Abstract
The aim of this study is to assess factors that influence the uptake of short-term contraceptives among married women aged between 15 and 49 years in Afghanistan. The cross-sectional Afghanistan 2015 Demographic and Health Survey provided the dataset for this analysis. We included 22,974 women and applied multivariable logistic regression to investigate the influencing factors for the uptake of short-term contraceptives. 92% of Afghan women knew at least one type of short-term contraception but only 17% were using short term contraceptives. Short term contraceptive use was most prevalent among women in the age group between 30 and 40 who were educated, employed, and rich. Most of the users were living in the western parts of Afghanistan and women from the Balooch and Pashtun ethnic groups were most likely to use short-term contraceptives. Media exposure and women empowerment were also positively associated with the use of short-term contraceptives. We did not find an association with living in urban or rural settings. Contraception promotion in Afghanistan requires multisectoral efforts, tailored to the needs of women from low and middle socioeconomic strata. Health promotion activities, empowering women, strengthening education, and training of service providers on effective counseling are options that should be considered to improve the current situation.
Similar content being viewed by others
Introduction
According to the World Health Organization, ‘Family Planning (FP) allows people to attain their desired number of children and determine the spacing of pregnancies. It is achieved through the use of contraceptive methods and the treatment of involuntary infertility’. FP is an effective approach to reduce maternal and child mortality1,2. Studies have shown that the use of contraceptives has prevented approximately 272,000 maternal deaths worldwide, which is equivalent to a 44% reduction in maternal mortality. Other studies have revealed that contraception use is strongly associated with a reduction in neonatal deaths2,3,4,5.
Globally, about 12% of married women have an unmet need for contraception with the majority of them living in low and middle income countries6. Recent data showed that in 2017 out of 206 million pregnancies in developing countries, around 43% were unintended. According to WHO, about 214 million women of reproductive age who want to avoid pregnancy are not using any method of contraception7. This unmet need for contraception results in millions of unwanted pregnancies7. A study showed that promotion of contraceptives in developing countries over the past 2 decades has avoided up to 40% of maternal deaths simply by reducing the number of unwanted pregnancies8.
Depending on the source of literature, the maternal mortality ratio in Afghanistan lies between 12919 and 63810 in year 2017, making them rank among the highest worldwide. Traditionally, Afghans tend to have large families, and even though the fertility rate has declined in recent years from 7.4 in 2000, to 5.1 in 201811, the total fertility rate is still considered high compared to its South Asian neighbors12.
Over the past decade, there was an increase in the prevalence of contraceptive use from 7% in 2003 over 11% in 2012 to a still low 23% in 201513. The report of the Afghanistan Demographic and Health Survey (AfDHS) revealed that around 53% of women were not in need of contraception and around 24% had an unmet need for contraception which is considered very high9. Given Afghanistan’s high fertility rate and relatively high prevalence of unmet need for contraception, the prevalence of contraception is considered low compared to other countries in the region and all over the world14.
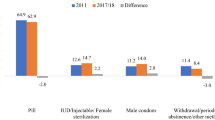
Contraceptives may either be classified into modern and traditional methods, or according to the duration of their effectiveness into long term, short term, and permanent contraceptives. According toAfDHS, in 2015, in Afghanistan 95% of married women and 92% of married men know at least one method of FP9. Despite this high level of awareness, the prevalence of contraception utilization remained low at 23%, with 16% being short-term contraceptives, 3% being traditional methods, and less than4% being intrauterine devices, sterilization and implants9. The report also showed that the met need for contraception was equally distributed for spacing and limiting, each responsible for 11%. However from 24% unmet need, 18% was for spacing and 7% for limiting, which adds more importance to short-term methods in the country.
In Afghanistan, very few studies15,16,17 assessed the predictors of family planning modern methods, but neither particularly explored the determinants of short-term methods, amidst their utmost importance.
In this study we hypothesize that the use of short-term contraceptive methods in Afghanistan is influenced by women’s sociodemographic characteristics, exposure to FP Information, and women’s empowerment. Therefore, we aimed to assess the factors that influences the uptake of short-term contraceptives among married women aged between 15 and 49 years in Afghanistan.
Methodology
Pills, injectables, and male condoms, which are classified as short-term methods18, were by far the most widely known and practiced methods among both women and men, and we therefore focused our analysis only on these short-term methods. To gain a better understanding of the context, our analysis explicitly focuses on predictors of and barriers to the use of short-term contraceptives. We used the nationally representative (except for Baghlan Province) AfDHS dataset. Data collection was carried out between July 15, 2015, and February 23, 2016. The AfDHS 2015 used an updated version of the Household Listing Frame as sampling frame19, which included information from 25,974 enumeration areas (EAs). The required number of households was estimated for each EA using location (province, and district) and type of residence (urban or rural)9.
The stratified two stage random sample design resulted in representative estimates of demographic and health indicators. Details on the data collection process can be found elsewhere9. All ever married women between the age of 15–49 years who were permanent residents of the selected households or visitors who stayed in the households the night before the survey were eligible for the survey. All participants have agreed to take part in the survey and signed the informed consent forms (For minor participants informed consent has been obtained from their legal guardians). Women who were pregnant at the time of survey were excluded for this analysis, because they will not utilize contraception. The data from this survey are openly available under https://dhsprogram.com/data/availabledatasets.cfm.
A total of 29,461 out of 30,434 eligible women (response rate 96.8%) were interviewed in the survey. Out of these, we excluded 6514 women (22.1%) who were pregnant at the time of data collection, hence, remained with a total of 22,947 women (Fig. 1).
The survey protocol was approved by the Inner-City Fund (ICF) Institutional Review Board and the Ministry of Public Health of Afghanistan, and the survey methods were performed in-line with the relevant guidelines and regulations9.
The outcome variable for this analysis was the current use of short-term contraceptives as binary indicator. As potential explanatory variables we considered: age, education, wealth index, occupation, place of residence, ethnicity, region, media exposure, and women empowerment. Media exposure was created from the questions that asked the women if they had heard of FP messages from TV, radio, or magazines. Based on this, the participants were categorized as ‘exposed to FP information’ if they affirmed to at least one of these questions. The women empowerment variable was created based on questions about women’s involvement in household decisions regarding income, purchases, family visits, and their health. Women were categorized as ‘partially empowered’ if they were involved in 1 or 2 of the decisions, and ‘fully empowered’ if they were involved in 3 or 4 of the decisions.
For the descriptive analysis we used the Pearson’s Chi square test to assess the existence of an association between the use of short-term contraceptives and the explanatory variables. Then we used logistic regression to estimate odds ratios for the independent variables.
Since the dataset was large, and all the variables were found to be significant at level of 95% confidence interval, we decided for more strict criteria to minimize the risk of chance and set the statistical significance to α = 0.01 and calculated 99% of confidence intervals with robust standard errors. Moreover, all the predictors were significant in the univariate model except place of residence, therefore we performed the full model analysis. We first decided to establish the final model through the backward elimination method, but since the data was hardly changing with that, we included all the variables in the final adjusted model. Stata version 12 IC was used for analyses.
Ethical approval
Since we used the secondary data from DHS, we did not need ethical clearance for this analysis as this survey was already approved by the IRB of Afghan Ministry of Public Health. Participant have agreed to take part in the survey and signed the consent form.
Results
Sociodemographic distribution and use of short-term contraceptives
Table 1 shows that 20.3% (4656 women) of the participants (non-pregnant women) in this survey were between 25 and 29 years old, followed by the age group of 20–24 (18% equal to 4270 women). Over 85% (19,690) of women were illiterate, and around 87% (20,070) of the participants were unemployed. Almost three quarters of the participants belonged to Pashtun and Tajik ethnic groups. Three quarter (74.4% equal to 17,073) of the women were living in rural areas. The number of women who did not have access to FP information was almost twice as high as of those who had access. Moreover, around one third (8023) of the participants were classified as unempowered, 23.5% (5396) as partially empowered, and 37.7% (8,662) as fully empowered.
Overall use of short-term contraceptives was quite low: among the total of 22,947 participants, 17% used short term contraceptives and 6% employed long-acting methods and traditional methods.
Table 1 shows that the proportion of unmet need for spacing is higher than for limiting in all categories. Considering the age groups, the unmet need for spacing was highest (33.71% equal to 1413 women) in the age group of 20–24, and lowest (2.95% equal to 86 women) in the 45–49 age group, while for limiting this trend showed different pattern with the lowest (1.30% equal to 15 women) in the 15–19 age group and highest (13.95% equal to 476 women) in the age group of 35–39.
Distribution of unmet need by ethnicity and regions was also heterogeneous. Turkmen women had the highest (32.83%, or 153 women) unmet need for spacing while Balooch women had the lowest (14.03%, or 39 women). Similarly the unmet need for limiting varied from 9.15% (143 person) among Uzbek women to 0.8% (7 person) in Nooristani women.
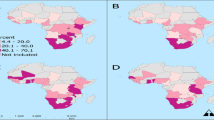
Women living in the northeastern region had the highest (26.62%, or 660 women) unmet need for spacing, while those in the western region had the lowest (15.16% equal to 510 women).
Women empowerment showed remarkably different prevalences of unmet need. Unempowered women had the highest (71.16% equal to 6213 women) unmet need for spacing, while partially and fully empowered women had 19.68% (1039 women) and 21.82% (1842 women) respectively.
The unmet need was almost equally distributed among women with varying levels of education, employment status, wealth status, living settings, and access to FP information.
Multivariable logistic regression analysis
The result from the multiple logistic regression revealed an association between all the predicting factors and use of short-term contraception. The only factor which was not significantly (p value = 0.45) associated was the place of residence and we did not find any significant difference in the use of short-term contraception among women living in urban and rural settings (Table 2).
As shown in Table 2, the likelihood of using contraceptives was lowest in the youngest age group, compared to the oldest, and increased with age up to 30–39 years, while it decreased again afterwards. Interestingly women in the age group of 30–40 were nearly 4 times more likely to use short-term contraceptives compared to younger women and 2 times more than those at older ages.
Education level was also significantly associated with the use of short-term contraceptives. Surprisingly women with primary education were more likely to adhere to the use of contraceptives (AOR 1.27 CI 1.05–1.52) compared to illiterate women, however there was no significant difference in the uptake of short-term contraception between those who had secondary and higher education and those with no education. An increase in the wealth index was also significantly associated with the uptake of short-term contraceptive use. The richest women were 2 times (AOR 1.99, CI 1.59–2.46) more likely to use short-term contraception compared to the poorest. Employed women were more likely (AOR 1.2, CI 1.01–1.42) to use short-term contraceptives compared to unemployed women. Region of residence equally played an important role in the uptake of contraceptives in Afghanistan (Table 2). The usage of short-term contraceptives was very high among women in the western region (AOR 2.06, CI 1.76–2.41) compared to the other 6 regions. Women living in the Northeastern, Northwestern, Eastern, and Southeastern regions were least likely to use short term contraceptives compared to those living in the central region. Regarding ethnicity, we considered the Pashtun ethnic group as a reference for having the largest proportion in the dataset and compared the other ethnic groups with this category. Only Balooch women did use short-term contraceptives significantly more often (AOR 1.23, CI 0.84–1.81) compared to the reference ethnic group, while Nooristani and Pashai women had the lowest ratios compared to the Pashtun group. Access to FP information also showed a strong association with short term contraceptive uptake. Women who had access to FP information were 1.4 (AOR 1.43, CI 1.29–1.59) times more likely using short-term contraceptives compared to those with no access. We also found an association between women empowerment and uptake of short-term contraception as partially empowered women were 1.55 (AOR 1.55, CI 1.36–1.75) times and fully empowered women were 1.23 (AOR 1.23, 1.09–1.38) times more likely to use short-term contraception compared to unempowered women. Interestingly we found that partially empowered women were more likely using short-term contraception than fully empowered women.
Discussion
Our results highlight that the majority of the women’s sociodemographic characteristics (age, literacy, marital status, wealth, ethnicity, region, access to FP information and women empowerment) were significantly associated with short-term contraceptive use, which supports our hypothesis. These results mostly follow the findings of several studies in the region and all over the world20,21,22,23,24, however to our surprise the place of residence did not make a significant difference which was not consistent with what was already known from the region17,25. Interestingly the association with living setting disappeared after adjusting for other characteristics, especially wealth. There could be many contextual implications for this result such as social and religious norms, financial dependency of women, cultural restrictions, and stigmatization towards seeking FP services, all of which affect the uptake of contraception in the entire population independent of their living setting. Moreover, short-term methods are easy to access (could be found easily in dispensaries), and easy to apply (they do not require skilled healthcare workers), therefore those living in rural areas are more likely to adhere to short-term methods, thus we did not find any significant difference in the uptake of short-term contraception between these two groups.
Similar to several studies in the region and other developing countries21,22,26, our study revealed a significant association between age and contraceptive use. In our study, the prevalence of short-term contraceptive uptake was higher among women aged between 30 and 40 years old while women younger than 20 years had the lowest rate. This could be due to several reasons: they are newly married and do not want to avoid pregnancy; these women are less aware of the methods27; reproductive health is still a taboo28 and thus, young women feel ashamed to discuss such issues and to seek FP services.
Region and ethnicity also play a role in the usage of contraception. There was a remarkable difference in contraception usage across different regions, as women living in the western parts of the country were 4 times more likely to use contraceptives compared to those who were living in the eastern region. Surprisingly a huge difference was found in the uptake of contraception among ethnic groups with Balooch women using contraception nearly 13 times more than Nooristani women. The basic conception behind these variations could be the geography and security concerns which may limit the provision of health services in these regions. Since Nooristan is a deprived and mountainous province in the east of Afghanistan, and it was highly insecure in 2015, this might explain the low uptake. The Balooch on the other had, live near the border between Afghanistan and Iran in the west of the country where there is better access to health services which may a strong contributor to the observed high contraceptive uptake.
Access to FP information is an important determinant of contraceptive uptake. In the DHS survey women were already considered as knowledgeable if they were able to name at least one method of FP. Having stated in the DHS survey to know about contraceptives does not necessarily imply knowledge about its correct application, nor does it determine actual use. What we looked at in our study was their exposure to FP information which we assumed, increased their knowledge about the methods, the benefits, side effects and further aspects of FP. This finding is consistent with other studies conducted in the region and other developing countries29,30,31. Moreover if we look towards other aspects, there could be discrepancies between knowledge and empowerment. The strong cultural anchor of having big families plays an important role which puts women under pressure to bear as many children as possible and not use contraceptives, even if they have knowledge on contraceptives. In our study we only looked at media exposure, and due to a huge number of missing values in the dataset, we did not include other channels (exposure at the health facility and information through community health workers). We found a significant association between media exposure and short-term contraceptive uptake, and we believe that if we had been able to include other channels into our analysis, the association might have become stronger.
Women empowerment has already been widely known as an important indicator which contributes to many health outcomes and similarly, we found a strong association between empowerment and use of short-term contraception. Gender equality provides the opportunity to a woman to freely discuss and decide about major health aspects specifically the reproductive health issues. Moreover, those women who have autonomy in their households are in a better position to have access to health services. An Interesting finding in our study was that partially empowered women were more likely using short-term contraception compared to fully empowered and unempowered. This statement can be supported by a culturally bonded norm where in Afghan families, women are getting more empowered and autonomous as they get grow older and older. Thus, we can assume that those women who are empowered are more of old ages of older ages, therefore and thus they are more likely to use contraception as we already also discussed it in the age category, however the relatively lower odds of contraception uptake in fully empowered women can be justified by their very old ages in which they might prefer to use long-term or permanent methods more often frequently than short -term ones.
Barriers of contraception uptake
Poor access to contraception, insufficient information about free provision of FP services, fear of side effects, insecurity, cultural and religious disagreements, and gender issues are considered potential barriers for contraception uptake in Afghanistan16,28,32. Since the majority of the population in Afghanistan is living under the poverty line33, we would conclude poor economic status as a barrier to contraception uptake. Furthermore, cultural beliefs such as preference of male children in certain regions of Afghanistan, social stigma and taboos against contraception, early marriage, familial pressures, and religious beliefs that stopping pregnancy is forbidden in Islam28, are important barriers for contraception uptake. Additionally, some people believe that large families are desirable for some reasons such as having someone to help parents in their old ages, securing economic status by having more people to work, and compensating possible losses due to conflicts.
Since we only conducted a quantitative analysis, we identified some of the potential barriers, but there might be some underpinning factors and barriers which need investigation using qualitative research methods.
Recommendations
FP is a wide area which requires a multisectoral collaboration and approach to promote in the society. Considering the country’s current emergency, particularly the suspension of world bank donation to the health system, there is a crucial need for efforts to strengthen the entire health system. As a result of the crisis, it is predicted that around 2331 health centers will be closed, and approximately 25,000 health workers including 7500 female workers will be unemployed in near future34. Moreover, with the decision of the new government, female workers got unemployed and banned from education. This lack of women’s access to health services, unavailability of essential medicines, lack of female health staff, and women unemployment will affect the entire health system specifically the health of mothers and children, contributing to an increment in the maternal mortality ratio as well as child and neonatal deaths. Therefore, advocacy for donors to support the area of mother and child health is the first suggestion for ensuring access and availability of health services, including FP methods. Community based provisions and the use of community health workers (CHWs) to educate both men and women and provide FP services is recommended. Mass media should be used to promote and advocate for FP. Since Afghanistan is a country in which religion plays an important role in daily life, one of the effective approaches to advocate for the promotion of FP would be to use religious leaders in the society. Some small-scale initiatives have already been launched in this regard, showing promising results35. Inclusion of FP methods as clinical attachments or as part of the medical and nursing curriculum which is currently lacking, as well as regular trainings for service providers on correct and comprehensive counseling are also known to be effective approaches for contraceptive promotion. Improving logistics and supply chain management specifically in the eastern parts of the country would be a crucial step.
There have been many basic improvements in FP in recent decades in Afghanistan, such as the development of the Reproductive, Maternal, Newborn, Child, and Adolescent Health (RMNCH) strategy, a costed implementation plan36, and commitment to the vision of FP2020 by increasing the number of health centers providing family planning services, and adding implants to the essential medicine list37, we still need to strengthen the initiatives.
We also suggest conducting qualitative research to find out the reason behind non-use and discontinuation of contraceptive methods. Conducting Focus Group Discussions and In-depth interviews not only with women but also with husbands and in-laws about different aspects of FP such as expectations of the society, decision making regarding FP, and level of knowledge on contraception, is highly recommended.
The aforementioned recommendations could serve the policy makers in the future government of Afghanistan to develop and implement interventions based on empirical evidence which may contribute to the improvement of the health sector, especially the field of mother and child health.
Strengths and limitations
Using DHS data provides us with a trustworthy source and good data quality compared to many single studies. However, in the original study it was assumed that security issues might not have allowed to cover all the selected areas, therefore 101 reserve clusters were selected for replacement and later 70 clusters replaced the areas which were identified insecure. At the end the AfDHS was unable to collect data from Zabul province in the southeastern region due to security concerns. This issue might have resulted in underestimating the national prevalence rate, because Zabul province is mostly occupied by Pashtun women. The large sample size of 22,974 participants provides a solid basis for statistically robust uni- and multivariable analyses, which is corroborated by the strict confidence interval of 99% employed in this study.
On the other hand, the cross-sectional design of the study restricts the establishment of causal relationships between outcome and exposure. Moreover, some of the potential influencing factors such as number of children, distance from the health facility, and number of ANC visits were not included in this study which might have introduced some residual confounding to this analysis. In addition, men were not included in this analysis. Since this dataset only included married women, we can consider this as a potential limitation of the analysis because there might be higher unmet need for contraception among sexually active unmarried women.
Additionally, the dataset had 44 (0.2%) missing values for ethnicity, 19 (0.1%) missing values for occupation, access to FP information had 85 (0.4%) missing values and the women empowerment variable had 866 (3.8%) missing values. Regarding the women empowerment variable, most probably the questions were too sensitive to be answered by all which resulted in information bias.
Conclusion
Our study revealed a good awareness of the Afghan women on contraceptive methods; however, the use of short-term contraceptives remains low, with only one fifth of the sample population employing them. Low utilization of FP is driven by security, cultural belief, geography, wealth, knowledge, and age. Therefore, policy makers should collaboratively put in place measures to secure funding for the area of mother and child health, enhance mass education on contraception, reduce the barriers on the access to FP services, promote education and employment for women, and deploy efforts to address the misconceptions on FP methods.
Data availability
We used the Afghanistan DHS 2015 dataset which is openly available under https://dhsprogram.com/data/available-datasets.cfm.
Abbreviations
- FP:
-
Family Planning
- DHS:
-
Demographic and Health Survey
- FGD:
-
Focus Group Discussion
- WHO:
-
World Health Organization
- ICF:
-
Inner city Fund
- CHW:
-
Community Health Workers
- RMNCH:
-
Reproductive, maternal, newborn, child, and adolescent health
References
Bongaarts, J. Does family planning reduce infant mortality rates?. Popul. Dev. Rev. 13(2), 323–334 (1987).
Ahmed, S., Li, Q., Liu, L. & Tsui, A. O. Maternal deaths averted by contraceptive use: An analysis of 172 countries. Lancet 380(9837), 111–125 (2012).
Shaw, D. The ABC’s of Family Planning (University of Britis, 2010).
Johns Hopkins Bloomberg School of Public Health. Contraceptive Use Averts 272,000 Maternal Deaths Worldwide 2012. https://publichealth.jhu.edu/2012/ahmed-contraception.
Bradshaw, C. J. A. et al. Lower infant mortality and access to contraception reduce fertility in low- and middle-income nations. MedRxiv. 2021, 1–23 (2021).
United Nations. Trends in Contraceptive Use Worldwide (Department of Economic and Social Affairs: Population Division, 2015).
World Health Organization. Family Planning/Contraception 2018. https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception. Accessed 2 April 2020.
Cleland, J., Conde-Agudelo, A., Peterson, H., Ross, J. & Tsui, A. Contraception and health. The Lancet. 380(9837), 149–156 (2012).
Central Statistics Organization Afghanistan. Ministry of Public Health, ICF a Afghanistan Demographic and Health Survey (ADHS) 2015 (Central Statistics Organization, 2017).
World Health Organization. Maternal Mortality in 2000–2017. https://www.who.int/gho/maternal_health/countries/afg.pdf. Accessed 2 April 2020.
Central Statistics Organization Afghanistan. Ministry of Public Health (Institute aKRT, Afghanistan Health Survey, 2019).
Un.org. World Population Prospects: The 2017 Revision|Multimedia Library: United Nations Department of Economic and Social Affairs. United Nations. https://www.un.org/development/desa/publications/world-population-prospects-the-2017-revision.html. Accessed 4 May 2019.
Osmani, A. K., Reyer, J. A., Osmani, A. R. & Hamajima, N. Factors influencing contraceptive use among women in Afghanistan: Secondary analysis of Afghanistan Health Survey 2012. Nagoya J. Med. Sci. 77(4), 551–561 (2015).
World Bank. Contraceptive prevalence, any methods (% of women ages 15–49). The World Bank Data 2019 https://data.worldbank.org/indicator/SP.DYN.CONU.ZS. Accessed 4 May 2019.
Sabawoon, A., Anwar, I. & Behzad, A. Factors Affecting Contraceptive Use and Unmet Need among Currently Married Women in Afghanistan: Further Analysis of the 2015 Afghanistan Demographic and Health Survey. DHS Working Paper (2018).
Packer, C. A. et al. Factors associated with reported modern contraceptive use among married men in Afghanistan. Reprod. Health. 17(1), 64 (2020).
Rasooly, M. H., Ali, M. M., Brown, N. J. & Noormal, B. Uptake and predictors of contraceptive use in Afghan women. BMC Womens Health. 15, 9 (2015).
Tibaijuka, L. et al. Factors influencing use of long-acting versus short-acting contraceptive methods among reproductive-age women in a resource-limited setting. BMC Womens Health. 17(1), 25 (2017).
ICF International. DHS Sampling and Household Listing Manual: Demographic and Health Surveys Methodology (MEASURE DHS, 2012).
Baksu, A., Gunes, G., Aki, G., Tuysuz, F. & Goker, N. Change in contraceptive choices and the effect of education on use of contraception at the family planning clinic of Sisli Etfal Training and Research Hospital, Istanbul, Turkey. Eur. J. Contracept. Reprod. Health Care. 10(2), 98–104 (2005).
Stephenson, R., Baschieri, A., Clements, S., Hennink, M. & Madise, N. Contextual influences on modern contraceptive use in sub-Saharan Africa. Am. J. Public Health. 97(7), 1233–1240 (2007).
Okech, T. C., Wawire, D. N. W. & Mburu, D. T. K. Contraceptive use among women of reproductive age in Kenya’s city slums. Int. J. Bus. Soc. Sci. 2011, 2 (2011).
Novignon, J. Trend and determinants of contraceptive use among women of reproductive age in Ghana. APS 28, 956 (2014).
Adeyemi, A. S. et al. Contraceptive prevalence and determinants among women of reproductive age group in Ogbomoso, Oyo State, Nigeria. Open Access J. Contracept. 7, 33–41 (2016).
Uddin, M. M., Kabir, M., Choudhury, S. R., Ahmed, T. & Bhuyan, M. R. Rural-urban differential in contraceptive use status in Bangladesh. Rural Demogr. 12(1–2), 1–20 (1985).
Arbab, A. A., Bener, A. & Abdulmalik, M. Prevalence, awareness and determinants of contraceptive use in Qatari women. East Mediterr. Health J. 17(1), 11–18 (2011).
Craig, A. D., Dehlendorf, C., Borrero, S., Harper, C. C. & Rocca, C. H. Exploring young adults’ contraceptive knowledge and attitudes: Disparities by race/ethnicity and age. Womens Health Issues. 24(3), e281–e289 (2014).
Shafiqullah, H., Morita, A., Nakamura, K. & Seino, K. The family planning conundrum in Afghanistan. Health Promot. Int. 33(2), 311–317 (2018).
Cohen, B. Family planning programs, socioeconomic characteristics, and contraceptive use in Malawi. World Dev. 28(5), 843–860 (2000).
Okigbo, C. C., Speizer, I. S., Corroon, M. & Gueye, A. Exposure to family planning messages and modern contraceptive use among men in urban Kenya, Nigeria, and Senegal: A cross-sectional study. Reprod. Health. 12, 63 (2015).
Zahra, F. & Kahn, J. R. Does the message matter?: Family planning message exposure and women’s birth spacing intentions in Pakistan. Reprod. Health. 1, 1–10 (2017).
Samar, S. et al. Towards gender equality in health in Afghanistan. Glob. Public Health. 9(Suppl 1), S76-92 (2014).
World Data Lab. World Poverty Clock 2019. https://worldpoverty.io/?utm_source=google&utm_medium=search&utm_campaign=WorldpovertyData&campaignid=1695797724&adgroupid=67866496684&adid=329359366977&gclid=CjwKCAjwza_mBRBTEiwASDWVvo6gX-zkS2ooSKzjYQIQartrdGjGyG3qm8n2vc0I8rAjBnujZK-B5hoCOegQAvD_BwE. Accessed 4 May 2019.
Safi, N., Singh, L. S., Naseri, S. & Anwari, P. An alternative model for health service delivery in Afghanistan. Lancet 398(10310), 1481–1482 (2021).
Sato, M. Challenges and Successes in Family Planning in Afghanistan (Springer, 2007).
Health MoP. Birth Spacing/Family Planning Costed Implementation Plan (CIP) 2018-20222018.
FP 2020. Afghanistan Commitment Maker Since 2016. https://www.familyplanning2020.org/afghanistan. Accessed 14 Nov 2019.
Acknowledgements
We greatly acknowledge the DHS program granting access to the 2015 Afghanistan Demographic and Health Survey data. The tireless support and cooperation given by the entire team involved in this study at the Heidelberg Institute of Global Health as well as a DAAD scholarship that made conducting this research possible is highly acknowledged.
Author information
Authors and Affiliations
Contributions
S.N. and P.D., conceived and planned the research. S.N. developed the theory, designed the model and the computational framework, analyzed the data, and wrote the manuscript with close coordination of P.D. and V.W. V.W. contributed to the analysis of the data and advised and supervised the whole process of data analysis. I.S. contributed to developing the idea of research, data cleaning process, and data analysis. A.D. contributed to data analysis and critically provided feedback on the revision of the manuscript. A.M.E. provided critical feedback and helped shape the research, analysis, and data interpretation. All authors approved the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Noormal, A.S., Winkler, V., Eshraqi, A.M. et al. Factors influencing the uptake of short-term contraceptives among women in Afghanistan. Sci Rep 12, 6632 (2022). https://doi.org/10.1038/s41598-022-10535-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10535-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.