Abstract
Adhesive cementation of ceramic veneers may increase pulpal temperature (PT) due to the combined effect of heat generated by the curing unit and the exothermic reaction of the luting agent (LA). PT increase may induce pulpal damage. The aim was to determine the PT rise during the luting of ceramic veneers (CV) of different thicknesses with light- or dual-curing (LC, DC) adhesive cements as well as pre-heated restorative resin-based composites (PH-RBC). For this a thermocouple sensor was positioned in the pulp chamber of a prepared maxillary central incisor. LC, DC adhesive cements and PH-RBCs heated to 55 °C were used for the luting of CVs of 0.3, 0.5, 0.7, and 1.0 mm thicknesses. The exothermic reaction of LAs added significantly to the thermal effect of the curing unit. PT change ranged between 8.12 and 14.4 °C with the investigated combinations of LAs and ceramic thicknesses (p ≤ 0.01). The increase was inversely proportional to the increasing CV thicknesses. The highest rise (p ≤ 0.01) was seen with the polymerization of PH-RBCs. Temperature changes were predominantly influenced by the composition of the LA, which was followed by CV thickness.
Similar content being viewed by others
Introduction
Ceramic laminate veneers are widely used as esthetic restorations for the correction of unfavorable tooth appearance. The design of the preparation, tissue removal, as well as the thickness of the restoration is dependent on the specific indication for the ceramic veneer. Their proportionality is not unequivocal1. Although conventional tooth preparation for laminate veneers can be considered a reliable technique, minimally invasive or even ‘prepless’ veneers are regarded as additional methods applicable for tooth preparation2.
The clinical success and durability of a porcelain veneer is greatly influenced by the strength of the adhesion formed between the interfaces of the three different components; the porcelain veneer, luting agent and tooth surface3. A close apposition of the enamel and the porcelain surfaces has a synergistic effect on the overall bond strength of the enamel/luting agent/porcelain complex4. This complex is characterized by a higher bond strength compared to the sum of the individual attachments between the enamel/luting agent and luting agent/porcelain4. In order to provide this ultimate linkage, adhesive resin cements are typically used for the cementation of ceramic veneers. This also improves the fracture resistance of the inherently brittle ceramics5. Their good esthetic and mechanical properties as well as low solubility in the oral environment can further improve the quality of these restorations3,6,7. Within the group of adhesive cements, light-curing resin cements are generally preferred due to their longer working time and superior color stability8. Since the porcelain veneer absorbs between 40 and 50% of the emitted light, their thickness is the primary factor in determining light transmittance available for polymerization9. In case of a porcelain with a thickness of more than 0.7 mm, light-cured resin composites do not reach their maximum hardness10. In such cases, the use of dual-cured adhesive resin cements is advised. Failures associated with these adhesive resin cements are disintegration in marginal integrity and discoloration1,11.
The use of pre-heated restorative resin-based composites (RBC) as luting agents was first described in 198712. Their application is enjoying increasing popularity in today’s clinical practice. Given their reduced viscosity, allowing for thin film thickness, good adaptation and the benefits of high filler content the use of pre-heated RBCs as luting agents has been extensively assessed by clinical studies and laboratory investigations13,14,15,16,17,18. The increased filler load improves mechanical- and bond strength, thereby improving fracture resistance15,19. In comparison to resin cements, pre-heated RBCs are also less expensive as well as offer a greater range of shades. Additionally, they decrease polymerization shrinkage and stress generation in the exposed cement layer at the bonded interface which imparts greater resistance to intraoral degradation16. Aside from these benefits however, pre-heated RBCs were also found to negatively influence the adaptation of fixed dental prostheses as reported by a recent systematic review20.
Regardless of the luting agent used, a high degree of conversion (DC) is key to achieving the previously described benefits through different thicknesses of ceramic veneers21,22. Although, the use of a high-irradiance curing unit or longer exposure duration can improve DC, these processes also involve thermal reactions which could potentially be hazardous to the dental pulp23,24. The temperature rise during the curing of resin-based dental materials is attributed to both the energy absorbed during irradiation with light-curing units and the exothermic reaction of polymerization25,26,27. Although, both the remaining dentin thickness and the ceramic veneer have temperature-shielding effects, the pulpal temperature (PT) rise may still exceed the presumed threshold of 5.5 °C, even without the use of a resin cement28. The exothermic reaction which characterises polymerization can further increase PT and is proportional with the amount of C=C bonds present in the given resin cement. The capacity of the inorganic compartments to absorb external energy also affect heat diffusion within the material29,30. According to a systematic review on porcelain veneers, the frequency of endodontic failure (1%) is similar to debonding (0.8%), however the overall clinical survival is still considered to be high31. An ex vivo study showed a temperature rise of 5.5 °C lasting for 40 s to lead to immediate cell damage32. The examined cells were protected against apoptosis by a complex interaction of molecular processes. Apoptosis was detected when temperatures reached 7.5 °C32. In support of this observation, in a recent in vivo study, the authors concluded that increased PTs may induce inflammatory reactions, even if the temperature rise does not exceed the previously defined threshold of 5.5 °C33. Whilst the real significance of pulpal temperature rise is still controversial, it is accepted that it should be kept as low as possible during dental procedures involving the polymerization of light cured materials34,35. The temperature increase detected during RBC polymerization is the sum of the exothermic reaction of polymerization and the energy absorbed during irradiation with light curing units (LCU)25,26. This topic has been investigated by several studies in the past. These have addressed in particular the impact of the radiant energy, spectral characteristics of the curing unit and the RBC type or shade as well as applied thickness on the temperature rise within the pulp chamber36,37,38,39. Most of the studies found the applied radiant energy to be the crucial factor in pulpal temperature rise. The exothermic reaction of the RBCs was also found to be a contributing factor26,38,39,40. The use of resin-based adhesive cements and pre-heated RBCs as luting agents for ceramic veneers are widely indicated since these materials can increase the fracture resistance of ceramic restorations. Adhesive luting is also a more conservative approach which preserves larger amounts of dental tissue5,41,42. Although, the thermal effect of LCUs and the exothermic polymerization of the adhesive luting material dominates during veneer cementation, the shielding effect of the ceramic veneer against light transmission may modify this unfavorable temperature rise within the pulp chamber. Taking light attenuation into consideration as a function of the restoration thickness, it is assumed that the temperature rise is strongly influenced by the interposing ceramic thickness28,43. Although data is already available on the thermal effect of resin-based materials as well as the shielding effect of ceramics, their combinatorial effect is less investigated. Therefore, the purpose of the present in vitro study was to compare the intrapulpal thermal changes resulting from the cementation of various thickness ceramic veneers with light- and dual-curing adhesive resin cements as well as pre-heated sculptable submicron and microhybrid bulk-fill RBCs. The null-hypotheses of the research were two-fold; (1) there is no difference in PT change using different luting agents during ceramic veneer cementation, and that (2) there is no significant influence of ceramic layer thickness on PT rise.
Methods
Resin-based luting agents, ceramic plates and radiant exposure
During this in vitro study the effects of four resin-based luting agents (RLA); a light-curing (LC) and a dual-curing (DC) adhesive resin cement, a pre-heated sculptable submicron-filled and a pre-heated sculptable microhybrid restorative RBC on PTs were analyzed. The brands, chemical compositions and manufacturers are presented in Table 1.
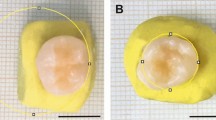
Medium translucent A1 shade lithium disilicate ceramic plates (7 × 7 mm) were fabricated from GC Initial LiSi veneering ceramic ingots (GC Initial LiSi Press; GC Europe, Leuven, Belgium) by heat-pressed method and were then fired and glazed from one side (veneered surface) according to the manufacturer’s instruction. The specimens were then finished to achieve an even and smooth surface using 220-, 400-, and 600-grit sandpaper under water-cooling. This was followed by polishing using silicone points. Ceramic plates, intended to represent the veneers, were fabricated in thicknesses of 0.3 mm, 0.5 mm, 0.7 mm and 1.0 mm. The final dimensions of each ceramic plate were confirmed using a digital caliper with 0.001 mm accuracy (ABS Digimatic Caliper; Mitutoyo, Tokyo, Japan). The ceramic specimens were not acid-etched or silanated and nor were they coated with an adhesive.
The single dose capsulated restorative RBCs were pre-heated to 55 °C in a composite warming device (Ena Heat; Micerium, Avegno, Italy) for 15 min. Each capsule was heated just once for the cementation of 1 specimen only. The resulting RBC temperatures were measured with a non-contact infrared (IR) optics coupled to a digital thermometer (TESTO 845; Testo Magyarország, Budapest, Hungary). The IR thermometer was able to register temperatures in an area as small as 1 mm2 (optical resolution of 75:1) with a resolution of 0.1/1 °C and a data sampling frequency of 10 measurements per second. For the measurements conducted during the actual luting with the pre-heated RBCs, the ceramic plates were also pre-warmed in the same device to reduce heat dissipation.
During the experiments the same Light Emitting Diode (LED) light curing unit (LCU) (LED.D; Woodpecker, Guilin, China; Λ = 420–480 nm; 8 mm exit diameter fiberglass light guide) was used operated in a standard mode for 40 s. This was powered by a line cord at room temperature of 24 °C ± 1 °C controlled by an air-conditioner. The positioning of the light guide tip was standardized ensuring each sample received the same light beam character. The radiant exitance (mW/cm2) and exposure (J/cm2) delivered by the light curing unit (LCU) were measured using a radiometer (checkMARC; Bluelight Analytics, Halifax, Canada). The radiant exitance at the tip of the LCU was measured by placing the tip at a standard distance of 1 mm from the radiometer sensor. The radiant exposure was also calculated. The light attenuation of the four different thicknesses of ceramic plates was measured similarly, by placing the tip of the LCU at a standard distance of 1 mm over the ceramic specimen which was positioned centrally on the sensor.
Sample preparation for pulpal temperature measurements
All methods were performed in accordance with the Declaration of Helsinki principled. Ethical approval was granted by the Regional Research Ethical Committee of University of Pécs to use extracted teeth for research purposes (approval number: IRB: PTE/3795) and informed consent was obtained from the subject. The maxillary central incisor to be used in this study was removed for periodontal reasons (severe attachment loss indicating extraction). The freshly extracted, caries-free, cleaned tooth was initially kept in physiological saline. A single tooth model was chosen for all experimental trials to limit any effects from structural differences in enamel and dentin26. The vestibular surface was prepared and polished flat leaving a two-millimeter thin layer of enamel and dentin from the buccal wall of the pulp chamber. The enamel thickness to be removed was estimated and controlled by a digital intraoral radiograph. Five millimeters of the root apex were also removed to expose the root canal. All pulpal residues were removed with endodontic files. This was followed first by irrigation with 5.25% sodium-hypochlorite solution, then saline and finally dried with paper points. To allow the insertion of the 0.5 mm diameter Cu/CuNi K-type thermocouple probe (Type K thermocouple; TC Direct, Budapest, Hungary) a hole was created on the palatal cingulum of the tooth with a one-millimeter diameter cylindrical diamond bur. The thermocouple sensor was fixed to the dentin on the buccal wall of the pulp chamber by means of a thin layer of cyanoacrylate glue (Loctite Super Glue; Loctite, Düsseldorf, Germany). The palatal hole was closed with flowable RBC (Filtek Supreme Flowable; 3 M, St. Paul, MN, USA). The remaining enamel and dentin thickness as well as the position of the thermocouple were confirmed radiographically. The pulp chamber and root canal were subsequently injected with ECG gel (Aqua Sound Basic; Ultra-gel Hungary 2000, Budapest, Hungary) to replicate pulp tissue. Flowable RBC was used to close the apical orifice and the tooth was embedded in clear acrylic one millimeter below the cemento-enamel junction. The tooth was immersed in a water bath of 37.0 ± 0.5 °C. Temperature measurements and heat registrations were recorded by a digital thermometer (El-EnviroPad-TC; Lascar Electronics, Salisbury, UK) attached to the thermocouple, with resolution of 0.1 °C and frequency of one measurement per second.
Firstly, only the thermal effect of the LCU after a 40 s exposure was measured. To provide heat conduction, a transparent heat conducting silicone gel (8462 Silicone Grease; MG Chemicals, Burlington, Ontario, Canada; heat conductivity: 0.16 W/mK) was applied between the dentin and ceramic surfaces. The temperature changes during the cementation of 0.3 mm, 0.5 mm, 0.7 mm and 1.0 mm ceramic specimens, with the application of the four investigated RLA were measured (Fig. 1).
RLA of a standard volume was applied to the center of the non-glazed ceramic surface. This was then centrally oriented to the prepared tooth surface and manually loaded with a 5 N load in the case of resin adhesive cements, and 10 N load when pre-heated restorative RBCs were investigated. Measurements from preliminary tests showed that the manual placement of the ceramic body with a load of 5 or 10 N achieved a consistent RLA layer thickness of 100 ± 10 μm. An algometer was used to ensure the size of the load (Force Dial FDK 16; Wagner, Greenwich, USA). Excess luting agent was removed using a microbrush and the RLA was photoactivated through the ceramic plate for 40 s.
The cemented specimen was then swiftly removed and the thickness measured using the digital caliper. The film thickness was calculated from the difference between the thickness of the cemented specimen and the ceramic plate alone. There were a total of 16 groups for the various ceramic veneer/RLA combinations, and temperature measurements were recorded 5 times for each (n = 5).
Since no dental adhesive system or ceramic surface treatment was used, the polymerized RLA could easily be removed from both the tooth and ceramic plate following the measurements without leaving any deposits on either of the surfaces. This enabled the same tooth to be re-used for each measurement.
Statistical analysis
Pilot study results and sample size formula were used to estimate sample size44.
Sample size formula: \(n=\frac{{({z}_{1-\frac{\alpha }{2}}+{z}_{1-\beta })}^{2}{({s}_{1}+{s}_{2})}^{2}}{({M}_{1}-{{M}_{2})}^{2}}\)
[z = standard score; α = probability of Type I error at 95% confidence level = 0.05; z1−α/2 = 1.96 for 95% confidence; β = probability of Type II error = 0.20; 1 − β = the power of the test = 0.80; z1−β = value of standard normal variate corresponding to 0.80 value of power = 0.84; s1 = standard deviation of the outcome variable of group 1 = 0.27; s2 = standard deviation of the outcome variable of group 2 = 0.44; M1 = mean of the outcome variable of group 1; M2 = mean of the outcome variable of group 2; (M1—M2) = 0.5 if it is expected to detect 0.5 °C difference between two investigated groups as significant.] Using the formula Nfinal = \(\frac{2n}{1-0.1}\) the predicted sample size (n) was found to be a total of 4.9 samples per group. According to the calculation n = 5 per group sample size was selected.
The statistical analyses were performed with SPSS (Version 26.0; IBM, Armonk, NY, USA). The normal distribution of the data was tested with the Kolmogorov–Smirnov test. The data was subsequently subjected to a parametric statistical test. The differences in light attenuation and temperature change were compared with one-way analysis of variance (ANOVA). Tukey’s post hoc adjustment was used for multiple comparison in all ANOVA models. Multivariate analysis (general linear model) and partial eta-squared statistics were used to test the influence and describe the relative effect size for luting material and ceramic thickness as independent factors. P values below 0.05 were considered statistically significant.
Results
The remaining dentin-enamel thickness was 2 ± 0.2 mm based on the measurements taken at three different locations on the radiographic image of the tooth. The maximum radiant exitance of the LED LCU was 1320 ± 10 mW/cm2. The drop of total radiant exposure was significant (p < 0.01) through all the investigated ceramic thicknesses. There was a radiant exitance reduction of 30%, 40%, 50% and 60% through the 0.3 mm, 0.5 mm, 0.7 mm and 1.0 mm thick ceramic specimens, respectively. One-way ANOVA and Tukey’s post hoc tests indicated that the differences between the light irradiance transmitted through the ceramic plates of different thicknesses were statistically significant (p < 0.01).
In the case of PT changes, light curing without the interposition of ceramic veneers or RLA increased the 37 °C base temperature by 9 °C. The interposition of a ceramic plate (without RLA) limited this temperature increase and was found to be inversely proportional with the ceramic thickness (Fig. 2).
The statistical analysis did not find a statistically significant difference in light attenuation between either the 0.3 and 0.5 mm thick specimens, or the 0.7 and 1.0 mm thick ceramic veneers. Contrastingly, the difference was shown to be significant between 0.5 and 0.7 mm (p < 0.01). The 1.0 mm thick ceramic specimen reduced the thermal effect of the light curing unit by 2.5 °C, the 0.7 mm by 2.3 °C, the 0.5 mm ceramic by 1.3 °C and the 0.3 mm thick ceramic plate by 1.1 °C.
Overall, the highest temperature rise during the polymerization of different RLAs through different thicknesses of ceramic veneers was seen with the application of the pre-heated restorative RBC FOB_55 °C (p < 0.001), which was followed by the pre-heated restorative RBC EQ_55 °C (p < 0.001). With the above RLAs, a statistically significant difference in temperature increase was found when cured through the 0.3 mm (p < 0.001), 0.7 mm (p = 0.037) and 1.0 mm (p = 0.005) thick ceramic veneers. Generally, the pre-heated materials increased the pulpal temperature by approximately 3–3.5 °C which occurred precisely as the cement was applied to the tooth surface. The time between removal of the RBC from the heating device and application to the tooth surface took 3–4 s and additional 6–7 s were required to apply the veneer before light curing.
When luting with the dual-curing adhesive cement (VE_DC) a lower temperature increase was found compared to the pre-heated restorative RBCs. The lowest temperature increase was recorded during the polymerization of the light-cure adhesive cement VE_LC (Fig. 3).
The results of the one-way ANOVA and Tukey's post hoc adjustment tests performed on the temperature recordings taken during the polymerization of ceramic veneers with different RLAs are presented in Table 2.
As regards to the various ceramic veneer thicknesses, only the 0.3 mm thick specimen resulted in a significantly higher PT increase with the application of VE_LC, VE_DC, FOB_55 °C RLA (p < 0.001). On comparison of the 0.5 mm, 0.7 mm and 1.0 mm thicknesses, no significant rise in PT was demonstrated with VE_DC, EQ_55 °C and FOB_55 °C RLA. Statistically significant differences in temperature rise were measured between the 0.5 mm and 1.0 mm thick veneers (p < 0.002) and the 0.7 mm and 1.0 mm veneers (p < 0.002) with the application of VE_LC. The above-mentioned ceramic thicknesses in combination with VE_LC showed a heat dissipating effect on comparison to the thermal effect of the light-curing unit alone (Fig. 4). The results of the one-way ANOVA and Tukey's post hoc adjustment tests on the recorded intrapulpal temperature changes during the polymerization of various RLAs through different thicknesses of ceramic veneers are presented in Table 3.
Pulpal temperature changes during polymerization of light-cured, dual-cured resin cements and pre-heated resin composites through different thicknesses of ceramic veneers. The grey layer shows the pulpal temperature rise caused by the light-curing unit alone. The image was constructed by SigmaPlot software (for Windows v. 12.0 build 12.2.0.45, Systat Software, Palo Alto, CA, USA).
A 4 (Material) × 4 (Temperature) mixed-model ANOVA revealed that the main effect for both Material and Thickness on temperature change values were significant (p < 0.001) and the effect size was considered to be large (Material Partial ƞ2 was 0.96 and Thickness Partial ƞ2 was 0.64). The interaction of the two factors (Material × Temperature) did not show a significant effect (p = 0.28; Partial ƞ2 = 0.15) on the PT change during veneer cementation with the investigated materials. The high R2 value means a very close fit to the exponential regression lines (Fig. 5).
Discussion
The present in vitro study demonstrated significant differences in PT changes when using light-cured, dual-cured adhesive cements, pre-heated restorative RBCs in combination with different ceramic thicknesses for veneer cementation. Hence both null-hypotheses were rejected. These results are consistent with other findings regarding the material-dependent temperature-increasing effect of RBC polymerization or the shielding effect of the interposed ceramic on PT rise25,26,28,43. General Linear Model demonstrated the importance of the RBC composition, as the effect size of the Material factor was found to be large on the PT rise. This is in line with a recent in vitro study where the effects of distinct types of RBCs on intrapulpal temperature rise were compared and the influence of the resin matrix system and filler content was found to be significant26. The effect size was shown to be medium for ceramic thickness implying that the shielding effect of the ceramic was less reliable compared to the exothermic effect of the adhesive luting agent. The present investigation highlights, that even though the interposed ceramic veneer attenuates the light intensity and thus the delivered energy for polymerization, the exothermic temperature rise associated with the adhesive luting agent may jeopardize pulp health.
In this study the measurements were carried out on a single permanent central incisor without the use of an adhesive system for all experimental groups to provide the same tooth-related conditions and eliminate any effect which may arise from structural and optical differences of the enamel and dentin. Although this provided a standard model to detect differences in temperature changes during the polymerization of RLAs, the lack of an adhesive layer application can be considered a limitation of the present study. The polymerized adhesive layer may serve as a barrier to heat transfer under clinical conditions. It is important to consider, that during polymerization of the adhesive layer the PT may increase faster than during the photocuring of the RBC, especially with an irradiance above 1000 mW/cm245. Heat generated by the irradiation of the RBC could potentially compound thermal damage, as the pulpal and dentin temperatures are already higher due to the adhesive layer polymerization.
Thermal transfer to the pulp is strongly dependent on the thickness of the remaining tooth structure28,46. The thermal conductivity of enamel and dentin is ~ 0.45–0.93 W/mK and ~ 0.11–0.96 W/mK, respectively, which is considered to be low47. Increasing the thickness of the dentin results in an enhanced thermal-insulation effect28. One would assume that the increasing veneer thickness necessitates a proportional increase in the removal of tooth hard tissues, but in reality, veneer preparation design is strongly dependent on the specific indication. For instance, to align a buccoverted tooth, significant tissue removal could be required with a veneer of only minimal thickness. In contrast, for a palatoverted tooth, a thick veneer can optically align the tooth without any preparation. Consequently, the desired veneer thickness is not necessarily proportional to the amount of hard tissue removal. In the present study a standardized, conventional preparation design with ~ 2 mm remaining enamel / dentin thickness was employed for all the measurements in order to detect the effects of various veneer thicknesses and the type of the luting materials only. Although, the standard thickness of tooth structure could be a limitation of our study, considering the above-mentioned situations the 2 mm thick enamel/dentin in combination with different ceramic veneer thickness could be relevant clinical scenario.
Aside from the distance between the prepared tooth surface and the pulp, the effect of the pulpal blood circulation, perfusion rate, the volume and motion of the dentinal tubule fluid as well as the surrounding periodontal tissues also play important roles in heat conduction and protection against the rise of PT48. The clinical relevance of increased PT is the potential risk of thermal pulp damage23. Simulation of the pulpal circulation can decrease the intrapulpal temperature rise by two to four times compared to the results obtained in tests without simulation49. Although in vitro experiments demonstrated a material-dependent PT rise, which could exceed the 5.5 °C—considered to be the pathological threshold26—, it was concluded thereafter in an in vivo study, that neither a 2 mm deep cavity preparation nor the RBC polymerization resulted in a pulpal temperature rise approaching values that could represent a risk for thermal damage to the pulp50. As a limitation of our experiment, the study design lacked a simulation of the microcirculation. Although the tooth was held in a 37 ± 0.5 °C water bath for the duration of the study, this physiological temperature is not able to account for all the mechanisms by which heat is dissipated in vivo as the PT rises. The authors employed such a study design to illustrate the temperature changes which arise specifically due to the extent of the exothermic reaction which occurs in the investigated materials during veneer cementation. To provide the light required for the polymerization of the RLAs a second-generation LED LCU was used in this study with a radiant exitance of 1320 ± 10 mW/cm2 at a wavelength range of 420–480 nm. According to several previous experiments, the duration and intensity of the applied light seemed to be the most crucial factor in PT rise24,35,51,52,53. Results of the present study confirm this statement, since light-curing without the interposition of a ceramic veneer or RLA increased (ΔT = 9 °C) the PT by a significant degree. The extended exposure time (40 s) with a light irradiance of 1320 mW/cm2 resulted in 52.8 J/cm2 delivered radiant exposure. Because of the shielding effect of the ceramic and dentin during cementation, a high-intensity light or extended exposure time is recommended for complete polymerization. This also achieves acceptable mechanical properties and biocompatibility21,54,55,56. Whilst the increased delivered radiant exposure is beneficial to RLA polymerization, a strong positive correlation was found between energy density and PT rise57. Aside from the irradiance, the type and characteristics of the curing unit also have an impact on the amount of heat generated within the tooth39,58. During veneer cementation, ceramic interposition exhibits a temperature shielding effect. Results from the present investigation are consistent with the findings of previous studies which also showed an inverse relationship between ceramic thickness and temperature rise28. Our results showed, that the regression curve for temperature against the different thicknesses of ceramic showed a linear LCU energy loss with increasing thickness, which reflects the light attenuation occurring through an absorptive/scattering medium. Although the thickness of the ceramic veneer was found to be less significant in the pulpal temperature rise, as the difference proved to be significant between all the investigated veneer thicknesses only with the application of VE_LC. The linear regression model showed the value of the coefficient of determination to be only 5.6%. The shielding effect was lowest when polymerization occurred through the 0.3 mm thick ceramic veneers. The difference was significant compared to all thicker ceramics except when EQ_55 °C was used. Partial eta squared test showed that although the effect of ceramic thickness was significant on the pulpal thermal change the size of its effect was less when compared to that of the material’s. Regarding the relationship between resin cement hardness—which may reflect the degree of conversion—and ceramic type, thickness, translucency, and curing time, it was demonstrated that the effect size of ceramic thickness is the lowest among the other factors59. Aside from the light and heat attenuation capacity of ceramics, the shielding effect of increasing thickness of dentin may be more pronounced28.
Incomplete polymerization of the adhesive cement can lead to decreased bond strength, release of potentially toxic residual monomers, color change, increased risk of microleakage and debonding21,54,60. The heat energy released by the intense or extended lighting however, could cause injury to vital pulp tissues depending on the extent and length of the heat exposure32. Besides the characteristics of the employed light, the exothermic polymerization reaction of the luting agent also plays a significant role in PT rise. Our study design together with the single tooth model25,26 ensured uniform conditions allowing the comparison of the exothermic thermal change between different RLAs only. Previous researches found the exothermic reaction to be proportional to the amount of resin matrix available for polymerization and also found that the inorganic compartments affect heat diffusion within the material by their capacity to absorb external and internal energy26,29,30.
Furthermore, the type and concentration of the photoinitiator/accelerator system and the polymerization conditions also have an impact on the thermal change of the RBC during polymerization61. The latter includes, among others, the layer thickness of the applied material, spectral characteristics of the LCU, exposure time and the pre-polymerization temperature of the RBC62,63,64. Since the experimental conditions were standardized, the differences in the thermal change of the RLAs can be attributed to the different components. Regarding the composition of the investigated materials, although the light- and dual-cure RLAs have the same resin matrix/filler ratio, the dual-cure showed a significantly higher temperature rise compared to the light-cure RLA. The interpositioning of a ceramic veneer can reduce not only the degree of conversion in the case of the light-cure but also the dual-cure resin cement65,66. In the latter, the chemical setting allows for a more efficient polymerization compared to the light-cured resin cement21. Dual-cured resin cements are therefore able to compensate for decreased light transmission and may convert monomers to polymers more efficiently even with increased ceramic thicknesses. Since however, the polymerization of dual-cure RLA progresses to a higher degree, the accompanying exothermic reaction can further increase the PT as it was demonstrated also by our results.
Pre-heated restorative RBCs are used increasingly as luting agents for ceramic restorations due to their advantageous properties14,67. Although pre-heated RBCs have demonstrated better color stability, marginal adaptation, degree of conversion and strengthen ceramics13,68,69, the results of the present study warn of their potential hazard to pulp health as a result of their stronger thermal effect. Increased pre-cure temperature of the pre-heated RBCs elevated the PT by approximately 3 °C immediately, at the moment of the veneer placement. The temperature continued to rise with photocuring as the result of the heat generated by the light exposure and exothermic reaction. This may increase the degree of conversion and crosslinking by enhancing free radical and monomer mobility and intensifying collisions among molecules70,71. According to our results, the highest temperature rise was recorded with the use of FOB_55 °C followed by that of EQ_55 °C. On comparing the filler-matrix ratio, FOB contains 58.5 vol% inorganic component while EQ has 71 vol% filler content.
It means, that the former’s monomer ratio, thus the amount of C=C bonds is higher, leading to more a pronounced exothermic reaction. Furthermore, the chemical composition of the monomer matrix also has a strong influence on the polymerization kinetics. EQ is a BisGMA/TEGDMA based RBC, while FOB’s matrix is composed of UDMA, AUDMA, 1,12-DDMA, AFM monomers. BisGMA is considered to be the most viscous molecule among the above-mentioned monomers due to the strong intramolecular hydrogen bonding. This results in a limited rotational freedom, thus leading to reduced mobility and reactivity of this monomer during the polymerization process72. On the other hand, UDMA represents a combination of relatively high molecular weight with a high concentration of double bonds and low viscosity. This was shown to reach a higher degree of conversion and is characterized by an enhanced exothermic reaction73. Additionally, it is reasonable to assume a role also for a further FOB constituent, the so-called AFM, an addition-fragmentation chain transfer dimethacrylate monomer. This molecule participates readily in network formation by copolymerizing with multifunctional methacrylates further increasing the release of exothermic heat74. In addition to the monomer system, the filler-matrix ratio is also decisive regarding the degree of monomer to polymer conversion and exothermic heat release. EQ filler loading is higher compared to the filler content of FOB, which may restrict light penetration and the mobility of monomers and radicals.
It should be noted, that even though the partial eta-squared statistics demonstrated a high impact for the type and composition of luting material on pulpal thermal change, the results cannot be directly extrapolated to other RLAs.
Despite the limitations of this in vitro study, it can be concluded, that the intrapulpal temperature can increase above 8.12 °C during veneer cementation, using different combinations of RLA materials and ceramic thicknesses. The temperature values were predominantly influenced by the composition of the RLA materials followed by the thickness of the ceramic veneer. Moreover, the application of pre-heated restorative RBCs as luting agents resulted in a significantly higher temperature rise compared to that measured in the case of adhesive resin cements.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Veneziani, M. Ceramic laminate veneers: clinical procedures with a multidisciplinary approach. Int. J. Esthet. Dent. 12, 426–448 (2017).
D’Arcangelo, C., Vadini, M., D’Amario, M., Chiavaroli, Z. & De Angelis, F. Protocol for a new concept of no-prep ultrathin ceramic veneers. J. Esthet. Restor. Dent. 30, 173–179. https://doi.org/10.1111/jerd.12351 (2018).
Peumans, M., Van Meerbeek, B. V., Lambrechts, P. & Vanherle, G. Porcelain veneers: A review of the literature. J. Dent. 28, 163–177. https://doi.org/10.1016/s0300-5712(99)00066-4 (2000).
Stacey, G. D. A shear stress analysis of the bonding of porcelain veneers to enamel. J. Prosthet. Dent. 70, 395–402. https://doi.org/10.1016/0022-3913(93)90073-w (1993).
Moraes, R. R. et al. Light-activation of resin cement trough ceramic: Relationship between irradiance intensity and bond strength to dentin. J. Biomed. Mat. Res. 85B, 160–165. https://doi.org/10.1002/jbm.b.30928 (2008).
Müller, J. A., Rohr, N. & Fischer, J. Evaluation of ISO 4049: water sorption and solubility of resin cements. Eur. J. Oral Sci. 125, 141–150. https://doi.org/10.1111/eos.12339 (2017).
Stewart, G. P., Jain, P. & Hodges, J. Shear bond strength of resin cements to both ceramic and dentin. J. Prosthet. Dent. 88, 277–284. https://doi.org/10.1067/mpr.2002.128034 (2002).
Stamatacos, C. & Simon, J. F. Cementation of indirect restorations: an overview of resin cements. Compend. Contin. Educ. Dent. 34, 42–46 (2013).
Rasetto, F. H., Driscoll, C. F., Prestipino, V., Masri, R. & von Fraunhofer, J. A. Light transmission through all-ceramic dental materials: A pilot study. J. Prosthet. Dent. 91, 441–446. https://doi.org/10.1016/S0022391304001106 (2004).
Linden, J. J., Swift, E. J., Boyer, D. B. & Davis, B. K. Photo-activation of resin cements through porcelain veneers. J. Dent. Res. 70, 154–157. https://doi.org/10.1177/00220345910700021201 (1991).
Fradeani, M., Redemagni, M. & Corrado, M. Porcelain laminate veneers: 6- to 12-year clinical evaluation: A retrospective study. Int. J. Periodontics Restorative Dent. 25, 9–17 (2005).
Friedman, M. Multiple potential of etched porcelain laminate veneers. J. Am. Dent. Assoc. Spec No, 83E-87E, https://doi.org/10.14219/jada.archive.1987.0317 (1987)
Almeida, J. R., Schmitt, G. U., Kaizer, M. R., Boscato, N. & Moraes, R. R. Resin-based luting agents and color stability of bonded ceramic veneers. J. Prosthet. Dent. 114, 272–277. https://doi.org/10.1016/j.prosdent.2015.01.008 (2015).
Magne, P., Razaghy, M., Carvalho, M. A. & Soares, L. M. Luting of inlays, onlays, and overlays with preheated restorative composite resin does not prevent seating accuracy. Int. J. Esthet. Dent. 13, 318–332 (2018).
Gresnigt, M. M. M. et al. Effect of luting agent on the load to failure and accelerated-fatigue resistance of lithium disilicate laminate veneers. Dent. Mater. 33, 1392–1401. https://doi.org/10.1016/j.dental.2017.09.010 (2017).
Coelho, N. F., Barbon, F. J., Machado, R. G., Bocato, N. & Moraes, R. R. Response of composite resins to preheating and the resulting strengthening of luted feldspar ceramic. Dent. Mater. 35, 1430–1438. https://doi.org/10.1016/j.dental.2019.07.021 (2019).
Gresnigt, M. M. M. et al. Performance of ceramic laminate veneers with immediate dentine sealing: An 11 year prospective clinical trial. Dent. Mater. 35, 1042–1052. https://doi.org/10.1016/j.dental.2019.04.008 (2019).
D’Arcangelo, C., De Angelis, F., Vadini, M. & D’Amario, M. Clinical evaluation on porcelain laminate veneers bonded with light-cured composite: Results up to 7 years. Clin. Oral Investig. 16, 1071–1079. https://doi.org/10.1007/s00784-011-0593-0 (2012).
Kameyama, A. et al. Luting of CAD/CAM ceramic inlays: direct composite versus dual-cure luting cement. Biomed. Mater. Eng. 25, 279–288. https://doi.org/10.3233/BME-151274 (2015).
de Souza, T.J.S., Freitas, A.S., Ferreira, D.M.T.P., Maia, L.C. & Rabello, T.B. Does the use of preheated restorative resin composite as a luting agent influence the adaptation of fixed dental prostheses? A systematic review. J. Prosthet. Dent. https://doi.org/10.1016/j.prosdent.2022.02.008 (2022).
Novais, V. R. et al. Degree of conversion and bond strength of resin-cements to feldspatic ceramic using different curing modes. J. Appl. Oral. Sci. 25, 61–68. https://doi.org/10.1590/1678-77572016-0221 (2017).
Runnacles, P., Correr, G., Filho, F. B., Gonzaga, C. C. & Furuse, A. Y. Degree of conversion of a resin cement light-cured through ceramic veneers of different thicknesses and types. Braz. Dent. J. 25, 38–42. https://doi.org/10.1590/0103-6440201302200 (2014).
Zach, L. & Cohen, G. Pulp response to externally applied heat. Oral Surg. Oral Med. Oral Pathol. 19, 515–530. https://doi.org/10.1016/0030-4220(65)90015-0 (1965).
Leprince, J., Devaux, J., Mullier, T., Vreven, J. & Leloup, G. Pulpal-temperature rise and polymerization efficiency of LED curing lights. Oper. Dent. 35, 220–230. https://doi.org/10.2341/09-203-L (2010).
Baroudi, K., Silikas, N. & Watts, D. C. In vitro pulp chamber temperature rise from irradiation and exotherm of flowable composites. Int. J. Paediatr. Dent. 19, 48–54. https://doi.org/10.1111/j.1365-263X.2007.00899.x (2009).
Lempel, E. et al. Degree of conversion and in vitro temperature rise of pulp chamber during polymerization of flowable and sculptable conventional, bulk-fill and short-fibre reinforced resin composites. Dent. Mater. 37, 983–997. https://doi.org/10.1016/j.dental.2021.02.013 (2021).
Seelbach, P., Finger, W. J., Ferger, P. & Balkenhol, P. M. Temperature rise on dentin caused by temporary crown and fixed partial denture materials: Influencing factors. J. Dent. 38, 964–973. https://doi.org/10.1016/j.jdent.2010.08.008 (2010).
Kuo, W. C., Chang, Y. H., Lin, C. L. & Kuo, J. S. Effects of different ceramic and dentin thicknesses on the temperature rise during photocuring. J. Dent. Sci. 6, 210–215. https://doi.org/10.1016/j.jds.2011.09.005 (2011).
Atai, M., Ahmadi, M., Babanzadeh, S. & Watts, D. C. Synthesis, characterization, shrinkage and curing kinetics of a new low-shrinkage urethane dimethacrylate monomer for dental application. Dent. Mater. 23, 1030–1041. https://doi.org/10.1016/j.dental.2007.03.004 (2007).
Watts, D. C., McAndrew, R. & Lloyd, C. H. Thermal diffusivity of composite restorative materials. J. Dent. Res. 66, 1576–1578. https://doi.org/10.1177/00220345870660101201 (1987).
Alenezi, A., Alsweed, M., Alsidrani, S. & Chrcanovic, B. R. Long-term survival and complication rates of porcelain laminate veneers in clinical studies: a systematic review. J. Clin. Med. 10, 1074. https://doi.org/10.3390/jcm10051074 (2021).
Lynch, C. D., Roberts, J. L., Al-Shehri, A., Milward, P. J. & Sloan, A. J. An ex-vivo model to determine dental pulp responses to heat and light-curing of dental restorative materials. J. Dent. 79, 11–18. https://doi.org/10.1016/j.jdent.2018.08.014 (2018).
Gross, D. J. et al. In vivo temperature rise and acute inflammatory response in anesthetized human pulp tissue of premolars having Class V preparations after exposure to Polywave® LED light curing units. Dent. Mater. 36, 1201–1213. https://doi.org/10.1016/j.dental.2020.05.015 (2020).
Kwon, S. J. et al. Thermal irritation of teeth during dental treatment procedures. Restor. Dent. Endod. 38, 105–112. https://doi.org/10.5395/rde.2013.38.3.105 (2013).
Jakubinek, M. B., O’Neill, C., Felix, C., Price, R. B. & White, M. A. Temperature excursions at the pulp-dentin junction during the curing of light-activated dental restorations. Dent. Mater. 24, 1468–1476. https://doi.org/10.1016/j.dental.2008.03.012 (2008).
Shortall, A., El-Mahy, W., Stewardson, D., Addison, O. & Palin, W. Initial fracture resistance and curing temperature rise of ten contemporary resin-based composites with increasing radiant exposure. J. Dent. 41, 455–463. https://doi.org/10.1016/j.jdent.2013.02.002 (2013).
Yazici, A. R., Muftu, A., Kugel, G. & Perry, R. D. Comparison of temperature changes in the pulp chamber induced by various light curing units, in vitro. Oper. Dent. 31, 261–265. https://doi.org/10.2341/05-26 (2006).
Kim, M. J., Kim, R. J. Y., Ferracane, J. & Lee, I. B. Thermographic analysis of the effect of composite type, layering method, and curing light on the temperature rise of photo-cured composites in tooth cavities. Dent. Mater. 33, e373-383. https://doi.org/10.1016/j.dental.2017.07.007 (2017).
Al-Qudah, A., Mitchell, C., Biagioni, P. A. & Hussey, D. L. Effect of composite shade, increment thickness and curing light on temperature rise during photocuring. J. Dent. 35, 238–245. https://doi.org/10.1016/j.jdent.2006.07.012 (2007).
Runnacles, P. et al. Comparison of in vivo and in vitro models to evaluate pulp temperature rise during exposure to a Polywave® LED light curing unit. J. Appl. Oral Sci. 27, e20180480. https://doi.org/10.1590/1678-7757-2018-0480 (2019).
Filho, A. M., Vieira, L. C. C., Araujo, E. & Baratieri, L. N. Ceramic inlays and onlays: Clinical procedures for predictable results. J. Esthet. Restor. Dent. 15, 338–351 (2003).
Opdam, N. J. M., Frankenberger, R. & Magne, P. From, “direct versus indirect” toward an integrated restorative concept in the posterior dentition. Oper. Dent. 41, S27–S34. https://doi.org/10.2341/15-126-LIT (2016).
Bueno, A. L. N., Arrais, C. A. G., Jorge, A. C. T., Reis, A. F. & Amaral, C. M. Light-activation through indirect ceramic restorations: does the overexposure compensate for the attenuation in light intensity during resin cement polymerization?. J. Appl. Oral Sci. 19, 22–27. https://doi.org/10.1590/s1678-77572011000100006 (2011).
Padam, S. Sample size for experimental studies. J. Clin. Prev. Card. 1, 88–93 (2012).
Millen, C. et al. A study of temperature rise in the pulp chamber during composite polymerization with different light curing units. J. Contemp. Dent. Pract. 8, 29–37 (2007).
Loney, R. W. & Price, R. B. T. Temperature transmission of high-output light-curing units through dentin. Oper. Dent. 26, 516–520 (2001).
Lin, M., Xu, F., Lu, T. J. & Bai, B. F. A review of heat transfer in human tooth-experimental characterization and mathematical modelling. Dent. Mater. 26, 501–513. https://doi.org/10.1016/j.dental.2010.02.009 (2010).
Raab, W. H. Temperature related changes in pulpal microcirculation. Proc. Finn. Dent. Soc. 88, 469–479 (1992).
Kodonas, K., Gogos, C. & Tziafas, D. Effect of simulated pulpal microcirculation on intrapulpal temperature changes following application of heat on tooth surfaces. Int. Endod. J. 42, 247–252. https://doi.org/10.1111/j.1365-2591.2008.01508.x (2009).
Zarpellon, D. C. et al. In vivo pulp temperature changes during class V cavity preparation and resin composite restoration in premolars. Oper. Dent. 46, 374–384. https://doi.org/10.2341/20-098-C (2021).
Hannig, M. & Bott, B. In-vitro pulp chamber temperature rise during composite resin polymerization with various light-curing sources. Dent. Mater. 15, 275–281. https://doi.org/10.1016/s0109-5641(99)00047-0 (1999).
Daronch, M., Rueggeberg, F. A., Hall, G. & De Goes, M. F. Effect of composite temperature on in vitro intrapulpal temperature rise. Dent. Mater. 23, 1283–1288. https://doi.org/10.1016/j.dental.2006.11.024 (2007).
Zarpellon, D. C. et al. Influence of Class V preparation on in vivo temperature rise in anesthetized human pulp during exposure to a Polywave ® LED light curing unit. Dent. Mater. 34, 901–909. https://doi.org/10.1016/j.dental.2018.03.003 (2018).
De Souza, G., Braga, R. R., Cesar, P. F. & Lopes, G. C. Correlation between clinical performance and degree of conversion of resin cements: A literature review. J. Appl. Oral. Sci. 23, 358–368. https://doi.org/10.1590/1678-775720140524 (2015).
Archegas, L. R. P., Caldas, D. B. M., Rached, R. N., Soares, P. & Souza, E. M. Effect of ceramic veneer opacity and exposure time on the polymerization efficiency of resin cements. Oper. Dent. 37, 281–289. https://doi.org/10.2341/11-134-L (2012).
Ilday, N. O., Bayindir, Y. Z., Bayindir, F. & Gurpinar, A. The effect of light curing units, curing time, and veneering materials on resin cement microhardness. J. Dent. Sci. 8, 141–146. https://doi.org/10.1016/j.jds.2012.09.014 (2013).
Vinagre, A. Pulp temperature rise induced by light-emitting diode light-curing units using an ex vivo model. Materials. 12, 411. https://doi.org/10.3390/ma1203041 (2019).
Mouhat, M., Mercer, J., Stangvaltaite, L. & Ortengren, U. Light-curing units used in dentistry: Factors associated with heat development-potential risk for patients. Clin. Oral. Investig. 21, 1687–1696. https://doi.org/10.1007/s00784-016-1962-5 (2017).
Ilie, N. & Hickel, R. Correlation between ceramics translucency and polymerization efficiency through ceramics. Dent. Mater. 24, 908–914. https://doi.org/10.1016/j.dental.2007.11.006 (2008)
Bandarra, S. et al. Biocompatibility of self-adhesive resin cement with fibroblast cells. J. Prosthet. Dent. 125(705), e1-7. https://doi.org/10.1016/j.prosdent.2021.01.002 (2021).
Leprince, J. G., Palin, W. M., Hadis, M., Devaux, J. & Leloup, G. Progress in dimethacrylate-based dental composite technology and curing efficiency. Dent Mater. 29, 139–156. https://doi.org/10.1016/j.dental.2012.11.005 (2013).
Ilie, N. & Stark, K. Curing behavior of high-viscosity bulk-fill composites. J. Dent. 42, 977–985. https://doi.org/10.1016/j.jdent.2014.05.012 (2014).
Tauböck, T. T., Tarle, Z., Marovic, D. & Attin, T. Pre-heating of high-viscosity bulk-fill resin composites: Effects on shrinkage force and monomer conversion. J. Dent. 43, 1358–1364. https://doi.org/10.1016/j.jdent.2015.07.014 (2015).
Emami, N. & Söderholm, K. J. How light irradiance and curing time affect monomer conversion in light-cured resin composites. Eur. J. Oral. Sci. 111, 536–542. https://doi.org/10.1111/j.0909-8836.2003.00082.x (2003).
Kilinc, E., Antonson, S. A., Hardigan, P. C. & Kesercioglu, A. The effect of ceramic restoration shade and thickness on the polymerization of light- and dual-cure resin cements. Oper. Dent. 36, 661–669. https://doi.org/10.2341/10-206-L (2011).
Kim, M. J., Kim, K. H., Kim, Y. H. & Kwon, T. Y. Degree of conversion of two dual-cured resin cements light-irradiated through zirconia ceramic disks. J. Adv. Prosthodont. 5, 464–470. https://doi.org/10.4047/jap.2013.5.4.464 (2013).
Daronch, M., Rueggeberg, F. A., Moss, L. & De Goes, M. F. Clinically relevant issues related to preheating composites. J. Esthet. Restor. Dent. 18, 340–350. https://doi.org/10.1111/j.1708-8240.2006.00046.x (2006).
Mundim, F. M. et al. Color stability, opacity and degree of conversion of preheated composites. J. Dent. 39, e25–e29. https://doi.org/10.1111/j.1708-8240.2006.00046.x (2011).
Froes-Salgado, N. R. et al. Composite pre-heating: effects on marginal adaptation, degree of conversion and mechanical properties. Dent. Mater. 26, 908–914. https://doi.org/10.1016/j.dental.2010.03.023 (2010).
Daronch, M., Rueggeberg, F. A. & De Goes, M. F. Monomer conversion of pre-heated composite. J. Dent. Res. 84, 663–667. https://doi.org/10.1177/154405910508400716 (2005).
Daronch, M., Rueggeberg, F. A., De Goes, M. F. & Giudici, R. Polymerization kinetics of pre-heated composite. J. Dent. Res. 85, 38–43. https://doi.org/10.1177/154405910608500106 (2006).
Barszczewska-Rybarek, I. M. A guide through the dental dimethacrylate polymer network structural characterization and interpretation of physico-mechanical properties. Materials. 12, 4047. https://doi.org/10.3390/ma12244057 (2019).
Sideridou, I. D. & Karabela, M. M. Effect of the amount of 3-methacryloxypropyltrimethoxysilane coupling agent on physical properties of dental resin nanocomposites. Dent. Mater. 25, 1315–1324. https://doi.org/10.1016/j.dental.2009.03.016 (2009).
Andrzejewska, P. K., Stansbury, J. W. & Bowman, C. N. Application of an addition-fragmentation-chain-transfer monomer in di(meth)acrylate network formation to reduce polymerization shrinkage stress. Polym. Chem. 8, 4339–4351. https://doi.org/10.1039/C7PY00702G (2017).
Acknowledgements
This research was funded by the Bolyai János Reasearch Scholarship (BO/713/20/5); the ÚNKP-21-5 New National Excellence Program of the Ministry for Innovation and Technology from the Source of the National Research, Development and Innovation Fund (ÚNKP-21-5-PTE-1353); PTE-ÁOK-KA-2020/24.
Funding
Open access funding provided by University of Pécs.
Author information
Authors and Affiliations
Contributions
E.L. conceptualization, methodology, software, validation, resources, writing—original draft preparation, funding acquisition; D.K. conduction of the experiment, data curation, formal analysis, project administration; D.Sz. conduction of the experiment; D.J. conduction of the experiment; B.V.L. writing—review and editing; J.Sz. visualization, supervision. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lempel, E., Kincses, D., Szebeni, D. et al. Intrapulpal temperature changes during the cementation of ceramic veneers. Sci Rep 12, 12919 (2022). https://doi.org/10.1038/s41598-022-17285-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17285-x
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.