Abstract
Metabolic syndrome and lumbar spinal stenosis (LSS) are common age-related diseases. However, the causal relationship between them remains unclear. This study aimed to identify the effects of LSS on metabolic syndrome incidence in community-dwelling adults. This prospective cohort study included participants of the Aizu cohort study (LOHAS) aged < 75 years as of 2008. Participants with metabolic syndrome at baseline were excluded. The primary outcome measure was metabolic syndrome incidence, and the main explanatory variable was the presence of LSS, as assessed by a self-reported questionnaire. A multivariate Cox proportional hazard regression model was used to estimate hazard ratios (HRs) for metabolic syndrome incidence during the 6-year follow-up period. Complete-case analyses were compared with the multiple imputation results. Among 1599 participants, 1390 complete cases were analyzed (mean [SD] age 62.3 [9.0] years; females, 734 [52.8%]). Among those participants, 525 (37.8%) developed metabolic syndrome during the follow-up of 3.89 [1.96] years. The presence of LSS was associated with developing metabolic syndrome (HR, 1.41; 95% confidence interval [CI] 1.02–1.95). Multiple imputation results showed similar trends of those having complete-case data (HR, 1.47; 95% CI 1.08–2.00). This finding suggests the importance of prevention and management of LSS in community settings.
Similar content being viewed by others
Introduction
Metabolic syndrome, also known as syndrome X or the deadly quartet1, is a combination of several metabolic abnormalities. It is a major risk factor for cardiovascular diseases and a leading cause of morbidity and mortality2. Metabolic syndrome incidence in developed countries increases with age, occurring particularly in those older than 40 years3,4. Aging is also commonly associated with musculoskeletal disorders. Such an important disorder is lumbar spinal stenosis, an age-related degenerative condition in which changes occur in the discs and facet joints. The disease involves lower extremity pain, numbness, or weakness5,6. Studies have shown that the prevalence of lumbar spinal stenosis increases with age and is estimated to be 1.9% in respondents aged 40–49 years, 4.8% in those aged 50–59 years, 5.5% in those aged 60–69 years, and 10.8% in those aged 70–79 years7.
Although metabolic syndrome and lumbar spinal stenosis are common diseases whose prevalence increases with age, they are often considered separately due to their different symptoms and pathologies. Recent research has reported the coexistence of lumbar spinal stenosis and lifestyle-related diseases, such as diabetes mellitus, peripheral artery disease, hypertension, and heart disease8,9,10,11. However, these were not prospective studies, rather cross-sectional studies that did not identify causal relationships.
We hypothesized that lumbar spinal stenosis was a risk factor for metabolic syndrome due to extremely sedentary behavior, and the inability to meet the guidelines for physical activity12 could lead to metabolic syndrome. This study aimed to identify a longitudinal association between lumbar spinal stenosis and the incidence of metabolic syndrome in community-dwelling adults.
Methods
Study population
This prospective cohort study was based on the Locomotive Syndrome and Health Outcomes in the Aizu Cohort Study (LOHAS), with a follow-up time of up to 6 years. The LOHAS was designed in 2008 to investigate the risk of cardiovascular disease, quality of life, medical costs, and mortality attributable to locomotor dysfunction. The study recruited community-dwelling individuals from the towns of Minami-Aizu and Tadami in Fukushima Prefecture, Japan who were enrolled in a National Health Insurance plan and who participated in annual health checkups (specific health checkups targeting individuals aged < 75 years) conducted by their local governments. Both towns are in valleys surrounded by mountains, and the main industry in the region is agriculture. A detailed study protocol was provided in previous publications13,14. The LOHAS baseline survey included 2725 participants. The inclusion criteria for this study were having participated in the LOHAS and being aged < 75 years. The exclusion criteria were as follows: participants for whom metabolic syndrome could not be assessed at baseline owing to missing components for evaluating metabolic syndrome, those without at least one annual special health checkup until 2014, or those with metabolic syndrome at baseline. The study protocol was approved by the Research Ethics Committee of Fukushima Medical University School of Medicine and was performed in accordance with the ethical standards established in the 1964 Declaration of Helsinki and its later amendments. All participants provided written informed consent before participating in the study.
Baseline survey
Special health checkups and questionnaires were provided at the baseline survey. All assessments were performed between April and July 2008. Each participant underwent all examinations on the same day. Special health checkups included an interview for medical history and lifestyle habits such as smoking and drinking status; measurement of weight, height, and blood pressure; physical examination; and blood chemistry tests for serum triglyceride, serum total cholesterol, serum low high-density lipoprotein cholesterol, hemoglobin A1c, and other parameters, with no instructions to fast beforehand. The baseline self-reported questionnaire for participants included information on the following characteristics: marital status, job status, dietary habits, physical activity, health-related quality of life, and locomotor dysfunction.
Definitions of metabolic syndrome
Metabolic syndrome was defined as the presence of three or more of the following risk factors15, identified during the annual special or standard health checkups: (1) enlarged waist circumference (≥ 80 cm in females or ≥ 90 cm in males); (2) increased triglyceride level (≥ 150 mg/dL, or taking a drug prescribed for high triglycerides); (3) low high-density lipoprotein cholesterol (< 50 mg/dL in females or < 40 mg/dL in males, or taking drugs prescribed for low high-density lipoprotein cholesterol); (4) elevated blood pressure (systolic blood pressure ≥ 130 and/or diastolic blood pressure ≥ 85 mmHg, or receiving antihypertensive drug treatment); (5) elevated glucose (hemoglobin A1c levels ≥ 5.6% or receiving a drug prescribed for elevated glucose).
Main explanatory variable
The main explanatory variable was lumbar spinal stenosis, which was identified using a self-reported questionnaire, developed as a diagnostic support tool for lumbar spinal stenosis16. This questionnaire consisted of 10 items (Q1–Q10). According to the clinical prediction rule, those with a total score of ≥ 4 points in Q1–Q4 or a score of ≥ 1 in Q1–Q4 and ≥ 2 in Q5–Q10 were identified as positive for the presence of lumbar spinal stenosis. The sensitivity and specificity of the positive criteria in a validation dataset were 84% and 78%, respectively.
Other variables
In the special health checkup or health checkup, height and weight were measured, and the body mass index (BMI) was calculated. We recorded data on age, sex (male or female), smoking status (current or never/former), and drinking habits (every day, sometimes, rarely, or never). Data collected by questionnaires included information on employment (yes or no) and the number of metabolic syndrome components at baseline (0, 1, or 2). We also recorded the mental health domain score on the SF-36 Health Survey (higher score indicates better mental health)17 and the level of physical activity as assessed by the Japanese version of the International Physical Activity Questionnaire (IPAQ)18. The IPAQ is one of the most widely used physical activity evaluation tools in the world, and responses to the questionnaire were classified as low, moderate, or high activity, according to the scoring program19.
Statistical analysis
The baseline demographics were summarized. Continuous variables are presented as mean and SD, and categorical variables as frequency and percentage. The t-test and chi-squared test analyzed continuous and categorical variables, respectively. The follow-up was managed as an annual special or standard health checkup. The endpoint of the present study was the development of metabolic syndrome or the last health checkup.
Cox proportional hazard regression univariable and multivariable models were used to calculate the hazard ratio (HR) and 95% confidence interval (CI) for metabolic syndrome incidence during the 6-year follow-up in association with lumbar spinal stenosis at baseline. After unavailable analysis, we performed a multivariable analysis that included age, sex, smoking status, alcohol consumption, number of metabolic syndrome components at baseline, and mental health as confounding factors. In the sub-analysis, the incidence of each of the five metabolic syndrome components and obesity (BMI ≥ 25 kg/m2) was analyzed in the participants by a multivariable Cox proportional hazard regression model. The outcome variables were the incidence of each of the five components or obesity during the annual special health checkups or health checkups results. The explanatory variables were the same components at baseline, lumbar spinal stenosis, and possible confounding factors (age, sex, smoking status, alcohol consumption, number of metabolic syndrome components at baseline, and mental health). A subgroup analysis stratifying participants by age (< 65 years and ≥ 65 years) was also performed.
Selection bias and loss of information due to missing data in the primary explanatory variables and covariates were managed by multiple imputations under the missing at random assumption as sensitivity analysis20. The variables used in the regression or logistic regression analyses were used to generate 20 imputed datasets. Rubin’s rules were applied to combine the estimates and standard errors21.
We also compared the complete-case analyses with the multiple imputation results. All analyses were performed using STATA, Version 17.0 (StataCorp, College Station, TX, USA). All tests were two-tailed.
Results
Participant characteristics
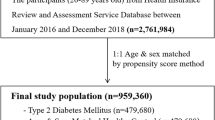
A flowchart of the analyzed population is shown in Fig. 1. Of the 2725 participants, 1126 were excluded, leaving 1599 subjects for this study. Of these, 1390 participants were analyzed as complete cases having no missing data. The characteristics of the study population compared based on the presence of lumbar spinal stenosis are summarized in Table 1. The mean (SD) age was 62.3 (9.0) years, and 734/1390 (52.8%) participants were females. Lumbar spinal stenosis was more prevalent in subjects with enlarged waist circumference and obesity at baseline (Table 2).
Metabolic syndrome incidence in the overall case analysis
The cumulative incidence of metabolic syndrome during the 3.89 (1.96) years follow-up period was 525 (37.8%). The relationship between lumbar spinal stenosis and metabolic syndrome incidence is shown in Table 3. The presence of lumbar spinal stenosis in participants without metabolic syndrome at baseline was associated with the development of metabolic syndrome in the univariable Cox regression model (HR, 1.48; 95% CI 1.08–2.05). The association between the presence of lumbar spinal stenosis and metabolic syndrome development persisted even after adjusting for possible confounders (HR, 1.41; 95% CI 1.02–1.95). The presence of lumbar spinal stenosis in participants without metabolic syndrome at baseline in the group aged < 65 years was associated with the development of metabolic syndrome in the multivariable Cox regression model (HR, 2.28; 95% CI 1.38–3.75; Supplementary Table S1), while participants aged ≥ 65 years showed no association (HR, 1.06; 95% CI 0.69–1.63; Supplementary Table S2).
Incidence of metabolic syndrome components and obesity in the overall case analysis
Of the five metabolic syndrome components and obesity, the risk for new occurrence of enlarged waist circumference and elevated triglyceride during follow-up was higher in patients with lumbar spinal stenosis at baseline than in those without (adjusted HR, 1.93; 95% CI 1.06–3.49 and adjusted HR, 1.49; 95% CI 1.04–2.13, respectively; Table 4).
Incidence of metabolic syndrome in the multiple imputations analysis
The results from multiple imputations and complete cases showed similar trends. The presence of lumbar spinal stenosis in participants without metabolic syndrome at baseline influenced the incidence of metabolic syndrome in the univariable and multivariable Cox regression models (univariable model: HR, 1.51; 95% CI 1.11–2.06; multivariable model: HR, 1.47; 95% CI 1.08–2.00; Supplementary Table S3).
Discussion
We prospectively investigated the association between lumbar spinal stenosis and the incidence of metabolic syndrome in community-dwelling adults. Our study identified lumbar spinal stenosis as a risk factor for metabolic syndrome incidence.
To our knowledge, this was the first study to prospectively analyze the relationship between lumbar spinal stenosis and metabolic syndrome in a community setting. Additionally, we determined that triglyceride levels, a component of metabolic syndrome, was associated with lumbar spinal stenosis. Our results also revealed a similar trend for enlarged waist circumstance. Previous cross-sectional studies have shown an association between lumbar spinal stenosis and lifestyle-related diseases, although the definitions differed between studies. Lotan et al.22 investigated 537 patients with spinal stenosis in a hospital setting. Hypertension (23.2 vs. 7.8%) and diabetes mellitus (13.6 vs. 5.9%) were more prevalent in the study group than the general population. In another study of 395 patients diagnosed with spinal stenosis, degenerative disk disease, or osteoporotic vertebral fractures, patients in the spinal stenosis group had a significantly higher rate of diabetes mellitus than the other groups23. Uesugi et al.11 investigated the relationship between lumbar spinal stenosis and comorbidities in 526 patients with lumbar spinal stenosis in a community setting. The results showed significant associations between diabetes mellitus and high blood pressure and lumbar spinal stenosis. Maeda et al.8 also showed that diabetes mellitus and low ankle-brachial index values were significantly associated with lumbar spinal stenosis. Our results differed from those of previous studies, all of which were cross-sectional. Lower cumulative incidence during study periods may be affected because of the longitudinal study design. The commutative incidence of BMI (112/1052; 10.6%), lower high-density lipoprotein cholesterol levels (98/1352; 7.2%), and elevated glucose levels (107/1157; 9.2%) was lower than that of waist circumference (159/804; 19.5%) or triglyceride levels (377/1292; 29.2%) (Table 4). Our results provide further understanding regarding these relationships, although additional research is warranted.
Our study showed that the presence of lumbar spinal stenosis was associated with the incidence of metabolic syndrome in only participants aged < 65 years. Previous Asian-based studies24,25 have reported that the prevalence of metabolic syndrome peaks at the age of 60–70 years, while the number of geriatric syndromes, such as delirium, falls, incontinence, and frailty, increases in those aged ≥ 65 years26. This suggests that there may be a diversity of factors associated with metabolic syndrome in older age. The effect of lumbar spinal stenosis on metabolic syndrome may be reduced in individuals aged ≥ 65 years.
As an etiological explanation for our results, low physical activity might mediate the association between lumbar spinal stenosis and metabolic syndrome. Norden et al.12 investigated physical activity using an accelerometer in 75 patients with lumbar spinal stenosis. Most participants were extremely sedentary and did not meet the guidelines for physical activity. Patients with degenerative musculoskeletal disorders are limited in their walking ability27, and physical activity is decreased in community-dwelling older individuals with musculoskeletal pain28. It is known that low levels of physical activity and sedentary behavior lead to lifestyle-related diseases in middle-aged and older people29,30. Several studies showed reverse causality between lumbar spinal stenosis and/or lower back pain and lifestyle-related diseases. One review showed that as arteriosclerosis due to hypertension and dyslipidemia progresses, posterior aortic wall calcification occurs, leading to the progression of intervertebral disc degeneration31. Other studies found that diabetes mellitus leads to pathological changes and early joint degeneration32,33. Research on the relationship between lumbar spinal stenosis and lifestyle-related diseases searches for causation; however, further research is needed to find whether direct, indirect, or lifestyle factors exist.
Although the etiological relationship between lumbar spinal stenosis and metabolic syndrome has not been clarified, this study aimed to investigate one aspect of the relationship between them in a long-term community-dwelling cohort. Despite the important findings of this study, several limitations should be considered. First, there might be information bias in this study. We used a questionnaire, a non-objective assessment tool, to identify lumbar spinal stenosis. The sensitivity and specificity of this questionnaire were 84% and 78%, respectively16. Some of the participants reporting having lumbar spinal stenosis may not have actually been diagnosed with lumbar spinal stenosis. We think, however, that using this questionnaire was the best way to test our hypothesis in a community setting. The definition of metabolic syndrome has been modified and changed over time. Although we used the most recent definition available at the time of the study, these relationships could become unstable in the future. Second, we had no data on treatments for lumbar spinal stenosis and did not follow-up on lumbar spinal stenosis symptoms. Some of the participants identified as having lumbar spinal stenosis might have sought care and treatment for the condition. Since we hypothesized that lumbar spinal stenosis at baseline was associated with the incidence of metabolic syndrome, improvements in spinal symptoms may have protected them from the incidence of metabolic syndrome. The results of this study are not overestimated. Third, we stratified follow-up by years, not months and/or days. As special health checkups or health checkups were held frequently, the impact of time was small. Fourth, as this was an observational study; therefore, there might be other potential biases between lumbar spinal stenosis and metabolic syndrome. Finally, this study was conducted in a small area in Japan. Therefore, the generalizability of our results should be carefully considered. Further studies are required to validate and generalize the results of this study.
Conclusion
We prospectively investigated the association between lumbar spinal stenosis and metabolic syndrome incidence. Lumbar spinal stenosis was identified as a risk factor for metabolic syndrome occurrence. By maintaining an appropriate physical activity level and moderate exercise, it is possible to prevent the occurrence of metabolic syndrome. The study findings provide useful information for the prevention and management of the metabolic syndrome. We recommend conducting an etiological study that would include a comparison using objective measures in lumbar spinal stenosis and metabolic syndrome or a study to determine how decreasing physical activity due to lumbar spinal stenosis mediates the incidence of metabolic syndrome.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to ethical restrictions, however further analyses may be completed by the authors on reasonable request.
References
Eckel, R. H., Grundy, S. M. & Zimmet, P. Z. The metabolic syndrome. Lancet (London, England) 365, 1415–1428 (2005).
Dominguez, L. J. & Barbagallo, M. The biology of the metabolic syndrome and aging. Curr. Opin. Clin. Nutr. Metab. Care 19, 5–11 (2016).
Scuteri, A. et al. Metabolic syndrome across Europe: Different clusters of risk factors. Eur. J. Prev. Cardiol. 22, 486–491 (2015).
Aguilar, M., Bhuket, T., Torres, S., Liu, B. & Wong, R. J. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA 313, 1973–1974 (2015).
Katz, J. N. & Harris, M. B. Clinical practice. Lumbar spinal stenosis. N. Engl. J. Med. 358, 818–825 (2008).
Katz, J. N. et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheumatism. 38, 1236–1241 (1995).
Yabuki, S. et al. Prevalence of lumbar spinal stenosis, using the diagnostic support tool, and correlated factors in Japan: A population-based study. J. Orthop. Sci. 18, 893–900 (2013).
Maeda, T. et al. Factors associated with lumbar spinal stenosis in a large-scale, population-based cohort: The Wakayama Spine Study. PLoS ONE 13, e0200208 (2018).
Asadian, L., Haddadi, K., Aarabi, M. & Zare, A. Diabetes mellitus, a new risk factor for lumbar spinal stenosis: A case-control study. Clin. Med. Insights Endocrinol. Diabetes 9, 1–5 (2016).
Sekiguchi, M. et al. Relationship between lumbar spinal stenosis and psychosocial factors: A multicenter cross-sectional study (DISTO project). Eur. Spine J. 24, 2288–2294 (2015).
Uesugi, K., Sekiguchi, M., Kikuchi, S. & Konno, S. Relationship between lumbar spinal stenosis and lifestyle-related disorders: A cross-sectional multicenter observational study. Spine (Phila Pa 1976) 38, E540-545 (2013).
Norden, J., Smuck, M., Sinha, A., Hu, R. & Tomkins-Lane, C. Objective measurement of free-living physical activity (performance) in lumbar spinal stenosis: Are physical activity guidelines being met?. Spine J. 17, 26–33 (2017).
Otani, K. et al. Locomotor dysfunction and risk of cardiovascular disease, quality of life, and medical costs: Design of the Locomotive Syndrome and Health Outcome in Aizu Cohort Study (LOHAS) and baseline characteristics of the study population. J. Orthop. Sci. 17, 261–271 (2012).
Ono, R. et al. Gender difference in association between low back pain and metabolic syndrome: Locomotive syndrome and health outcome in Aizu cohort study (LOHAS). Spine (Phila Pa 1976) 37, 1130–1137 (2012).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
Konno, S. et al. A diagnostic support tool for lumbar spinal stenosis: A self-administered, self-reported history questionnaire. BMC Musculoskelet. Disord. 8, 102 (2007).
Yamazaki, S., Fukuhara, S. & Green, J. Usefulness of five-item and three-item Mental Health Inventories to screen for depressive symptoms in the general population of Japan. Health Qual. Life Outcomes 3, 48 (2005).
Murase, N., Katsumura, T., Ueda, C., Inoue, S. & Shimomitsu, T. Validity and reliability of Japanese version of International Physical Activity Questionnaire [in Japanese]. J. Health Welfare Stat. 49, 1–9 (2002).
Lee, P. H., Macfarlane, D. J., Lam, T. H. & Stewart, S. M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act 8, 115 (2011).
Rubin, D. B. & Schenker, N. Multiple imputation in health-care databases: An overview and some applications. Stat. Med. 10, 585–598 (1991).
Rubin, D. B. Multiple Imputation for Nonresponse in Surveys (Wiley, 2011).
Lotan, R., Oron, A., Anekstein, Y., Shalmon, E. & Mirovsky, Y. Lumbar stenosis and systemic diseases: Is there any relevance?. J. Spinal Disord. Tech. 21, 247–251 (2008).
Anekstein, Y. et al. Diabetes mellitus as a risk factor for the development of lumbar spinal stenosis. Israel Med. Assoc. J. IMAJ 12, 16–20 (2010).
Ge, H. et al. The prevalence and associated factors of metabolic syndrome in Chinese aging population. Sci. Rep. 10, 20034 (2020).
Hirode, G. & Wong, R. J. Trends in the prevalence of metabolic syndrome in the United States, 2011–2016. JAMA 323, 2526–2528 (2020).
O’Caoimh, R. et al. Prevalence of frailty in 62 countries across the world: A systematic review and meta-analysis of population-level studies. Age Ageing 50, 96–104 (2021).
Winter, C. C. et al. Walking ability during daily life in patients with osteoarthritis of the knee or the hip and lumbar spinal stenosis: A cross sectional study. BMC Musculoskelet. Disord. 11, 233 (2010).
Murata, S. et al. Association between objectively measured physical activity and the number of chronic musculoskeletal pain sites in community-dwelling older adults. Pain Med. (Malden, Mass.) 20, 717–723 (2019).
Joseph, J. J. et al. Physical activity, sedentary behaviors and the incidence of type 2 diabetes mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA). BMJ Open Diabetes Res. Care 4, e000185 (2016).
Oliveira, R. G. & Guedes, D. P. Physical activity, sedentary behavior, cardiorespiratory fitness and metabolic syndrome in adolescents: Systematic review and meta-analysis of observational evidence. PLoS ONE 11, e0168503 (2016).
Kauppila, L. I. Atherosclerosis and disc degeneration/low-back pain—A systematic review. Eur. J. Vasc. Endovasc. Surg. 37, 661–670 (2009).
Brownlee, M. Biochemistry and molecular cell biology of diabetic complications. Nature 414, 813–820 (2001).
Selvarajah, D. et al. Early involvement of the spinal cord in diabetic peripheral neuropathy. Diabetes Care 29, 2664–2669 (2006).
Acknowledgements
We thank the staff of the Tadami Town Office, Minamiaizu Town Office, and Institute for Health Outcomes and Process Evaluation Research for their help with participant recruitment and data acquisition. We also thank all subjects who agreed to participate in this study.
Author information
Authors and Affiliations
Contributions
Study concept and design: R.O., M.T., Y.Y., K.O., S.Y., S.F. Acquisition of data: K.O., M.S. Analysis and interpretation of data: R.O., M.T., Y.Y., S.Y., S.K., S.K., S.F. Drafting of the manuscript: all authors. Critical revision of the manuscript for important intellectual content: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ono, R., Takegami, M., Yamamoto, Y. et al. Impact of lumbar spinal stenosis on metabolic syndrome incidence in community-dwelling adults in Aizu cohort study (LOHAS). Sci Rep 12, 11246 (2022). https://doi.org/10.1038/s41598-022-15173-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15173-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.