Abstract
In this study, we investigate the influence of the seven genes (VHL, PBRM1, SETD2, BAP1, KDM5C, MTOR and TP53) most frequently mutated in clear cell renal cell cancer (ccRCC) on cancer-specific survival (CSS) in the prospective Netherlands Cohort Study on diet and cancer. DNA isolated from routinely archived formalin-fixed paraffin-embedded tumour blocks from 252 incident ccRCC cases was available for targeted next generation sequencing. Based on the sequencing quality and the completeness of information on clinical characteristics and follow-up, we could use 110 cases for survival analysis. The association with CSS for each mutated gene in these cases was tested using multivariable Cox proportional hazards models to estimate hazards ratios (HR) and confidence intervals (CIs), and we observed mutations in one or more of the seven genes in 64 out of 110 cases (58%). In the multivariable-adjusted analyses, mutations in VHL and PBRM1 were associated with better CSS (HRs (95% CI) 0.34 (0.13‒0.89) and 0.17 (0.04–0.66), respectively), although these results were not statistically significant after multiple testing correction. No association was observed for the other five genes, which may be attributable to limited power.
Similar content being viewed by others
Introduction
Kidney cancer is an often lethal disease with a mortality rate of 3 per 100,000 population in Western Europe1. Renal cell cancer (RCC) accounts for approximately 90% of all kidney cancer, with clear cell renal cell carcinoma (ccRCC) being the most common RCC subtype (70%)2,3. Various clinical characteristics have been established as prognostic factors for ccRCC, including tumour size, stage, grade and necrosis4. In addition to these clinical characteristics, the mutational profile of the tumour may also be a prognostic factor. High-throughput sequencing databases such as the Catalogue of Somatic Mutations in Cancer (COSMIC) and The Cancer Genome Atlas (TCGA) project provide a clear overview of the genes that are frequently mutated in ccRCC5,6. Based on 512 ccRCC cases in the PanCancer study of TCGA, the most frequently mutated genes in ccRCC are: VHL (41%), PBRM1 (38%), SETD2 (12%), BAP1 (10%), MTOR (8%) and KDM5C (5%)6,7,8. In addition, while the mutation rate of TP53 in the TCGA is low (3%), the COSMIC database indicates that TP53 may also be frequently mutated in ccRCC (7%)9.
These genes have been implicated in a number of ccRCC-related processes. Inactivation of the VHL tumour-suppressor gene leads to disrupted molecular oxygen sensing10, whereas PBRM1, SETD2, KDM5C and BAP1 are chromatin-modifying proteins, and their inactivation is a prominent feature in the development of ccRCC10,11,12,13. MTOR, which is part of the PI3K/AKT/mTOR signalling pathway, is involved in multiple biological functions that regulate cell growth (e.g. cell survival, metabolism and proliferation) and represents a promising therapeutic target14,15,16. However, while the roles of all these genes in the development of ccRCC has been extensively investigated, there is less evidence regarding their role in ccRCC prognosis. In previous studies, mutations in BAP1, SETD2, KDM5C and TP53 have been associated with an unfavourable prognosis in ccRCC17,18,19, but the BAP1 association is the only one that has been consistently reported by several studies (Supplementary Table S1.1). No consistent associations with cancer-specific survival (CSS) have been found for VHL, PBRM1 and MTOR18,19,20,21,22.
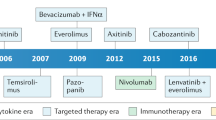
In the present study, we assessed the association between mutations in the most frequently mutated genes in ccRCC—VHL, PBRM1, SETD2, BAP1, MTOR, KDM5C and TP53—and CSS. In addition, we evaluated the association between the co-occurrence of mutations in these genes and CSS using data from the Netherlands Cohort Study on diet and cancer (NLCS), a large-scale population-based prospective cohort study with a long follow-up (23.3 years)23. A characteristic feature of the NLCS cohort is its treatment-naive population. Because surgery was the default ccRCC therapy and targeted therapies were not widely available in the period when most included patients were diagnosed (1986‒2008), only a few patients received adjuvant therapy in the first 3 months post-diagnosis.
Results
Targeted sequencing
The characteristics of the cases and samples and the mutation frequency of the genes included in the analysis are described in Table 1. Supplementary Table S2.1 provides an overview of sample and sequencing characteristics for all 252 sequenced samples and the 121 samples ultimately included in analyses. The mean duration of storage of the formalin-fixed paraffin-embedded (FFPE) tissue blocks was 9.8 years (SD 3.3), and a longer duration of storage before DNA isolation was associated with a lower DNA concentration in stock after DNA isolation, while the amount of DNA fragmentation was associated with a reduction in average read depth (Supplementary Table S2.2). Overall, 72 of the 121 (59.5%) cases had mutations in at least one of the seven target genes, and we identified 45 (37.2%) mutations in VHL, 27 (22.3%) in PBRM1, 14 (11.6%) in SETD2, 12 (9.9%) in KDM5C, 7 (5.8%) in BAP1 was, 3 (2.5%) in MTOR and 3 (2.5%) in TP53 (see Fig. 1).
Combinations of mutations present in ccRCC cases in the Netherlands Cohort Study on diet and cancer (N = 121). (A) Mutation frequency for the seven selected genes. (B) Co-mutation plot of all sequenced samples. Each column represents one ccRCC case. Mutations in the individual genes labelled on the left are shown by the grey-blue bars.
Mutations and clinical characteristics
Based on sequencing quality, 121 ccRCC cases were available for further analysis. However, due to missing data, the final number of cases varied slightly per clinical characteristic (Table 2). Of the seven selected genes, four (VHL, PBRM1, SETD2 and KDM5C) were mutated in at least 10 cases and thus included in our logistic regression models of the association with clinical characteristics (Table 2). In neither the univariable models nor the multivariable-adjusted models did we observe a statistically significant association between tumour characteristics and the mutation status of VHL, PBRM1, SETD2 and KDM5C.
To assess the association between clinical characteristics and mutation status, we performed sensitivity analyses using Pearson chi-square tests, where applicable (Supplementary Table S1.2). These sensitivity analyses were performed to confirm findings from logistic regression models and gain insight into the associations for the genes for which there were too few cases with a mutation to assess using regression models. Here again, similar to the logistic regression models, we found no association with tumour grade, stage or size for VHL, PBRM1, SETD2 and KDM5C. Nor was any association found between these clinical characteristics and mutations in BAP1, MTOR and TP53.
Survival analysis
After excluding cases missing clinical information about a priori confounders, we included 110 cases in the survival analyses. Overall, no mutations were identified in 46 cases. Kaplan–Meier curves for the association of mutated PBRM1 or VHL with CSS are displayed in Fig. 2A,B, respectively. Cases with PBRM1 mutations had a higher CSS than cases without a PBRM1 mutation, although this association only reached borderline statistical significance (p-value = 0.057, Wilcoxon test). Mutations in VHL seemed beneficial to CSS, although these results were not statistically significant (p-value = 0.118, Wilcoxon test). In age- and sex-adjusted Cox regression models truncated at 10 years of follow-up (model 1, Table 3), we observed an increased CSS for patients with VHL mutations [Hazard Ratio (HR) (95% Confidence Interval (CI)] 0.53 (0.24–1.17) or PBRM1 mutations [HR (95% CI) 0.36 (0.12–1.01)] compared to those without VHL or PBRM1 mutations, although this was again not statistically significant. In the multivariable-adjusted results (model 2, Table 3) that included patient clinical characteristics (tumour grade, size and stage), the association became stronger [HR (95% CI), VHL = 0.33 (0.14–0.79), PBRM1 = 0.25 (0.08–0.79)]. Cases with mutations in VHL had a statistically significant increased CSS compared to cases without mutations in VHL [HR (95% CI) 0.33 (0.14–0.79)], and we found similar associations for PBRM1 mutations [HR (95% CI) 0.26 (0.08–0.79)]. After mutual adjustment for other genes, excluding MTOR due to the instability of the estimations (model 3, Table 3), the association of PBRM1 with CSS became slightly stronger [HR (95% CI) 0.17 (0.04–0.66)], while the association of VHL remained the same [HR (95% CI) 0.34 (0.13–0.89)]. The statistically significant effect of VHL and PBRM1 mutations on CSS became non-significant after multiple testing correction using the Benjamini–Hochberg method (q-values = 0.063 and 0.063, respectively).
The association between other mutated genes and CSS should be interpreted with caution given the low number of ccRCC-related deaths in our study population. Overall, we observed that mutations in most genes were related to an increased survival (with the exceptions of KDM5C and SETD2), although most of the findings were not statistically significant and were based on a small number of cases (Table 3).
Sensitivity analyses using the complete time of follow-up but truncating the analyses at 5-years follow-up found similar results to those for 10 years of follow-up (Supplementary Tables S1.3, S1.4). Differences were only observed for SETD2, with the effect of SETD2 mutations became less favourable when truncating follow-up time. This effect is likely influenced by the high number of deaths among cases with SETD2 mutations at the beginning of follow-up, as seen in the Kaplan–Meier curve (Supplementary Fig. S1.1).
Co-occurrence of VHL and PBRM1 mutations
The inventory of single occurrence or co-occurrence of mutated genes in all 121 cases was dominated by the presence of cases with mutations in VHL only, followed by cases with mutations in both VHL and PBRM1, cases with PBRM1 mutations only and cases with VHL and SETD2 mutations (Fig. 1). Given the frequent co-occurrence of VHL and PBRM1 mutations, we assessed the influence of having: (1) either no VHL or PBRM1 mutation, (2) a mutated VHL gene or PBRM1 gene, or (3) a mutation in both VHL and PBRM1. The effect of VHL and PBRM1 mutations is visualized in the Kaplan–Meier curves in Fig. 2C. Here we observed that the highest CSS occurs with presence of mutations in both genes and the lowest CSS with the absence of mutations in both genes. Cox regression analysis assessing the combination of PBRM1 and VHL found similar effect estimates for a VHL mutation without a PBRM1 mutation and for a PBRM1 mutation without a VHL mutation (model 3), as compared to the per-gene analyses [HR (95% CI) 0.32 (0.11–0.94), p-value = 0.039 and HR (95% CI) 0.16 (0.03–0.80), p-value = 0.026, respectively]. After FDR-adjustment, none of these associations remained statistically significant (Table 3). Even though we observed an even stronger association of the co-occurrence of VHL and PBRM1 mutations with CSS, we cannot draw clear inferences from these results due to limited statistical power. Given the lack of statistical power, we did not assess the less frequent combinations of other mutated genes (Fig. 1B).
Discussion
We investigated the association between mutations in the seven genes most frequently mutated in ccRCC and CSS in a large-scale prospective cohort featuring long-term follow-up of a population-based selection of cases who underwent surgery for ccRCC but only rarely received adjuvant treatment in the first 3 months post-diagnosis. As expected, VHL was the most frequently mutated gene, followed by PBRM1, SETD2, KDM5C, BAP1, MTOR and TP53, with mutation frequencies in line with those reported by the TCGA PanCancer project6.
In our study, the presence of mutations in VHL and/or PBRM1 was associated with a favourable CSS, and this association became stronger after adjustment for clinical characteristics. These effects appear to be independent of each other, as similar associations with CSS were observed when assessing patients who had mutations in VHL but not PBRM1, and vice versa. Prior to FDR-correction, we also observed a statistically significant association of the co-occurrence of PBRM1 and VHL mutations to CSS, but we cannot draw conclusions from these results due to the low number of ccRCC-related deaths in this subgroup. In a previous study19, data from the Memorial Sloan Kettering Cancer Center cohort showed no clear effect on CSS for combined VHL and PBRM1 mutations, whereas data from the TCGA suggested a slightly worse CSS.
Supplementary Table S1.1 briefly summarizes CSS data from other studies. In one study, PBRM1 mutations did show a trend toward favourable CSS, although the association was not statistically significant [HR (95% CI) 0.87 (0.57‒1.34), p-value = 0.528]18. Only one out of several studies reported that the group of VHL mutation carriers showed a trend toward favourable CSS21, although this association was also not statistically significant [HR (95% CI) 0.53 (0.25‒1.09), p-value = 0.079]. In a study based on ccRCC cases from the NLCS from 1986 to 199725, all diagnosed using a combination of single-stranded conformational polymorphism and direct sequencing, no association between VHL mutations and CSS was reported22. However, when we restricted our analysis to those cases diagnosed before 1997 to assess differences between the two studies within the same cohort (data not shown), we found results similar to our main analyses. It is noteworthy that, in analyses by Smits et al., the proportion of cases with a mutation in VHL is higher (52.5%) than in our study (30.1%) when only looking cases diagnosed up to 199722. This discordance in results may be caused by the relatively conservative variant calling thresholds employed in our study.
It is still unclear how mutations in both PBRM1 and VHL might lead to a more favourable CSS. PBRM1 and VHL mutations are known to be enriched in the early events of ccRCC development, whereas other mutated genes play a role in ccRCC progression26,27. This is in line with a previously reported in vivo study that showed that mice deficient for both VHL and PBRM1 develop only low-grade kidney cancer28. A statistically significant association has previously been reported between the presence of mutations in PBRM1 and low-grade ccRCC tumours in patients29, but no association was found between mutations in VHL and tumour grade25. In our study, neither PBRM1 nor VHL was significantly associated with lower grade tumours. In addition, all the survival analyses in our study were adjusted for tumour grade, thus we do not believe that the associations we observed were affected by tumour grade.
While it was not statistically significant, we did observe a potential association between VHL mutations and tumour stage and size. There was already some conflicting evidence on these associations, as one prior study observed similar associations30, whereas another did not31. In our study, multivariable models were adjusted for underlying clinical characteristics, which leads us to believe that the protective effects on CSS we observe for mutations in VHL and PBRM1 are independent of underlying tumour characteristics.
In our study, selective drop-out may have occurred with the exclusion of cases with insufficient read depth. However, chi-square tests detected no difference in the distribution of clinical characteristics between the 252 cases eligible for DNA sequencing and the 121 samples ultimately included in analyses (data not shown). Furthermore, we observed no clear differences in the effect of clinical characteristics on the prognosis of ccRCC in Cox regression models between these two subsets (data not shown). We therefore assume that the effect of selection bias is limited. After drop-out, we had a more-limited sample size and a low prevalence of individual gene mutation frequencies, which led to lower power to detect associations, especially after adjusting for multiple testing. This is apparent in the imprecision of our results, which often show wide CIs. Overall, the frequencies of mutations we observe are in line with the mutation frequencies reported by the TCGA PanCancer project, which adds credibility to our findings6,7,8. We may have been hampered by a limited number of cases with tumour stage IV, as these patients were less likely to receive surgical treatment22. Given the years in which tumour classification was performed, our study uses an older tumour grade classification (Fuhrman grading system)32,33 and tumour staging system (UICC staging system)24. One of the main differences between these classifications was the T-stage threshold between T1 and T2 with regards to tumour size. To remedy this, we combined tumour stages 1 and 2 into one category and adjusted all our models that included tumour stage by tumour size.
This study was subject to limitations. Firstly, no information was available on the methylation status of the genes included in the panel, even though prior studies have implicated promoter methylation in the inactivation of VHL. In this study, we only assessed the effect of mutation status, not the effect of hypermethylation on the inactivation of VHL. As a result, we may have underestimated the proportion of cases with inactivation of VHL. The additional effect on CSS of inactivation through hypermethylation in VHL remains inconclusive based on currently available evidence and thus provides a valuable research opportunity for future studies22,34,35. Secondly, due to the limited power in analyses for SETD2, KDM5C, BAP1, TP53 and MTOR, we were unable to assess the influence of specific combination of mutations. This highlights the need for larger-scale studies in order to gain additional insights into mutational patterns.
One of the strengths of our study is that it is based on a large population-based prospective cohort study. Our sample population is homogenously collected from one country, which contrasts with other studies, which have mostly included cohorts from multiple countries with varying healthcare systems or case series from individual specialised centres. In addition, adjuvant treatment may cause difficulties in discerning effects between high and low risk groups in prognostic studies36. However, our population received limited adjuvant treatment after surgery. Based on information detailing the treatment plan for the first 3 months post-diagnosis, only one case out of 121 was reported to have received immunotherapy. This study is thus able to provide insights into the effects of somatic mutations on the prognosis, with no or limited influence of preoperative treatment. This may aid researchers and clinicians in gaining a better understanding of the intrinsic mechanism that drives ccRCC prognosis. In recent studies, the incorporation of genomics into risk models for prognostication of RCC has been shown to improve the model prediction. The somatic mutational profile of tumours may enable clinicians to identify patients with an expected poorer prognosis, opening up the opportunity to adjust their treatment strategy accordingly37,38.
Materials and methods
Study population
Our study population was derived from the NLCS, a prospective cohort study initiated in 198623. As described in detail elsewhere, the NLCS included 120,852 participants aged 55‒69 years at baseline39. The entire cohort was followed for cancer incidence by record linkage with the Netherlands Cancer Registry, the Dutch pathology registry (PALGA) and Statistics Netherlands (CBS). The completeness of cancer follow-up through record linkage is estimated to be over 96%40.
Ethics statement
Individuals invited to participate in the NLCS received an invitation letter with details on the study and the use of their data. In addition, they received the baseline questionnaire, which included an envelope for returning toenail clippings. By completing and returning the baseline questionnaire, individuals provided informed consented to participate in the NLCS (response rate 35.5%). Individuals were informed about the possibility to end their participation at any time, at which point all their data would be removed. All methods were performed in accordance with the relevant guidelines and regulations applicable at that time (1986). The institutional review boards of Maastricht University (Maastricht) and the Netherlands Organization for Applied Scientific Research TNO (Zeist) approved the NLCS (on February 2, 1985 and January 6, 1986, respectively). In addition, the institutional review board of Maastricht University (Maastricht) later re-evaluated the original approval of the study protocol and procedures and amended the original approval to include the collection and genetic analysis of tumour blocks (April 12, 2010). Participants did not provide written informed consent to the sharing of data.
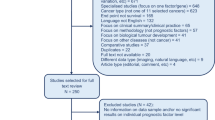
Sample collection
In total, 608 RCC cases were identified in 20.3 years of follow-up from 1986 to 2006 (Fig. 3)23. Among these cases, 568 histologically confirmed RCC cases identified through PALGA were selected for the collection of FFPE tissue blocks. FFPE blocks were successfully retrieved from 51 pathology laboratories for 454 cases. Tumour type histology was revised by two experienced uropathologists using the WHO-classification of tumours3. Of the 454 cases, 366 were of the ccRCC type23. DNA was isolated from collected paraffin tissue blocks in two series. Series 1 included patients diagnosed between 1986 and 1997 and DNA samples collected in 200325. Series 2 included patients diagnosed between 1997 and 2008 and DNA samples collected in 201223. Follow-up was completed up to 31 December 2009. For our study, we selected 252 out of the 366 ccRCC cases based on the availability of sufficient DNA to perform targeted sequencing. In Series 1 samples, the tumour cell fraction was estimated by visual inspection of H&E-stained tissue sections by an uropathologist and varied between 20 and 100% (median 95%). In Series 2, all tumour blocks were subjected to macrodissection of the tumour area in order to enrich for tumour cells prior to DNA analysis. The investigations involving human samples were conducted according to the Declaration of Helsinki41 and were covered by the METC permit MEC 85-012-8/ah.
Targeted sequencing
All DNA samples were subjected to a unique molecular identifier‒based targeted sequencing approach based on Single Primer Enrichment Technology (Ovation™ Custom Target Enrichment System, NuGEN, San Carlos, CA, USA). We applied our previously designed custom landing probe panel for enrichment of the consensus coding regions of the 32 genes most frequently mutated in ccRCC, supplemented with 10 genes associated with the VHL/HIF pathway and the (PI3K)-AKT-MTOR pathway in ccRCC42,43.
DNA samples from 252 ccRCC cases were subjected to our sequencing protocol. Aliquots of 500 ng DNA were sheared into 500-bp fragments by Adaptive Focused Acoustics™ (Covaris, Woburn, MA, USA) and subjected to targeted sequencing, as described previously42. Enriched libraries were sequenced with the Illumina HISEQ 2500™ (Illumina, San Diego, CA, USA) using single-end next generation sequencing with 100-bp reads. The average read depth per gene varied from 13 to 57.
Sequence data analysis and somatic mutation identification
Sequencing data were processed using a pipeline following the Genome Analysis Toolkit (GATK) best practice recommendations, with HaplotypeCaller from GATK and FreeBayes used as variant caller44,45. Called variants were annotated and filtered to identify true somatic mutations, as described previously42. For the current study, we focussed on the six genes with a mutation frequency ≥ 5% in the TCGA PanCancer database, VHL, PBRM1, SETD2, BAP1, MTOR and KDM5C6, supplemented with TP53 because of its high mutation frequency (7%) in the COSMIC database9. To minimize the chance of false positive results, samples were only included for further analysis if they had an average read depth of at least 20 unique reads for six genes and a read depth of at least 15 for TP53. Next, we determined the somatic variant with the highest mutant allele frequency (MAF) in each patient. Variants with a MAF ≥ 50% of the highest MAF seen on a per sample basis and ≥ 4 mutant reads were considered major variants. This method helps to account for variations in tumour content between samples. The absolute mutant read threshold limits the number of false positives in regions with low coverage. Major clone variants present in more than four samples were excluded because they are likely due to sequencing errors or common population-specific variants. The Integrative Genomic Viewer was used to confirm the authenticity of any doubtful somatic mutations46.
The sizeable drop-out (52%) when we restricted our study to samples with an average read depth of at least 20 for six out of the seven genes led us to analyse which sample characteristics were associated with the average read depth of samples under study. This issue is discussed in detail in the Supplementary Data S2.
Clinical characteristic assessment
Clinical characteristics at diagnosis were derived from excerpts of pathology reports provided by PALGA. From this information, tumour size was assessed based on the largest diameter and was categorized into two tier groups: diameter ≤ 70 mm and diameter > 70 mm17. The morphological features of ccRCC and the tumour grade were assessed by two pathologists23 using the Fuhrman tumour grade system32,33. Tumour stage was provided by the Netherlands Cancer Registry and updated with information from the pathology reports according to the UICC TNM staging system24. Information on the cause of death, RCC-related (ICD-10: C64) or other, was obtained from Statistics Netherlands (CBS).
Statistical analysis
Statistical analysis was performed using Stata statistical software: release 15 (StataCorp., 2015, College Station, TX). The association between mutated genes and tumour stage (stage 1 and 2 vs. stage 3 and 4), tumour grade (grade 1 and 2 vs. grade 3 and 4) and tumour size (≤ 70 mm vs. > 70 mm and continuous) was examined in both univariable and mutually adjusted logistic regression models. We only included genes with at least 10 cases with a mutation in logistic regression analyses. In a sensitivity analysis, we performed univariable analyses for all seven selected genes using chi-square tests. If cells contained five or fewer cases, Fisher’s exact test was used.
We tested the association of each mutated gene with CSS. The survival time (in years) was measured from the time of first diagnosis to the time of death. Cox proportional hazards models were used to estimate HRs and 95% CIs. Analyses were performed using both an age- and sex-adjusted model (model 1) and a multivariable-adjusted model (model 2) that included the following a priori selected confounders: age at diagnosis, sex, tumour grade, tumour size and tumour stage. In model 3, the co-occurrence of mutations in the seven genes was added to model 2. A two-sided p-value < 0.05 was considered statistically significant. Multiple testing correction using the Benjamini–Hochberg method47 was performed for model 348. False discovery-adjusted p-values, i.e. q-values, were considered statistically significant if q < 0.05. Sensitivity analyses were done using the complete time of follow-up and truncating the follow-up time to 5 years. The proportional hazards assumption was tested using the scaled Schoenfeld residuals and log–log curves49. Kaplan–Meier curves and Wilcoxon tests were used to evaluate the cause-specific survival of ccRCC cases with and without each mutated gene. For all cases included in the Cox regression analysis, we also made an inventory of the co-occurrence of mutations involving multiple genes in order to select the most frequent combinations to test for an effect on CSS. In addition, we assessed whether correcting for the collection series had any effect on the survival analysis results. As adjusting for the collection series (Series 1 vs. Series 2) did not largely influence results, and the conclusions remained similar (data not shown), we only present the results unadjusted for collection series.
Conclusions
In summary, we observe an association between mutations in VHL and PBRM1 and a favourable ccRCC-specific survival. This effect persisted after adjustment for clinical characteristics and the presence of co-occurring mutations in frequently mutated genes in ccRCC. However, the association did not maintain statistical significance after correction for multiple testing, which may be attributed to the low number of samples.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available because the participants did not provide written informed consent to the sharing of data.
References
Ferlay, J., Ervik, M., Lam, F., Colombet, M., Mery, L., Piñeros, M., Znaor, A., Soerjomataram, I., Bray, F. Global Cancer Observatory: Cancer Today. https://gco.iarc.fr/today (accessed on 22 Apr 2020).
Ljungberg, B. et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol 67, 913–924. https://doi.org/10.1016/j.eururo.2015.01.005 (2015).
Eble, J., Sauter, G., Epstein, J., Sesterhenn, I. World Health Organization Classification of Tumours. Pathology and Genetics. Tumours of the Urinary System and Male Genital Organs (IARC Press, 2004).
Frank, I. et al. An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: The SSIGN score. J. Urol. 168, 2395–2400. https://doi.org/10.1097/01.ju.0000035885.91935.d5 (2002).
Forbes, S. A. et al. COSMIC: Somatic cancer genetics at high-resolution. Nucleic Acids Res. 45, D777–D783. https://doi.org/10.1093/nar/gkw1121 (2017).
Cancer Genome Atlas Research Network. Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature 499, 43–49. https://doi.org/10.1038/nature12222 (2013).
Cerami, E. et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2, 401–404. https://doi.org/10.1158/2159-8290.Cd-12-0095 (2012).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal 6, 1. https://doi.org/10.1126/scisignal.2004088 (2013).
Forbes, S. A. et al. COSMIC: Mining complete cancer genomes in the Catalogue of Somatic Mutations in Cancer. Nucleic Acids Res. 39, D945-950. https://doi.org/10.1093/nar/gkq929 (2011).
Kim, H. S., Kim, J. H., Jang, H. J., Han, B. & Zang, D. Y. Clinicopathologic significance of VHL gene alteration in clear-cell renal cell carcinoma: An updated meta-analysis and review. Int. J. Mol. Sci. https://doi.org/10.3390/ijms19092529 (2018).
Zhang, J. & Zhang, Q. VHL and hypoxia signaling: Beyond HIF in cancer. Biomedicines 6, 35. https://doi.org/10.3390/biomedicines6010035 (2018).
Sanchez, D. J. & Simon, M. C. Genetic and metabolic hallmarks of clear cell renal cell carcinoma. Biochim. Biophys. Acta Rev. Cancer 1870, 23–31. https://doi.org/10.1016/j.bbcan.2018.06.003 (2018).
Büscheck, F. et al. Prevalence and clinical significance of VHL mutations and 3p25 deletions in renal tumor subtypes. Oncotarget 11, 237–249. https://doi.org/10.18632/oncotarget.27428 (2020).
Fan, D. et al. Prognostic significance of PI3K/AKT/ mTOR signaling pathway members in clear cell renal cell carcinoma. PeerJ 8, e9261–e9261. https://doi.org/10.7717/peerj.9261 (2020).
Guo, H. et al. The PI3K/AKT pathway and renal cell carcinoma. J. Genet. Genom. 42, 343–353. https://doi.org/10.1016/j.jgg.2015.03.003 (2015).
Makhov, P. et al. Resistance to systemic therapies in clear cell renal cell carcinoma: Mechanisms and management strategies. Mol. Cancer Ther. 17, 1355–1364. https://doi.org/10.1158/1535-7163.Mct-17-1299 (2018).
Manley, B. J. et al. Integration of recurrent somatic mutations with clinical outcomes: A pooled analysis of 1049 patients with clear cell renal cell carcinoma. Eur. Urol. Focus 3, 421–427. https://doi.org/10.1016/j.euf.2016.06.015 (2017).
Hakimi, A. A. et al. Impact of recurrent copy number alterations and cancer gene mutations on the predictive accuracy of prognostic models in clear cell renal cell carcinoma. J. Urol. 192, 24–29. https://doi.org/10.1016/j.juro.2014.01.088 (2014).
Hakimi, A. A. et al. Adverse outcomes in clear cell renal cell carcinoma with mutations of 3p21 epigenetic regulators BAP1 and SETD2: A report by MSKCC and the KIRC TCGA research network. Clin. Cancer Res. 19, 3259–3267. https://doi.org/10.1158/1078-0432.CCR-12-3886 (2013).
Hakimi, A. A. et al. Clinical and pathologic impact of select chromatin-modulating tumor suppressors in clear cell renal cell carcinoma. Eur. Urol. 63, 848–854. https://doi.org/10.1016/j.eururo.2012.09.005 (2013).
Patard, J. J. et al. Low CAIX expression and absence of VHL gene mutation are associated with tumor aggressiveness and poor survival of clear cell renal cell carcinoma. Int. J. Cancer 123, 395–400. https://doi.org/10.1002/ijc.23496 (2008).
Smits, K. M. et al. Genetic and epigenetic alterations in the von hippel-lindau gene: The influence on renal cancer prognosis. Clin. Cancer Res. 14, 782–787. https://doi.org/10.1158/1078-0432.CCR-07-1753 (2008).
Deckers, I. A. et al. Promoter CpG island methylation in ion transport mechanisms and associated dietary intakes jointly influence the risk of clear-cell renal cell cancer. Int. J. Epidemiol. 46, 622–631. https://doi.org/10.1093/ije/dyw266 (2017).
International Union Against Cancer (UICC). TNM Classification of Malignant Tumours, Third Edition, Revised Edition (ed. Harmer, M.) (Springer, 1982).
van Houwelingen, K. P. et al. Prevalence of von Hippel–Lindau gene mutations in sporadic renal cell carcinoma: Results from The Netherlands cohort study. BMC Cancer 5, 57. https://doi.org/10.1186/1471-2407-5-57 (2005).
Sato, Y. et al. Integrated molecular analysis of clear-cell renal cell carcinoma. Nat. Genet. 45, 860–867. https://doi.org/10.1038/ng.2699 (2013).
Turajlic, S. et al. Deterministic evolutionary trajectories influence primary tumor growth: TRACERx renal. Cell 173, 595-610 e511. https://doi.org/10.1016/j.cell.2018.03.043 (2018).
Gu, Y. F. et al. Modeling renal cell carcinoma in mice: Bap1 and Pbrm1 inactivation drive tumor grade. Cancer Discov. 7, 900–917. https://doi.org/10.1158/2159-8290.CD-17-0292 (2017).
Pena-Llopis, S. et al. BAP1 loss defines a new class of renal cell carcinoma. Nat. Genet. 44, 751–759. https://doi.org/10.1038/ng.2323 (2012).
Brauch, H. et al. VHL alterations in human clear cell renal cell carcinoma: Association with advanced tumor stage and a novel hot spot mutation. Cancer Res. 60, 1942–1948 (2000).
Schraml, P. et al. VHL mutations and their correlation with tumour cell proliferation, microvessel density, and patient prognosis in clear cell renal cell carcinoma. J. Pathol. 196, 186–193. https://doi.org/10.1002/path.1034 (2002).
Ficarra, V. et al. Prognostic value of renal cell carcinoma nuclear grading: Multivariate analysis of 333 cases. Urol. Int. 67, 130–134 (2001).
Fuhrman, S. A., Lasky, L. C. & Limas, C. Prognostic significance of morphologic parameters in renal cell carcinoma. Am. J. Surg. Pathol. 6, 655–663 (1982).
Patard, J. J. et al. Absence of VHL gene alteration and high VEGF expression are associated with tumour aggressiveness and poor survival of renal-cell carcinoma. Br. J. Cancer 101, 1417–1424. https://doi.org/10.1038/sj.bjc.6605298 (2009).
Banks, R. E. et al. Genetic and epigenetic analysis of von Hippel-Lindau (VHL) gene alterations and relationship with clinical variables in sporadic renal cancer. Can. Res. 66, 2000–2011. https://doi.org/10.1158/0008-5472.Can-05-3074 (2006).
Kiemeney, L. A., Verbeek, A. L. & van Houwelingen, J. C. Prognostic assessment from studies with non-randomized treatment assignment. J. Clin. Epidemiol. 47, 241–247. https://doi.org/10.1016/0895-4356(94)90005-1 (1994).
Voss, M. H. et al. Genomically annotated risk model for advanced renal-cell carcinoma: A retrospective cohort study. Lancet Oncol. 19, 1688–1698. https://doi.org/10.1016/S1470-2045(18)30648-X (2018).
D’Avella, C., Abbosh, P., Pal, S. K. & Geynisman, D. M. Mutations in renal cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 38, 763–773. https://doi.org/10.1016/j.urolonc.2018.10.027 (2020).
van den Brandt, P. A. et al. A large-scale prospective cohort study on diet and cancer in The Netherlands. J. Clin. Epidemiol. 43, 285–295 (1990).
Goldbohm, R. A. Estimation of the coverage of dutch municipalities by cancer registries and PALGA based on hospital discharge data. Tijdschr. Soc. Gezondh. 72, 80–84 (1994).
World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310, 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013).
Ferronika, P. et al. Comprehensive profiling of primary and metastatic ccRCC reveals a high homology of the metastases to a subregion of the primary tumour. Cancers (Basel) https://doi.org/10.3390/cancers11060812 (2019).
Ferronika, P. et al. Mutational heterogeneity between different regional tumour grades of clear cell renal cell carcinoma. Exp. Mol. Pathol. 115, 104431. https://doi.org/10.1016/j.yexmp.2020.104431 (2020).
Garrison, E. & Gabor, M. Haplotype-based variant detection from short-read sequencing. arXiv preprint arXiv 2012, 1207.3907.
McKenna, A. et al. The Genome Analysis Toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303. https://doi.org/10.1101/gr.107524.110 (2010).
Robinson, J. T. et al. Integrative genomics viewer. Nat. Biotechnol. 29, 24–26. https://doi.org/10.1038/nbt.1754 (2011).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B (Methodological) 57, 289–300 (1995).
McDonald, J. H. Handbook of Biological Statistics, 3rd ed. (Sparky House Publishing, 2014).
Schoenfeld, D. A. Sample-size formula for the proportional-hazards regression model. Biometrics 39, 499–503 (1983).
Acknowledgements
We are indebted to the participants of this study and wish to thank the Netherlands Cancer Registry (IKNL) and the Netherlands Pathology Registry (PALGA). We are grateful to Dr. C. Hulsbergen-van de Kaa and Dr. M. Baldewijns for revising the tumour histology. We also thank the staff of the Netherlands Cohort Study for their valuable contributions. Furthermore, we thank Dr. E. Birnie for his advice on the statistical data analysis and K. McIntyre for editing our manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.E., L.S. and K.K.; formal analysis, J.P. and P.F.; methodology, J.P., P.F., L.S. and K.K.; supervision, L.S. and K.K.; visualization, J.P.; writing—original draft, J.P., P.F., L.S. and K.K.; writing—review & editing, H.W., M.E., M.T., K.S., K.L., P.B. and R.S. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van de Pol, J.A.A., Ferronika, P., Westers, H. et al. Evaluation of a seven gene mutational profile as a prognostic factor in a population-based study of clear cell renal cell carcinoma. Sci Rep 12, 6478 (2022). https://doi.org/10.1038/s41598-022-10455-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10455-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.