Abstract
We investigated the association between working status changes and hand-grip strength (HGS) among middle-aged and older Korean adults using data from the 2006–2018 Korean Longitudinal Study of Aging. After excluding those with less than normal HGS in the baseline year, newly added panels, and missing values, 3843 participants (2106 men; 1737 women) were finally included. After adjusting for potential confounders, we used a 2-year lagged multivariable generalized estimating equation model to examine this association longitudinally. Men who quit working or who continued to be non-working were more likely to have lower HGS than those who continued to work (working → non-working, adjusted odds ratio [OR]: 1.47, 95% confidence interval [CI] 1.26–1.70; non-working → non-working, adjusted OR: 1.52, 95% CI 1.34–1.72). Compared to women who continued to work, the other three groups showed high ORs with low HGS (working → non-working, adjusted OR: 1.19, 95% CI 1.01–1.40; non-working → working, adjusted OR: 1.18, 95% CI 0.98–1.42; non-working → non-working, adjusted OR: 1.38, 95% CI 1.22–1.56). Middle-aged and older adults whose working status changed to non-working were at higher risk of reduced HGS than others and required muscular strength training interventions to improve HGS and prevent sarcopenia.
Similar content being viewed by others
Introduction
The loss of muscle mass and strength is a prominent feature of the aging population and is commonly characterized by sarcopenia1,2. Studies on sarcopenia have increased, revealing that muscle strength reduction results in poor health outcomes such as functional disabilities, cognitive decline, chronic morbidities, and all-cause mortality3,4,5,6. Hand-grip strength (HGS)—a simple, quick, reliable, and inexpensive method for measuring strength—is used for measuring the overall muscle strength in older adults and is known to be correlated with leg strength7,8. Recent studies have proved the validity of using hand dynamometers to assess health and nutritional status9,10, and several previous studies have used HGS as a proxy measure for muscle function and physical health2,11,12,13. HGS measurement is increasingly common as a clinically viable screening tool for determining muscle weakness and detecting other clinically relevant health outcomes1. Both the Asian Working Group for Sarcopenia (AWGS) and the European Working Group on Sarcopenia in Older People (EWGSOP) also apply HGS as a criterion for sarcopenia7,8.
Unemployment is known to affect health adversely14. Previous studies have shown that unemployed older people have poor physical and mental health15,16 and low quality of life17, proving that economic activity in old age is an important determinant of health and quality of life. Furthermore, older people change their working status more frequently than young people for various reasons, such as retirement and health problems, leading to diverse health outcomes. There are many studies on the health status of older people who quit economic activity18,19. Still, few studies have attempted to examine the effects of changes in working status in old age on health outcomes using longitudinal data. Moreover, when investigating the relationship between working status and health, HGS has rarely been used to indicate overall strength and health in older people.
Therefore, we aimed to investigate the association between changes in working status and HGS among Korean middle-aged and older adults based on a longitudinal panel study. Confirming this association through a large sample of population-based panel data would help establish a basis for improving the health and well-being of the aging population.
Methods
Data and study population
The data analyzed in this study were obtained from the Korean Longitudinal Study of Aging (KLoSA). The KLoSA is a longitudinal panel survey of nationally representative Koreans aged ≥ 45 years, excluding institutionalized people and Jeju Island residents. The Korea Labor Institute has conducted a survey every 2 years since 2008 to build primary data for establishing effective social and welfare policies and preparing for an aging society. Data pertaining to family, health, employment, income, assets, subjective expectations, and quality of life are collected20,21. As the KLoSA is publicly accessible and informed consent was obtained from all participants, no further ethical approval was required.
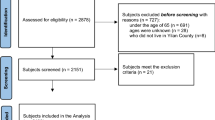
In this study, we utilized data from the first to seventh waves of the KLoSA (2006–2018). In all, 10,254 individuals participated in the baseline survey conducted in 2006. Considering the study hypothesis, those with low HGS in the baseline year were excluded (n = 2060). In addition, individuals that did not participate in the first to seventh waves (n = 2640) and those with missing values (n = 1711) were excluded. Finally, 3843 individuals (2106 men; 1737 women) were included in the analysis as the study population. In conducting this observational study, we followed the STROBE checklist22. The detailed flow of the sample selection process is depicted in Fig. 1.
Measures
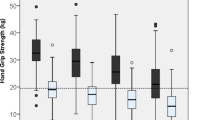
HGS, the dependent variable in this study, was measured in kilograms using a hand-grip dynamometer (Model number: 6103, TANITA, Japan). The participants in the KLoSA were asked to squeeze the dynamometer twice for each hand in a sitting position, and the mean value of four trials was recorded. Since previous studies have confirmed that HGS is significantly different in men and women13,23, we analyzed the data by stratification according to sex. In the present study, HGS was analyzed as a categorical variable according to the criteria presented by the AWGS in 2019. Low HGS was defined as those with HGS < 28 kg for men and < 18 kg for women24.
Each participant was asked about their working status through the question, "Are you currently working for income?" In this context, working included being employed, running their own business, and helping a family member or relatives. The response options were "Yes" or "No". Changes in working status per wave, which was the main variables of interest, were classified into four groups: (1) working → working, (2) working → non-working, (3) non-working → working, and (4) non-working → non-working.
Covariates included socioeconomic and health-related variables for each wave. Socioeconomic factors included age (45–59, 60–69, 70–79, and ≥ 80 years), marital status (married, unmarried, or separate), region (urban and rural), the highest level of education (middle school and below, high school, and college and above), and personal income level, which were divided into tertiles, with tertile 3 indicating the highest earner. Health-related factors included satisfaction with health status, body mass index (BMI), activities of daily living (ADL), instrumental activities of daily living (IADL), cognitive function, and regular physical exercise. Perceived satisfaction with health status was classified into dissatisfied, average, and satisfied. BMI was calculated from self-reported height and weight data on the first wave and divided into three groups (underweight: BMI < 18.5 kg/m2, normal: BMI 18.5–24.95 kg/m2, and overweight: BMI ≥ 25 kg/m2). ADL and IADL indices were classified as 0 and 1, with 0 points indicating normality and 1 point indicating the need for help25. Cognitive function was measured by the Korean version of the MMSE score during the first wave, and with a total score of 30, the cut-off level for cognitive impairment was 24 points26. Regular physical exercise was defined as "Yes" if they exercised at least once a week and "No" if not25.
Statistical analysis
The chi-square test was conducted to investigate and compare the general characteristics of the study population. We also used a 2-year lagged multivariable generalized estimating equation (GEE) model to longitudinally examine the association between changes in working status and HGS after adjusting for potential confounders27. The key results are presented as odds ratios (ORs), regression coefficients (β), and 95% confidence intervals (CIs). The statistical package SAS version 9.4 (SAS Institute Inc.; Cary, NC, USA) was used for all analyses, and p-values < 0.05 were deemed statistically significant.
Results
Table 1 shows the general characteristics of the study population in the baseline year (2006–2008) at the first time point of changes in working status. The four groups of changes in working status showed statistically significant differences in HGS for both sexes. Other covariates also showed significant differences in HGS for men, except for region, and women, except for region and BMI.
Table 2 presents the results of the GEE analysis of the association between changes in working status and HGS after adjusting for all potential confounding variables. Among men, it was found that those who quit working and those who continued to be non-working were more likely to have lower HGS than those who continued to work (working → non-working, adjusted OR: 1.47, 95% CI 1.26–1.70; non-working → non-working, adjusted OR: 1.52, 95% CI 1.34–1.72). Conversely, in women, compared to those who continued to work, all of the other three groups showed high ORs with low HGS (working → non-working, adjusted OR: 1.19, 95% CI 1.01–1.40; non-working → working, adjusted OR: 1.18, 95% CI 0.98–1.42; non-working → non-working, adjusted OR: 1.38, 95% CI 1.22–1.56). A similar tendency was also observed in analyzing HGS as a continuous variable. Compared with the group who continued to work, the group who quit working and those who continued to be non-working showed highly significant regression coefficients (Supplementary Table 1).
Additionally, we conducted sensitivity analyses to examine this association using different criteria for defining HGS (Table 3). The European Working Group on Sarcopenia in Older People 2 defined the criteria for low HGS as < 27 kg for men and < 16 kg for women28,29. We also performed the analysis by defining the low 25 percentiles of KLoSA, the data used in this study, as low HGS. The criteria were < 26.75 kg for men and < 16.25 kg for women. Even when other criteria were applied, the association between changes in working status and HGS was confirmed.
Discussion
In this nationally representative longitudinal panel study, we found an association between changes in working status and HGS among Korean adults aged > 45 years. In particular, those who quit their jobs and continued to be non-working were likelier to have lower HGS than those who continued to work. These results suggest that what affects HGS is the final working status, so it can be interpreted that the risk of low HGS is higher when the final working status is non-working. In addition, there was a difference in the association with HGS between the two groups with changes in working status. Although not statistically significant, the men who changed from non-working to working status were less likely to have reduced HGS. This suggests that if middle-aged and older adults resume economic activity, their muscle strength, including HGS, is expected to improve. Similar to the findings of our longitudinal study, a cross-sectional study proved that there was a higher likelihood of low HGS in unemployed elderly men30.
Factors affecting HGS have been identified in previous studies4. For example, HGS and its association with cognitive functioning31,32,33, depressive symptoms34, and ADL disability35 have been studied. Studies have revealed the effects of HGS on health-related outcomes, such as mortality36,37 and multimorbidity38 in older and ill patients. In addition, the impact of working hours and working conditions on health status or health-related behaviors have already been proven39,40,41. However, few studies have examined the relationship between changes in working status and HGS in community-dwelling adults. As the working status of many people is expected to change due to the outbreak of coronavirus disease 2019 (COVID-19)42, the results of this study are thought to be useful as evidence for the development of interventions aimed at promoting strength training among middle-aged and older people.
Studies conducted in Asia generally define HGS weakness according to the AWGS criteria. However, when we redefined the low HGS criteria based on the KLoSA data in the sensitivity analysis, the criteria for both men and women were slightly lower than those obtained with the AWGS criteria. This may mean that the HGS of Koreans is weak compared to Asian standards, further suggesting the lack of strength training in the Korean context. We also suggest that to facilitate advanced research on the effects of sarcopenia on health in the future, Korean criteria should be clearly established.
Our study has certain strengths and limitations. A major strength is that the sample size was relatively large and adequately represented Korean adults; therefore, our results can be generalized to the national level. However, one important limitation of this study is that only absolute HGS was considered when defining the dependent variable. Although there is a concept of relative HGS (RHGS), which is calculated by dividing the BMI by absolute HGS, we did not use RHGS because the height and weight required to calculate BMI were not accurately measured as they were self-reported variables. Instead, we included BMI as a covariate, and a subgroup analysis was performed according to BMI. Second, we adjusted the exercise variable, but we could not confirm the type and duration of the exercise. While it was confirmed that exercise was associated with HGS, it would be useful to conduct additional analyses by supplementing the questionnaire items on the type and duration of exercise. Third, although we attempted to adjust for covariates that may affect HGS, residual confounding effects of unmeasured variables could not be ruled out. For example, we could not adjust for variables related to the type of job and the reasons for the changes in working status. Further studies should complement these factors to introduce more appropriate interventions for the aging population.
Conclusion
This study identified an association between changes in working status and HGS among middle-aged and older Korean adults. In particular, individuals who quit working or continued to have a non-working status were at a higher risk of low HGS than others. Our findings suggest the need to introduce muscular strength training interventions to improve HGS and prevent sarcopenia in the aging population.
Data availability
The dataset analyzed in the present study is publicly accessible. Available online: https://survey.keis.or.kr/klosa/klosa01.jsp.
Abbreviations
- AWGS:
-
Asian Working Group for Sarcopenia
- EWGSOP:
-
European Working Group on Sarcopenia in Older People
- HGS:
-
Hand-grip strength
- KLoSA:
-
Korean Longitudinal Study of Aging
References
McGrath, R. P., Kraemer, W. J., Snih, S. A. & Peterson, M. D. Handgrip strength and health in aging adults. Sports Med. 48, 1993–2000 (2018).
Taekema, D. G., Gussekloo, J., Maier, A. B., Westendorp, R. G. & de Craen, A. J. Handgrip strength as a predictor of functional, psychological and social health. A prospective population-based study among the oldest old. Age Ageing. 39, 331–337 (2010).
Cooper, C. et al. Tools in the assessment of sarcopenia. Calcif. Tissue Int. 93, 201–210 (2013).
Riviati, N., Setiati, S., Laksmi, P. W. & Abdullah, M. Factors related with handgrip strength in elderly patients. Acta Med. Indones 49, 215–219 (2017).
Keller, K. & Engelhardt, M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 3, 346 (2013).
Vianna, L. C., Oliveira, R. B. & Araújo, C. G. S. Age-related decline in handgrip strength differs according to gender. J. Strength Conditioning Res. 21, 1310–1314 (2007).
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis. Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 39, 412–423 (2010).
Chen, L.-K. et al. Sarcopenia in Asia: Consensus report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 15, 95–101 (2014).
Luna-Heredia, E., Martín-Peña, G. & Ruiz-Galiana, J. Handgrip dynamometry in healthy adults. Clin. Nutr. 24, 250–258 (2005).
Budziareck, M. B., Duarte, R. R. P. & Barbosa-Silva, M. C. G. Reference values and determinants for handgrip strength in healthy subjects. Clin. Nutr. 27, 357–362 (2008).
Jang, S.-K., Kim, J.-H. & Lee, Y. Effect of relative handgrip strength on cardiovascular disease among Korean adults aged 45 years and older: Results from the Korean Longitudinal Study of Aging (2006–2016). Arch. Gerontol. Geriatr. 86, 103937 (2020).
Velghe, A., De Buyser, S., Noens, L., Demuynck, R. & Petrovic, M. Hand grip strength as a screening tool for frailty in older patients with haematological malignancies. Acta Clin. Belg. 71, 227–230 (2016).
Leyk, D. et al. Hand-grip strength of young men, women and highly trained female athletes. Eur. J. Appl. Physiol. 99, 415–421 (2007).
Wilson, S. H. & Walker, G. Unemployment and health: A review. Public Health 107, 153–162 (1993).
Ahn, J., Kim, N.-S., Lee, B.-K., Park, J. & Kim, Y. Comparison of the physical and mental health problems of unemployed with employees in South Korea. Arch. Environ. Occup. Health 76, 163–172 (2021).
Breslin, F. C. & Mustard, C. Factors influencing the impact of unemployment on mental health among young and older adults in a longitudinal, population-based survey. Scand. J. Work Environ. Health. 5–14 (2003).
Worach-Kardas, H. & Kostrzewski, S. Quality of life and health state of long-term unemployed in older production age. Appl. Res. Qual. Life 9, 335–353 (2014).
Sickles, R. C. & Taubman, P. An analysis of the health and retirement status of the elderly. Econometrica J. Econometr. Soc. 1339–1356 (1986).
Park, H. & Kim, G. Exploring a direction of the development of an education program for health improvement of the unemployed elderly. J. Korea Acad.-Ind. Cooperation Society 18, 428–435 (2017).
University of Southern California Dornsife Center for Economic and Social Research. The Gateway to Global Aging Data. https://g2aging.org/. Accessed 22 June 2022.
Jang, S.-N. Korean Longitudinal Study of Ageing (KLoSA): Overview of research design and contents. Encyclopedia Geropsychol. 1–9 (2015).
Von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 147, 573–577 (2007).
Sevene, T. G. et al. Hand grip strength and gender: Allometric normalization in older adults and implications for the NIOSH lifting equation. J. Lifestyle Med. 7, 63 (2017).
Chen, L.-K. et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Directors Assoc. 21, 300-307.e302 (2020).
Service, K. E. I. User's Guide for the 2018 Korean Longitudinal Study of Ageing (KLoSA) (2018).
Crum, R. M., Anthony, J. C., Bassett, S. S. & Folstein, M. F. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA 269, 2386–2391 (1993).
Nari, F., Jeong, W., Jang, B. N., Lee, H. J. & Park, E.-C. Association between healthy lifestyle score changes and quality of life and health-related quality of life: A longitudinal analysis of South Korean panel data. BMJ Open 11, e047933 (2021).
Reiss, J. et al. Consequences of applying the new EWGSOP2 guideline instead of the former EWGSOP guideline for sarcopenia case finding in older patients. Age Ageing 48, 719–724 (2019).
Van Ancum, J. M. et al. Impact of using the updated EWGSOP2 definition in diagnosing sarcopenia: A clinical perspective. Arch. Gerontol. Geriatr. 90, 104125 (2020).
Kwak, Y., Kim, Y. & Chung, H. Sex-associated differences in the handgrip strength of elderly individuals. West. J. Nurs. Res. 42, 262–268 (2020).
Alfaro-Acha, A. et al. Handgrip strength and cognitive decline in older Mexican Americans. J. Gerontol. A Biol. Sci. Med. Sci. 61, 859–865 (2006).
McGrath, R. et al. Handgrip strength is associated with poorer cognitive functioning in aging Americans. J. Alzheimers Dis. 70, 1187–1196 (2019).
McGrath, R. et al. The longitudinal associations of handgrip strength and cognitive function in aging Americans. J. Am. Med. Directors Assoc. 21, 634-639.e631 (2020).
Gopinath, B., Kifley, A., Liew, G. & Mitchell, P. Handgrip strength and its association with functional independence, depressive symptoms and quality of life in older adults. Maturitas 106, 92–94 (2017).
Snih, S. A., Markides, K. S., Ottenbacher, K. J. & Raji, M. A. Hand grip strength and incident ADL disability in elderly Mexican Americans over a seven-year period. Aging Clin. Exp. Res. 16, 481–486 (2004).
Al Snih, S., Markides, K. S., Ray, L., Ostir, G. V. & Goodwin, J. S. Handgrip strength and mortality in older Mexican Americans. J. Am. Geriatr. Society. 50, 1250–1256 (2002).
Ling, C. H. et al. Handgrip strength and mortality in the oldest old population: The Leiden 85-plus study. CMAJ 182, 429–435 (2010).
Cheung, C.-L., Nguyen, U.-S.D., Au, E., Tan, K. C. & Kung, A. W. Association of handgrip strength with chronic diseases and multimorbidity. Age 35, 929–941 (2013).
Berniell, M. I. The effects of working hours on health status and health behaviors. in 15th IZA European Summer School in Labor Economics (2012).
D’Souza, R. M. et al. The health effects of jobs: Status, working conditions, or both?. Aust. N. Z. J. Public Health 29, 222–228 (2005).
Artazcoz, L., Cortès, I., Escribà-Agüir, V., Cascant, L. & Villegas, R. Understanding the relationship of long working hours with health status and health-related behaviours. J. Epidemiol. Community Health 63, 521–527 (2009).
Kawohl, W. & Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry 7, 389–390 (2020).
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI20C1130). Additionally, this work was supported by the National Research Foundation of Korea(NRF) grant funded by the Korea government(MSIT) (No. 2022R1F1A1062794).
Author information
Authors and Affiliations
Contributions
I.Y. made a substantial contribution to the concept or design of the work; I.Y. and Y.S.P. contributed to the acquisition, analysis, or interpretation of data; I.Y., E.P., and S.-I.J. drafted the article or revised it critically for important intellectual content. All authors approved the version to be published and participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yun, I., Park, Y., Park, EC. et al. Association between changes in working status and hand-grip strength among Korean middle-aged and older adults: a longitudinal panel study. Sci Rep 12, 12897 (2022). https://doi.org/10.1038/s41598-022-16373-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16373-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.