Abstract
As a marker of hypercoagulability, plasma D-dimer is associated with progression of many cancers but remains controversial in gastric cancer (GC). We aim to investigate the predictive value of D-dimer for postoperative outcomes after radical gastrectomy of GC patients. We enrolled 903 consecutive patients with GC who underwent radical gastrectomy and the clinicopathological characteristics were compared. Risk factors for overall survival (OS) and disease-free survival (DFS) were determined using multivariate cox regression analysis. We also compared the survival difference based on Kaplan–Meier method after a one-to-one propensity score matching (PSM). Patients with elevated D-dimer had older age (p < 0.001), advanced TNM stage (p < 0.001), larger tumor size (p = 0.005), lower 5-year OS rate (32.8% vs 62.6%, p < 0.001) and DFS (29% vs 59.6%, p < 0.001). In multivariate analysis, elevated D-dimer was independently associated with shorter OS [hazard ratio (HR): 1.633, 95% confidence interval (CI) 1.178–2.264, p = 0.003] and DFS (HR: 1.58, 95% CI 1.151–2.169, P = 0.005). After PSM, the 5-year OS rate of patients with elevated D-dimer was still significantly lower than matched group (32.8% vs 40.6%, p = 0.005), so was DFS (29% vs 36.6%, p = 0.008). Preoperative elevated D-dimer is an independent risk factor for GC patients undergoing curative gastrectomy.
Similar content being viewed by others
Introduction
As a global health threat, approximately one million people worldwide are newly diagnosed with gastric cancer each year. Gastric cancer remains the fifth most frequently diagnosed disease and the third leading cause of cancer-related death, despite a decline in morbidity and mortality worldwide over the past 50 years1. An estimated 4.3 million new cancer cases and 2.9 million new cancer deaths occurred in China in 20182.Gastric cancer is the second leading cause of cancer death in men and women in China. An estimated 679,100 new cases of gastric cancer are diagnosed in China each year3. As more than 80% of patients diagnosed at an advanced stage, 5-year survival rate of gastric cancer still remains very low4.
Hypercoagulability is frequently observed in several tumors, which not only closely related to thrombosis, but also associated with tumor progression. D-dimer, as a degradation product of fibrin, is produced when cross-linked fibrin is degraded by plasmin induced fibrinolytic activity. D-dimer have been used as a screening and diagnostic tool in numerous coagulopathies and thrombotic disease. To date, a growing number of reports have demonstrated that hemostatic abnormalities are closely related to cancer5, such as lung6,7, breast8,9, esophageal10, colorectal11, and gastric cancer12. Many studies confirmed that high D-dimer levels may predict poor outcomes for GC patients13,14,15,16. Consistently, our previous research showed that D-dimer is not only an indicator of venous thrombosis but also a marker for predicting cancer progression in GC patients17. In contrast, Liang et al. reported that elevated preoperative D-dimer was not an independent prognostic factor for GC based on propensity score matching analysis18. Based on this controversy, the aim of our study was to explore the correlation between preoperative D-dimer and long-term survival of GC patients after curative surgery. In order to improve credibility, we collected data from three medical centers. Taking into consideration that baseline characteristics may influence the accuracy of prognostic analysis of D-dimer, we conduct analysis on both whole series and matching series based on COX proportional hazard model and propensity score method, respectively.
Results
Demographic and clinicopathological features of two patient groups before PSM
We retrospectively enrolled 1771 consecutive cases and 903 remained for analysis after excluding 868 patients according to exclusion criteria (18 cases of gastric stump cancer, 12 cases with D-dimer data missing, 435 cases at stage IV, 20 cases treated with palliative surgery, 5 cases treated with exploratory laparotomy, 44 cases with R1 resection, 48 cases treated with neoadjuvant chemotherapy before surgery, 86 cases concurrent with thrombotic disease, 113 patients refused to surgical treatment and 87 cases lost to follow-up) (Fig. 1). Among all patients, 687 were (76.1%) men and 290 (32.1%) patients were over 65 years old. To assess the relationship between hypercoagulability and disease progression, the whole series were divided into NDG group (D-dimer < 1 mg/l, n = 742) and EDG group (D-dimer ≥ 1 mg/l, n = 161) according to the upper limit of normal value of clinical reference of D-dimer. Patients in EDG had a higher proportion of female (30.4% vs 22.5%, p = 0.041), higher INR(median: 1.03 vs 1.02, p = 0.012), FIB (median: 3.44 g/l vs 3.12 g/l, p < 0.001), FDP (median: 3.2 mg/l vs 0.9 mg/l, p < 0.001), more advanced TNM stage (p < 0.001), higher LNR (median: 0.21 vs 0.05, p < 0.001), larger tumor size (median: 4.5 cm vs 4 cm, p = 0.005), shorter OS (median: 19 months vs 39 months, p < 0.001) and shorter DFS (median: 18.5 months vs 39 months, p < 0.001) (Table 1). No significant difference was found in PT, PTA, PTR, TT, APTT, tumor location and histology. Correlations of D-dimer and other clinicopathologic features was listed. Spearman correlation analysis demonstrated a greatly relationship between plasma D-dimer and age (P < 0.001), tumor size (P = 0.002), T stage (P = 0.001), N stage (< 0.001) and TNM stage (P < 0.001) (see Supplementary Table S1 online).
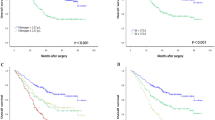
Plasma D-dimer is an independent risk factor for GC survival
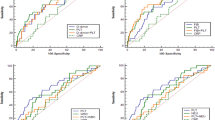
The optimal cutoff value of PT, PTA, PTR, INR, APTT, TT, FIB, D-dimer and FDP determined by ROC analysis was 13.2, 102.6, 1, 0.96, 38.9, 16.5, 3.8, 1 and 2.1, respectively (Supplementary Table S2, Supplementary Fig. 1–3). In univariate COX regression analysis, elder age, distal stomach (proximal stomach for reference), higher coagulation indicators (PTA, INR, TT, FIB, D-dimer and FDP), higher LNR, larger tumor size and advanced TNM stage were significantly associated with shorter OS. In multivariate analysis, age (HR: 1.918, 95% CI 1.436–2.561, P < 0.001), D-dimer (HR: 1.633, 95% CI 1.178–2.264, P = 0.003), LNR (HR: 4.707, 95% CI 2.886–7.677, P < 0.001), tumor size (HR: 1.085, 95% CI 1.032–1.141, P = 0.002), adjuvant chemotherapy (HR: 0.42, CI%: 0.286–0.615, P < 0.001) and TNM stage (TNM II stage: HR: 4.063, 95% CI 1.897–8.705, P = 0.001, TNM III stage: HR: 9.296, 95% CI 4.669–18.51, P < 0.001) were independent prognostic factors for OS (Table 2). The 5-year OS rate in EDG was markedly lower than in NDG (32.8% vs 62.6%, p < 0.001) (Fig. 2A). Independently prognostic factors for DFS were the same as for OS: age (HR:1.914, 95% CI 1.448–2.531, P < 0.001), D-dimer (HR: 1.58, 95% CI 1.151–2.169, P = 0.005), LNR (HR: 4.865, 95% CI 3.037–7.793, P < 0.001), tumor size (HR: 1.084, 95% CI 1.034–1.141, P = 0.001), chemotherapy (HR: 0.434, CI%: 0.3–0.63, P < 0.001) and TNM stage (TNM II stage: HR: 3.615, 95% CI 1.792–7.293, P < 0.001, TNM III stage: HR: 7.803, 95% CI, 4.136–14.722, P < 0.001) (see Supplementary Table S3 online). Significant difference was found between NDG and EDG for 5-year DFS rate (29% vs 59.6%, p < 0.001) (Fig. 3A).
Survival analysis of two patient groups after PSM
To eliminate the influence of other covariates on D-dimer prognostic analysis, PSM using a one-to-one nearest neighbor matching method was implemented. After matching, 161 patients in NDG were matched to EDG after adjusting age, gender, TNM stage, tumor location and histology (Fig. 1). There was no significant difference in gender, age, PTA, PTR, INR, TT, APTT, TNM stage, histology and LNR in matched series. Patients in EDG still had shorter OS (median: 19 months vs 25 months, p = 0.005) and shorter DFS (median: 18.5 months vs 24 months, p = 0.007) (Table 3). To our surprise, Spearman correlation analysis indicated a relationship between D-dimer and tumor size (P = 0.002) and N stage (0.011) (see Supplementary Table S4 online). Whereas age (P = 0.053), T stage (P = 0.117) and TNM stage (P = 0.056) showed no correlation with D-dimer. After PSM, the 5-year OS rate in EDG was still shorter than in NDG (32.8% vs 40.6%, p = 0.005) (Fig. 2B), so was DFS (29% vs 36.6%, p = 0.008) (Fig. 3B).
Discussion
In our present study, we investigated the prognostic value of plasma D-dimer for long term survival of GC patients with radical gastrectomy. Our findings indicated that elevated plasma D-dimer was independently associated with poorer OS and DFS. Preoperative D-dimer may provide clinicians with convenient and inexpensive clinical decision-making guidance for patients undergoing radical gastrectomy.
Patients with tumor load are often in a hypercoagulable state. Tumor progression and hypercoagulable state complement each other. Domenico Russo et al. reported that tumor cells as well as host cells which are influenced by local cancer-related inflammatory response express high level of tissue factors (TF) which in turn promoted hypercoagulation19. Consistently, Guangjun Nie et al. elucidated that targeting tumor-specific TF remarkably suppress hypercoagulable state20. Hypercoagulable state not only increases the risk of thrombotic disease but also promotes tumor progression. Tumor cells promote hypercoagulability through complex mechanisms and then promote self-progress through hypercoagulation. In fact, the risk of a venous thromboembolism is 4- to sevenfold higher in patients with cancer than in those without which is known as Trousseau's syndrome21. As part of the coagulation pathway, the platelet/fibrin (ogen) axis has been shown to promote metastasis by preventing natural killer (NK) cells from clearing newly formed micrometastases22. Specific thrombin inhibitors, or genetically-mediated decrease in prothrombin expression, significantly limit metastasis23. This confirms that tumor progression and hypercoagulability are mutually reinforcing. Recent studies have shown that long-term anticoagulation with warfarin is strongly associated with reduced incidence of various cancers24. Therefore, we inferred that the level of coagulation markers may reflect the progress of the tumor. D-dimer is produced when cross-linked fibrin is degraded by plasmin induced fibrinolytic activity. Studies about D-dimer and GC prognosis have been undertaken in many tumor diseases11,17. Cihan Ay et al. illuminated that high D-dimer levels were associated with poor OS and increased mortality risk in cancer patients25. Long Liu et al. reported that high D-dimer level may predict poor outcome of GC patients14. Controversially, Yuexiang Liang et al. illuminated that preoperative D-dimer was not an independent prognostic factor for patients with GC after curative resection18. Although the difference in research results may be due to regional differences in distribution and the influence of confounding factors, it is significant to explore the prognostic value of D-dimer in GC.
Our previous studies focused on the effect of D-dimer on short-term survival in GC patients and our current research reviewed 907 GC patients with radical gastrectomy and followed them up for up to 10 years. To detect possible confounding factors, we conducted multivariate analysis and found that elevated plasma D-dimer was an independent risk factor for OS and DFS. To eliminate the influence of interference factors on survival analysis, we performed PSM analysis to adjust age, gender, TNM stage, tumor location and histology. After PSM, the difference of age, gender, TNM stage, and histology were no longer significant but the difference of 5-year OS rate between two groups still remained (EDG vs NDG: 32.8% vs 40.6%, p = 0.005). The 5-year DFS rate of NDG (36.6%) was also significantly higher than EDG (29%) (P = 0.008). This revealed that D-dimer may not only be a marker of coagulation and but also a marker of GC progression. Cancer-associated coagulation disorder is often accompanied by thrombocytosis, hyperfibrinogenemia and D-dimer elevation. It was reported that preoperative hyperfibrinogenemia was an unfavorable prognostic factor for OS in patients with GC15. However, our results demonstrated that fibrinogen is not an independent prognostic factor for GC. As one of the hallmarks of hypercoagulable state, it is not surprising that fibrinogen is associated with tumor progression. However, after balancing other coagulation indicators, we found that only elevated D-dimer was an independent risk factor for GC. Some studies have reported that thrombocytosis functioned as an independent prognostic factor for GC patients26,27,28. In general, the interaction between the coagulation system and tumor cells is closely related to thrombosis and tumor progression. Elevated levels of circulating TF have been reported in tumor patients. TF-mediated thrombin generation mediates platelet activation that is crucial for hypercoagulation in malignancy29. Platelets contain both pro- and antiangiogenic factors, but platelets and platelet adhesion support angiogenesis30. Because platelets secrete factors including matrix metalloproteinases, platelet factor 4 and VEGF, tumors may use the proangiogenic properties of platelets for the formation of new blood vessels, supporting the migration and the activation of endothelial cells31. However, we did not find an association between platelets and gastric cancer survival. Tumor promotes hypercoagulable state through procoagulant substances. While a procoagulant milieu supports tumor immune escape and interferes with immune therapy32. It seems that anticoagulation therapy may has a positive effect on tumors. In fact, Low-molecular-weight heparin (LMWH) can prolong survival in cancer patients with or without deep vein thrombosis33. The risk of venous thromboembolism (VTE) in cancer patients is significantly higher than that in normal people. For cancer-associated VTE, full-dose oral Xa inhibitors have better efficacy than LMWH 34. In other words, anticoagulation therapy can not only inhibit tumor progression, but also reduce the risk of tumor-related thrombotic diseases. However, LMWH may have some benefit in limiting cancer progression, but this benefit appears to depend on cancer type, cancer stage, and the specific formulation of LMWH35. Moreover, the anticoagulation strategies of tumor patients in different periods and how to synergize with traditional treatment methods need to be further studied. Whether D-dimer can be used as a marker of therapeutic effect also need to be explored.
Retrospective nature was one limitation of our study. Although we enrolled clinical data from three tertiary referral centers, but they are located in northwest China, which may cause bias. On the other hand, the effect of postoperative radiotherapy on survival analysis was not taken into consideration in this study.
Conclusions
Elevated preoperative D-dimer levels is closely associated with older age, advanced clinical pathological stage, larger tumor size and more lymph node metastasis. It’s also identified as an independent prognostic factor for GC patients after radical gastrectomy.
Materials and methods
Patients
We retrospectively enrolled 903 GC patients who underwent radical gastrectomy between January 2009 and February 2017. Disease clinical staging (I-IV) depended on the eighth edition systems recommended by American Joint Committee on Cancer (AJCC). Patients follow up data were obtained by regular follow-up. The date of final follow-up was in June 2021. The interval between the dates of radical surgery and either the time of the last follow-up or the time of death was defined as OS, between the dates of radical survival and either the time of the last follow-up or the time of relapse was defined as DFS. For OS, the endpoint event was any cause of death. For DFS, the endpoint event was disease recurrence, death or secondary tumor. Censoring meant that no endpoint event was observed at the last follow-up. Inclusion criteria: (1) all patients were newly diagnosed with GC; (2) all patients were pathologically diagnosed; (3) all patients had pre-treatment coagulation test; (4) stage I-III disease; (5) age ≥ 18 years; (6) Radical treatment and R0 resection. Exclusion criteria: (1) accompanying or secondary to other tumors; (2) had history of venous thrombosis or received any anti-coagulation treatment; (3) acute infection or diffuse intravascular coagulation; (4) pregnancy or lactation; (5) history of neoadjuvant chemotherapy; (6) Lost to follow-up. Pre-treatment coagulation indicators was those closest to the time of treatment. This study was approved by the Ethics Committee of First Affiliated Hospital of Xi'an Jiaotong University. Informed consent was obtained from all subjects and/or their legal guardian(s). All methods were performed in accordance with the relevant guidelines and regulations.
Coagulation index assay
Venous blood was collected in sodium citrate tubes. The levels of FIB, FDP and D-dimer were analyzed by latex-enhanced immunoturbidimetric assay. All the samples were collected before any treatments. The normal level of FIB, D-Dimer and FDP in human plasma is less than 4.0 g/l, 1.0 mg/l and 5.0 mg/l, respectively.
Evaluation of baseline characteristics
We collected gender, age at surgery, pre-treatment laboratory test [including prothrombin time (PT), prothrombin activity (PTA), prothrombin ratio (PTR), activated partial prothrombin time (APTT), international normalized ratio (INR), thrombin time (TT), fibrinogen (FIB), D-dimer, fibrin degradation products (FDP)], T stage, N stage, Tumor-node-metastasis (TNM) stage, histology, OS, DFS, lymph nodes retrieval and tumor size. Lymph node ratio (LNR) was calculated by dividing the number of positive lymph nodes by the number of resected lymph nodes. We focused on the effect of hypercoagulability on tumor, so we set the upper limit of normal range of coagulation parameters as the cut-point. We classified tumors into two groups based on histology: undifferentiated type (including undifferentiated or poorly differentiated adenocarcinoma, mucinous carcinoma and signet ring cell carcinoma), differentiated type (including well or moderately differentiated adenocarcinoma).
Statistical analysis
The optimal cutoff vale of parameters was obtained by receiver operating characteristic curve (ROC). The cutoff value of age was set to 65 years. Cases were divided into normal D-dimer group (NDG) and elevated D-dimer group (EDG) based on cutoff value. Categorical variates were presented as frequencies and percentages and compared using the chi-square test or Fisher exact test. Continuous non-normal variates were presented as the median and interquartile range (IQR) and compared with log-rank tests, while continuous normally distributed variates were presented as mean and standard deviation and compared by Student's t-tests. Differences of OS and DFS were assessed by the log-rank test and visualized using the Kaplan–Meier method. We divided age, PT, PTA, PTR, INR, APTT, TT, FIB, D-dimer and FDP into two groups based on cutoff values. Then independent factors of OS and DFS was determined by multivariate Cox regression analyses and assessed by the Wald test. Variates with P < 0.05 in univariate analysis were included in multivariate analysis. To eliminate the influence of potential confounders on survival analysis, PSM analysis was performed by a one-to-one nearest neighbor matching method. Match tolerance was set to 0.02. The matching factor involved in the propensity model was age, gender, TNM stage, tumor location and histology.
Statistical analysis and plotting were performed with SPSS Statistics (version 22.0, IL, USA), GraphPad Prism v.8.0.1 (La Jolla, CA, USA). X-tile 3.6.1 software36 (Yale University, New Haven, CT, USA). 2-sided p < 0.05 were considered statistical significantly.
Data availability
The data generated in this study are available upon request from the corresponding author.
References
Thrift, A. & El-Serag, H. Burden of Gastric Cancer. Clin. Gastroenterol. Hepatol. 18, 534–542 (2020).
Feng, R., Zong, Y., Cao, S. & Xu, R. Current cancer situation in China: good or bad news from the 2018 Global Cancer Statistics?. Cancer Commun. (Lond). 39, 22 (2019).
Chen, W. et al. Cancer statistics in China, 2015. CA Cancer J. Clin. 66, 115–132 (2016).
Zong, L., Abe, M., Seto, Y. & Ji, J. The challenge of screening for early gastric cancer in China. Lancet 388, 2606 (2016).
Edwards, R. et al. Abnormalities of blood coagulation tests in patients with cancer. Am. J. Clin. Pathol. 88, 596–602 (1987).
Altiay, G. et al. High plasma D-dimer level is associated with decreased survival in patients with lung cancer. Clin. Oncol. (R Coll. Radiol.). 19, 494–498 (2007).
Unsal, E., Atalay, F., Atikcan, S. & Yilmaz, A. Prognostic significance of hemostatic parameters in patients with lung cancer. Respir. Med. 98, 93–98 (2004).
Yigit, E. et al. Relation between hemostatic parameters and prognostic/predictive factors in breast cancer. Eur. J. Intern Med. 19, 602–607 (2008).
Blackwell, K. et al. Plasma D-dimer levels in operable breast cancer patients correlate with clinical stage and axillary lymph node status. J. Clin. Oncol. 18, 600–608 (2000).
Diao, D. et al. Prognostic value of the D-dimer test in oesophageal cancer during the perioperative period. J. Surg. Oncol. 108, 34–41 (2013).
Blackwell, K. et al. Circulating D-dimer levels are better predictors of overall survival and disease progression than carcinoembryonic antigen levels in patients with metastatic colorectal carcinoma. Cancer 101, 77–82 (2004).
Tas, F. et al. Clinical and prognostic significance of coagulation assays in gastric cancer. J. Gastrointest. Cancer. 44, 285–292 (2013).
Go, S. et al. D-dimer can serve as a prognostic and predictive biomarker for metastatic gastric cancer treated by chemotherapy. Medicine (Baltimore) 94, e951 (2015).
Liu, L. et al. Elevated plasma D-dimer levels correlate with long term survival of gastric cancer patients. PLoS ONE 9, e90547 (2014).
Suzuki, T. et al. Hyperfibrinogenemia is associated with inflammatory mediators and poor prognosis in patients with gastric cancer. Surg. Today. 46, 1394–1401 (2016).
Dai, H. et al. D-dimer as a potential clinical marker for predicting metastasis and progression in cancer. Biomed. Rep. 9, 453–457 (2018).
Diao, D. et al. D-dimer: not just an indicator of venous thrombosis but a predictor of asymptomatic hematogenous metastasis in gastric cancer patients. PLoS ONE 9, e101125 (2014).
Liang, Y. et al. Elevated preoperative plasma D-dimer dose not adversely affect survival of gastric cancer after gastrectomy with curative intent: A propensity score analysis. Chin. J. Cancer Res. 30, 254–262 (2018).
Falanga, A., Schieppati, F. & Russo, D. Cancer tissue procoagulant mechanisms and the hypercoagulable state of patients with cancer. Semin. Thromb. Hemost. 41, 756–764 (2015).
Liu, S. et al. Tumor-specific silencing of tissue factor suppresses metastasis and prevents cancer-associated hypercoagulability. Nano Lett. 19, 4721–4730 (2019).
Ikushima, S. et al. Trousseau’s syndrome: Cancer-associated thrombosis. Jpn. J. Clin. Oncol. 46, 204–208 (2016).
Palumbo, J. et al. Platelets and fibrin(ogen) increase metastatic potential by impeding natural killer cell-mediated elimination of tumor cells. Blood 105, 178–185 (2005).
Wojtukiewicz, M. Z., Hempel, D., Sierko, E., Tucker, S. C. & Honn, K. V. Thrombin-unique coagulation system protein with multifaceted impacts on cancer and metastasis. Cancer Metastasis. Rev. 35, 213–233 (2016).
Haaland, G. S., Falk, R. S., Straume, O. & Lorens, J. B. Association of Warfarin use with lower overall cancer incidence among patients older than 50 years. JAMA Intern. Med. 177, 1774–1780 (2017).
Ay, C. et al. High D-dimer levels are associated with poor prognosis in cancer patients. Haematologica 97, 1158–1164 (2012).
Oh, S. et al. Prognostic impact of increased perioperative platelet count in gastric cancer patients. J. Surg. Res. 242, 296–303 (2019).
Hu, C. et al. Thrombocytosis is a significant indictor of hypercoagulability, prognosis and recurrence in gastric cancer. Exp. Ther. Med. 8, 125–132 (2014).
Shoda, K. et al. Thrombocytosis associated with poor prognosis in patients with gastric cancer. Gan To Kagaku Ryoho 42, 1980–1982 (2015).
Rondon, A. M. R., Kroone, C., Kapteijn, M. Y., Versteeg, H. H. & Buijs, J. T. Role of tissue factor in tumor progression and cancer-associated thrombosis. Semin Thromb Hemost. 45, 396–412 (2019).
Kisucka, J. et al. Platelets and platelet adhesion support angiogenesis while preventing excessive hemorrhage. Proc. Natl. Acad. Sci. USA 103, 855–860 (2006).
Ruf, W. Tissue factor and PAR signaling in tumor progression. Thromb. Res. 120, S7–S12 (2007).
Bauer, A. T., Gorzelanny, C., Gebhardt, C., Pantel, K. & Schneider, S. W. Interplay between coagulation and inflammation in cancer: Limitations and therapeutic opportunities. Cancer Treat Rev. 102, 102322 (2022).
Klerk, C. P. et al. The effect of low molecular weight heparin on survival in patients with advanced malignancy. J. Clin. Oncol. 23, 2130–2135 (2005).
Kearon, C. & Kahn, S. Long-term treatment of venous thromboembolism. Blood 135, 317–325 (2020).
Zhang, N. et al. Low molecular weight heparin and cancer survival: clinical trials and experimental mechanisms. J Cancer Res Clin Oncol. 142, 1807–1816 (2016).
Camp, R., Dolled-Filhart, M. & Rimm, D. X-tile a New Bio-informatics tool for biomarker assessment and outcome-based Cut-point optimization. Clin Cancer Res. 10, 7252–7259 (2004).
Acknowledgements
Thanks to Professor Gang Tian from the First Affiliated Hospital of Xi'an Jiaotong University for her guidance on our research.
Funding
This study was supported by the National Natural Science Foundation of China (NO.81501826), the National Natural Science Foundation of Shaanxi (2020JQ-504;2020JQ540, 2021JM256), clinical cancer research center of Shaanxi Province (2019LCZX-02) and Science Foundation of Xi’an (20YXYJ0002(2)).
Author information
Authors and Affiliations
Contributions
X.Z. and X.W. wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, X., Wang, X., Li, W. et al. D-dimer, a predictor of bad outcome in gastric cancer patients undergoing radical resection. Sci Rep 12, 16432 (2022). https://doi.org/10.1038/s41598-022-16582-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16582-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.