Abstract
Inpatient populations are at increased risk of hyperglycemia due to factors such as medications, physical inactivity and underlying illness, which increases morbidity and mortality. Unfortunately, clinicians have limited tools available to prospectively identify those at greatest risk. We evaluated the ability of 10 common genetic variants associated with development of type 2 diabetes to predict impaired glucose metabolism. Our research model was a simulated inpatient hospital stay (7 day bed rest protocol, standardized diet, and physical inactivity) in a cohort of healthy older adults (n = 31, 65 ± 8 years) with baseline fasting blood glucose < 100 mg/dL. Participants completed a standard 75 g oral glucose tolerance test (OGTT) at baseline and post-bed rest. Bed rest increased 2-h OGTT blood glucose and insulin independent of genetic variant. In multiple regression modeling, the transcription factor 7-like 2 (TCF7L2) rs7903146 T allele predicted increases in 2-h OGTT blood glucose (p = 0.039). We showed that the TCF7L2 rs7903146 T allele confers risk for loss of glucose tolerance in nondiabetic older adults following 7 days of bed rest.
Similar content being viewed by others
Introduction
Nondiabetic patients who develop hyperglycemia during hospitalization have increased lengths of stay and mortality risk1,2,3,4,5,6,7. In critically ill patients, mortality increases incrementally with rising blood glucose, and patients reaching values above 300 mg/dL have high mortality rates independent of diabetes diagnosis3. Likewise, postoperative hyperglycemia increases the risk of post-operative infection by 30% with every 40-point increase from normoglycemia (< 100 mg/dl)7. Currently, clinicians are unable to identify nondiabetic inpatients at greater risk for developing hyperglycemia, limiting their ability to initiate preventive therapy.
Dozens of common genetic variants are associated with increased risk for type 2 diabetes. For example, the odds of developing type 2 diabetes is 1.5 when having the transcription factor 7-like 2 (TCF7L2) rs7903146 T allele (rs7903146T), which is established across many ethnic groups8,9. The TCF7L2 rs7903146T variant is also associated with impaired pancreatic function and elevated glycated hemoglobin in nondiabetic individuals10,11. Though some genetic variants, including TCF7L2 rs7903146T, are associated with elevated glycemic indicators in nondiabetic individuals, more evidence is needed to determine how genetic testing of these risk variants may support clinical decision making in the inpatient setting.
Inpatient hyperglycemia is multifactorial and mediated by factors like physical inactivity, medications, medical nutrition therapies, and underlying acute illnesses/chronic disease2,4,5,12. Inpatient bed rest in healthy research subjects models the physical inactivity aspect of a hospital stay while avoiding the confounding influence of variable nutrition therapies and disease-related comorbidities. Therefore, inpatient bed rest is a powerful tool to understand how the interaction of physical inactivity and genetic variation may contribute to a decline in insulin sensitivity and subsequent impaired glucose tolerance independent of the catabolic burden of the clinical milieu.
We sought to determine if genetic testing for ten common type 2 diabetes risk variants could predict changes in fasting blood glucose or glucose intolerance during an oral glucose tolerance test (OGTT) challenge in healthy older adults completing a 7 day inpatient bed rest protocol. We selected genetic variants based on their previously reported effect size, effect on beta cell function, or location of the single nucleotide polymorphism (SNP), with preference for those located in exons9,13,14. Here we report on the ability of MTNR1B (rs10830963), NOTCH2 (rs10923931), RASGRP1 (rs7403531), PROX1 (rs2075423), HHEX (rs1111875), IGF2BP2 (rs4402960), CDKAL1 (rs7754840), SLC30A8 (rs13266634), ZFAND6 (rs11634397), and TCF7L2 (rs7903146) to predict changes in fasting blood glucose, 2-h OGTT blood glucose, and Matsuda Insulin Sensitivity Index (Matsuda-ISI)15 in 31 healthy older adults following a 7 day bed rest protocol.
Results
Participants
Thirty-one generally healthy older adults provided blood for genotyping and completed the inpatient bedrest protocol. Participants’ baseline characteristics are reported in Table 1.
Overall effect of bed rest
Baseline and 2-h OGTT serum insulin and 2-h OGTT blood glucose were significantly increased in healthy older adults following seven days of bed rest contributing to significantly decreased insulin sensitivity and increased insulin resistance as indicated by Matsuda-ISI and Homeostatic Model for Insulin Resistance (HOMA-IR16), respectively (Fig. 1). Complete overall glucose and insulin responses to OGTT before and after bed rest are reported in Supplementary Table S1.
Overall glycemic responses to a 7-day inpatient bed rest protocol. (a) Fasting blood glucose before and after bed rest. (b) Fasting serum insulin before and after bed rest (c) 2 h post-OGTT blood glucose before and after bed rest (d) 2 h post-OGTT serum insulin before and after bed rest. (e) Matsuda Insulin Sensitivity Index (Mat-ISI) before and after bed rest. (f) Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) before and after bed rest. *p-value < 0.05; **p-value < 0.01; ***p-value < 0.001. P-values are the result of paired t-test showing mean and standard deviation for variables meeting the assumptions (fasting blood glucose, 2 h post-OGTT blood glucose, and Matsuda Insulin Sensitivity Index); results of Wilcoxon Signed-Rank Tests showing median and interquartile range are shown for variables violating one or more assumptions (fasting insulin, 2 h post-OGTT insulin, and HOMA-IR).
Models predicting increases in blood glucose
During model selection, the Feasible Solutions Algorithm17,18,19 identified the TCF7L2 rs7903146T allele and its statistical interaction effect with baseline 2-h OGTT blood glucose as a significant predictor of increased 2-h OGTT blood glucose following bed rest when including baseline 2-h OGTT blood glucose, age, and BMI as main effects in the model (p = 0.039). The baseline 2-h OGTT blood glucose and the TCF7L2 rs7903146T allele together explained 23.65% of the variability in post-bed rest 2-h OGTT blood glucose values, after controlling for age and BMI. (Figs. 2 and 3). There were no significant baseline differences in age, BMI, systolic blood pressure, diastolic blood pressure, fasting blood glucose or baseline 2-h OGTT blood glucose between TCF7L2 rs7903146 genotype groups at study baseline (Supplementary Table S2). No other genotype predicted glycemic outcomes or Matsuda-ISI following seven days of bed rest.
Spaghetti plot of blood glucose 2 h before (PreBR) and after (PostBR) a 7-day inpatient bed rest protocol by TCF7L2 rs7903146T genotype (a) Individual 2-h OGTT blood glucose changes in C/C genotype group; (b) Individual 2-h OGTT blood glucose changes in C/T genotype group (c) Individual 2-h OGTT blood glucose changes in T/T genotype group; the dotted line on (a–c) is 140 mg/dl, which is the cut point for a normal 2-h blood glucose value of an OGTT. (p = 0.039 for partial F-test of overall model TCF7L2 rs7903146T allele as a significant predictor of increased 2-h OGTT blood glucose following bed rest when including baseline 2-h OGTT blood glucose, age, and BMI as main effects in the model).
Association of PreBR 2-h OGTT blood glucose with PostBR 2-h OGTT blood glucose. The black line represents no change in 2-h OGTT glucose following 7 days of bed rest. The green line represents a 30 mg/dL increase in blood glucose after the 7 day bed rest protocol. Individuals with the C/C risk genotype are shown as black circles, C/T risk variants are red circles and T/T risk variants are blue circles. (p = 0.039 for partial F-test of overall model TCF7L2 rs7903146T allele as a significant predictor of increased 2-h OGTT blood glucose following bed rest when including baseline 2-h OGTT blood glucose, age, and BMI as main effects in the model).
Discussion
Older adults with TCF7L2 rs7903146T risk variants are more likely to have increased 2-h OGTT blood glucose following seven days of bed rest. No significant relationships where found for the 9 other variants, but OGTT data for all SNPs assessed is presented in Supplementary Tables S3 and S4.
TCF7L2 is a transcription factor belonging to the Wnt signaling pathway present in pancreas, liver, and other tissues20,21. Whole-genome chromatinimmunoprecipitation (ChIP) combined with massively parallel DNA sequencing (ChIP-Seq) analyses show that TCF7L2 binds directly to several genes involved in glucose metabolism, including PCK1, FBP1, IRS1, IRS2, AKT2, ADIPOR1, PDK4 AND CPT1A22. Carriers of the rs7903146T allele exhibit impaired proinsulin conversion, higher proinsulin:insulin ratios, and greater likelihood of developing insulin-dependent type 2 diabetes23,24,25,26, but not hepatic or extrahepatic insulin resistance27,28. Paradoxically, some evidence indicates that liver and other tissues appear to be involved in TCF7L2 rs7903146T-associated glucose intolerance and insulin secretion29.
TCF7L2 risk alleles are associated with elevated post-OGTT and nocturnal blood glucose in nondiabetic adults25,26,30,31. The rs7903146T allele also associates with impaired glucose tolerance in adults with metabolic syndrome30 and obese adolescents25. Healthy, middle-aged and older nondiabetic participants with rs7903146T also exhibit higher nocturnal glucose31. However, similar to our findings, prior studies indicate that rs7903146T does not affect fasting blood glucose in healthy middle-aged adults32. This suggests that fasting blood glucose may not be an optimal biomarker to screen individuals with rs7903146T for risk of developing prediabetes and type 2 diabetes.
Thirty-eight young, healthy Caucasian men with TCF7L2 rs7903146T risk alleles exhibit a lower first-phase insulin response (FPIR) to an intravenous glucose tolerance test (IGTT) compared with those with the homozygous C genotype both before and after 9 days of bed rest (p = 0.01 and p = 0.0001, respectively)33. Following bed rest, the participants with the TCF7L2 rs7903146 risk variants also fail to show an incremental rise of FPIR in response to insulin resistance. Though FPIR is not a concept that is directly translatable outside of the context of an IGTT, the ability to rapidly secrete insulin in response to an OGTT in the early phase (up to 30 min after consumption of glucose) is a similar concept34. The liver responds to a robust early phase insulin response by reducing release of glucose, thereby limiting the overall blood glucose response to an OGTT or a meal, and this physiological trait that is lost in the development of type 2 diabetes35. Here we did not observe any relationship between rs7903146T risk alleles and insulin measures or calculated insulin sensitivity at any point after a 75 g glucose load, but we completed 2-h OGTT, which are not directly comparable to the IGTT or the FPIR.
Periods of physical inactivity promote insulin resistance in healthy adults36,37. If the reduced glucose tolerance we observed following a 7 day period of inactivity in healthy, nondiabetic adults persists, patients having rs7903146T variants could be especially susceptible to long-term impairments in glucose metabolism following inpatient stays. Future research should evaluate how rs7903146T affects blood glucose throughout hospital stay in both critically ill and non-critically ill hospital patients. Moreover, follow up studies should evaluate if rs7903146T predicts long-term glucose intolerance following an extended period of disuse in clinical populations in patients after discharge. Finally, utilizing OGTT, rather than fasting blood glucose, may be more appropriate for patients carrying the rs7903146T allele.
Our analysis showed an intriguing association between the TCF7L2 rs7903146T allele and loss of glucose tolerance after physical disuse; however, there were limitations. This study was not initially designed to test genotype–phenotype relationships. We recruited volunteers to test the effect of nutrition and physical activity on a broad range of outcomes following bed rest. Since parent study intervention groups did not associates with any glycemic outcome, and multivariate modeling did not identify parent study group assignment as a significant factor in the model, we feel confident that the genotype–phenotype relationship between TCF7L2 rs7903146T and 2-h OGTT blood glucose described here was not affected by parent study group assignment. Since we only genotyped 10 variants, we could not consider any possible contribution of genetic background to the outcomes. Finally, this small study was conducted in generally healthy older adults and would not be generalizable to other aged groups or those with acute or chronic illness.
The TCF7L2 rs7903146T genotype did not predict development of clinically diagnosable hyperglycemia (fasting blood glucose ≥ 126 mg/dl) or impaired glucose tolerance (2-h OGTT blood glucose ≥ 140 mg/dl) following bed rest. However, the findings from this study indicate that patients with the TCF7L2 rs7903146T allele may be at risk for accelerated decline in glucose tolerance with bed rest and may benefit from closer glucose monitoring during hospitalization.
Conclusion
We show for the first time that the TCF7L2 rs7903146 T allele associates with increased 2-h OGTT blood glucose in nondiabetic, older adults following seven days of bed rest and physical disuse. If these findings can be replicated in a clinical setting, the TCF7L2 rs7903146T allele may help clinicians identify nondiabetic inpatients at greater risk for accelerated glucose intolerance and hyperglycemia in an inpatient setting.
Methods
Participants
Thirty-one healthy older adults were recruited (65 ± 8 years), provided written informed consent, medically screened, and compensated for their time as part of a larger randomized-controlled trial. A fasting glucose ≥ 100 mg/dl, recent corticosteroid use, or evidence of chronic disease (vascular disease, unmanaged elevated blood pressure, and kidney disease) were considered exclusionary criteria for the study. All enrolled participants were community-dwelling, able to complete activities of daily living, and considered to be generally healthy. The study protocol was conducted within the inpatient unit of the Clinical and Translational Research Center at the University of Texas Medical Branch (UTMB) and in accordance with the Declaration of Helsinki and approved by the UTMB Institutional Review Board. All participants provided informed consent including consent for genetic analyses. Sample size was determined by subject enrollment in the parent study and available blood samples for genetic analyses. Recruitment and collection of blood for this secondary analysis began after the initial enrollment period for the parent clinical trial. Participants included in the present analysis were enrolled between 03/26/2014 and 10/10/2017, the latter of which was the last enrollment for the parent grant. This study was registered though clinicaltrials.gov on 03/05/2013 (NCT01846130).
Participants were assigned to one of five experimental conditions (protein consumption patterns, small bout of walking, or amino acid supplementation)38,39,40 that were outside of the scope of this study. Collection and storage of blood for genotyping was initiated in the middle of the parent grant, so not all study participants could be included in the analysis. The study statistician confirmed that there were no significant relationships between the study interventions and primary study outcomes (2-h OGTT glucose and Matsuda-ISI) presented here (p > 0.05). A brief description of each study intervention is available in Supplementary Table S5.
Bed rest
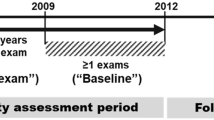
As previously reported38,39,40 participants completed 3 days of diet-stabilization/testing followed by seven days of horizontal bed rest in the UTMB Institute for Translational Sciences–Clinical Research Center (ITS-CRC). Consistent with our previous horizontal bed rest studies, subjects were continuously monitored for safety41. All bathing and toiletry activities were performed without bearing weight. The general experimental design is depicted in Fig. 4.
Diet
Participants were provided isoenergetic diets (55% carbohydrate, 29% fat, and 16% protein). Individualized daily energy requirements were estimated using the Harris–Benedict equation with activity factors of 1.6 and 1.3 used for the ambulatory and bed rest period, respectively38,39,41. Water was provided ad libitum. The breakfast meal presented after each OGTT was adjusted to compensate for the 75 g glucose load. Energy and macronutrient intake, taking plate waste into account, were analyzed by using Nutrition Data System for Research software (version 2011, Nutrition Coordinating Center, Minneapolis, MN).
Oral glucose tolerance test and serum insulin
Standard 75 g glucose load (Glucola, Azer Scientific, Morgantown, PA) oral glucose tolerance tests were administered before and after the 7-day bed rest protocol. Whole-blood samples (0, 30, 60, 90, and 120 min) were analyzed on an YSI Bioanalyzer (YSI, Yellow Springs, OH). Serum insulin was measured using a commercially available enzyme-linked immunosorbent assay (MilliporeSigma, Burlington, MA). Matsuda Insulin Sensitivity Index (Matsuda-ISI) was determined using the Matsuda formulas15.
SNP selection and genotyping
Though dozens of genetic variants have been reported to associate with diabetes and other metabolic conditions, we chose an initial subset of SNPs showing a relatively large effect size, a demonstrated impact on beta cell function, and/or evidence of translated protein products in older adults9,13,14.
Genomic DNA was extracted from whole blood samples using the DNeasy Blood Kit (QIAGEN, Germantown, MD) according to the manufacturer's instructions. TaqMan® Genotyping Assays (Thermo Fisher/Applied Biosystems, Foster City, CA) were used to genotype for MTNR1B (rs10830963), NOTCH2 (rs10923931), RASGRP1 (rs7403531), PROX1 (rs2075423), HHEX (rs1111875), IGF2BP2 (rs4402960), CDKAL1 (rs7754840), SLC30A8 (rs13266634), ZFAND6 (rs11634397), and TCF7L2 (rs7903146) (Supplementary Tables S6 and S7). The work was performed by the Genomics Core at the University of Texas Medical Branch according to the manufacturer’s instructions. Briefly, 5 ng of purified DNA was added to each well and dried down. Primers and all reagents were combined, and PCR was completed using an Applied Biosystems 7500 Fast Real-Time PCR System (Thermo Fisher/Applied Biosystems, Foster City, CA). Thereafter, Sequence Detection System (SDS) Software was used to perform a post-PCR plate read and analysis to call genotypes. Samples were run in triplicate and the core was able to make genotype calls for all participants and single nucleotide polymorphisms (SNP). Genotyping assays were completed at the same time using reagents from the same lot and were carried out by the same technician. To confirm accurate genotype calls, the genomics core demonstrated concordance with the known genotypes for Hela, HEK, HEMS and two other known reference samples. After statistical analyses revealed significant associations between the associations between the TCF7L2 rs7903146 genotype and change in glucose tolerance with best rest, we confirmed the genotyping results by genotyping for TCF7L2 rs4506565 which is in linkage disequilibrium with rs790314642,43.A TaqMan® Genotyping Assay was completed using the methods described above on a QuantStudio™ Fast Real-Time PCR System (Thermo Fisher/Applied Biosystems, Foster City, CA) in the Center for Muscle Biology at the University of Kentucky. Allele frequencies for TCF7L2 (rs7903146) and TCF7L2 rs4506565 from this study and other US groups are included in Supplementary Table S844. All genotyping results can be viewed in Supplementary Data File 1. The allelic discrimination plot for TCF7L2 rs7903146 provided by the UTMB Genomics Core is included in Supplementary Data File 2.
Statistical analyses
First, summary statistics were calculated for demographic and baseline characteristics. In particular, means and standard deviations were calculated for quantitative variables, while percentages were calculated for categorical variables. Genotype frequencies were calculated for each SNP, and Hardy Weinberg Equilibrium exact tests were also performed using the R package, HardyWeinberg45.
Prior to analysis of the primary outcome (fasting glucose, 2-h OGTT glucose) and the secondary outcome (Matsuda-ISI), a one-way ANOVA was run to screen for any significant baseline differences with each parent study intervention and genotype groups. Overall pre-post bed rest comparisons of quantitative variables were made using paired t-tests or Wilcoxon Signed-Rank tests depending on the result of a Shapiro-Wilks test on the pre-post differences in quantitative variables.
Statistical model selection46 was performed to identify multiple linear regression models that are able to predcit blood glucose and Matsuda score32. In particular, we were interested in identifying explanatory variables that improved predictions of each outcome after accounting for age, BMI, and baseline value of the outcome (if the baseline value was collected). Since adjustments were required, we used the Feasible Solutions Algorithm17,19 to generate candidate multivariate regression models for each outcome, using R2 as the statistical criterion for selection. Potential explanatory variables included all combinations of two of the 10 candidate SNPs, age, BMI, and/or parent study intervention.
The Feasible Solutions Algorithm identified candidate multiple linear regression models, from which a model was selected for each outcome variable. For the final multiple linear regression model selected, a partial F-test was performed to look for evidence that the identified SNP was helpful in predicting the post-time point primary outcome, after accounting for age, BMI, and baseline outcome value (as appropriate). For OGTT, a scatterplot was created to show the relationship between pre-BR OGTT and post-OGTT values observed in the data. Color of observed data point is used to distinguish TCF7L2 rs7903146 variants (Fig. 3). All analyses were performed in R version 3.6.1.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ahmann, A. Reduction of hospital costs and length of stay by good control of blood glucose levels. Endocr. Pract. 10(Suppl 2), 53–56 (2004).
Baker, E. H. et al. Hyperglycaemia is associated with poor outcomes in patients admitted to hospital with acute exacerbations of chronic obstructive pulmonary disease. Thorax 61(4), 284–289 (2006).
Krinsley, J. S. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin. Proc. 78(12), 1471–1478 (2003).
Olveira, G. et al. Parenteral nutrition-associated hyperglycemia in non-critically ill inpatients increases the risk of in-hospital mortality (multicenter study). Diabetes Care 36(5), 1061–1066 (2013).
Sarkisian, S. et al. Parenteral nutrition-associated hyperglycemia in noncritically ill inpatients is associated with higher mortality. Can. J. Gastroenterol. 24(7), 453–457 (2010).
Stead, L. G. et al. Hyperglycemia as an independent predictor of worse outcome in non-diabetic patients presenting with acute ischemic stroke. Neurocrit. Care 10(2), 181–186 (2009).
Ramos, M. et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann. Surg. 248(4), 585–591 (2008).
Cauchi, S. et al. TCF7L2 is reproducibly associated with type 2 diabetes in various ethnic groups: A global meta-analysis. J. Mol. Med. (Berl) 85(7), 777–782 (2007).
Andersson, E. A. et al. Genetic risk score of 46 type 2 diabetes risk variants associates with changes in plasma glucose and estimates of pancreatic β-cell function over 5 years of follow-up. Diabetes 62(10), 3610–3617 (2013).
Shah, M. et al. TCF7L2 genotype and alpha-cell function in humans without diabetes. Diabetes 65(2), 371–380 (2016).
Færch, K. et al. Incretin and pancreatic hormone secretion in Caucasian non-diabetic carriers of the TCF7L2 rs7903146 risk T allele. Diabetes Obes. Metab. 15(1), 91–95 (2013).
Mahmassani, Z. S. et al. Disuse-induced insulin resistance susceptibility coincides with a dysregulated skeletal muscle metabolic transcriptome. J. Appl. Physiol. 126(5), 1419–1429 (2019).
Cornelis, M. C. et al. Joint effects of common genetic variants on the risk for type 2 diabetes in US men and women of European ancestry. Ann. Intern. Med. 150(8), 541–550 (2009).
de Miguel-Yanes, J. M. et al. Genetic risk reclassification for type 2 diabetes by age below or above 50 years using 40 type 2 diabetes risk single nucleotide polymorphisms. Diabetes Care 34(1), 121–125 (2011).
Matsuda, M. & DeFronzo, R. A. Insulin sensitivity indices obtained from oral glucose tolerance testing: Comparison with the euglycemic insulin clamp. Diabetes Care 22(9), 1462–1470 (1999).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7), 412–419 (1985).
Miller, A. J. Selection of subsets of regression variables. J. R. Stat. Soc. Ser. A 147(3), 389–425 (1984).
Corrine, F. et al. Thompson Feasibility as a mechanism for model identification and validation. J. Appl. Stat. 48(11), 2022–2041 (2020).
Lambert J, G.L., Elliott C F, Thompson K, Stromberg A., rFSA: An R Package for Finding Best Subsets and Interactions. R J., 2019. 10(2).
Shu, L. et al. Transcription factor 7-like 2 regulates beta-cell survival and function in human pancreatic islets. Diabetes 57(3), 645–653 (2008).
Bailey, C. H. Improved meta-analytic methods show no effect of chromium supplements on fasting glucose. Biol. Trace Elem. Res. 157(1), 1–8 (2014).
Norton, L. et al. Chromatin occupancy of transcription factor 7-like 2 (TCF7L2) and its role in hepatic glucose metabolism. Diabetologia 54(12), 3132–3142 (2011).
Zhou, Y. et al. Survival of pancreatic beta cells is partly controlled by a TCF7L2-p53-p53INP1-dependent pathway. Hum. Mol. Genet. 21(1), 196–207 (2012).
Shen, J., Fang, Y. & Ge, W. Polymorphism in the transcription factor 7-like 2 (TCF7L2) gene is associated with impaired proinsulin conversion–A meta-analysis. Diabetes Res. Clin. Pract. 109(1), 117–123 (2015).
Cropano, C. et al. The rs7903146 variant in the TCF7L2 gene increases the risk of prediabetes/type 2 diabetes in obese adolescents by impairing beta-cell function and hepatic insulin sensitivity. Diabetes Care 40(8), 1082–1089 (2017).
Noordam, R. et al. Interrelationship of the rs7903146 TCF7L2 gene variant with measures of glucose metabolism and adiposity: The NEO study. Nutr. Metab. Cardiovasc. Dis. 28(2), 150–157 (2018).
Varghese, R. T. et al. Diabetes-associated variation in TCF7L2 is not associated with hepatic or extrahepatic insulin resistance. Diabetes 65(4), 887–892 (2016).
Ferreira, M. C. et al. TCF7L2 correlation in both insulin secretion and postprandial insulin sensitivity. Diabetol Metab. Syndr. 10, 37 (2018).
Bailey, K. A. et al. Evidence of non-pancreatic beta cell-dependent roles of Tcf7l2 in the regulation of glucose metabolism in mice. Hum. Mol. Genet. 24(6), 1646–1654 (2015).
Katsoulis, K. et al. TCF7L2 gene variants predispose to the development of type 2 diabetes mellitus among individuals with metabolic syndrome. Hormones (Athens) 17(3), 359–365 (2018).
van der Kroef, S. et al. Association between the rs7903146 polymorphism in the TCF7L2 gene and parameters derived with continuous glucose monitoring in individuals without diabetes. PLoS ONE 11(2), e0149992 (2016).
Faerch, K. et al. Incretin and pancreatic hormone secretion in Caucasian non-diabetic carriers of the TCF7L2 rs7903146 risk T allele. Diabetes Obes. Metab. 15(1), 91–95 (2013).
Alibegovic, A. C. et al. The T-allele of TCF7L2 rs7903146 associates with a reduced compensation of insulin secretion for insulin resistance induced by 9 days of bed rest. Diabetes 59(4), 836–843 (2010).
Del Prato, S. & Tiengo, A. The importance of first-phase insulin secretion: Implications for the therapy of type 2 diabetes mellitus. Diabetes Metab. Res. Rev. 17(3), 164–174 (2001).
Caumo, A. & Luzi, L. First-phase insulin secretion: Does it exist in real life? Considerations on shape and function. Am. J. Physiol. Endocrinol. Metab. 287(3), E371–E385 (2004).
Hamburg, N. M. et al. Physical inactivity rapidly induces insulin resistance and microvascular dysfunction in healthy volunteers. Arterioscler. Thromb. Vasc. Biol. 27(12), 2650–2656 (2007).
Dirks, M. L. et al. One week of bed rest leads to substantial muscle atrophy and induces whole-body insulin resistance in the absence of skeletal muscle lipid accumulation. Diabetes 65(10), 2862–2875 (2016).
Arentson-Lantz, E. J. et al. Countering disuse atrophy in older adults with low volume leucine supplementation. J. Appl. Physiol. 2, 2 (2020).
Arentson-Lantz, E. J. et al. Improving dietary protein quality reduces the negative effects of physical inactivity on body composition and muscle function. J. Gerontol. A Biol. Sci. Med. Sci. 2, 2 (2019).
Arentson-Lantz, E. et al. 2,000 steps/day does not fully protect skeletal muscle health in older adults during bed rest. J. Aging Phys. Act. 27(2), 191–197 (2019).
English, K. L. et al. Leucine partially protects muscle mass and function during bed rest in middle-aged adults. Am. J. Clin. Nutr. 103(2), 465–473 (2016).
Delgado-Lista, J. et al. Pleiotropic effects of TCF7L2 gene variants and its modulation in the metabolic syndrome: From the LIPGENE study. Atherosclerosis 214(1), 110–116 (2011).
Chandak, G. R. et al. Common variants in the TCF7L2 gene are strongly associated with type 2 diabetes mellitus in the Indian population. Diabetologia 50(1), 63–67 (2007).
Alexander, T. A. & Machiela, M. J. LDpop: An interactive online tool to calculate and visualize geographic LD patterns. BMC Bioinform. 21(1), 14 (2020).
Graffelman, J. Exploring diallelic genetic markers: The hardyweinberg package. J. Stat. Softw. 64(3), 23 (2015).
Kutner, M.H., Applied linear statistical models. 5th ed. The McGraw-Hill/Irwin series operations and decision sciences. 2005, Boston: McGraw-Hill Irwin. xxviii, 1396 p.
Acknowledgements
We sincerely thank Deborah Prusak and staff of the UTMB ITS-CRC and genomics core for their assistance.
Funding
Claude D. Pepper Older Americans Independence Center, University of Texas Medical Branch Grant number P30 AG024832. National Institute of Arthritis and Musculoskeletal and Skin Diseases Grant number R01 AR071398-04S1.Nursing Research at the National Institutes of Health Grant number R01 NR012973. National Center for Research Resources Grant number 1UL1RR029876. National Center for Advancing Translational Sciences UL1TR000071.
Author information
Authors and Affiliations
Contributions
D.P.J. and E.A.L. designed and executed the parent study. D.P.J., E.A.L., B.D.M., J.L.F., and C.S.F. participated in data collection and sample analysis. K.L.T. and J.L.F. performed data analysis. J.L.F., B.D.M. and E.A.L. prepared the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
DPJ has participated on scientific advisory panels, provided educational seminars, and received travel reimbursements and honoraria from the American Egg Board, Leprino Foods, National Cattlemen’s Beef Association, National Dairy Council, Nestle Nutrition, Sabra Wellness and Nutrition, and the U.S. Dairy Export Council. JLF, EAL, CSF, and KT report no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fry, J.L., Munson, B.D., Thompson, K.L. et al. The T allele of TCF7L2 rs7903146 is associated with decreased glucose tolerance after bed rest in healthy older adults. Sci Rep 12, 6897 (2022). https://doi.org/10.1038/s41598-022-10683-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10683-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.