Abstract
The aim of this study was to evaluate the real intensity level of exercise in a sample of patients with chronic disease from obesity, rheumatology, hematology and other departments involved in a hospital-based program of adapted physical activity (APA). For this cross-sectional study, we studied seventy-five patients with chronic disease and no beta-blocker treatment. They systematically performed a cardiopulmonary exercise test before participating in a supervised APA practice using a telemetry wireless system to monitor heart rate (HR) during the first session. Based upon the results of the functional evaluation of exercise performance, we studied two groups of patients: (1) No limitation in exercise performance (maximal oxygen uptake greater than or equal to 80% of the theoretical reference) and (2) limited exercise performance (maximal oxygen uptake less than 80% of the theoretical value). Fifty-two patients (69.3%) were women, mean age was 42.6 (± 13.8), and mean BMI was 36.7 (± 10.6). Most patients had been referred for obesity (57.3%). We found 39 patients with normal exercise capacities and 36 patients with limited exercise performance. There were no significant differences in demographic and clinical characteristics between the two groups. For all populations, the mean and median real intensity levels of exercise in a sample of patients were moderate (55–70% HR max) and were the same for both groups. During the most intensive 15-min bout of the APA session, the HR for patients in both groups was greater than 70% of the actual maximum HR. This study observed a moderate level of APA exercise intensity in patients suffering from various chronic diseases. We found no significant difference in intensity level of exercise between patients’ capacities, i.e., with and without limitation of their maximal performance.
Similar content being viewed by others
Introduction
Sedentary behavior and physical inactivity are major risk factors for non-communicable diseases, not only accounting for 9% of premature mortality but also leading to disability from chronic diseases and a substantial economic burden worldwide1,2,3. It has been demonstrated that active people live 3 years longer than inactive individuals4,5.
Sedentary behavior, defined as a low energy expenditure of < 1.5 metabolic equivalent units (MET) in a sitting or reclining posture during waking time, is not only the lowest end of the physical activity broad spectrum, but has also been suggested to be an independent predictor of metabolic risk1,6,7. It might be counteracted by regular moderately intensive physical activity (at least 150 min/week of physical activities where energy expenditure is between 3 and 5.9 METs)8,9.
In 2004, as a public health priority and to reduce the worldwide problems caused by the deleterious association of physical inactivity and sedentary behavior, the World Health Assembly adopted the WHO global strategy on diet, physical activity and health to promote physical activity. It also endorsed the new Global Action Plan on Physical Activity (GAPPA) 2018–2030, whose target is to reduce global levels of inactivity in adults and adolescents by about 15% by 203010,11.
The new WHO guidelines on physical activity and sedentary behavior were ratified in 2020 and, like previous recommendations, encouraged the integration of exercise counseling in clinical practice, including exercise prescription12. In that context, the American College of Sports Medicine (ACSM) launched a multinational initiative called “Exercise is Medicine” to make physical assessment and exercise prescription an integral component of disease prevention and treatment for all patients13,14,15.
In France, the promotion of physical activity was legitimized by the 2016 Health Act of the Ministry of Social affairs and Health which includes the amendment, “prescription of physical activity”, allowing physicians to prescribe physical activity to patients suffering from chronic disease16,17. In hospital settings, Adapted Physical Activity (APA) in rehabilitation is usually integrated with physiotherapy and is provided by physiotherapists in conjunction with exercise professionals holding an academic degree in APA18,19. The APA program is individualized to the patient and incorporates their physical fitness, exercise preferences, psychological aspects, and expectations. In addition, in the case of hemodialyzed patients, the introduction of APA programs in several countries has shown a positive impact but also shown that it must be included in a global and multidisciplinary approach20.
A combined aerobic exercise and resistance-training program is proposed to improve physical fitness, as well as exercises aimed to enhance flexibility and balance. The intensity of exercise should be moderate, providing roughly 55 to 70% of maximum heart rate (HR) or 3 to 5.9 METs and should not be uncomfortable for a patient21. Although APA is clearly distinct from rehabilitation, the line between both may sometimes be blurred, especially regarding the intensity of the physical activity performed during a training session.
Our main goal was to evaluate the real intensity level of exercise in a sample of patients suffering from chronic disease following a hospital-based session of the APA program, and to compare this intensity in two groups, those with and without a limitation on exercise performance capacity.
Methods
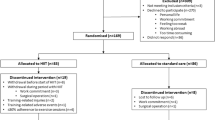
This is a cross-sectional monocentric study performed at the Nancy University Center of Sports Medicine and APA, France, between February 2020 and July 2021, in patients requiring implementation of APA. APA is a means that allows the movement of people who, due to their physical, mental, or social status, cannot perform physical activity under normal conditions. The inclusion criteria were age greater than 18 years old, with the ability to perform a cardiopulmonary exercise test and participate in supervised APA practice using a telemetry wireless system to monitor and record HR during the first session. The exclusion criteria were beta-blocker treatment and joint pain or limitations.
Demographic, clinical data and intervention
Data collected from the included patients were age, gender, and Body Mass Index (BMI). We classified the patient’s referral department categories behind the APA program into four groups: Obesity, Rheumatology, Hematology and Others. The patients' socio-professional status was also categorized: (1) executives and intermediate professions, (2) agricultural workers and artisans, (3) blue collar/manual workers (4) retirees, unemployed, others, (5) students and (6) incapacitated through ill health. A maximum cardiopulmonary exercise test was carried out on all included patients.
Following the cardiopulmonary exercise test, the sample was split into two groups22,23,24,25: (1) No limitation of exercise performance capacities: those with normal maximal oxygen uptake ([V′O2peak] greater than or equal to 80% of the reference value) and (2) limitation of exercise performance capacities defined by a reduced V′O2peak (less than 80% of the reference value). We used the Wasserman equation to determine reference values for capacities assessment22,26,27. The actual peak HR (HRpeak) was measured during the exercise test. We collected the VT1 first ventilatory threshold (VT1) in each exercise test. VT2 (second ventilatory threshold) could not be collected because it did not reach the patients.
-
Exercise test procedure: V′O2max was established during an incremental exhaustive exercise test on a cycle ergometer (eBike, GE Healthcare, France). For each patient, a progressively increasing work rate protocol was designed (rest, followed by an incremental phase of exercise every minute) so that volitional exhaustion is reached following 8–12 min of exercise. Respiratory and metabolic variables (minute-ventilation, tidal volume, frequency of breathing, V′O2, V′CO2) were measured breath-by-breath through a mask connected to a pneumotachograph and O2 and CO2 analyzers (Vyntus™ CPX, Vyaire, Germany). Criteria for the achievement of V′O2max were HR > 90% of the maximal reference value HR (220—age), respiratory exchange ratio ([RER] = V′CO2/V′O2) > 1.1 or V’O2 plateau22,23,28. The effort consisted of going up to the patient’s maximum capacity and was followed upon with a 6-min recovery phase to reach the resting state back.
The effort intensity levels are defined as such: sedentary: < 40% HR max or > 1.5METs, low: 40–55% HR max or 1,6 et 3 METs; moderate: 55 to 70% HR max or 3 and < 6 METs and high: 70 to 90% HR max or 6 to < 9 METs29.
During the APA session, HR was digitized at 1 Hz (using custo guard, Custo Med GmbH). The ratio between the APA session HR and exercise test HRpeak was used to assess the intensity of effort.
The hospital-based APA intervention
The APA program comprised two hospital-based APA interventions per week, supervised by a physiotherapist and a trained APA educator (exercise professionals). The typical session lasted 60 min with 20 min of constant aerobic effort on an ergocycle at a comfortable intensity level. Subsequently, a 20-min body weight reinforcement session, consisting of 1-min effort followed by 1–2-min recovery phases were performed. At the end of the session, a 10-min stretching time was planned. The intensity was individually set to correspond to moderate exercise (55 to 70% of maximum heart rate (HR), 3 to 5.9 és), where participants reached a comfortable level of exercise, following the speech rule which defined the maximum perceived exertion. The program was organized in two stages: 10 to 15 min of aerobic activity for warm-up then 30 min of strengthening activity in interval training of a maximum of 6 sets of a maximum of one minute.
Statistical analysis
Both descriptive and comparative analyses were made by accounting for the nature and distribution of the variables. Qualitative variables were described as frequencies and percentages; quantitative variables were evaluated using the mean ± standard deviation (SD) or with the median and interquartile range (IQR). The chi-square test or Fisher’s exact test with, if necessary, the exact calculation of Fisher, was used for the ordinal or nominal data analysis. We use the student T test to compare age, BMI, HR. The significance level was set at 0.05 for the entire study. IBM SPSS Statistics 23.0 was used for the data analysis.
Ethics and dissemination
All data used were obtained from the medical records. No supplementary examination was necessary for patients to meet the inclusion criteria. This study is registered with the Information Technology and Freedoms Commission for the University Hospital of Nancy (file number: 2021PI191) and on Clinicaltrials.gov (NCT05146544) and was designed in accordance with the general ethical principles outlined in the Declaration of Helsinki. This study has received approval from the French Ethics Committee (Comité d’éthique CHRU de Nancy, saisine n°336 01/12/2021). Informed consent was obtained from all subjects and their legal guardians. All patients gave their consent for the use of their medical data during the period they received medical care at the University Hospital.
Results
Seventy-five patients were included, 69.3% (n = 52) were women, mean age was 42.6 (± 13.8) and mean BMI was 36.7 (± 10.6) Kg/m2. Most patients were obese (57.3%) or had rheumatological disease (13.3%). Blue-collar/manual workers, executives/intermediate positions and retirees formed 56.0%, 18.7% and 16.0%, respectively, of the sample. Mean of HRpeak and V′O2peak were 153.9 (20.9) bpm and 17.2 (4.9) mL/min/kg respectively. HRpeak is about 87.0% of age predicted HRmax. Sixty-seven patients had RER greater than or equal to 1. Among this sample, fifty patients achieved VO2max. We categorized 39 (52.0%) and 36 (48.0%) of patients as having no limited (greater than or equal to 80% of the reference value) or limited (less than 80% of the reference value) exercise performance, respectively. There were no significant differences between the two categories for demographic and clinical characteristics (Table 1).
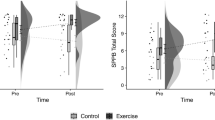
The 60-min APA session HR average was 105.3 (± 16.6) bpm which represents 69.2% of HRmax. There was a significant difference between the most intense 30 min, which was 105.2 (± 17.5) bpm represent 69.1% and the most intense 15 min, which was 115.5 (± 19.4) bpm, which represents 75.8% of HRpeak (p < 0.001). We observed higher HR in patients with limited exercise performance with HR over 115.6 (± 20.3) bpm, representing 77.8% of HRpeak over the most critical 15 min (p = 0.996). However, we found no significant difference between patients with normal and those with limited exercise performance in the three periods overall (Table 2).
Discussion
The mean and median real intensity level of exercise of hospital-based sessions of APA in a sample of patients was moderate (69.2% of maximal capacity). Only the most intensive 15 min produced an intensified level (75.8% of maximal capacity). In our sample of patients suffering from different chronic diseases, we found no significant statistical difference in maximal intensity during hospital-based APA sessions between subjects with and without performance limitation.
In theory, the maximal level of exertion for moderate physical activity corresponded to a comfortable effort completely in the group without any cardiopulmonary limitation, but the level of exercise for APA slightly exceeded the conventional target of 55–69% of HRpeak, achieving moderate exercise in performance limited patients (Table 2).
These results emphasize the need for precautionary functional assessment of cardiopulmonary fitness in fragile chronic disease patients prior to any exercise prescription since acute, vigorously intense exercise is well known to increase cardiovascular events30. Nevertheless, in order to include them in the global healthcare approach and get them supported, it is essential to recognize the role of exercise professionals. Our results therefore highlight the key role of healthcare professionals, not only to promote regular physical activity in patients but also to rigorously assess their health status. Indeed, based on accurate identification of specific groups of patients, taking into account patient preferences, and providing written physical activity programs, public health policy regarding physical activity on prescription has been shown to be effective in increasing the level of physical exercise in patients31,32. Throughout patient care, and in order to support a change to a more autonomously active and less sedentary lifestyle, healthcare professionals generally focus on patient-centred dialog, individually tailored physical activity recommendations with a written prescription, and follow-up. Because of the increased levels of stress during physical exercise, our results support the idea that healthcare professionals should meticulously evaluate the patient’s health status. This will undoubtedly enhance the effectiveness of the 2018–2030 WHO GAPPA slogan—“More active people for a healthier world”.
To reduce the potential risk of injury, elderly or debilitated patients should receive moderate intensity exercise prescription in preference to ideally moderate physical activity. It could be explained by a physiologic aging reduction induced by a regular practice. Ekelund et al. have recently demonstrated a dose–response association between reducing substantial risk and mildly intensive physical activity33. As previously noted by Blair et al., “a little is better than none” is an important public health message in the promotion of health-enhancing physical activity34. Moreover, a higher level of total physical activity, regardless of intensity level, associated with less time spent sedentary, decreases the risk of premature mortality33. In heart failure patients with preserved ejection fraction, high intensity interval training or continuous moderate training did not change peak oxygen uptake compared to control of guideline-based physical activity35. In the peculiar context of fragile or elderly patients, the interest of resistance training needs to be highlighted. Indeed, the benefical role of strength training in the reduction of falls in the elderly has been demonstrated, and has been more recently observed to lower mortality, with an additive effect when combined with dynamic exercise36,37,38.
This study has limitations. Firstly, the size sample prevents any extension of the results. In fact, the study was performed in a small sample (n = 75) practicing APA in a single hospital center. In addition, the presence of a large number of obese participants limited a subgroup exploration of different chronic pathologies. Therefore, although HR is the most convenient variable for evaluating the intensity in ecologic condition, it presents limitations. In fact, it is subject to numerous artefacts and the HR curve is influenced by age, gender, and performance39.
The main strength of this study is its originality, as we could record the actual practice intensity in APA sessions from physiological data recorded. We use for this study incremental exercise test and the ability to individual capacities. Indeed, VO2max as a gold standard to assess the functional capacities of patients. This study also incorporates all the recommendations of the Health Act of the Ministry of Social Affairs and Health.
In conclusion, our study explored a high level of exercise intensity (> 70% of HRpeak in exercise tests) in patients suffering from different chronic diseases, with and without performance limitation. Our results emphasize that training at the perceived exertion level could produce an efficient level of exercise to improve health. However, an analysis of a larger population in a longitudinal study would make this observation more explicit. This would also open up the possibility of creating personalized programs appropriate to the health status of the patient so that medical risk can be evaluated and an appropriate safe exercise program developed.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- APA:
-
Adapted physical activity
- BMI:
-
Body mass index
- HR:
-
Heart rate
- HRpeak:
-
Peak heart rate
- IQR:
-
Interquartile range
- RER:
-
Respiratory exchange ratio
- SD:
-
Standard deviation
- V′O2max:
-
Maximal oxygen uptake
- V′O2peak:
-
Oxygen uptake peak
- VT1:
-
First ventilatory threshold
References
Booth, F. W., Roberts, C. K., Thyfault, J. P., Ruegsegger, G. N. & Toedebusch, R. G. Role of inactivity in chronic diseases: Evolutionary insight and pathophysiological mechanisms. Physiol. Rev. 97, 1351–1402 (2017).
Lee, I.-M. et al. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 380, 219–229 (2012).
Ding, D. et al. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. The Lancet 388, 1311–1324 (2016).
Wen, C. P. et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. The Lancet 378, 1244–1253 (2011).
Lear, S. A. et al. The effect of physical activity on mortality and cardiovascular disease in 130,000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet 390, 2643–2654 (2017).
SBRN Terminology Consensus Project Participants et al. Sedentary behavior research network (SBRN): Terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 14, 75 (2017).
Wilmot, E. G. et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia 55, 2895–2905 (2012).
Ekelund, U. et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. The Lancet 388, 1302–1310 (2016).
Stamatakis, E. et al. Sitting time, physical activity, and risk of mortality in adults. J. Am. Coll. Cardiol. 73, 2062–2072 (2019).
World Health Organization. More Active People for a Healthier World: Global Action Plan on Physical Activity 2018–2030 (World Health Organization, 2018).
World Health Organization. Diet and Physical Activity: A Public Health Priority (World Health Organization, 2004).
World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance (World Health Organization, 2020).
Garber, C. E. et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 43, 1334–1359 (2011).
Lobelo, F., Stoutenberg, M. & Hutber, A. the exercise is medicine global health initiative: A 2014 update. Br. J. Sports Med. 48, 1627–1633 (2014).
Sallis, R. Exercise is medicine: A call to action for physicians to assess and prescribe exercise. Phys. Sportsmed. 43, 22–26 (2015).
Rivière, D. Medical prescription of physical activity. Rev. Pract. 70, 279–285 (2020).
Loi n°2016–41, art. L. 144 du 26 janvier 2016 de modernisation de notre système de santé (J.O. 27 Janvier, 2016).
Hutzler, Y. & Sherrill, C. Defining adapted physical activity: International perspectives. Adapt. Phys. Activ. Q. 24, 1–20 (2007).
Hutzler, Y. S. Evidence-based practice and research: A challenge to the development of adapted physical activity. Adapt. Phys. Activ. Q 28, 189–209 (2011).
Viana, J. L. et al. Sustained exercise programs for hemodialysis patients: The characteristics of successful approaches in Portugal, Canada, Mexico, and Germany. Semin. Dial. 32, 320–330 (2019).
Haseler, C., Crooke, R. & Haseler, T. Promoting physical activity to patients. BMJ 1, 5230. https://doi.org/10.1136/bmj.l5230 (2019).
American Thoracic Society & American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am. J. Respir. Crit. Care Med. 167, 211–277 (2003).
Pedersen, B. K. & Saltin, B. Exercise as medicine: Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 25, 1–72 (2015).
Carré, F. Cardiopulmonary exercise test for cardiologists. Lett. Cardiol. 22, 1–10 (2016).
Shvartz, E. & Reibold, R. C. Aerobic fitness norms for males and females aged 6 to 75 years: A review. Aviat. Space Environ. Med. 61, 3–11 (1990).
Radtke, T. et al. ERS statement on standardisation of cardiopulmonary exercise testing in chronic lung diseases. Eur. Respir. Rev. 28, 180101 (2019).
Clinical Exercise Testing with Reference to Lung Diseases. indications, standardization and interpretation strategies. Eur. Respir. J. 10, 2662–2689 (1997).
Metz, L. et al. A new equation based on the 6-min walking test to predict VO 2peak in women with obesity. Disabil. Rehabil. 40, 1702–1707 (2018).
Barthélémy, J.-C. et al. Actualisation des Repères du PNNS: Révisions des Repères Relatifs à l’Activité Physique et à la Sédentarité. ([Rapport de recherche] Agence nationale de sécurité sanitaire de l’alimentation, de l’environnement et du travail (ANSES, 2016).
Eijsvogels, T. M. H., Molossi, S., Lee, D., Emery, M. S. & Thompson, P. D. Exercise at the extremes. J. Am. Coll. Cardiol. 67, 316–329 (2016).
Onerup, A. et al. Physical activity on prescription in accordance with the Swedish model increases physical activity: A systematic review. Br. J. Sports Med. 53, 383–388 (2019).
Arsenijevic, J. & Groot, W. Physical activity on prescription schemes (PARS): Do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses. BMJ Open 7, e012156 (2017).
Ekelund, U. et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ 1, 4570. https://doi.org/10.1136/bmj.l4570 (2019).
Blair, S. N., Kohl, H. W., Gordon, N. F. & Paffenbarger, R. S. How much physical activity is good for health?. Annu. Rev. Public Health 13, 99–126 (1992).
Mueller, S. et al. Effect of high-intensity interval training, moderate continuous training, or guideline-based physical activity advice on peak oxygen consumption in patients with heart failure with preserved ejection fraction: A randomized clinical trial. JAMA 325, 542–551 (2021).
Hurley, B. F. & Roth, S. M. Strength training in the elderly: Effects on risk factors for age-related diseases. Sports Med. 30, 249–268 (2000).
Karlsson, M. K., Vonschewelov, T., Karlsson, C., Cöster, M. & Rosengen, B. E. Prevention of falls in the elderly: A review. Scand. J. Public Health 41, 442–454 (2013).
Saeidifard, F. et al. The association of resistance training with mortality: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 26, 1647–1665 (2019).
Birnbaumer, P. et al. Heart rate performance curve is dependent on age, sex, and performance. Front. Public Health 8, 98 (2020).
Acknowledgements
The sponsor was CHRU de Nancy (Direction de la Recherche et de l’Innovation).
Author information
Authors and Affiliations
Contributions
Ed.A. and B.C. had the original idea. Ed.A., B.C. and El.A. designed and conceived the protocol. E.A., B.C., and G.G. drafted the manuscript. Ed.A., B.C., G.G., El.A., A.M., M.T., O.H., M.P., J.P. and N.B. critically revised the manuscript for methodology and intellectual content. All authors approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Allado, E., Poussel, M., Albuisson, E. et al. Real intensity of physical activity capacity of patients with chronic disease: a cross-sectional study. Sci Rep 12, 12593 (2022). https://doi.org/10.1038/s41598-022-17047-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17047-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.