Abstract
IFNα and anti-IFNα autoantibodies have been implicated in susceptibility both for systemic lupus erythematosus (SLE) and viral infection. We aimed to analyze the SLE disease phenotype and risk for infection associated with anti-IFN-α IgG autoantibodies in SLE patients In this multidisciplinary retrospective single referral center study, all consecutive patients with SLE admitted between January 1st and November 30th 2020 were considered. All subjects fulfilled the ACR/EULAR 2019 criteria for SLE. Anti-IFNα IgG autoantibodies were quantified at admission by ELISA. Demographic, medical history, laboratory, treatment, and outcome data were extracted from electronic medical records using a standardized data collection form. 180 patients [female 87.2%, median age of 44.4 (34–54.2) years] were included. The median disease duration was 10 years [4–20] with a median SLEDAI score of 2 [0–4] at study time. Fifty-four (30%) patients had a past-history of lupus nephritis. One hundred and forty-four (80%) had received long-term glucocorticoids and 99 (55%) immunosuppressive drugs. Overall, 127 infections—mostly bacterial and viral—were reported in 95 (52.8%) patients. Twenty SLE patients (11.1%) had positive anti-IFNα IgG autoantibodies with a titer ranging from 10 to 103 UA/mL. Age, sex, SLE phenotype and treatment did not significantly differ between SLE patients with or without anti-IFNα. Infection rate was similar in both groups except for tuberculosis which was more frequent in patients with anti-IFNα (20% vs. 3.1%, p = 0.01). The prevalence of autoantibodies against IFNα is high in SLE and associated with a higher frequency of tuberculosis.
Similar content being viewed by others
Introduction
Type I interferon (mainly IFN-α) has been considered for decades as a pivotal cytokine in SLE1. IFN-α, produced mainly by plasmacytoid dendritic cells2,3, is known to be associated with disease activity, especially in lupus nephritis4 and anti-type I interferon receptor therapy has been shown to be efficient in SLE patients5. Recent reports also brought back to light the presence of IFN-α autoantibodies (anti-IFN-α) in up to 40% of SLE patients6. Interestingly, anti-IFN-α have been shown to alter the interferon signature and may thus be protective in SLE7,8. Anti-IFNα may also predispose to severe COVID-19 by blocking the action of this crucial antiviral cytokine9. Thereby, anti-IFN-α in SLE might on one hand help to control the disease and increase the risk of infection on the other hand10.
In order to give insight into the complex relationship between infection risk, SLE and anti-IFNα, we analyzed both infection history—including COVID-19—and SLE disease phenotype according to anti-IFN-α status.
Material and methods
Population study
All consecutive adult SLE patients admitted between January 1st and November 30th 2020, at Bichat Hospital in 5 distinct Departments of Medicine (Dermatology, Intensive Care Unit, Internal Medicine, Nephrology, and Rheumatology) were selected. Bichat Hospital, Paris, France is a referral national center for rare Autoimmune Diseases. All subjects fulfilled the ACR/EULAR 2019 criteria for Systemic Lupus Erythematosus11.
International Classification of Disease code (ICD-10) for SLE (M32) was used for screening. Data were extracted from the French Diagnosis Related Groups (DRG) based information system (PMSI) databases. Demographic, medical history, biological workup, treatment and follow-up data were retrieved from computerized medical files. Exclusion criteria included inability to confirm SLE after review of medical records and inability to retrieve serum specimens for anti-IFN-α analysis. COVID 19 was defined by a positive SARS-CoV-2 RT-PCR testing on a respiratory sample (nasopharyngeal swab or invasive respiratory sample) or a positive serology N-protein specific IgG without prior vaccination. Other prior infections were based on declared history confirmed by medical records.
Anti-IFNα IgG autoantibodies
The quantification of anti-IFN-α IgG autoantibodies was performed on serum samples draw at admission in the setting of care between January 1st and November 30th 2020. Serum samples were frozen at − 20 °C immediately after collection. Anti-IFN–α IgG were determined by ELISA according to the method described by Bastard et al.9. Plates were coated overnight at 4 °C with 1µg/mL recombinant human interferon-α (rhIFN-α2, Miltenyi Biotec) and incubated with 1:50 dilutions of serum samples from the patients. Horseradish peroxidase conjugate Fc specific anti-human IgG (Sigma) was added, the optical density was measured after addition of the substrate (TMB). Arbitrary units were calculated based on a standard curve obtained with the serum of a patient with known high titer of anti-IFNα autoantibodies. The positivity threshold determined in healthy controls was 10 UA/mL.
Ethical statement
Our study is a human non-interventional retrospective study where 1-study involved products with a marketing authorization that are prescribed in the usual manner and used in accordance with French agencies authorizations, 2-epidemiological methods were used to analyze the data, and 3-information used in the study were collected for clinical care. According to the Public Health French Law (French Research Standard MR-004), approval from institutional review board and written consent are not required for human non-interventional retrospective study. For ethical consideration, patients were however informed that data that was collected in medical records might be used for research study in accordance to privacy rule. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
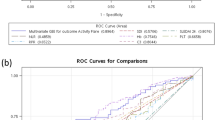
Statistical analysis
Continuous variables are expressed as median [IQR]. Categorical variables are expressed as frequencies and percentages. Data were compared between SLE patients with or without anti-IFN-α by using Fisher’s exact test for nominal variables, χ2 test for continuous variables with normal distribution and Kruskall-Wallis test for continuous non normal variables. We preplanned 4 analyses of COVID-19, viral infections, zoster, and tuberculosis frequency across groups. A Bonferroni correction taking into account these 4 comparisons was used. Statistical analyses were performed using R software.
Results
Characteristics of patients
From January 1st until November 30th 2020, 247 unique SLE patients who had at least an admission in our national referral center (Bichat Hospital, Paris, France) were eligible for the study according to ICD-10 identification. After careful review of individual medical records, the diagnosis of SLE according to ACR/EULAR 2019 criteria was not retained in 67 patients and 180 SLE patients (median age of 44.4 [34–54.2] years, 157 (87.2%) female) were eventually included. Admissions were unplanned (urgent) or planned in 42 (23.3%) and 138 (76.7%) cases, respectively. Unplanned admissions were due to lupus flares (n = 26/42, 61.9%) or infection (n = 7/42, 16.7%) in most cases. Planned admissions were related to SLE follow-up or treatment in 129 (n = 129/138, 93.5%) cases (Fig. S1).
The median SLEDAI disease activity score at admission was 2 [0–4]. Fifty-four (30%) patients had a past history of lupus nephritis. One hundred and forty-four (80%) had received long-term glucocorticoids and 99 (55%) immunosuppressive drugs at some point during follow-up. Steroids were currently prescribed in 62% at a median daily dose of 5 [0–9] mg at study time.
Overall, 127 prior infectious episodes—mainly bacterial (n = 68/127, 53.5%) and viral (n = 40/127, 31.5%)—were reported in 95 (n = 95/180, 52.8%) patients. Viral infection was mostly due to herpes zoster (n = 13/40, 32.5%) and Sars-Cov2 (n = 15/40, 37.5%). Nine (n = 9/180, 5%) patients had tuberculosis (Table 1).
Anti-IFNα IgG autoantibodies
Twenty SLE patients (11.1%) had positive anti-IFNα IgG autoantibodies with a titer ranging from 10 to 103 UA/mL (median = 15). Anti-IFNα autoantibodies were tested overtime in 54 (30%) patients. When identified at baseline (n = 7), anti-IFNα were confirmed during a follow-up in all but 2 cases. When absent at first screening (n = 47), anti-IFNα remained negative in all but 1 case. Age, sex, SLE features or treatment and history of infection including viral infection rates or types did not differ between SLE patients with or without anti-IFNα, except for tuberculosis disease which was more frequent in patients with anti-IFNα (20% vs 3.1%, p = 0.01) (Table 1). In all but 2 cases, TB had occurred a median of 48 [12–168] months before SLE diagnosis in untreated—no immunosuppressive drugs—patients (Table 2).
Discussion
Our study shows that, in a large cohort of carefully characterized SLE patients, 11% are positive for anti-IFNα IgG autoantibodies. This finding is consistent with previous reports on prevalence of anti-INFα antibodies in SLE7,12. Our study confirms the high prevalence of anti-IFNα in SLE as compared to the general population where the prevalence is estimated less than 1%9.
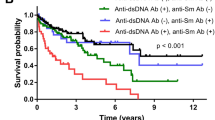
We found no significant correlation between anti-INFα autoantibodies and SLE disease activity. Published results are conflicting since anti-INFα antibodies have been associated with either increased7 or decreased8 lupus activity. The fact that almost all SLE patients in our cohort had low disease activity status may have impeded the proper analysis of anti-INFα impact on SLE activity based on SLEDAI score (Fig. S2). In vitro anti-IFNα autoantibodies inhibit IFNα signaling in SLE7 and may influence the disease phenotype. In our study, auto-immune cytopenia—mostly immune thrombocytopenia (ITP)—tended to be less frequent in SLE patients immunized against IFNα. Interestingly, IFNα and downstream interferon response genes are known to contribute to the pathogenesis of ITP13.
In the general population, neutralizing anti-IFNα IgG autoantibodies are detected in about 10% of patients with severe COVID-199. Anti-IFNα testing may help to identify individuals at high risk of life-threatening infection. Despite a high prevalence of anti-IFNα IgG autoantibodies in SLE and a poor prognosis of severe COVID-19 among patients with SLE14,15, no patients displayed severe COVID-19 in our series.
Anti-IFNα autoantibodies were associated with a higher frequency of TB in our SLE patients. Although SLE patients are known to be at higher risk of TB16, the interconnection of TB, SLE and anti-IFNα autoantibodies is not easy to decipher. First, since TB preceded SLE in most cases, the implication of SLE treatment is unlikely. Second, TB involved the lungs in 2/3 of cases as reported in the general population17. Third, IFNα, in contrast to IFN-γ18, is not known to play a key role in susceptibility for TB. Of note, the breach of tolerance observed in SLE triggers a broad range of autoantibodies including anti-IFNα and IFN-γ7,12 autoantibodies. In human SLE, large case–control studies have shown that autoantibodies—especially antinuclear antibodies—are present in serum months to years before clinical disease onset19. No specific study has addressed the timing of anti-IFNα in the course of SLE. In our study, serial testing over a short period showed that in most SLE patients the anti-IFNα positive or negative status remained stable. Such issues could be addressed prospectively by using serial anti-IFNα testing both in SLE and TB patients.
Our study presents several limitations. First, the study is a retrospective single center study. Second, it has limited power due to the rather limited prevalence of anti-IFNα autoantibodies in SLE even though it is much higher than in the general population. Third, repeated anti-IFNα testing was performed in only a third of patients. Fourth, the neutralizing activity of the autoantibodies on type I IFN was not tested in vitro.
Conclusion
The prevalence of autoantibodies against IFNα is high in SLE and unexpectedly associated with a high frequency of past tuberculosis.
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- ACR:
-
American college of rheumatology
- CNS:
-
Central nervous system
- COVID:
-
Coronavirus infectious disease
- DRG:
-
Diagnosis related groups
- EULAR:
-
European alliance of associations for rheumatology
- F:
-
Female
- GFR:
-
Glomerular filtration rate
- HCQ:
-
Hydroxychloroquine
- ICU:
-
Intensive care unit
- ICD:
-
International classification of disease
- IFN:
-
Interferon
- ITP:
-
Immune thrombocytopenia
- LN:
-
Lymph node
- M:
-
Male
- PMSI:
-
Programme de médicalisation des systèmes d'information
- S:
-
Steroids
- SLE:
-
Systemic lupus erythematosus
- SLEDAI:
-
Systemic lupus erythematosus disease activity index
- TB:
-
Tuberculosis
- VZV:
-
Varicella-zoster virus
References
Crow, M. K. Type I interferon in the pathogenesis of lupus. J Immunol. 192, 5459–5468 (2014).
Jego, G. et al. Plasmacytoid dendritic cells induce plasma cell differentiation through type I interferon and interleukin 6. Immunity 19, 225–234 (2003).
Sacre, K., Criswell, L. A. & McCune, J. M. Hydroxychloroquine is associated with impaired interferon-alpha and tumor necrosis factor-alpha production by plasmacytoid dendritic cells in systemic lupus erythematosus. Arthritis Res Ther. 14, R155 (2012).
Feng, X. et al. Association of increased interferon-inducible gene expression with disease activity and lupus nephritis in patients with systemic lupus erythematosus. Arthritis Rheum. 54, 2951–2962 (2006).
Morand, E. F. et al. Trial of anifrolumab in active systemic lupus erythematosus. N. Engl. J. Med. 382, 211–221 (2020).
Gupta, S., Nakabo, S., Chu, J., Hasni, S. & Kaplan, M. J. Association between anti-interferon-alpha autoantibodies and COVID-19 in systemic lupus erythematosus. medrxiv https://doi.org/10.1101/2020.10.29.20222000 (2020).
Gupta, S. et al. Distinct functions of autoantibodies against interferon in systemic lupus erythematosus: A comprehensive analysis of anticytokine autoantibodies in common rheumatic diseases: Anti-interferon functions in SLE. Arthritis Rheumatol. 68, 1677–1687 (2016).
Morimoto, A. M. et al. Association of endogenous anti-interferon-α autoantibodies with decreased interferon-pathway and disease activity in patients with systemic lupus erythematosus. Arthritis Rheum. 63, 2407–2415 (2011).
Bastard, P., Rosen, L. B. & Zhang, Q., et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 370(6515), eabd4585 (2020).
Mageau, A., Nicaise Roland, P. & Goulenok, T. et al. Systemic lupus erythematosus flare following SARS-CoV2 infection: the implication of IFNα and anti-IFNα autoantibodies. Clin. Exp. Rheumatol. https://doi.org/10.55563/clinexprheumatol/5pubx8. Online ahead of print (2022).
Aringer, M. et al. 2019 European league against rheumatism/American college of rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 71, 1400–1412 (2019).
Slavikova, M. et al. Incidence of autoantibodies against type I and type II interferons in a cohort of systemic lupus erythematosus Patients in Slovakia. J. Interferon Cytokine Res. 23, 143–147 (2003).
Sehgal, K. et al. Plasmacytoid dendritic cells, interferon signaling, and FcγR contribute to pathogenesis and therapeutic response in childhood immune thrombocytopenia. Sci. Transl. Med. 5, 193ra9 (2013).
Mageau, A. et al. SARS-CoV-2 infection among inpatients with systemic lupus erythematosus in France: a nationwide epidemiological study. Ann. Rheum. Dis. 80, 1101–1102 (2021).
Mageau, A. et al. Survival after COVID-19-associated organ failure among inpatients with systemic lupus erythematosus in France: A nationwide study. Ann. Rheum. Dis. 81, 569–574 (2022).
Pego-Reigosa, J. M. et al. The risk of infections in adult patients with systemic lupus erythematosus: systematic review and meta-analysis. Rheumatology (Oxford) 60, 60–72 (2020).
Furin, J., Cox, H. & Pai, M. Tuberculosis. Lancet 393, 1642–1656 (2019).
Boisson-Dupuis, S. et al. Inherited and acquired immunodeficiencies underlying tuberculosis in childhood. Immunol. Rev. 264, 103–120 (2015).
Arbuckle, M. R. et al. Development of autoantibodies before the clinical onset of systemic lupus erythematosus. N Engl. J. Med. 349, 1526–1533 (2003).
Funding
Funding is provided by French Agence Nationale de la Recherche (ANR) [grants # ANR-21-COVR-0034 COVALUS] to Karim Sacre.
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. K.S. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design: MB, PNR, KS. Acquisition of data: M.B., P.N.R., C.F., E.D., V.D., P.D., D.D., T.G., F.F., P.M., J.F.T., T.P., K.S. Analysis and interpretation of data: M.B., P.N.K., A.M., C.F., K.S.
Corresponding author
Ethics declarations
Competing interests
The authors declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Beydon, M., Nicaise-Roland, P., Mageau, A. et al. Autoantibodies against IFNα in patients with systemic lupus erythematosus and susceptibility for infection: a retrospective case-control study. Sci Rep 12, 11244 (2022). https://doi.org/10.1038/s41598-022-15508-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15508-9
This article is cited by
-
Tuberculosis remains a leading contributor to morbidity due to serious infections in Indian patients of SLE
Clinical Rheumatology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.