vendor map with, however, noticeable deviations in the ventricles, as well as in some of the CSF region. The ratio of the T2 values and the relative deviation error between the phase-based method and SE–SE is shown in Fig. 6, for the different volunteers. Over all volunteers the T2 ratio (T2 phase-based-method/T2 SE–SE) and relative deviation error are 0.80 and 15.45% for WM, and 0.85 and 19.76% for GM (detailed description is in Supplementary Information S4).
Human imaging—T2 from the phase-based method or SE–SE, and α from the phase-based method or the vendor’s scan. (a) SE–SE Sagittal magnitude image at TE = 30 ms and the estimated T2 maps in three main cross-sections. (b) An α map using the vendor’s pulse sequence. (c) Sagittal magnitude image with φinc = 3 and α = 15°, as well as the estimated T2 and α maps in three main cross-sections. α map shown here was smoothed by a 3 × 3 filter to reduce the effect of local CSF signal. Orange arrows point to the cerebellum and brainstem regions suffering from low flip angles due to B1 inhomogeneity; their inner structure is much more pronounced—and clearly visible—in the phase-based T2 images. Purple arrows point to a region in the CSF that resulted in a low magnitude signal.
Comparison of T2 estimation between the phase-based method and SE–SE. The plot shows the ratio T2 phase-based-method/T2 SE–SE per volunteer, both for WM and for GM. The error bars depict the relative deviation error [see Eq. (1)].
Finally, high-resolution whole-brain T2 mapping was performed with the phase-based method, with 1 mm and 0.85 mm isotropic voxels. To acquire whole-brain high-resolution images, × 5.11 acceleration was used—combining elliptic sampling and × 2 acceleration in both phase encoding directions. Each of the four scans with 1 mm resolution was 1:13 min giving a total scan time of 4:52 min. For 0.85 mm each scan was 1:42 min long and the total scan time was 6:48 min. Figure 7 shows the estimated T2 maps for the 0.85 mm scan (Fig. S12 shows the 1 mm resolution images). To provide even higher robustness following the reduced SNR of the high-resolution datasets, we also incorporated denoising based on a DnCNN deep-learning network33 (provided in MATLAB, The Mathworks, Natick MA, for Gaussian noise removal). This entailed denoising of θ1 and θ2 before the estimation of T2. The denoising greatly improved the observed details of the cerebellum structure, a region with especially low flip angles (Fig. 7b).
Human whole-brain T2 maps with a 0.85 mm isotropic voxel. (a) without denoising, (b) with denoising, based on DnCNN model for Gaussian noise removal. Arrows point to the cerebellum region, which especially benefits from denoising. Top row, Sagittal and Coronal planes. Bottom two rows, six slices of the Axial plane, at 10 mm intervals.
Discussion
The expected rewards of pushing the limits and moving to 7 T MRI are increased spatial resolution and shorter scan durations. Both these features are essential for clinical and research imaging, all the more so for quantitative methods. However, scanning at 7 T also poses new challenges, including high power deposition and severe RF field inhomogeneity. The extended phase-based method shown here delivers high-resolution brain T2 imaging while overcoming the above challenges. This is achieved by relying on a modified 3D SGRE sequence, using the phase of the signal to encode the T2 dependence. The 3D SGRE images are also highly robust to B0 inhomogeneity. This can be seen in the magnitude images of both the phantom example (Fig. 3a) and the human images (Fig. 5). The SE–SE is more distorted both at the edges of the agar tubes and near the nasal areas in the human images. The B0-dependent phase is reliably canceled out by the two scans with opposite phase increments (φinc) of the RF pulse train. However, shifts in the global phase between scans may occur, which will require corrections. Similarly, the scans may be sensitive to movements, which will affect the phase. Incorporating a second echo acquisition could be used to correct for both the phase shifts and motion34. Aiming to shorten the total scan duration, one can also consider estimation of the global phase from a single pair, thus reducing the number of scans to three. However, in this case careful analysis and phase unwrapping will be required in the third, non-paired, scan. In this case, phase unwrapping can be especially challenging in regions with short T2*, where B0 changes rapidly, resulting in high local changes in the background phase. Very short T2* may also affect T2 estimation due to limited SNR in such regions.
The current implementation used a non-selective hard pulse for the 3D acquisition. Although this works well for whole brain acquisition as in this study, in other cases it can be a limitation. For faster acquisition and to limit potential aliasing, the use of slab-selective pulses is beneficial. Figure S9 shows that as long as the slab is thick enough, compared to the slice thickness, the estimated T2 is correctly estimated. However, for a single slice-selective acquisition, the simulation by which the T2 and RF field maps are estimated must also account for the slice profile. This was already demonstrated in other T2 mapping methods such as balanced SSFP19.
Another sensitivity of the method that requires discussion is the sensitivity to movement and potential inaccuracy in the RF pulse phase. Although we did not observe noticeable movement in our human scanning, a simulation to examine these vulnerabilities was performed (see Supplementary Information, Section S5). The movement was simulated assuming a constant velocity during the scan, which will result in an additional parabolic phase term accumulated during the scan. Examining the error due to potential head movement of 1–2 voxels during the scan, it resulted in a small error, less than 1% for a movement of up to 5 mm/min. However, for large movement within a voxel, such as due to flow, the error of the estimated T2 can be significant; reaching 20%, for a velocity of 0.5 mm/s.
Two simulations were also performed to analyze possible hardware inaccuracies: (i) a constant error in the actual RF-phase increment, (ii) a randomly distributed error in the actual phase of the RF pulse. In the first case, a constant error of 0.1° resulted in < 4% error, In the second, a randomly distributed error with σ = 0.2° resulted in a negligible error with standard deviation of 0.07 ms in the estimated T2. It is also important to note that the estimation of the T2 in the CSF and other tissues with high T2 values (> 0.5 s) is challenging with this method, since the signal’s phase curve slowly converges for T2 > 100 ms (see Fig. 2a) and so the T2 contours in the (θ1,θ2) space grow denser with T2 (see Fig. 2b). In addition, local intensity drops in CSF voxels, resulting in low SNR voxels, can occur due to fluid movement (purple arrows in Fig. 5 point to such area), thus further limiting T2 estimation of CSF.
The important advantage of the phase-based approach for T2 mapping is its whole-brain coverage ability. The method shows robust results in the brainstem region and even in parts of the spinal cord (see Fig. 5). These results are achieved without the need for additional hardware to reduce the RF field inhomogeneity, such as dielectric pads or multi-channel transmit coil. Naturally, the method can also benefit from a dielectric pad or multi-channel transmit coils to improve the SNR, especially in regions with low flip angles. The current configuration (φinc1, φinc2, αscan1, RFA, and TR) was designed for the RF field distribution in the brain, and was shown to robustly extract the RF field distribution in the 3D head-shaped phantom (which has a slightly larger RF field inhomogeneity than in vivo). If another region will be of interest, the configuration—the RF pulse phase increments and the scan flip angles—can be adapted accordingly.
It is worth noting that θ1 on its own, calculated from the first pair of scans (with φinc1 = ± 3°), achieves a “T2 weighted” image (see Fig. S10 for the 0.85 mm case), unlike the magnitude of these scans. θ1, however, suffers from pronounced RF field inhomogeneity, which is removed by using two sets of scans (giving θ1 and θ2), as was implemented here, allowing the generation of T2 maps.
In our study, the estimation algorithm is based on an interpolation procedure, where the simulated data serves as the ground-truth. This method is similar to the dictionary-based approach in MRF, but is based on two measurement points (θ1, θ2) that allow us to represent the parameters of interest, T2 and α, in the (θ1, θ2) 2D space. This offers the advantage of mapping the T2 of interest by a simple linear interpolation. An improvement in the estimation algorithm was implemented in the low flip angles’ range, which extended the viable flip angles (Figs. S5 and S8). In this study, we demonstrated the low variability and small bias of the estimations in both simulations and phantom experiments. In the phantom experiment with agar tubes, the method provides T2 estimation with low variability—a × 3.2 (1.4 × 2.3) lower variability-to-scan-time factor than that of SE–SE. The T2 values were estimated by the phase-based method with a small bias (aslope = 1.01 and relative deviation error of 0.5% compared to SE–SE).
However, the in-vivo T2 ratio of the phase-based method to SE–SE was 0.79 ± 0.16 for WM and 0.86 ± 0.19 for GM. Similarly, there is a ratio of × 0.82 and × 0.88 between the reported values with 4-scans in Table 1 to the values in Ref.18. This result is also similar to the results in Ref.22,34. Possible reasons for the different ratios found for WM and GM are a partial volume of GM and CSF as well as deviations due to T1. Although T1 has a small impact on the phase of the signal and its effect was reduced in our implementation. The ~ 0.8 ratio between the T2 estimated by the phase-based approach and by SE–SE could arise for several reasons, among which are a contribution due to exchange and magnetization transfer35, diffusion36, and different contributions of the fast and slow T2 components to the two methods37,38. For the magnetization transfer no discrepancy was observed between the estimated T2 values in the agarose tubes, although exchange mechanisms are known to be at work in agarose and therefore produce magnetization transfer effects. However, different effects of exchange in the living tissue can still be a factor contributing to the acquired complex signal of the steady state acquisition. We also examined potential diffusion contributions to the estimated T2 by scanning a sample of smoked fish (which had and ADC of ~ 0.6 × 10−3 mm2/s, similar to white matter) and did not observe a significant effect (not shown). One of the potential factors is the larger contribution of the fast-relaxing species compared to SE–SE, primarily due to much shorter echo times, which was also observed in several previous studies38. Thus, although the estimated T2 was robustly repeated in the volunteers’ data, the resulting ratio between the phase-based method and SE–SE in-vivo still requires further analysis.
The fast high-resolution T2 maps of the whole brain that were acquired—1 mm isotropic in 4:52 min and 0.85 mm isotropic in 6:49 min—offer a significant clinical gain. Further acceleration of the method should be possible. One option is to reduce the TR, however, this will require switching the SAR monitoring to the less restrictive “First” level. For this, the effect of the TR on the variability of the estimation was examined (see Fig. S4) and showed that shorter TR result in similar estimation variability. In addition, acceleration methods, tuned to the 3D SGRE acquisition and employing the Compressed Sensing technique, can achieve even higher acceleration factors. We also demonstrated the option of employing denoising based on deep-learning techniques that is trained to remove Gaussian noise. This further improves the quality of the images and can be used to further accelerate the scan.
Overall, the extension of the phase-based steady-state method to estimate both T2 and RF field map, demonstrated in this work, provides a fast and high-resolution acquisition method for quantitative T2 mapping of the whole brain at 7 T acquired with a single-channel transmit coil. Standardized high-resolution methods are imperative for 7 T MRI to advance multi-site studies and promote personalized medicine.
Materials and methods
Bloch simulations
1D single voxel simulations based on the Bloch equations were performed with a custom MATLAB (The Mathworks, Natick MA) code39 to examine the signal in steady state. The simulations included an excitation pulse, an acquisition and a net total spoiler (including the area of the acquisition) of 3/Δx (Δx the 1D voxel size). The number of initial repetitions to reach steady-state (“dummy scans”) was set to 500, which was verified to provide reliable steady states. Following the dummy scans, a single acquisition was simulated. The simulation was repeated over a grid of flip angles and T2 values, for different values of T1, φinc, and TR. The grid covered T2 from 0 to 200 ms with a resolution of 4 ms, and flip angles from 0° to 70° with a resolution of 1°. The resulting θ(T2, α) map was interpolated prior to its use in the estimation algorithm with 1 ms in T2 and 0.1° in alpha, generating θ1(T2, α) and θ2(T2, α) for relevant φinc and RFA factors.
Estimation algorithm
The estimation algorithm included the following steps:
Preparatory step #0.1: global phase removal
In practice, the phase (\(\angle S\)) of the signal S at a voxel is comprised of the steady-state phase θ(α, T2, T1) plus a global phase θ0. The global phase θ0 arises from several factors, with a dominant contribution from B0. It can be eliminated by repeating the scan twice, once with + φinc and once with -φinc, and setting θ(α,T2,T1)=\(\angle \left({S}_{{+\varphi }_{inc}}\cdot conj\left({S}_{{-\varphi }_{inc}}\right)\right)/2\) (as was shown in Ref.27). The implemented acquisition thus includes four scans: the two scans (φinc1, αscan1) and (φinc2, αscan2), and their repetition with a negative phase increment to remove θ0.
Preparatory step #0.2 (optional): denoising
For high-resolution human imaging, a denoising procedure based on a DnCNN deep-learning network33 (provided in MATLAB 2021a, for Gaussian noise removal) was incorporated. The denoising procedure was implemented on the measured θ1, θ2 with the command denoised_θ1 = denoiseImage(θ1, net), where the net was set by the command net = denoisingNetwork('dncnn').
Estimation step #1: T2 and α estimation by interpolation
First, using Matlab’s scatteredInterpolant(), we generated two interpolants, T2(θ1, θ2) and α(θ1, θ2), which map (θ1, θ2) to the desired quantities T2 and α. These interpolants were then used to estimate T2 and α from any (θ1, θ2) pair, at each voxel.
As mentioned, phase dependence on T1 is small, but it can account for ~ 15% of the final T2 estimation. Thus, in human imaging, to reduce the error due to T1, voxels were classified as either “high” or “low” T1 by empirically thresholding \(\left|{S}_{{\alpha }_{\text{scan2}}}\right|/\left|{S}_{{\alpha }_{\text{scan1}}}\right|\). Separate maps—T2(θ1, θ2) and α(θ1, θ2)—were used for each classification, based on T1 = 1 s (representing white matter—WM) and T1 = 2 s (the rest). With this correction, the error was further reduced (see simulation results in Fig. S6).
Estimation step #2: T2 estimation update for low flip angles
First, the flip angles α found in the previous step were smoothed, generating αsmoothed. For low flip angle voxels with αsmoothed < 4.5°, the flip angles were temporarily set to αtemp = 4.5°, and the matching temporary T2 quantities, T2-temp, were found by interpolation—using αtemp and θ2 (the phase from the scan using the higher flip angle, αscan2 = RFA∙αscan1). The final T2 was found through the linear connection T2 = (αtemp/αsmoothed)∙T2-temp.
Estimation step #3: handling of negative θ1 or θ2
For θ1 < 0 (and θ2 > 0), the θ2 from step #1 together with αsmoothed from step #2 were used to estimate T2; using the above simulated θ2(T2,α) for the known α. Similarly, for θ2 < 0 (and θ1 > 0), θ1 and αsmoothed were used to estimate T2.
Validation of the estimation algorithm was performed by generating N = 100 noisy repetitions of each point in the simulated datasets of θ1(T2,α) and θ2(T2,α). This was done using a fixed noise which resulted in the SNR varying with T2 and α, depending on the intensity at each point. The noise was fixed to produce an SNR of 180 for the simulated data at T2 = 38 ms and α = 13°; resembling the SNR in the human images acquired with 1.5 mm resolution. The SNR was set as an average SNR over the two signals |S1| and |S2|. To validate the simulations, the standard deviation of T2 was compared to a measured one in an agar-tubes experiment, both with the same SNR. For this validation two agar-tubes were used—with T2 values of T2 = 34 ms and T2 = 38 ms, representing WM and GM at 7 T. The flip angle distribution in this experiment was uniform (α = 13°). The measured and simulated SNR was 298, resulting in a T2 standard deviation of 0.36 ms in the measurement and 0.32 ms in the simulation, providing comparable results. The variability and bias of the method, under the simulated noise, were examined as a function of T2, α, φinc, TR and RFA.
Pulse sequence considerations
The sequence is based on a Siemens 3D GRE sequence that was modified to enable control over both the φinc and the gradient spoiler moment. The RF pulse we used was a hard pulse.
An important aspect to consider is the gradient spoiler moment intensity and its effect on the T2 estimation, as well as on image artifacts (in the form of residual signals from spurious echoes). A set of scans was performed to examine the spoiler effect. The gradient spoiler moment needs to provide complete dephasing inside a voxel, which defines a preferable gradient moment size to be \(\succsim\) 1/Δr (Δr = √(Δx2 + Δy2 + Δz2)). We found it useful to add a parameter to the pulse sequence that directly controls the net gradient spoiler moment (after all previous gradients had been rephased). The net spoiler was set to be equally distributed in all three directions, which was found useful in reducing artifacts. However, our experiments also showed that the gradient moment affected the measured phase, and thus the estimated T2. Figure S7a shows this dependence. Phantom experiments were used to calibrate the gradient spoiler moment to provide the T2 estimate closest to that from SE–SE. Accordingly, the gradient moment was set in all experiments to 0.015 [mT/m∙sec] in each direction. This moment is expected to provide dephasing for Δr \(\succsim\) 0.9 mm. As shown in Fig. S7b, under this moment, the estimated T2 did not change for the voxel sizes tested.
MRI scanning
All scans in this study were performed on a 7 T MRI system (MAGNETOM Terra, Siemens Healthcare, Erlangen) using a commercial 1Tx/32Rx head coil (Nova Medical, Wilmington, MA).
When comparing the results of the phase-based method to SE–SE, inside a region, the relative deviation error from the fit was calculated as
where aslope is the slope found for each fit, and N is the number of voxels in the comparison.
Phantom imaging
Five tubes with agar concentrations of 1.5, 2, 2.5, 3 and 3.5% were used to compare the phase-based T2 estimation to the gold standard SE–SE, using three TE values (10, 30 and 50 ms). A 3D head-shaped phantom that was designed to model the RF field distribution in the brain was used to examine the T2 and RF field estimation. This phantom was originally designed to include three sub-compartments30, suitable for mimicking brain, muscle and lipid tissues. However, the version used in this study was filled with two “tissue” types: the inner compartment mimicked the “brain” and the outer one, “muscle” (the planned lipid layer was also filled with “muscle”). Both compartments contained 0.1 mM gadopentetate dimeglumine (GdDTPA), for a T1 close to that of human white matter, and consisted of an agarose suspension of 2.5% and 3% for the “brain” and “muscle” compartments, respectively. NaCl (5.5 gr/L) was used to achieve an in-vivo-like RF field distribution. For details, see Ref.30.
α maps from the phase-based method were compared to the equivalent α maps generated by the vendor. As the RF field maps provided by the vendor are scaled to 90°, they were rescaled to the αscan of the phase-based method, before comparison. The average deviation between the α maps by the phase-based method and by the vendor were calculated in two main planes (Sagittal and Axial).
The common scan parameters for the phase-based method and SE–SE used in the agar-tube experiments in Fig. 3a) were: FOV 200 × 200 × 104 mm3, resolution 1.1 × 1.1 × 2 mm3, acquired matrix size 176 × 176 × 52. The phase-based method specific parameters were (φinc1 = 3°, α1 = 15°) and (φinc2 = 1.5°, α2 = 30°), TR/TE 10/2.2 ms, using 4 scans with a total scan duration of 6:06 min. The specific scan parameters for SE–SE were: TR—6500 ms, 3 scans with TE = 10,30,50 ms, × 3 in-plane acceleration, with a total scan duration of 19:04 min. The T2 and α maps were estimated based on Bloch simulation with T1 = 2 s.
The common scan parameters for the phase-based method and SE–SE that were used for the 3D head-shaped phantom in Fig. 3b): FOV 220 × 220 × 144 mm3, isotropic resolution of 1.5 mm, bandwidth per pixel 400 Hz. The phase-based method specific parameters were acquired matrix size 150 × 148 × 96, (φinc = 3, α = 15°) and (φinc = 1.5, α = 30°), TR/TE 10/2.1 ms, using 4 scans with a total scan duration of 9:28 min. The specific scan parameters for SE–SE (Fig. 3c) were: acquired matrix size 144 × 144 × 96, TR—6500 ms, 3 scans with TE = 10, 30, 50 ms, × 3 acceleration, with a total scan duration of 21:12 min. The vendor RF field map scan parameters (Fig. 3d): FOV 220 × 220 × 144 mm3, resolution 2.3 × 2.3 × 4 mm. The T2 and α maps were estimated based on Bloch simulation with T1 = 1.5 s (based on estimated T1 of the “brain” tissue).
Human imaging
All methods were carried out in accordance with the Weizmann Institute of Science guidelines and regulations. This study was approved by the Internal Review Board of the Wolfson Medical Center (Holon, Israel) and all scans were performed after obtaining informed suitable written consents. Human scanning of six volunteers with isotropic 1.5 mm resolution was acquired for the comparison with SE–SE. The comparison was performed after the SE–SE and the phase-based method images were realigned using SPM12 (https://www.fil.ion.ucl.ac.uk/spm/) to ensure there was no movement between the scans.
An additional volunteer was scanned with the phase-based method with 1 mm and 0.85 mm resolution. These scans were acquired with an acceleration of × 5.11—using elliptical sampling and × 2 acceleration in both phase encoding directions. The BART40 software was used to reconstruct this dataset.
Scan parameters for the phase-based method and SE–SE comparison with isotropic 1.5 mm voxel
Phase-based method: FOV 220 × 220 × 144 mm3, acquired matrix size 150 × 148 × 96, bandwidth per pixel 400 Hz, TR/TE 10/2.1 ms, (φinc1 = 3°,αscan1 = 15°), (φinc1 = 1.5°, αscan2 = 24–26°) (the αscan2 varied from 24° to 26° according to the specific volunteer’s 100% “Normal” SAR level), with duration of 4 scans—9:28 min. SE–SE: FOV 220 × 220 × 132 mm3, acquired matrix size 144 × 144 × 88, bandwidth per pixel 400 Hz, TR- 6500 ms, TE = 10, 30, 50 ms, using 3 scans with a total scan duration of 21:12 min. Vendor RF field map scan parameters: FOV 220 × 220 × 192 mm3, resolution 3 × 3 × 4 mm.
Phase-based method 1 mm resolution parameters
FOV 220 × 220 × 160 mm3, bandwidth per pixel 400 Hz, TR/TE 10/2.7 ms, (φinc1 = 3°,αscan1 = 15°), (φinc1 = 1.5°, αscan2 = 25°), duration of 4 scans—4:52 min.
Phase-based method 0.85 mm resolution parameters
FOV 220 × 220 × 163 mm3, bandwidth per pixel 400 Hz, TR/TE 10/2.7 ms, (φinc1 = 3°,αscan1 = 15°), (φinc1 = 1.5°, αscan2 = 25°), duration of 4 scans—6:49 min.
Data availability
All scans collected in this study were performed according to procedures approved by the Internal Review Board of the Wolfson Medical Center (Holon, Israel). Since this protocol was not defined as an open repository, the data is not provided, to provide the ethics and privacy issues of clinical data. The code will be made available via a request to the corresponding author.
References
Uğurbil, K. et al. Brain imaging with improved acceleration and SNR at 7 Tesla obtained with 64-channel receive array. Magn. Reson. Med. 82, 495–509 (2019).
Zeineh, M. M. et al. Ultrahigh-resolution imaging of the human brain with phase-cycled balanced steady-state free precession at 7 T. Investig. Radiol. 49, 278–289 (2014).
Wu, X. et al. High-resolution whole-brain diffusion MRI at 7T using radiofrequency parallel transmission. Magn. Reson. Med. 80, 1857–1870 (2018).
Gras, V. et al. Design of universal parallel-transmit refocusing k T -point pulses and application to 3D T2-weighted imaging at 7T: Universal pulse design of 3D refocusing pulses. Magn. Reson. Med 80, 53–65 (2018).
Bouhrara, M. et al. Quantitative age-dependent differences in human brainstem myelination assessed using high-resolution magnetic resonance mapping. Neuroimage 206, 116307 (2020).
Knight, M. J. et al. Quantitative T2 mapping of white matter: Applications for ageing and cognitive decline. Phys. Med. Biol. 61, 5587–5605 (2016).
Juras, V. et al. The comparison of the performance of 3 T and 7 T T2 mapping for untreated low-grade cartilage lesions. Magn. Reson. Imaging 55, 86–92 (2019).
Henry, T. R. et al. Hippocampal sclerosis in temporal lobe epilepsy: Findings at 7 T. Radiology 261, 199–209 (2011).
Bruschi, N., Boffa, G. & Inglese, M. Ultra-high-field 7-T MRI in multiple sclerosis and other demyelinating diseases: from pathology to clinical practice. Eur. Radiol. Exp 4, 59 (2020).
Luo, Z. et al. The correlation of hippocampal T2-mapping with neuropsychology test in patients with Alzheimer’s disease. PLoS ONE 8, e76203 (2013).
Shepherd, T. M. et al. New rapid, accurate T 2 quantification detects pathology in normal-appearing brain regions of relapsing-remitting MS patients. NeuroImage Clinical 14, 363–370 (2017).
Emmerich, J. et al. Rapid and accurate dictionary-based T 2 mapping from multi-echo turbo spin echo data at 7 Tesla: Dictionary-Based T 2 Mapping. J. Magn. Reson. Imaging 49, 1253–1262 (2019).
Hilbert, T. et al. Accelerated T2 mapping combining parallel MRI and model-based reconstruction: GRAPPATINI: Accelerated T2 mapping. J. Magn. Reson. Imaging 48, 359–368 (2018).
Vaughan, J. T. et al. 7T vs 4T: RF power, homogeneity, and signal-to-noise comparison in head images. Magn. Reson. Med. 46, 24–30 (2001).
Ineichen, B. V., Beck, E. S., Piccirelli, M. & Reich, D. S. New prospects for ultra-high-field magnetic resonance imaging in multiple sclerosis. Invest. Radiol. 56, 773–784 (2021).
Ma, D. et al. Magnetic resonance fingerprinting. Nature 495, 187–192 (2013).
Cloos, M. A. et al. Multiparametric imaging with heterogeneous radiofrequency fields. Nat. Commun. 7, 12445 (2016).
Leroi, L. et al. Simultaneous proton density, T1, T2, and flip-angle mapping of the brain at 7 T using multiparametric 3D SSFP imaging and parallel-transmission universal pulses. Magn. Reson. Med. 84, 3286–3299 (2020).
Heule, R., Celicanin, Z., Kozerke, S. & Bieri, O. Simultaneous multislice triple-echo steady-state (SMS-TESS) T1, T2, PD, and off-resonance mapping in the human brain. Magn. Reson. Med 80, 1088–1100 (2018).
Kobayashi, N. et al. Development and validation of 3D MP-SSFP to enable MRI in inhomogeneous magnetic fields. Magn. Reson. Med. 85, 831–844 (2021).
Deoni, S. C. L., Peters, T. M. & Rutt, B. K. High-resolution T1 and T2 mapping of the brain in a clinically acceptable time with DESPOT1 and DESPOT2. Magn. Reson. Med. 53, 237–241 (2005).
Heule, R., Bause, J., Pusterla, O. & Scheffler, K. Multi-parametric artificial neural network fitting of phase-cycled balanced steady-state free precession data. Magn. Reson. Med. 84, 2981–2993 (2020).
Shcherbakova, Y., van den Berg, C. A. T., Moonen, C. T. W. & Bartels, L. W. On the accuracy and precision of PLANET for multiparametric MRI using phase-cycled bSSFP imaging. Magn. Reson. Med. 81, 1534–1552 (2019).
Deoni, S. C. L. Transverse relaxation time (T2) mapping in the brain with off-resonance correction using phase-cycled steady-state free precession imaging. J. Magn. Reson. Imaging 30, 411–417 (2009).
Heule, R., Ganter, C. & Bieri, O. Triple echo steady-state (TESS) relaxometry: TESS relaxometry. Magn. Reson. Med. 71, 230–237 (2014).
Heule, R. et al. Triple-echo steady-state T2 relaxometry of the human brain at high to ultra-high fields: TESS T2 relaxometry of the human brain at high to ultra-high fields. NMR Biomed. 27, 1037–1045 (2014).
Wang, X., Hernando, D. & Reeder, S. B. Phase-based T2 mapping with gradient echo imaging. Magn. Reason. Med. 84, 609–619 (2020).
Tamir, J. I. et al. T2 shuffling: Sharp, multicontrast, volumetric fast spin-echo imaging. Magn. Reson. Med. 77, 180–195 (2017).
Reeder, S. B. & Wang, X. System and method for determining patient parameters using radio frequency phase increments in magnetic resonance imaging. Patent No. US 10,845,446 B2 (2020).
Jona, G., Furman-Haran, E. & Schmidt, R. Realistic head-shaped phantom with brain-mimicking metabolites for 7 T spectroscopy and spectroscopic imaging. NMR Biomed. 34, e4421 (2021).
Zur, Y., Stokar, S. & Bendel, P. An analysis of fast imaging sequences with steady-state transverse magnetization refocusing. Magn. Reson. Med. 6, 175–193 (1988).
Zur, Y., Wood, M. L. & Neuringer, L. J. Spoiling of transverse magnetization in steady-state sequences. Magn. Reson. Med. 21, 251–263 (1991).
Zhang, K., Zuo, W., Chen, Y., Meng, D. & Zhang, L. Beyond a Gaussian denoiser: Residual learning of deep CNN for image denoising. IEEE Trans. on Image Process. 26, 3142–3155 (2017).
Tamada, D. & Reeder, S. B. Phase-based T2 mapping using RF phase-modulated dual echo steady-state (DESS) imaging. Proc. Intl. Soc. Mag. Reson. Med. 29, 3081 (2021).
Zhang, J., Kolind, S. H., Laule, C. & MacKay, A. L. How does magnetization transfer influence mcDESPOT results?: MT Influence on mcDESPOT. Magn. Reson. Med. 74, 1327–1335 (2015).
Bieri, O., Ganter, C. & Scheffler, K. On the fluid-tissue contrast behavior of high-resolution steady-state sequences: Fluid-tissue contrast behavior of high-resolution SSFP. Magn. Reason. Med. 68, 1586–1592 (2012).
Zhang, J., Kolind, S. H., Laule, C. & MacKay, A. L. Comparison of myelin water fraction from multiecho T2 decay curve and steady-state methods: Multiecho T2 relaxation method and mcDESPOT. Magn. Reson. Med. 73, 223–232 (2015).
Deoni, S. C. L., Rutt, B. K., Arun, T., Pierpaoli, C. & Jones, D. K. Gleaning multicomponent T1 and T2 information from steady-state imaging data: 2D relaxometry with steady-state imaging. Magn. Reson. Med. 60, 1372–1387 (2008).
Dumez, J.-N. & Frydman, L. Multidimensional excitation pulses based on spatiotemporal encoding concepts. J. Magn. Reson. 226, 22–34 (2013).
Generalized Magnetic Resonance Image Reconstruction using The Berkeley Advanced Reconstruction Toolbox. https://mrirecon.github.io/bart/.
Acknowledgements
We are grateful to Dr. Sagit Shushan (Wolfson Medical Center), Dr. Edna Haran and the Weizmann Institute’s MRI technician team—E. Tegareh and N. Oshri—for assistance in the human imaging scans. We thank Dr. Jean-Nicolas Dumez for the Bloch simulation code.
Author information
Authors and Affiliations
Contributions
The theoretical analysis and manuscript drafting were carried out by R.S. and A.S. The data collection and experiment analysis were carried out by R.S.
Corresponding author
Ethics declarations
Competing interests
A.S. is employed by Siemens Healthcare Ltd, Israel; all other authors declare no competing financial interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Movie S1.
Supplementary Movie S2.
Supplementary Movie S3.
Supplementary Movie S4.
Supplementary Movie S5.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seginer, A., Schmidt, R. Phase-based fast 3D high-resolution quantitative T2 MRI in 7 T human brain imaging. Sci Rep 12, 14088 (2022). https://doi.org/10.1038/s41598-022-17607-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17607-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.