Abstract
Stay-at-home restrictions such as closure of non-essential businesses were effective at reducing SARS-CoV-2 transmission in New York City (NYC) in the spring of 2020. Relaxation of these restrictions was desirable for resuming economic and social activities, but could only occur in conjunction with measures to mitigate the expected resurgence of new infections, in particular social distancing and mask-wearing. We projected the impact of individuals’ adherence to social distancing and mask-wearing on the duration, frequency, and recurrence of stay-at-home restrictions in NYC. We applied a stochastic discrete time-series model to simulate community transmission and household secondary transmission in NYC. The model was calibrated to hospitalizations, ICU admissions, and COVID-attributable deaths over March–July 2020 after accounting for the distribution of age and chronic health conditions in NYC. We projected daily new infections and hospitalizations up to May 31, 2021 under the different levels of adherence to social distancing and mask-wearing after relaxation of stay-at-home restrictions. We assumed that the relaxation of stay-at-home policies would occur in the context of adaptive reopening, where a new hospitalization rate of ≥ 2 per 100,000 residents would trigger reinstatement of stay-at-home restrictions while a new hospitalization rate of ≤ 0.8 per 100,000 residents would trigger relaxation of stay-at-home restrictions. Without social distancing and mask-wearing, simulated relaxation of stay-at-home restrictions led to epidemic resurgence and necessary reinstatement of stay-at-home restrictions within 42 days. NYC would have stayed fully open for 26% of the time until May 31, 2021, alternating reinstatement and relaxation of stay-at-home restrictions in four cycles. At a low (50%) level of adherence to mask-wearing, NYC would have needed to implement stay-at-home restrictions between 8% and 32% of the time depending on individual adherence to social distancing. At moderate to high levels of adherence to mask-wearing without social distancing, NYC would have needed to implement stay-at-home restrictions. In threshold analyses, avoiding reinstatement of stay-at-home restrictions required a minimum of 60% adherence to mask-wearing at 50% adherence to social distancing. With low adherence to mask-wearing and social distancing, reinstatement of stay-at-home restrictions in NYC was inevitable. High levels of adherence to social distancing and mask-wearing could have attributed to avoiding recurrent surges without reinstatement of stay-at-home restrictions.
Similar content being viewed by others
Introduction
In March 2020, New York City (NYC) became the epicenter of the COVID-19 epidemic, accounting for more than one-third of the total confirmed cases in the US. Two weeks after the first case was reported in NYC, Governor Cuomo declared stay-at-home restrictions that included banning large gatherings and closing schools and non-essential businesses1,2. Facial mask-wearing in public became mandatory in mid-April3. Following the introduction of these policies, the daily reported new cases in NYC declined to fewer than 700 per day in early June, down from over 10,000 cases per day at the peak of the epidemic in April 2020.
New York State (NYS) implemented tiered reopening guidance between early June and late September, first reopening industries such as construction and manufacturing, followed by in-store retail, outdoor and indoor dining, and elementary schools, all at limited capacity4. However, due to a concern for a potential resurgence of cases, the reopening in each region of the state was contingent on meeting several criteria, including maintaining < 2 new daily hospitalizations per 100,000 residents, and > 30% hospital and ICU bed capacity region-wide. The state-wide policy required ongoing monitoring of these metrics, and recommended the reinstatement of restrictions in a given region if the criteria were exceeded5.
Mask-wearing and social distancing are the two critical measures to mitigate the transmission of respiratory diseases5,6. Two meta-analyses of respiratory diseases caused by coronaviruses, including Severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and SARS-CoV-2, demonstrated that mask-wearing and social distancing effectively reduced viral transmission7,8. Using a natural experiment examining the association between the state-wide mandate orders for face cover in public and the daily confirmed COVID-19 cases from all states, a study reported that community-wide mask-wearing could have accounted for declines in COVID-19 growth rates in the US during Spring 20209. Mathematical modeling of SARS-CoV-2 in New York and elsewhere have estimated the extent to which mask-wearing reduces population-level transmission10 but has not examined the impact in the context of reinstatement or relaxation of stay-at-home restrictions upon reopening. High adherence to mask-wearing and social distancing may allow the city to reopen by controlling the epidemic, and avoiding surges in cases and hospitalizations thus consequential reinstatement of stay-at-home restrictions.
In this study, we used mathematical modeling to examine the impact of individual adherence to social distancing and mask-wearing on COVID-19 epidemic and duration, frequency, and recurrence of stay-at-home restrictions in NYC. The study findings can have important implications for settings with limited vaccine availability or other emerging infectious diseases in the period when only non-pharmaceutical interventions are available.
Methods
Mathematical model
We adapted an existing stochastic, discrete-time model of community transmission of SARS-CoV-211,12 by adding a lagged transmission of community-acquired infections to household members and a compartment to represent quarantine of those who have received testing or contact tracing. We measured outcomes of infections, hospitalizations, and deaths as well as duration, frequency, and recurrence of stay-at-home restrictions by May 31, 2021. The revised model structure has been presented elsewhere12. Briefly, the model represents individuals who are susceptible (S), exposed (E), infectious (I), quarantined (Q), or removed/recovered (R).
The model structures are described as following:
where \({\uprho }_{3} {\text{ is min}}\left( {1, \frac{\lambda *\kappa }{\mu }} \right)*\left( {\theta - min\left( {\rho_{1} + \rho_{2} , \theta } \right)} \right)\) and \(P\ \text{ is}\ \rho_{1} + \rho_{2} + \rho_{3}\). All parameters are described in Table 1. In NYC, zt is the number of importations on day t, which was set to 7 on January 15th and 7 on February 22nd for the importations linked to the initial outbreak in Wuhan and other global importations, respectively, and one to represent the initial case found in NYC. The transmission in the model was stochastic with a log-normal distribution with a standard deviation of 0.722 (\(p)\), a value determined based on Seattle’s 2018–2019 influenza season11.
In addition, we assumed a secondary attack rate of 25% for within-household transmission after March 17, 2020 when stay-at-home policies were instated19. The model accounted for age-specific and comorbidity-adjusted infection-fatality ratio (IFR). We calculated the age-specific IFR adjusting for the increased severity for hospitalizations and deaths among those with underlying comorbidities by age groups (10–19; 20–29; 30–39; 40–49; 50–59; 60–69; 70–79; 80 + years). IFR was inferred from the case-fatality ratio in South Korea by mid-March 2020 (1.01%). Given that the testing and contact tracing were widely conducted in Korea, we assumed that CFR would provide a reasonable approximation for IFR. By early March, ~ 95% of the contacts of the confirmed index cases related to the main outbreak cluster in Daegu, Korea, which accounted for > 79% all confirmed cases in Korea, were traced and tested20. Therefore, we assumed the IFR would be slightly lower by 5%, resulting in the overall IFR estimate of 0.94. Then, we estimated the IFR in NYC adjusting for the age and comorbidities distribution in NYC. The model was implemented in Python 3.7 and outputs were analyzed and graphed using R 3.6.1.
Model assumptions and calibration
The model used NYC’s distribution of age and chronic condition, obtained from New York Behavioral Risk Factor Surveillance System Data in 201721 and 2013–2014 New York City Health and Nutrition Examination Survey (NYC HANES)22, and census23 to estimate the impact of the epidemic on COVID-19 hospitalization and mortality. We assumed that the average time from infection to symptom onset to be 5.1 days24, and from symptom onset to hospitalization to be 11 days25. Based on the information provided by the NYC Department of Health and Mental Hygiene (DOHMH) during the early epidemic by April 2020, the average lengths of stay at hospitals among non-intensive care unit (ICU) admitted patients were assumed to be 11 days. Critically ill patients were assumed to be first admitted to non-ICU hospital beds for three days, then transferred to the ICU for 21 days before returning to non-ICU hospital beds for another 14 days. Given the absence of effective interventions in the early epidemic, we assumed that 28.8% of the hospitalized would die, with an average length of ICU stay of 2 days before death25. In addition, the model was conducted in the context of no available vaccinations, given the timeline of vaccine development. Table 2 shows the list of parameters with uncertainty ranges. In sensitivity analysis, we varied the key parameters across the uncertainty ranges and measured the cumulative deaths (Figure S1).
The model was calibrated to the publicly available data on daily new hospitalizations for COVID-19 and confirmed and probable data COVID-19 attributable deaths from the NYC DOHMH and the internal data on daily number of patients with COVID-19 in ICUs from the NYS Department of Health’s Hospital Emergency Response Data System (HERDS). The data for HERDS data was self-reported by hospitals. An effective reproduction number (Re) was adjusted to minimize the sum of squared residuals between these data and their corresponding model outputs. The daily hospitalization data in mid-April was updated later with more certainty, and this update increased reported hospitalizations by 30% in the two months following the initial report. Therefore, when calibrating the model, we raised the upper 95% confidence interval to allow for up to 30% under-reporting of daily new hospitalizations and number of patients with COVID-19 in ICUs. New daily cases of COVID-19 were not used as a target for calibration due to changing testing eligibility and accessibility throughout the period of analysis. However, the calibration was constrained to ensure that new infections in the simulation must exceed the number of new cases identified through testing.
We estimated the initial reproduction number (R0) at the beginning of the epidemic in NYC and the Re after the pandemic peak of March–April 2020. The estimated Re under subsequent relaxation of stay-at-home restrictions was obtained by propagating the uncertainty in the initial R0 while maintaining fixed benchmarks for possible levels of mask-wearing and social distancing. On June 1, 2020, NYC launched a new contact-tracing program, NYC Test & Trace Corps, hiring 3,000 contact tracers and set a target of carrying out 50,000 daily tests16,17,37. Based on these data, we assumed that a citywide random daily testing of 50,000 and contact tracing program with 3000 tracers from June 1, 2020 to May 31, 2021. We assumed that each tracer could successfully trace two contacts of an index case per day, and that contacts were quarantined for an average of four days after being infectious (i.e., half of the average infectious period of eight days). All methods were performed in accordance with the relevant guidelines and regulations.
Model scenarios for adherence to social distancing and mask-wearing
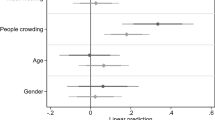
We simulated model scenarios in which relaxation of stay-at-home restrictions occurred with different degrees of individual adherence to social distancing and mask-wearing. At one extreme, we simulated a return to pre-pandemic activity with no social distancing or mask-wearing. Social distancing was represented as keeping 6 feet of distance from others. We applied the effect of inter-person spacing on SARS-CoV-2 transmission from a meta-analysis of close contact events8 where the risk of transmission from an infected individual was reduced by 2.02 times per additional 1 m distance. Social distancing scenarios assumed that 50% of population would maintain 6 feet of distance with all contacts outside the household. We further assumed four different levels of adherence to mask-wearing. Two recent meta-analyses estimated that wearing any face masks including surgical masks, 12–16 layer cotton masks, or N95 respirators reduces transmission by 65–85%7,8. We conservatively used the lower estimate of 65% as a benchmark for mask efficacy. This was further modified by the estimated proportion of individuals wearing masks outside the home, estimated at between 65% and 89% in surveys in NYC and elsewhere38,39,40,41. Given that the impact of mask-wearing would greatly vary by population coverage and adherence, we varied the percentage of adherence to wearing any mask correctly at 50%, 70%, and 90% to represent low, moderate, and high adherence38,39,40,41.
Thresholds to reinstate or relax stay-at-home restrictions
We incorporated the guidelines from NYS health authorities for the conditions under which regional stay-at-home restrictions could be relaxed or needed to be reinstated5. We assumed that stay-at-home restrictions would resume if the rate of new COVID-19 hospitalizations exceeded 2 per 100,000 residents per day. In consultation with NYC DOHMH, we developed the assumption that stay-at-home restrictions may be relaxed if COVID-19 hospitalizations dropped to the lowest levels observed prior to the initial relaxation on June 1, 2020: a rate of 0.8 per 100,000 residents per day. We assumed that stay-at-home restrictions and relaxations would continue to occur in cycles until May 31, 2021, if NYC meets the thresholds of ≥ 2 or ≤ 0.8 hospitalizations per 100,000 residents per day to relax or reinstate stay-at-home restrictions, respectively. We assumed phased relaxation over 4 weeks as done in Summer 2020, with a multiplicative effect on Re for each stage of relaxation, resulting in exponential growth in Re between the fully-restricted state and the fully-relaxed state.
Ethics approval
This study used publicly available data and was exempt from ethical review by the Institutional Review Boards of both New York University Grossman School of Medicine and NYC DOHMH.
Results
Model calibration to the growth in hospitalizations, ICU admissions, and deaths early in the NYC SARS-CoV-2 epidemic yielded an estimated R0 of 3.08 (IQR 2.97–3.42) at the beginning of the epidemic in NYC with an Re that declined to a minimum value of 0.50 (IQR 0.47–0.59) on April 10. Stay-at-home restrictions such as the closure of non-essential businesses and schools, large in-person gatherings, as well as individual adherence to social distancing and mask-wearing, succeeded in bringing the Re below one until summer 2020. The Re was estimated to rebound upon relaxation of stay-at-home restrictions depending on different adherence levels to social distancing and mask-wearing (Table 3).
Reinstatement of stay-at-home restrictions would immediately lower transmission (Fig. 1); however, due to the time lag from infections to hospitalizations, daily hospitalizations would continue to grow, peaking ~16 days after the reinstatement of stay-at-home restriction (Fig. 2). Similarly, deaths would continue to grow and peak 21 days after the resumption of stay-at-home restrictions (Fig. 3).
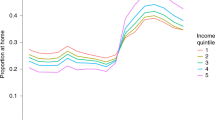
Estimated time spent under resumption and relaxation of restrictions between June 1, 2020 and May 31, 2021 by adherence to social distancing and mask-wearing. Yellow bars indicate the time spent under resumption of restrictions. Green and blue bars indicate the time up to 4 weeks (partial relaxation) and ≥ 4 weeks (full relaxation) after relaxation of restrictions, respectively. Adherence to mask-wearing is assumed as follows: 0% (Scenario 1 and 2), 50% (Scenario 3 and 4), 70% (Scenario 5 and 6), or 90% (Scenario 7 and 8). Adherence to social distancing is assumed to be 0% (Scenario 1, 3, 5, and 7) or 50% (Scenario 2, 4, 6, and 8).
Daily COVID-19 new infections under resumption and relaxation of restrictions between June 2020 and May 2021: (A) without adherence to social distancing and (B) with 50% adherence to social distancing. Each colored line indicates the level of mask adherence at 0% (red), 50% (orange), 70% (green) or 90% (blue).
Daily COVID-19 new hospitalizations under resumption and relaxation of restrictions between June 2020 and May 2021: (A) without adherence to social distancing and (B) with 50% adherence to social distancing. Each colored line indicates the level of mask adherence at 0% (red), 50% (orange), 70% (green) or 90% (blue).
Impact of adherence to social distancing and mask-wearing on epidemic growth upon reopening, and duration and frequency of reinstatement of stay-at-home restrictions
Under the most pessimistic assumptions of no mask-wearing and no social distancing (Scenario 1), NYC would have cycled between reinstatement and relaxation of stay-at-home restrictions four times by May 31, 2021. Only 26% of that time period would have been spent under full relaxation of stay-at-home restrictions (Fig. 1; Scenario 1, blue bars), with an additional 31% spent under partial relaxation (green bars) and 43% spent under stay-at-home restrictions (yellow bars). Under this assumption, the epidemic would have grown the fastest, reaching 9,300 daily new infections (Fig. 2A, red curve). A 54-day period of reinstated stay-at-home restrictions would have been necessary to bring new hospitalizations below the re-opening threshold of 0.8 per 100,000 residents (Fig. 3A, red curve). Phased reopening would have lasted 52 days before reaching the closure threshold, and the next closure would have lasted for 51 days before again reaching the re-opening threshold. More COVID-19 deaths (n = 18,690) would have occurred over the four cycles of re-opening than the cumulative COVID-19 deaths that had occurred (n = 17,716) prior to June 2020 (Fig. 4A, red curve).
Daily COVID-19-attributable deaths under resumption and relaxation of restrictions between June 2020 and May 2021: (A) without adherence to social distancing and (B) with 50% adherence to social distancing. Each colored line indicates the level of mask adherence at 0% (red), 50% (orange), 70% (green) or 90% (blue).
With the addition of either 50% adherence to social distancing (Scenario 2) or low adherence to mask-wearing (Scenario 3), the epidemic would have grown more slowly upon relaxation of stay-at-home restrictions and required reinstatements of restriction three times by May 31, 2021, increasing the portion of time spent under full relaxation of stay-at-home restrictions from 26 to 37%. Low adherence to mask-wearing with 50% adherence to social distancing (Scenario 4) or high adherence to mask-wearing without social distancing (Scenario 7) would have required one-time reinstatement of stay-at-home restrictions by May 31, 2021 (Fig. 1), further increasing the portion of time spent under full relaxation of stay-at-home restrictions to 76%. The combination of 50% adherence to social distancing and moderate to high adherence to mask-wearing would have enabled NYC to remain fully open without any reinstatement of stay-at-home restrictions (Scenarios 6 and 8). In threshold analyses (Fig. 5), avoiding reinstatement of stay-at-home restrictions required a minimum of 60% adherence to mask-wearing together with 50% adherence to social distancing.
Threshold analysis of adherence necessary to prevent any reinstatement of stay-at-home restrictions between June 2020 and May 2021 in NYC. Dark grey region corresponds to a range of adherence to social distancing and mask-wearing which necessitates the reinstatement of stay-at-home restrictions, while light grey region corresponds to a range avoiding any reinstatement of stay-at-home restrictions.
Discussion
NYC succeeded in reducing SARS-CoV-2 transmission through a stay-at-home order and restrictions on non-essential businesses, schools, and other in-person gatherings. As transmission decreased, phased reopening began in June 2020. However, there was a need to understand the potential impacts of reopening and identify opportunities to reduce harm. Our modeling results indicate that low adherence to mask-wearing and social distancing would have led to undesired consequences of repeated cycles of shutdown and reopening. On the other hand, our modeling results also highlight that high adherence to social distancing and mask-wearing could prevent any subsequent cycles of shutdown and reopening.
After the relaxation of stay-at-home restrictions, cities, states, and countries across the globe experienced resurgence42,43,44. Multiple states in the United States and countries across the globe paused reopening plans or reinstated restrictions. As cases rapidly surged, UK reinstated a national lockdown in early November 202045, and other countries including Greece and Germany subsequently reinstated and extended lockdown measures46,47. In contrast, countries including Hong Kong and Vietnam recorded fewer than 2,000 cases per million and 30 deaths per million by the end of 202142. These countries implemented highly restrictive mitigation measures and demonstrated high adherence to mask-wearing and social distancing, which likely contributed to their low COVID-19 burden and ability to resume many social, economic, educational, and religious activities48,49,50.
In NYC, adherence to mask-wearing was moderate, varying from 65% to 89% in the summer of 202038,39,40,41. At these levels of mask-wearing, our model projected that NYC would have exceeded the threshold to reinstate stay-at-home restrictions if people were not successfully able to maintain social distancing. Prior to citywide metrics exceeding thresholds, NYC and NYS deployed response programs in particular neighborhoods experiencing growing caseloads including targeted restrictions51. These targeted stay-at-home restrictions likely contributed to slowing down the epidemic growth in these selected neighborhoods52.
The availability and uptake of SARS-CoV-2 testing, the ability to conduct contact tracing services, and access to opportunities for safe isolation are key elements of epidemic control. We have previously shown12 that NYC’s testing and contact tracing capacities contributed to reducing transmission, but the magnitude of this effect would be insufficient to contain the epidemic if mask-wearing and social distancing were not also practiced.
Our study has several limitations. First, we represented a simplification of the impact of social distancing and mask wearing, and did not incorporate differences in these behaviors over or by neighborhood. Neighborhoods with more crowded living conditions and greater proportions of essential workers may experience differential impacts of masks and social distancing. Indeed, a study showed that higher levels of COVID-19 infections were observed in the neighborhoods where subway usage declined the least, in part due to the concentration of essential workers in these communities53. Second, the compartmental model used in this analysis did not capture social networks, geographic variation, or individual-level variation such as the propensity for superspreading. The model did represent household transmission during lockdown with a simple assumption that 25% of community cases would beget a household case after one generation time, but actual household transmission is more complex and heterogeneous. Third, we have not directly measured age-mixing patterns and did not attempt to predict possible shifts in the age-distribution of infections, which may have significant effects on disease burden54. Fourth, important aspects of the interaction between the impact of testing and contact tracing and the impact of social distancing and mask wearing remain unexplored. However, our previous work suggests that current levels of testing and contact tracing would be far from sufficient for avoiding epidemic resurgence12 unless paired with mask-wearing and social distancing, although innovations such as daily point-of-use testing55, automated digital contact tracing56,57,58, and targeted testing through sewage surveillance59,60 could amplify the impact of testing and tracing.
Our work was conducted prior to the availability of vaccines or other pharmaceutical interventions against COVID-19. On December 13th, 2020, a nurse in NYC became the first American to become vaccinated against COVID-19 outside of experimental trials. As vaccines became more broadly available, thresholds for imposing stay-at-home orders ceased to be followed. As of March 2022, 97% of NYC adults have received at least one vaccine dose27, and an adaptive reopening approach is unlikely, provided that vaccines maintain efficacy against SARS-CoV-2 variants. However, our analysis may have relevance in settings with limited vaccine availability, in the event of a future variant that escapes vaccine protection, or as a framework for planning public health responses to future pandemics.
Conclusions
Our modeling suggests that a combination of social distancing with moderate to high levels of mask-wearing could avoid the need for reinstatement of stay-at-home restrictions when vaccination and effective treatments for SARS CoV-2 are unavailable. Even low to moderate adherence may suffice to enable relaxation of stay-at-home restrictions for the majority of time. However, low adherence to mask-wearing and social distancing, even in the context of testing and contact tracing at feasible levels, would have led to multiple cycles of reinstated stay-at-home restrictions, with a minority of time spent fully reopened.
Data availability
Data on COVID-19 cases, hospitalizations, and deaths in NYC is publicly available at https://github.com/nychealth/coronavirus-data by the NYC DOHMH. Data on daily number of patients with COVID-19 in ICUs from the NYS Department of Health’s HERDS were used under the agreement for the current study. However, the data are available from the authors upon reasonable request and with permission of the NYS Department of Health’s HERDS.
References
New York State. ‘New York State on PAUSE’ Executive Order. https://coronavirus.health.ny.gov/new-york-state-pause (2020).
New York State. Governor Cuomo Issues Guidance on Essential Services Under The ‘New York State on PAUSE’ Executive Order (accessed 15 June 2021). https://www.governor.ny.gov/news/governor-cuomo-issues-guidance-essential-services-under-new-york-state-pause-executive-order (2020).
Amid Ongoing COVID-19 Pandemic, Governor Cuomo Issues Executive Order Requiring All People in New York to Wear Masks or Face Coverings in Public | Governor Andrew M. Cuomo (accessed 21 September 2020) https://www.governor.ny.gov/news/amid-ongoing-covid-19-pandemic-governor-cuomo-issues-executive-order-requiring-all-people-new
New York City Department of Health and Mental Hygiene. COVID-19: Guidance for Businesses and Schools (accessed 2 November 2020) https://www1.nyc.gov/site/doh/covid/covid-19-businesses-and-facilities.page (2020).
New York State. NY Forward: A guide to reopening new york & building back better (2020).
Centers for Disease Control and Prevention. CDC Activities and Initiatives Supporting the COVID-19 Response and the President’s Plan for Opening America Up Again (2020).
Liang, M. et al. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med. Infect. Dis. 36, 101751 (2020).
Chu, D. K. et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 395, 1973–1987 (2020).
Lyu, W. & Wehby, G. L. Community use of face masks and COVID-19: Evidence from a natural experiment of state mandates in the US. Health Aff. 39, 1419–1425 (2020).
Eikenberry, S. E. et al. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis. Model 5, 293–308 (2020).
Thakkar, N., Selvaraj, P., Famulare, M. & Klein, D. COVID in New York City: A Model-Based Perspective. https://covid.idmod.org/ (2020).
Kim, H.-Y., Mcgillen, J. B., Bershteyn, A. & Braithwaite, S. R. Requirements for testing, tracing, and quarantine to enable safe relaxation of COVID-19 stay-at-home policies in a US metropolitan area: A mathematical modelling analysis. In 23rd International AIDS Conference.
Bai, Y. et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 323, 1406–1407 (2020).
Linton, N. M. et al. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: A statistical analysis of publicly available case data. J. Clin. Med. 9, 538 (2020).
New York City Department of Health and Mental Hygiene. NYC Coronavirus Disease 2019 (COVID-19) Data (accessed 15 June 2021). https://github.com/nychealth/covid-vaccine-data
Otterman S. N.Y.C. Hired 3,000 Workers for Contact Tracing. It’s Off to a Slow Start. New York Times (accessed 23 February2021). https://www.nytimes.com/2020/06/21/nyregion/nyc-contact-tracing.html (2020).
NYC Health + Hospitals. NYC Test & Trace Corps (2020).
Rothwell, J. Americans’ Social Contacts During the COVID-19 Pandemic. Gallup (accessed 29 March 2022). https://news.gallup.com/opinion/gallup/308444/americans-social-contacts-during-covid-pandemic.aspx (2020).
Shah, K., Saxena, D. & Mavalankar, D. Secondary attack rate of COVID-19 in household contacts: A systematic review. QJM An. Int. J. Med. https://doi.org/10.1093/qjmed/hcaa232 (2020).
Daegu Disaster Management Headquater. COVID-19 daily briefing in Daegu metropolitan City (March 8th, 2020, 10:30am) (accessed 21 July 2021). https://blog.naver.com/daegu_news/221843112460 (2020).
Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia (2017).
Thorpe, L. E. et al. Rationale, design and respondent characteristics of the 2013–2014 New York City Health and Nutrition Examination Survey (NYC HANES 2013–2014). Prev. Med. Rep. 2, 580–585 (2015).
United States Census Bureau. 2013–2017 American Community Survey 5-Year Estimates (2018).
Lauer, S. A. et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann. Intern. Med. https://doi.org/10.7326/M20-0504 (2020).
Cummings, M. J. et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 395, 1763–1770 (2020).
Subramanian, R., He, Q. & Pascual, M. Quantifying asymptomatic infection and transmission of COVID-19 in New York City using observed cases, serology, and testing capacity. Proc. Natl. Acad. Sci. 118, e2019716118 (2021).
New York City Department of Health and Mental Hygiene. NYC Coronavirus Disease 2019 (COVID-19) Data (accessed 30 June 2020). https://github.com/nychealth/coronavirus-data (2020).
Stadlbauer, D. et al. Repeated cross-sectional sero-monitoring of SARS-CoV-2 in New York City. Nature 590, 146–150 (2021).
Richardson, S. et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized With COVID-19 in the New York City Area. JAMA 323, 2052–2059 (2020).
Goyal, P. et al. Clinical characteristics of covid-19 in New York City. N. Engl. J. Med. 382, 2372–2374 (2020).
Argenziano, M. G. et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: Retrospective case series. BMJ 369, m1996 (2020).
Mukherjee, V. et al. Clinical outcomes in critically ill coronavirus disease 2019 patients: A unique New York City public hospital experience. Crit. Care Explor. 2, e0188 (2020).
Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US | Cardiology | JAMA Internal Medicine | JAMA Network. 2022; published online March 29. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2768602
McAloon, C. et al. Incubation period of COVID-19: A rapid systematic review and meta-analysis of observational research. BMJ Open 10, e039652 (2020).
Thompson, C. N. COVID-19 outbreak: New York City, February 29–June 1, 2020. MMWR Morb. Mortal Wkly. Rep. https://doi.org/10.15585/mmwr.mm6946a2 (2020).
Rees, E. M. et al. COVID-19 length of hospital stay: A systematic review and data synthesis. BMC Med. 18, 270 (2020).
The City of New York. Test & Trace Corps (2020).
Nguyen, H. Nearly two in three Americans say wearing face masks in public should be mandatory. YouGov. published online June 26 (accessed 21 September 2020). https://today.yougov.com/topics/health/articles-reports/2020/06/26/americans-wearing-face-masks-should-be-mandatory (2020).
Igielnik, R. Most Americans say they regularly wore a mask in stores in past month | Pew Research Center. Pew Res. Cent. published online June 23 (accessed 21 September 2020). https://www.pewresearch.org/fact-tank/2020/06/23/most-americans-say-they-regularly-wore-a-mask-in-stores-in-the-past-month-fewer-see-others-doing-it/ (2020).
Greenberg, S. Siena College Poll. Siena Res. Inst. published online May 27 (accessed 21 September 2020). www.siena.edu/scri (2020).
Brown, E., Corona, J., Correal, A. & Mhute, W. Are New Yorkers Wearing Face Masks? Here’s What We Found in Each Borough (accessed 21 September 2020). https://www.nytimes.com/2020/08/20/nyregion/nyc-face-masks.html (2020).
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard (accessed 27 January 2020). https://covid19.who.int/ (2020).
Chadwick, L. Coronavirus: The 11 countries where WHO Europe says COVID-19 is on the rise | Euronews. Euronews (accessed 15 June 2021). https://www.euronews.com/2020/06/26/coronavirus-the-11-countries-where-who-europe-says-covid-19-is-on-the-rise (2020).
Associated Press. Coronavirus: India hits 2 million cases as health volunteers go on strike (accessed 15 June 2021). https://www.nbcnews.com/news/world/coronavirus-india-hits-2-million-cases-health-volunteers-go-strike-n1236116 (2020).
The United Kingdom Government Digital Service. Prime Minister announces new national restrictions. published online Oct 30 (accessed 8 February 2021). https://www.gov.uk/government/news/prime-minister-announces-new-national-restrictions (2020).
U.S. Embassy & Consulate in Greece. COVID-19 Information (accessed 8 February 2021). https://gr.usembassy.gov/covid-19-information/
Berry, A. German lockdown: Merkel announces tough new COVID curbs. Dtsch. Welle. 2020; published online Dec 13 (accessed 8 February 2021). https://p.dw.com/p/3mdqK
Ryu, S., Ali, S. T., Jang, C., Kim, B. & Cowling, B. J. Effect of nonpharmaceutical interventions on transmission of severe acute respiratory syndrome coronavirus 2, South Korea, 2020. Emerg. Infect Dis. 26, 2406–2410 (2020).
Ha, B. T. T. et al. Combating the COVID-19 epidemic: Experiences from Vietnam. Int. J. Environ. Res. Public Health 17, 3125 (2020).
Cowling, B. J. et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Heal. 5, e279–e288 (2020).
NYC Health & Hospitals. Mayor De Blasio Expands Hyper-Local Testing Response In Sunset Park (accessed 15 June 2021). https://www.nychealthandhospitals.org/pressrelease/mayor-de-blasio-expands-hyper-local-testing-response-in-sunset-park/ (2020).
New York State. Governor Cuomo Announces New Cluster Action Initiative (accessed 15 June 2021). https://www.governor.ny.gov/news/governor-cuomo-announces-new-cluster-action-initiative (2020).
Sy, K. T. L., Martinez, M. E., Rader, B. & White, L. F. Socioeconomic disparities in subway use and COVID-19 outcomes in New York City. Am. J. Epidemiol. 190, 1234–1242 (2021).
Zhang, J. et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 368, 1481–1486 (2020).
Subsoontorn, P., Lohitnavy, M. & Kongkaew, C. The diagnostic accuracy of isothermal nucleic acid point-of-care tests for human coronaviruses: A systematic review and meta-analysis. Sci. Rep. 10, 1–13 (2020).
Braithwaite, I., Callender, T., Bullock, M. & Aldridge, R. W. Automated and partly automated contact tracing: A systematic review to inform the control of COVID-19. Lancet Digit. Heal. 2, e607–e621 (2020).
Health, T. L. D. Contact tracing: Digital health on the frontline. Lancet Digit. Heal. 2, e561 (2020).
Ferretti, L. et al. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science 368, 1–13 (2020).
Daughton, C. G. Wastewater surveillance for population-wide Covid-19: The present and future. Sci. Total Environ. 736, 139631 (2020).
Medema, G., Heijnen, L., Elsinga, G., Italiaander, R. & Brouwer, A. Presence of SARS-Coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ. Sci. Technol. Lett. 7, 511–516 (2020).
Acknowledgements
We thank the New York City Department of Health and Mental Hygiene Bureau of Vital Statistics team and staff members and Incident Command System Surveillance and Epidemiology Section for data management.
Funding
This work was supported by the New York City Department of Health and Mental Hygiene.
Author information
Authors and Affiliations
Contributions
H.K., A.B., J.B., and R.S.B. designed the research; H.K. and J.B. performed the analysis; H.K. wrote the initial draft of the manuscript. J.S., J.S., C.K., R.W., and R.N. provided the COVID-19 epidemic data in N.Y.C. and helped to interpret the results. All authors contributed to revise the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, HY., Bershteyn, A., McGillen, J.B. et al. Social distancing and mask-wearing could avoid recurrent stay-at-home restrictions during COVID-19 respiratory pandemic in New York City. Sci Rep 12, 10312 (2022). https://doi.org/10.1038/s41598-022-13310-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13310-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.