Abstract
Low health-related quality of life (HRQOL) is associated with adverse outcomes in diabetic kidney disease (DKD) patients. We examined the modifiable factors associated with low HRQOL in these patients. We enrolled 141 DKD patients. HRQOL was assessed with the Short Form 36 (SF-36) questionnaire. Low HRQOL was defined as a score > one standard deviation below the mean. Depression and anxiety were assessed with the Hospital Anxiety and Depression Scale (HADS-D and HDAS-A, respectively). The patients’ median age was 65 years, and 73% were men. The prevalence rates of anxiety and depression were 8% (n = 11) and 17% (n = 24), respectively. Forty (28%) patients were identified as poor sleepers, and 40 (28%) had low physical activity levels. Anxiety, depression, and poor sleep quality were negatively correlated with SF-36 scores. Higher levels of physical activity and the estimated glomerular filtration rate (eGFR) were correlated with higher SF-36 scores, which indicated better health status. Higher depression scores (HADS-D scores) were associated with low HRQOL, independent of factors including age, sex, smoking status, comorbidities, eGFR, anemia, sleep quality, anxiety levels, and physical activity levels (odds ratio, 1.43; 95% confidence interval, 1.17–1.75). Among the clinical and psycho-physical factors, depression was a main determinant of low HRQOL in DKD patients.
Similar content being viewed by others
Introduction
Diabetic kidney disease (DKD) develops in approximately 40% of patients with diabetes. Despite recent therapeutic advances, the annual incidence of DKD has more than doubled over the last decade1. This substantial increase in prevalence is progressive as the population is aging, obesity is more prevalent, and more people survive cardiovascular problems2. DKD is associated with an increased risk of all-cause death and cardiovascular disease and imparts a substantial burden through health care costs as the leading cause of end-stage kidney disease (ESKD) worldwide3.
Health-related quality of life (HRQOL) refers to an individual’s beliefs, perceptions, experiences, and expectations for enjoyment in terms of life that may be affected by one’s health condition4. Patients with diabetes and kidney disease have lower HRQOL than the general population. Additionally, it is now widely accepted that low HRQOL is associated with an increased risk of cardiovascular diseases and death in patients with chronic kidney disease (CKD)5,6. A better understanding of HRQOL would allow clinicians to provide patient-centered care and improve long-term outcomes. However, although low HRQOL is increasingly recognized as an important predictor of adverse outcomes, previous studies have focused on nonmodifiable clinical factors such as age, sex, and comorbidities in association with HRQOL. Therefore, it is important to identify potentially modifiable risk factors associated with low HRQOL in patients with CKD.
This study was conducted to examine clinical factors associated with HRQOL using the Short Form 36 (SF-36) Health Survey Questionnaire in patients with DKD. In particular, we focused on modifiable factors such as depression, anxiety, sleep quality, anemia, glycemic control, and physical activity.
Methods
Study design and study subjects
We recruited outpatients with DKD between April 2017 and March 2018 from the nephrology clinic of a single tertiary hospital. The inclusion criteria were predialysis or dialysis patients with DKD who were aged ≥ 18 years and using glucose-lowering agents such as oral hypoglycemic agents or insulin. DKD was defined as biopsy-proven diabetic nephropathy or was clinically determined in diabetic patients with an estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m2, with or without persistent proteinuria for 3 months or longer and without any other specific reason7. Persistent proteinuria was defined as a urinary albumin-to-creatinine ratio (uACR) ≥ 30 mg/g or a urinary protein-to-creatinine ratio (uPCR) ≥ 0.2 g/g. The eGFR was obtained using the Chronic Kidney Disease Epidemiology Collaboration creatinine equation8. All clinical studies were conducted in accordance with the guidelines of the 2013 Declaration of Helsinki. All patients signed informed consent forms. The study protocol was approved by the Institutional Review Board of the Samsung Medical Center.
Data collection and measures
Demographic data on age, sex, body mass index (BMI), smoking status, comorbidities, medication history, diabetes duration, and dialysis were collected through an interview and medical chart review at baseline enrollment. Comorbidity burden was measured using the modified Charlson Comorbidity Index (CCI), which included the following comorbid conditions: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebral vascular accident, dementia, chronic obstructive pulmonary disease, connective tissue disease, peptic ulcer disease, liver disease, diabetes mellitus, renal insufficiency, leukemia, lymphoma, solid tumor, liver disease, and AIDS/HIV9. The age factor was excluded from the index to examine the influence of age on HRQOL independent of comorbidities. Anthropometric and blood pressure measurements were performed by trained personnel, and laboratory data, including white blood cell counts, hemoglobin (Hb) levels, serum creatinine levels, HbA1c levels, and uACR or uPCR values, were measured at baseline. For dialysis patients, the above measurements were performed midweek before an HD (hemodialysis) session.
Health-related questionnaires were administered with the aid of study personnel. For enrolled dialysis patients, the questionnaires were answered midweek before an HD session. Sleep quality was measured using the Korean version of the Pittsburgh Sleep Quality Index (PSQI-K), which is comparable to the original version. It is a valid and reliable screening tool to identify “good” and “poor” sleepers10. The PSQI consists of 18 questions covering sleep quality, sleep-onset latency, sleep efficiency, sleep duration, sleep disturbance, sleeping medication use, and daytime dysfunction. Each item is scored from 0 to 3, yielding a global PSQI score ranging from 0 to 21, with higher scores indicating lower sleep quality. A total score > 5 indicates poor sleep, while a total score ≤ 5 indicates good sleep. To determine anxiety and depression levels, the Hospital Anxiety and Depression Scale (HADS) was used11,12. This scale is divided into an anxiety subscale (HADS-A) and a depression subscale (HADS-D), both containing seven intermingled items. Each item has 4 response categories ranging from 0 to 3, with total scores ranging from 0 to 21. For both anxiety and depression, scores of 0–7 are considered normal, 8–10 are considered borderline abnormal, and 11–21 are considered abnormal12. The Korean version of the International Physical Activity Questionnaire (IPAQ)-Short Form records physical activity in the last seven days13. The 7-item IPAQ was used to identify the total minutes spent on moderate- and vigorous-intensity physical activity, walking, and inactivity over the last seven days. Responses were converted to metabolic equivalent task minutes per week (MET-min/wk) measures according to the IPAQ scoring protocol14. Physical activity levels were categorized as low, moderate, and high. Low physical activity was defined as inactivity or some activity that was not enough to fall into categories 2 or 3. Moderate physical activity was defined as any of the following three criteria: three or more days of vigorous activity with at least 20 min per day; five or more days of moderate-intensity activity or walking with at least 30 min per day; or five or more days of any combination of walking, moderate-intensity, or vigorous-intensity activities achieving a minimum of at least 600 MET-min/wk. High physical activity was defined as any one of the following criteria: vigorous-intensity activity for at least three days and accumulating at least 1500 MET-min/wk or seven or more days of any combination of walking, moderate- or vigorous-intensity activities and accumulating at least 3000 MET-min/wk.
HRQOL assessment
The SF-36 (version 2.0) was used to assess comprehensive HRQOL15,16. It comprises 36 questions, eight scales (physical functioning [PF], role limitation caused by physical problems [RF], bodily pain [BP], general health [GH], vitality [VT], social functioning [SF], role limitation caused by emotional problems [RE], and mental health [MH]), and two summary measures. Responses to each question were transformed into SF-36 equivalent scores, and scores ranged from 0 to 100, with higher numerical scores indicating better HRQOL. The PF, RF, BP, and GH subscales were summarized in a physical component summary (PCS), while the VT, SF, RE and MH subscales were summarized in a mental component summary (MCS). We defined low HRQOL as an SF-36 score > one standard deviation (SD) below the mean, referring to previous studies with CKD patients17,18. Likewise, we defined low physical health and low mental health as PCS scores and MCS scores > one SD below the mean, respectively.
Statistical analyses
Data are expressed as percentiles for categorical variables, and medians and interquartile ranges (IQRs) for continuous variables. Chi-squared analysis or Fisher's exact test for categorical variables and the Kruskal–Wallis test for continuous variables were used to determine differences in baseline characteristics according to CKD stages. Differences in SF-36, PCS, and MCS scores between good sleepers and poor sleepers were assessed using the Mann–Whitney rank sum test. The Jonckheere–Terpstra test was used to determine trend significance in continuous variables. Spearman’s correlation coefficients were used to examine relationships between clinical parameters and SF-36 scores. The association between low HRQOL assessed by the SF-36 score and clinical factors was investigated using multivariable logistic regression analysis adjusted for age, sex, CCI score, smoking status, Hb level, eGFR and PSQI-K, HADS-A, HADS-D, and IPAQ scores, and the results were reported as odds ratios (ORs) and 95% confidence intervals (95% CIs). For the multiple logistic regression analysis, we selected confounding factors based on potential confounding factors that were proven in previous studies, the variables that showed significant association with low HRQOL in our univariate analysis, and our variables of interest. The goodness of fit of the logistic regression models was assessed using the area under the ROC curve (AUC)19. The multicollinearity of the variables was assessed using the variance inflation factor (VIF) with a reference value of 10 before interpreting the final output. Likewise, the association of clinical factors with low HRQOL, as assessed by the PCS score and MCS score, was investigated using the aforementioned methods. Additional logistic regression analyses were performed excluding dialysis patients since dialysis treatment itself could be a mediator in the association between HRQOL and clinical factors. Because of the lack of a solid definition of low HRQOL, additional sensitivity analyses with the aforementioned adjustments were performed using a linear regression model for the association of clinical factors with the SF-36 score as a continuous variable. Cook’s distance20 was used in regression analysis to find influential outliers in a set of predictor variables. There were no missing data or significant outliers. All statistical analyses were performed using SPSS version 25.0 for Windows (IBM, Armonk, NY, USA), SAS version 9.4 (SAS Institute, Cary, NC) and R 4.0.3 (Vienna, Austria; http://www.R-project.org/). A p value < 0.05 was considered significant.
Results
Study participants’ characteristics
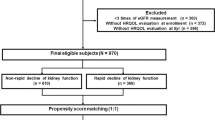
A total of 141 patients with DKD were enrolled and completed the SF-36 and other questionnaires (Supplementary Fig. 1). The median age was 65 (57–72) years, and 103 (73%) patients were male. Fifty-six patients were categorized as having CKD stage 3, 41 were categorized as having stage 4, and 44 were categorized as having stage 5, including 28 patients on hemodialysis. Overall, the prevalence rates of anxiety and depression were 8% (n = 11) and 17% (n = 24), respectively, based on a HADS score of ≥ 8. Among a total of 24 depressive patients, 7 (29%) were on dialysis. Forty (28%) patients were identified as poor sleepers, and 40 (28%) had low physical activity levels.
The baseline characteristics of the patients according to CKD stage are summarized in Table 1. The CCI scores were higher in patients with advanced CKD stages (p < 0.001 for trend). Similarly, the PSQI-K scores were higher in patients with advanced CKD stages (stage 3, 2.0 [1.0–5.0]; stage 4, 2.0 [1.0–5.5]; stage 5, 4.0 [2.3–8.0], p = 0.005 for trend). Twenty-three percent (n = 13) of the patients with CKD stage 3, 24% (n = 10) of those with stage 4, and 39% (n = 17) of those with stage 5 were poor sleepers (p = 0.1 for trend). Anxiety scores, depression scores, and physical activity levels did not differ by CKD stage. SF-36 scores decreased progressively with advanced CKD stages (stage 3, 78.8 [71.0–82.1]; stage 4, 70.5 [56.4–81.5]; stage 5, 69.8 [56.9–81.6], p = 0.012 for trend).
SF-36 score distributions
Distributions of SF-36 scores according to CCI scores, sleep quality, anxiety, depression, and physical activity levels are presented in Fig. 1. SF-36 scores did not differ according to CCI scores (p = 0.122; Fig. 1a). Conversely, poor sleepers showed lower HRQOL scores than good sleepers; the median (IQR) SF-36 total score was 69.9 (53.3–79.6) and 77.0 (64.8–82.2; p = 0.011) for poor and good sleepers, respectively (Fig. 1b). The SF-36 total score was progressively lower in patients with higher HADS-A scores; the SF-36 total scores were 74.8 (63.6–82.0), 59.8 (48.7–80.1), and 36.7 (27.2–46.1) in patients with normal, borderline abnormal, and abnormal HADS-A scores, respectively (p = 0.026 for trend) (Fig. 1c). Similarly, patients with higher HADS-D scores showed progressively lower SF-36 total scores; the SF-36 total scores were 77.0 (66.1–82.3), 59.8 (53.5–73.1), and 44.1 (35.2–58.4) in patients with normal, borderline abnormal, and abnormal HADS-D scores, respectively (p < 0.001 for trend) (Fig. 1d). The subjects with higher physical activity levels showed progressively higher SF-36 total scores; the SF-36 total scores were 65.4 (53.3–76.9), 77.6 (65.8–82.8), and 78.6 (68.9–82.1] in patients with low, moderate, and high physical activity levels, respectively (p = 0.003 for trend) (Fig. 1e).
Distribution of health-related quality of life according to comorbidities (A), sleep quality (B), anxiety (C), depression (D), and physical activity level (E) among patients with diabetic kidney disease. Bars and error bars indicate the median value and interquartile range, respectively. Abbreviations: CCI Charlson Comorbidity Index, MCS mental component summary, SF-36 Short Form 36 of life Health Survey Question, SQ sleep quality, PA physical activity, PCS physical component summary.
Association between clinical factors and HRQOL
Correlations between clinical variables and HRQOL scores were analyzed. As depicted in Table 2, SF-36 total scores were negatively correlated with anxiety, depression, and sleep quality. HRQOL scores were positively correlated with the eGFR and physical activity levels.
In the multivariable logistic regression analyses, adjusted for age, sex, smoking status, CCI score, Hb level, eGFR and PSQI-K, HADS-A, HADS-D, and IPAQ scores, that were performed to determine the factors associated with low HRQOL as assessed by the SF-36 total score, depression scores (HADS-D) were associated with low HRQOL, independent of age, sex, smoking status, comorbidities (CCI score), eGFR, anemia, sleep quality (PSQI-K score), anxiety (HADS-A score), and physical activity level (IPAQ score); the OR (95% CI) per 1-score increment was 1.43 (1.17–1.75) (p < 0.001) (Table 3). However, the association of the eGFR, PSQI-K score, anxiety score, and IPAQ score with low HRQOL was attenuated in the multivariable logistic regression analysis. In particular, the HADS-D score showed an evident association with physical health; the OR (95% CI) per 1-score increment of HADS-D scores was 1.36 (1.13–1.64) (p = 0.001). However, the association between the HADS-D score and mental health was attenuated. Rather, anxiety scores (HADS-A) were independently associated with low mental health (Table 3). Our fitting model showed no significant difference between the model and the observed data (AUC value, 0.8515 for overall HRQOL; 0.7949 for Physical health; 0.8511 for Metal health). The VIF showed no evidence of a multicollinearity problem among the independent variables (all VIFs < 3).
Sensitivity analyses
We performed sensitivity analyses to confirm the robustness of the results. In linear regression analysis, the HADS-D score was the most potent modifiable factor associated with HRQOL; a higher HADS-D score was associated with a lower SF-36 total score, PCS score, and MCS score (Supplementary Table 1).
In the analyses that excluded dialysis patients (n = 28), a consistent association between depression and low HRQOL was observed; the ORs (95% CIs) per 1-score increment of HADS-D scores were 1.43 (1.14–1.80) and 1.31 (1.07–1.60) for low HRQOL as assessed by the SF-36 total score and PCS score, respectively (all p < 0.05, Supplementary Table 2). Additionally, a consistent association between anxiety and low mental health was observed; the OR (95% CI) per 1-score increment of HADS-A scores was 1.32 (1.03–1.69) (p = 0.031).
Discussion
We examined clinical and psycho-physical factors, including health-related behaviors associated with HRQOL, in patients with DKD stage 3–5, focusing especially on modifiable factors. We found that depression was a main determinant of low HRQOL in these patients, independent of factors including age, sex, comorbidities, smoking status, kidney function, anemia, glycemic control level, sleep quality, anxiety, and physical activity level. This association between depression and low HRQOL, in particular, was evident in the physical health domain.
Approximately 20–40% of patients with predialysis CKD, as well as those on maintenance dialysis, have depression21. Diabetes in particular is known to be a risk factor for depression in patients with CKD22. Moreover, DKD progression is associated with an increased risk of depression23. In patients with CKD or ESKD, depression is associated with increased health-care utilization, lower treatment compliance, and poor social and occupational role functioning24,25,26. Moreover, although HRQOL is an important patient-centered outcome, and low HRQOL is increasingly recognized as an important predictor of adverse outcomes such as progression to ESKD and all-cause and cardiovascular mortalities in patients with CKD, previous studies have largely focused on nonmodifiable clinical factors such as age, sex, and comorbidities in association with HRQOL. Depression as a modifiable factor has been shown to have a negative effect on HRQOL in patients with diabetes27 and CKD28,29. Some authors even reported that depressive symptoms were more associated with low HRQOL than measures of dialysis adequacy, other demographic variables, and low hemoglobin levels30,31. However, the association between depression and low HRQOL shown in previous studies might have been affected by health-related behaviors such as sleep quality, physical activity, and smoking status. Low physical activity levels and poor sleep quality are known to be associated with low HRQOL in patients with CKD32,33. In this study, low physical activity levels and poor sleep quality were also associated with low HRQOL. However, after adjusting for nonmodifiable and modifiable factors, depression was the most relevant modifiable factor associated with low HRQOL. In particular, we found that depression was more obviously associated with low physical health than with low mental health. Similar to our results, a previous study34 showed that the PCS score was more impaired than the MCS score in patients with predialysis CKD, and the PCS score was negatively associated with depression in multivariate analysis. When depression is added to the diabetic state, the effect of depression on HRQOL can be more additive for the PCS score than the MCS score35. In addition to depression, there are several sociodemographic and clinical factors associated with low HRQOL in patients with CKD. The Chronic Renal Insufficiency Cohort (CRIC) and Hispanic CRIC studies have reported that younger age, female sex, diabetes, peripheral vascular disease, congestive heart failure, low education level, obesity, and lower eGFR were significantly associated with low HRQOL in large diverse CKD cohorts5. Anemia may also negatively affect HRQOL, and hemoglobin correction is associated with improved HRQOL in patients with CKD36. In the present study, however, only depression was associated with low HRQOL in multivariate analysis.
This study has some limitations that should be considered in the interpretation of the results. First, our findings are limited in the assessment of causal relationships between depression and HRQOL because the study was cross-sectional. Therefore, the possibility of reverse causality between low HRQOL and depression may exist. However, most previous studies of patients with CKD have demonstrated the role of depression as a risk factor for low HRQOL. Moreover, low HRQOL as a risk factor for depression is rather likely to act as a mediator in the association between various risk factors and depression. In addition, although we adjusted for confounding factors in the analyses for the association with the quality of life in patients with DKD, unmeasured factors may still remain. In particular, factors such as marital status, education level, and income level may influence quality of life but these factors were not addressed in this study. Second, this study included dialysis patients. Dialysis treatment itself can reduce HRQOL and increase symptoms such as anxiety, depression, and sleep disorders, and may act as a confounding factor in the association between these factors and HRQOL. However, when we performed the sensitivity analysis excluding dialysis patients, the results did not change. Third, we used the HADS instead of structured clinical interviews to assess depression and anxiety; hence, misclassification was possible. Nevertheless, the HADS is known to be a reliable and valid tool for identifying depression in patients with CKD and ESKD. Moreover, this misclassification error was nondifferential, which would likely bias our results toward the null. Last, this was a single-center study with a relatively small sample size. Moreover, DKD patients with an eGFR ≥ 60 mL/min/1.73 m2 were excluded from this study, therefore limiting the generalizability of our results, especially for DKD populations with preserved renal function. Therefore, our study highlights the potential need for randomized controlled trials to assess the temporal relationship between depression and low HRQOL in patients with DKD and to further evaluate the effect of early detection of depression and appropriate depression care on the health outcomes of these patients. Notwithstanding these limitations, the strength of our study is that we conducted comprehensive analyses including health-related behaviors, such as smoking, sleep quality, and physical activity, as well as modifiable and nonmodifiable clinical characteristics to examine factors associated with HRQOL in patients with DKD.
Conclusion
This study investigated various factors associated with low HRQOL in patients with DKD and identified depression as a major determinant of reduced quality of life. These findings reinforce the importance of assessing depression in patients with DKD and incorporating this assessment into clinicians’ management decisions, urging future studies to provide biological rationale and evaluate causality.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Persson, F. & Rossing, P. Diagnosis of diabetic kidney disease: State of the art and future perspective. Kidney Int. Suppl. 2011(8), 2–7. https://doi.org/10.1016/j.kisu.2017.10.003 (2018).
Alicic, R. Z., Rooney, M. T. & Tuttle, K. R. Diabetic kidney disease: Challenges, progress, and possibilities. Clin. J. Am. Soc. Nephrol. 12, 2032–2045. https://doi.org/10.2215/CJN.11491116 (2017).
Afkarian, M. et al. Kidney disease and increased mortality risk in type 2 diabetes. J. Am. Soc. Nephrol. 24, 302–308. https://doi.org/10.1681/asn.2012070718 (2013).
Finkelstein, F. O., Wuerth, D. & Finkelstein, S. H. Health related quality of life and the CKD patient: Challenges for the nephrology community. Kidney Int. 76, 946–952. https://doi.org/10.1038/ki.2009.307 (2009).
Porter, A. C. et al. Predictors and outcomes of health-related quality of life in adults with CKD. Clin. J. Am. Soc. Nephrol. 11, 1154–1162. https://doi.org/10.2215/CJN.09990915 (2016).
Mapes, D. L. et al. Health-related quality of life as a predictor of mortality and hospitalization: The Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int. 64, 339–349. https://doi.org/10.1046/j.1523-1755.2003.00072.x (2003).
National Kidney, F. KDOQI clinical practice guideline for diabetes and CKD: 2012 Update. Am. J. Kidney Dis. 60, 850–886. https://doi.org/10.1053/j.ajkd.2012.07.005 (2012).
Inker, L. A. et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 367, 20–29. https://doi.org/10.1056/NEJMoa1114248 (2012).
Beddhu, S., Bruns, F. J., Saul, M., Seddon, P. & Zeidel, M. L. A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am. J. Med. 108, 609–613 (2000).
Sohn, S. I., Kim, D. H., Lee, M. Y. & Cho, Y. W. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath 16, 803–812. https://doi.org/10.1007/s11325-011-0579-9 (2012).
Bjelland, I., Dahl, A. A., Haug, T. T. & Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 52, 69–77 (2002).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370 (1983).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395. https://doi.org/10.1249/01.mss.0000078924.61453.fb (2003).
International Physical Activity Questionnaire (IPAQ). Guidelines for data processing and analysis of the international physical activity questionnaire (IPAQ): Short and long forms. 2005 (accessed 01 July 2020). https://sites.google.com/site/theipaq/.
Han, C. W., Lee, E. J., Iwaya, T., Kataoka, H. & Kohzuki, M. Development of the Korean version of Short-Form 36-Item Health Survey: Health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J. Exp. Med. 203, 189–194 (2004).
Ware, J. E. Jr. & Sherbourne, C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 30, 473–483 (1992).
Oh, T. R. et al. Association between health related quality of life and progression of chronic kidney. Sci. Rep. 9, 1–9 (2019).
Modi, G. K. et al. Nonmedical factors and health-related quality of life in CKD in India. Clin. J. Am. Soc. Nephrol. 15, 191–199 (2020).
Steyerberg, E. W. & Vergouwe, Y. Towards better clinical prediction models: Seven steps for development and an ABCD for validation. Eur. Heart J. 35, 1925–1931. https://doi.org/10.1093/eurheartj/ehu207 (2014).
Cook, R. D. Detection of influential observation in linear regression. Technometrics 19, 15–18. https://doi.org/10.1080/00401706.1977.10489493 (1977).
Palmer, S. et al. Prevalence of depression in chronic kidney disease: Systematic review and meta-analysis of observational studies. Kidney Int. 84, 179–191. https://doi.org/10.1038/ki.2013.77 (2013).
Shirazian, S. et al. Depression in chronic kidney disease and end-stage renal disease: Similarities and differences in diagnosis, epidemiology, and management. Kidney Int. Rep. 2, 94–107. https://doi.org/10.1016/j.ekir.2016.09.005 (2017).
Takasaki, K., Babazono, T., Ishizawa, K., Miura, J. & Uchigata, Y. Relationship between diabetic nephropathy and depression: A cross-sectional analysis using the Diabetes Study from the Center of Tokyo Women’s Medical University (DIACET). BMJ Open Diabetes Res. Care 4, e000310. https://doi.org/10.1136/bmjdrc-2016-000310 (2016).
Abbas Tavallaii, S., Ebrahimnia, M., Shamspour, N. & Assari, S. Effect of depression on health care utilization in patients with end-stage renal disease treated with hemodialysis. Eur. J. Intern. Med. 20, 411–414. https://doi.org/10.1016/j.ejim.2009.03.007 (2009).
Sensky, T., Leger, C. & Gilmour, S. Psychosocial and cognitive factors associated with adherence to dietary and fluid restriction regimens by people on chronic haemodialysis. Psychother. Psychosom. 65, 36–42. https://doi.org/10.1159/000289029 (1996).
Wells, K. B. et al. The functioning and well-being of depressed patients. Results from the medical outcomes study. JAMA 262, 914–919 (1989).
Mishra, S. R., Sharma, A., Bhandari, P. M., Bhochhibhoya, S. & Thapa, K. Depression and health-related quality of life among patients with type 2 diabetes mellitus: A cross-sectional study in Nepal. PLoS ONE 10, e141385. https://doi.org/10.1371/journal.pone.0141385 (2015).
Lee, Y. J., Kim, M. S., Cho, S. & Kim, S. R. Association of depression and anxiety with reduced quality of life in patients with predialysis chronic kidney disease. Int. J. Clin. Pract. 67, 363–368. https://doi.org/10.1111/ijcp.12020 (2013).
Wang, W. L. et al. The prevalence of depression and the association between depression and kidney function and health-related quality of life in elderly patients with chronic kidney disease: A multicenter cross-sectional study. Clin. Interv. Aging 14, 905–913. https://doi.org/10.2147/cia.s203186 (2019).
Steele, T. E. et al. Quality of life in peritoneal dialysis patients. J. Nerv. Ment. Dis. 184, 368–374. https://doi.org/10.1097/00005053-199606000-00007 (1996).
Vazquez, I. et al. Psychosocial factors and quality of life in young hemodialysis patients with low comorbidity. J Nephrol 16, 886–894 (2003).
Tsai, Y. C. et al. Association of physical activity with cardiovascular and renal outcomes and quality of life in chronic kidney disease. PLoS ONE 12, e0183642. https://doi.org/10.1371/journal.pone.0183642 (2017).
Sung, S. A. et al. Sleep duration and health-related quality of life in predialysis CKD. Clin. J. Am. Soc. Nephrol. 13, 858–865. https://doi.org/10.2215/CJN.11351017 (2018).
Alhaji, M. M. et al. Determinants of quality of life as measured with variants of SF-36 in patients with predialysis chronic kidney disease. Saudi Med. J. 39, 653–661 (2018).
Goldney, R. D., Phillips, P. J., Fisher, L. J. & Wilson, D. H. Diabetes, depression, and quality of life: A population study. Diabetes Care 27, 1066–1070. https://doi.org/10.2337/diacare.27.5.1066 (2004).
Leaf, D. E. & Goldfarb, D. S. Interpretation and review of health-related quality of life data in CKD patients receiving treatment for anemia. Kidney Int. 75, 15–24. https://doi.org/10.1038/ki.2008.414 (2009).
Acknowledgements
The authors thank Eun-ji Lim, a research coordinator at the Samsung Biomedical Research Institute, for recruiting all the subjects and collecting the data for this study.
Funding
This study was supported by Genome & Company Co. Ltd (Grant No. PHO0171531).
Author information
Authors and Affiliations
Contributions
J.E.L. was involved in the study design, data collection, analysis, interpretation of results, and writing and review of the manuscript. Y.-J.L. contributed to the interpretation of the data, review of the manuscript and revision of the article for important intellectual content. S.K. was involved in the data collection, analysis, interpretation of results and writing of the manuscript. H.R.J., E.Y.J. and J.J. contributed to the conception and interpretation of the data. W.H., Y.-G.K. and D.J.K. were involved in the interpretation of the data, reviewed the manuscript and provided comments. All authors approved the final version of the manuscript. J.E.L. is the guarantor of this work and, as such, has full access to all of the data from the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, S., Jeon, J., Lee, YJ. et al. Depression is a main determinant of health-related quality of life in patients with diabetic kidney disease. Sci Rep 12, 12159 (2022). https://doi.org/10.1038/s41598-022-15906-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15906-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.