Abstract
Insufficient evidence is available comparing mortality and cause of death between general hypertrophic cardiomyopathy (HCM) and general non-HCM populations. We aimed to investigate how causes of death and mortality differ in subjects with and without HCM. Using the National Health Insurance Service database from 2009 to 2016, individuals who underwent health check-up(s) with or without a history of HCM were identified. Participants in the HCM group were matched at a 1:1 ratio with those in the non-HCM group using propensity scores calculated from the baseline covariates. Mortality rates and risks were compared between the groups. In total, 14,858 participants (7,429 each in the HCM and non-HCM groups) were followed up over a mean 4.4 ± 2.2 years (mean age, 61.0 years; male proportion, 66.8%). Compared to the non-HCM group, the HCM group showed a higher risk of all-cause and HCM-related mortality and a similar risk for non-cardiovascular mortality (hazard ratio [95% confidence interval] 1.57 [1.38–1.78], 2.71 [1.92–3.83], and 1.04 [0.88–1.23], respectively). The sensitivity analyses consistently showed that the HCM group showed higher risks of all-cause and HCM-related mortality than the non-HCM group. The female participants with HCM were associated with an increasing trend of the risks of all-cause mortality but not HCM-related mortality compared to their male counterparts (p for interaction < 0.001 and 0.185, respectively). In conclusion, compared to the non-HCM population, the general HCM population showed higher risks of both all-cause and HCM-related mortality, but had a similar risk of non-cardiovascular mortality.
Similar content being viewed by others
Introduction
Hypertrophic cardiomyopathy (HCM) is a common inherited cardiomyopathy that can clinically manifest with sudden cardiac death, heart failure, stroke, and arrhythmia1. Compared to the general population, patients with HCM were traditionally recognised as having a higher cardiovascular mortality rate2. However, the prognosis of HCM has improved significantly because of the recent advances in disease management, risk stratification, and family screening3. Additionally, a previous study reported that the life expectancy of patients with HCM might not be significantly different from that of the general population4. Therefore, it is necessary to update how the prognosis of HCM population differs from that of the non-HCM population in this contemporary management era. Currently, only a few studies are available that directly compared mortality between HCM and non-HCM populations5,6,7. Besides, a few earlier studies included patients with HCM who had a considerable burden of comorbidities, including hypertension and heart failure8,9. Thus, it remains unclear whether the impact of HCM on mortality is innate or secondary to other comorbidities. In addition, previous studies mostly investigated ‘referral’ patients with HCM5,7, so they are inevitably susceptible to selection bias, as this population is likely to have an increased proportion of high-risk patients, making it challenging to represent the general HCM population10. Therefore, this study was designed to compare the cause of death and mortality between the general HCM and non-HCM populations using propensity score matching of a nationwide cohort.
Methods
Ethical statement and data availability
This study conforms to the ethical guidelines of the Declaration of Helsinki revised in 2013 and was approved by the institutional review board of our institution (Seoul National University Hospital Institutional Review Board, No. 1905-106-1035). The need for informed consent was waived by the Seoul National University Hospital Institutional Review Board because the study used anonymised data. All raw data are accessible from the designated terminals approved by the National Health Insurance Service (NHIS).
Data source
This nationwide cohort study used the NHIS database of Korea. A summary of the database was previously reported11. In brief, the NHIS is the single public insurer that covers the entire Korean population and encourages any eligible Korean adult to receive general health check-ups provided by the NHIS biannually. Therefore, the NHIS database includes individual demographic information, history of diagnoses, and results of health check-ups. Additionally, we obtained the mortality data from Statistics Korea12, a government agency that provides causes of death for the entire Korean population based on the diagnostic codes on death certificates. Individuals’ history of diagnoses and causes of death are all coded according to the International Classification of Disease, Tenth Revision, Clinical Modification.
Study design
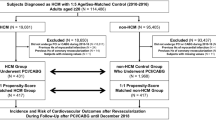
From 2009 to 2016, the NHIS database identified all individuals with HCM (n = 19,372) who were initial candidates for the HCM group. Individuals were excluded if they were younger than 20 years of age (n = 284), had no health check-ups within 2 years from the diagnosis of HCM (n = 9689), or had missing data for the study variables (n = 130). For the non-HCM group, we identified individuals without any history of HCM diagnosis from the same database. Then the two groups were matched at a 1:1 ratio using propensity scores calculated from the baseline covariates, resulting in 7429 participants for each group (Fig. 1). After propensity scoring matching, the two groups were well balanced (Fig. S1). Every participant was followed up from the date of the baseline health check-up until 31 December 2017. The primary outcome was set as all-cause mortality.
Definition of hypertrophic cardiomyopathy diagnosis and causes of death
In this study, HCM was confirmed when there were both the claims for diagnostic codes I42.1 or I42.2 at either admission or outpatient clinic visit and the registration of the Rare Intractable Diseases program (RID) for HCM12,13. RID is a policy implemented by the Ministry of Health and Welfare to expand medical insurance for rare diseases. For this reason, accurate test results and expert opinions are required to register patients with HCM into the RID. Because third-party experts review medical data during RID registration, patients with HCM registered with RID were reliable. Causes of death were categorised into three groups: HCM-related (including arterial thromboembolism, atrial fibrillation, sudden cardiac death, cerebrovascular disease, heart failure, and ventricular arrhythmia), other cardiovascular (including hypertensive disease, ischemic heart disease, and peripheral vascular disease), and non-cardiovascular causes (including all causes of death except I-codes). Detailed information or definitions are described in more detail in Table S1.
Study covariates
For each study participant, all study covariates were measured on the visit day for a health check-up. The covariates included age, sex, and physical measurements (height, body weight, body mass index, waist circumference, and blood pressures). We obtained information on health habits (smoking status, alcohol consumption, and regular exercise) from the survey for the health check-up. The blood test results (lipid profiles, serum creatinine level, and estimated glomerular filtration rate) were also collected. We investigated each participant’s comorbidities by reviewing a history of claimed diagnostic codes from the NHIS database. Detailed descriptions of each covariate are presented in Table S1.
Statistical analyses
In propensity score matching, a covariate was considered balanced between the groups if its absolute standardised difference (ASD) was < 0.1. For each category of causes of death, a survival analysis was performed using the Kaplan–Meier method. Mortality rates were calculated in 1,000 person-year. A log-rank test was used to evaluate the difference in survival between the groups. Subgroup analyses were performed for age strata (< 60 and ≥ 60 years) and sex.
Two sensitivity analyses were performed to support the main results (Fig. S2). The first sensitivity analysis used the 1:1 age- (exact) and sex-matched non-HCM population. Multivariate Cox proportional hazard regression analysis was used to estimate the mortality risks, and the data are presented as adjusted hazard ratios (HRs) with 95% confidence intervals (CIs). The second sensitivity analysis was performed to investigate the mortality of participants with HCM without significant coronary artery disease (i.e. having both ischaemic heart disease [IHD] and a history of percutaneous coronary intervention [PCI]). The HCM population without significant coronary artery disease was matched at a 1:1 ratio with the non-HCM population using the propensity scores. In this case, non-HCM individuals with significant coronary artery disease were also excluded from the non-HCM group. We performed falsification analyses to evaluate whether there was a significant selection bias between the groups. Falsification outcomes included herniated intervertebral disc (M51), sinusitis (H65-67), urinary incontinence (F980, N393, N394, and R32), and cataract (H25, H26, H28, and Q120).
For all analyses, p-values < 0.05 rejected the null hypothesis. SAS version 9.3 (SAS Institute, Cary, NC, USA) was used to perform all statistical analyses.
Declaration of Helsinki
This study conforms to the ethical guidelines of the Declaration of Helsinki revised in 2013.
Results
In total, 14,858 participants (7,429 each in the HCM and non-HCM groups) were included in the final analysis. The distribution of the two groups’ propensity scores was equalised after the matching process (Fig. S1). Additionally, after the matching process, all covariates were well balanced between the groups without statistical difference (ASD < 0.1 for each covariate). Baseline characteristics of the study population are presented in Table 1. Participants’ mean age was 61.0 years, and the proportion of men was 66.8% (n = 9,929). The most common comorbidity was hypertension (53.5%), and the mean systolic blood pressure was 127.5 ± 15.9 mmHg. The proportions of atrial fibrillation, IHD with PCI, heart failure, and implantable cardioverter defibrillator (ICD) implantation were 7.1%, 2.0%, 11.5%, and 0.1%, respectively.
Mortality according to cause of death
Over a mean follow-up of 4.4 ± 2.2 years, 1,011 (6.8%) cases of all-cause mortality were observed. Compared to the non-HCM group, the HCM group had significantly higher all-cause (8.3% versus 5.3%, p < 0.001), HCM-related (1.6% versus 0.6%, p < 0.001), and other cardiovascular mortalities (0.8% versus 0.5%, p = 0.006) (Table 2). Non-cardiovascular mortality was not significantly different between the two groups (p = 0.600). Regarding major causes of cardiovascular-related mortality, the HCM group had significantly higher mortality due to cerebrovascular disease (0.9% versus 0.3%, p < 0.001), IHD (0.7% versus 0.4%, p = 0.032), heart failure (0.3% versus 0.1%, p = 0.034), and atrial fibrillation (0.2% versus < 0.1%, p < 0.001) than the non-HCM group (Table 2). Mortality due to sudden cardiac death and ventricular arrhythmia was not significantly different between the two groups (p = 0.133 and 0.655, respectively), possibly due to low incidences of both events.
Mortality rates and risks according to cause of death
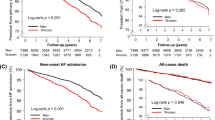
The cumulative incidence of mortality was significantly different between the two groups except for non-cardiovascular causes (Fig. 2). Compared to the non-HCM group, the HCM group had significantly higher mortality rates due to all-cause (19.1 versus 12.1 per 1,000 person-years, p < 0.001), HCM-related causes (3.7 versus 1.4 per 1,000 person-years, p < 0.001), and other cardiovascular causes (1.9 versus 1.1 per 1,000 person-years, p < 0.007), and had no difference in non-cardiovascular causes (8.5 versus 8.2 per 1,000 person-years, p = 0.609) (Fig. 3). Also, the HCM group was significantly associated with higher risks of mortality except for non-cardiovascular mortality than those of the non-HCM group (HR [95% CI] 1.57 [1.38–1.78], 2.71 [1.92–3.83], 1.77 [1.17–2.67], and 1.04 [0.88–1.23] for all-cause, HCM-related, other cardiovascular, and non-cardiovascular mortality, respectively) (Fig. 3). Mortality rates and risks by specific disease categories are presented in Table S2. Among the disease categories, the HCM group was significantly associated with increased risks of (in the highest order of) atrial fibrillation, ischaemic stroke, cerebrovascular disease (including ischaemic stroke), heart failure, and IHD compared to the non-HCM group (HR [95% CI] 14.2 [1.87–108.04], 3.26 [1.60–6.62], 2.74 [1.73–4.33], 2.15 [1.02–4.54], and 1.64 [1.04–2.58], respectively). Mortality risks of other disease categories, including sudden cardiac death and ventricular arrhythmia, were not significantly different between the two groups.
Cumulative mortality according to the cause of death. All-cause mortality, HCM-related mortality, and other cardiovascular mortality were significantly higher in the HCM group compared with those in the non-HCM group. Mortality from non-cardiovascular causes, however, were not significantly different between the HCM and the non-HCM groups. HCM hypertrophic cardiomyopathy.
Mortality rates and risks according to the cause of death. Mortality rates, mortality risks with 95% CIs, and p-values are presented. Mortality rates were higher in the HCM group than in the non-HCM group, irrespective of the cause of death. Compared to the non-HCM group, the HCM group was associated with significantly higher risks for all-cause, HCM-related, and other cardiovascular mortality. Non-cardiovascular mortality was comparable in the HCM group versus the non-HCM group. HCM hypertrophic cardiomyopathy, CV cardiovascular, REF reference, PY person-year, HR hazard ratio, CI confidence interval.
Subgroup, sensitivity, and falsification analyses
Participants with HCM aged both < 60 and ≥ 60 years were associated with increased risks of all-cause, HCM-related causes, and other cardiovascular mortalities with the exception of non-cardiovascular mortality compared to their non-HCM counterparts (all-cause mortality: HR [95% CI] 2.16 [1.46–3.21] and 1.65 [1.45–1.89]; HCM-related mortality: 3.46 [1.16–10.37] and 2.91 [2.02–4.18]; other cardiovascular mortality: 5.33 [1.19–23.79] and 1.68 [1.08–2.61]; and non-cardiovascular mortality: 1.14 [0.67–1.95] and 1.13 [0.95–1.35], respectively). However, there were no significant interactions between the two groups for the subgroups of age strata (< 60 and ≥ 60 years) (Fig. 4).
We observed that female participants with HCM had a trend of higher risks of all-cause and other cardiovascular mortalities than male participants with HCM (all-cause mortality: HR [95% CI] 2.40 [1.93–3.00] versus 1.25 [1.07–1.46]; other cardiovascular mortality: 3.25 [1.53–6.92] versus 1.31 [0.79–2.17]), when the non-HCM counterparts served as the reference (p for interaction < 0.001 and 0.046, respectively). However, no significant difference was noted in the HCM-related mortality between male and female participants with HCM (HR [95% CI] 2.20 [1.39–3.48] versus 3.61 [2.13–6.12], p for interaction = 0.185) (Fig. 4).
Results of the sensitivity analyses using multivariate Cox regression analysis are presented in Tables S3 and S4. Compared to the age- and sex-matched non-HCM group, the HCM group had a higher burden of comorbidity (Table S3). The multivariate Cox regression analysis reproduced the primary results except for other cardiovascular mortality, which showed no significant difference between the two groups (Table S4). The sensitivity analysis excluding participants with significant coronary artery disease also reproduced the primary results except for other cardiovascular mortality (Table S5). The HCM group showed a marginal significance of an increased risk of PCI compared to the non-HCM group (HR [95% CI] 1.24 [1.00–1.55], p = 0.053) (Table S5). There were no significant differences in the risks of falsified outcomes between the two groups (Table S6).
Discussion
In the present study, after matching the two groups using propensity scores, we observed that the HCM group showed higher risks of all-cause, HCM-related, and other cardiovascular mortalities, but had a similar risk of non-cardiovascular mortality, compared to the non-HCM group. The current study has a few strengths. First, we investigated a nationwide cohort of adults with HCM, allowing for inclusion of both referral and non-referral individuals simultaneously. Second, we compared the HCM population to the non-HCM population matched by propensity scores calculated from 30 covariates. Third, we analysed the differences in mortality rates and risks between the two groups according to cause of death. Finally, sensitivity and falsification analyses were performed to support the main results.
Here, we observed that the most common mode of death in the HCM group was non-cardiovascular causes (Table 2), with cancer being the most common non-cardiovascular cause (Table S2). This result may be driven by extended longevity of individuals with HCM resulting from improved medical care1, and thus, more individuals with HCM should have more chances to be diagnosed with cancer than before. Among the major causes of cardiovascular-related death, the most common was cerebrovascular disease, followed by IHD, heart failure, and atrial fibrillation. Sudden cardiac death and ventricular arrhythmia accounted for only a minor portion of mortality. These findings appear to be different from those of previous studies5,14. Songsirisuk et al. reported the cause of death in ‘referral’ patients with HCM recruited from a single tertiary hospital in Thai14. Although this study investigated a small number of patients (n = 161), the HCM-related mortality rate was 2%/year. The common causes of death were heart failure, sudden cardiac death, and stroke. In particular, the incidence of sudden cardiac death was 1%/year, which was in clear contrast to our study finding (0.03%/year, Table S2). A possible explanation for the difference may be related to the characteristics of patients recruited; that is, the earlier study recruited referral patients from a single tertiary institution, possibly leading to a referral bias and a higher rate of sudden cardiac death due to a higher proportion of high-risk patients with HCM compared to our study. Lorenzini et al. compared 4893 patients with HCM to the general non-HCM population in Europe, and reported that patients with HCM carried a higher risk of all-cause death than the general population5. They found that sudden cardiac death tended to decrease with age, but it occurred in 3.4% of patients enrolled. The proportion of sudden cardiac death in our study (0.2%) was lower than that of the previous report, which can possibly be explained by the difference in the mean age of the study population (60.8 years in the present study versus 49.2 years in the earlier report)5. One earlier study also reported a lower incidence of sudden cardiac death events in two tertiary centre registries15, corroborating our study finding. The difference is again partly explained by the fact that Lorenzini et al.'s study also targeted ‘referral’ HCM patients, as in Songsirisuk et al.'s report14, while we targeted general individuals with HCM from a nationwide cohort5. Besides, phenotypic differences between Eastern and Western countries may partly modify the prognosis of HCM, although the HCM phenotype cannot be differentiated in our nationwide HCM cohort.
We observed that females with HCM had a higher risk of all-cause mortality than their male counterparts, as observed in previous studies5,16,17. Additionally, we found that other cardiovascular mortality was higher in women than in men, while there was no significant difference in HCM-related mortality between the sexes. A previous report also found that there was no difference in HCM-related mortality between the sexes owing to the advances in contemporary management18, although females with IHD are at a higher risk of mortality than their male counterparts19. Especially, post-menopausal women are associated with a higher risk of hypertension and its subsequent cardiovascular complications than men due to the loss of vasodilatory effects of endogenous oestrogen Regarding non-cardiovascular mortality, female participants with HCM had only a marginal significance of increased risks compared to their male counterparts (p for interaction = 0.054) (Fig. 4). Taken together, these results suggest that female subjects with HCM may be more vulnerable to other cardiovascular mortality that was composed of hypertensive disorders, IHD, and peripheral arterial disease, than their male counterparts.
The Cox regression analysis for the sensitivity analysis showed that there was no difference in other cardiovascular and non-cardiovascular mortalities between the HCM and non-HCM groups (Table S4). In another sensitivity analysis that was performed after excluding participants with IHD and PCI, we again found no difference in other cardiovascular and non-cardiovascular mortalities between the two groups (Table S5). Therefore, the general participants with HCM still mainly suffer from HCM-related causes of mortality even in the contemporary management era; therefore, health education regarding HCM is required for the general population. More active education, early detection/diagnosis, and close follow-up may be helpful to reduce HCM-related causes of mortality in the general HCM population. This issue needs to be re-evaluated in the future.
Of interest, we observed that the HCM group had a marginal significance of a higher risk of PCI compared to the non-HCM group (Table S5). This phenomenon cannot be explained by the differences in cardiovascular risk factors, such as obesity, hypertension, diabetes mellitus, and dyslipidaemia, because the HCM and non-HCM groups were carefully matched using propensity scores. The most plausible explanation is that the individuals with HCM may be more regularly and closely monitored in a dedicated centre, which may facilitate detection and treatment of significant coronary disease. Thanks to the improved contemporary management strategy, the longevity of individuals with HCM has been significantly extended1. Nevertheless, individuals with HCM intentionally reduce physical activity at work and leisure time after being diagnosed with HCM because of a concern for sudden cardiac death20. However, individuals with HCM are not immune from cardiovascular diseases, such as coronary disease. Given that elderly individuals with HCM have a relatively low risk of sudden cardiac death, maintaining good cardiovascular fitness through appropriate physical activity may be beneficial and improve prognosis12. However, only recently have individuals with HCM been advised to perform regular exercise at an appropriate level21. In this respect, the risk of coronary artery disease requiring PCI observed in the current study should be focused on, especially in elderly individuals with HCM.
Limitations
A few study limitations should be acknowledged. First, the validity of the HCM diagnosis needs to be checked. Defining the HCM population by using diagnostic codes may have falsely estimated the actual HCM population. However, we used both the diagnostic codes and RID codes to improve the diagnostic accuracy. Such a definition validated a reasonable diagnostic accuracy (sensitivity, 91.5%; specificity, 100%; and positive predictive value, 92.6%) in our previous study13. In addition, the NHIS database has been widely and reliably used for HCM research8,12,22,23,24,25,26. Second, this study cannot be completely free from selection bias of the study population. To investigate the baseline characteristics at the time of HCM diagnosis, we screened the individuals who had a health check-up within 2 years from the diagnosis. However, this process may have preferentially selected individuals who are more interested in their health status, leading to a reduction in the mortality rate. Third, the generalisation of our results to the younger HCM population is limited because our study analysed the HCM population with a mean age of 61 years. Fourth, the follow-up periods of the study population were relatively short (4.4 ± 2.2 years). Fifth, although our study used a representative HCM population in South Korea, it was impossible to differentiate patients who were treated in the HCM specialty center from those who were not. This information may give further insights on the special need of HCM specialty center. Sixth, the study results might be partly influenced by survivorship bias. We excluded the HCM population aged less than 20 years, and the mean age of the study population is about 61 years. Thus, the resultant study population could be survivors from sudden cardiac death or those with a low risk for sudden cardiac death. This may explain a low sudden cardiac death rate observed in our study. However, Asian HCM population was reported to have a lower sudden cardiac death rate, even for the referral patients to the HCM specialty center15. Also, our study includes both referred and non-referred populations, and non-referred HCM patients were reported to have lower mortality10. Seventh, this study did not comprehensively investigate drug uses, and the difference in the uses of beta-blockers or calcium channel blockers may convey a bias in the study results. Eighth, the database we used in the current study do not allow for evaluating genetic testing results or echocardiography-based left ventricular outflow tract obstruction. Finally, it is difficult to infer any causality related to our results because the study was retrospective in nature.
Conclusions
This nationwide cohort study compared mortality and cause of death between the general HCM and general non-HCM matched populations. Among the major causes of cardiovascular-related mortality, cerebrovascular disease, IHD, heart failure, and atrial fibrillation were significantly more frequent in the HCM population than in the non-HCM population. Multiple statistical analyses consistently showed that compared to the non-HCM population, the HCM population had significantly higher risks of all-cause and HCM-related mortality. Our results suggest that such an increased mortality risk be an innate feature of HCM, independent of other concomitant comorbidities. Appropriate HCM-specialised medical care and surveillance may aid in further improvement in the prognosis of individuals with HCM in the modern era.
Data availability
The data is available from the Korean National Health Insurance Sharing Service (NHISS; https://nhiss.nhis.or.kr/) database which is open to researchers on request with approval by the Insitutional Review Board.
References
Maron, B. J. Clinical course and management of hypertrophic cardiomyopathy. N. Engl. J. Med. 379(7), 655–668 (2018).
Elliott, P. M. et al. Historical trends in reported survival rates in patients with hypertrophic cardiomyopathy. Heart 92(6), 785–791 (2006).
Maron, B. J., Maron, M. S. & Rowin, E. J. Perspectives on the overall risks of living with hypertrophic cardiomyopathy. Circulation 135(24), 2317–2319 (2017).
Maron, B. J. et al. Hypertrophic cardiomyopathy in adulthood associated with low cardiovascular mortality with contemporary management strategies. J. Am. Coll. Cardiol. 65(18), 1915–1928 (2015).
Lorenzini, M. et al. Mortality among referral patients with hypertrophic cardiomyopathy vs the general European population. JAMA Cardiol. 5(1), 73–80 (2020).
Pujades-Rodriguez, M. et al. Identifying unmet clinical need in hypertrophic cardiomyopathy using national electronic health records. PLoS ONE 13(1), e0191214 (2018).
Maron, B. J. et al. Risk stratification and outcome of patients with hypertrophic cardiomyopathy ≥ 60 years of age. Circulation 127(5), 585–593 (2013).
Moon, I. et al. Trends of the prevalence and incidence of hypertrophic cardiomyopathy in Korea: A nationwide population-based cohort study. PLoS ONE 15(1), e0227012 (2020).
Husser, D. et al. Prevalence of clinically apparent hypertrophic cardiomyopathy in Germany-An analysis of over 5 million patients. PLoS ONE 13(5), e0196612 (2018).
Maron, B. J. et al. Epidemiology of hypertrophic cardiomyopathy-related death: Revisited in a large non-referral-based patient population. Circulation 102(8), 858–864 (2000).
Choi, E. K. Cardiovascular research using the Korean National Health Information Database. Korean Circ. J. 50(9), 754–772 (2020).
Kwon, S., Lee, H.J., Han, K.D., et al. Association of physical activity with all-cause and cardiovascular mortality in 7666 adults with hypertrophic cardiomyopathy (HCM): More physical activity is better. Br. J. Sports Med. 55(18), 1034–1040.(2021).
Choi, Y. J. et al. Temporal trends of the prevalence and incidence of atrial fibrillation and stroke among Asian patients with hypertrophic cardiomyopathy: A nationwide population-based study. Int. J. Cardiol. 273, 130–135 (2018).
Songsirisuk, N. et al. Modes of death and clinical outcomes in adult patients with hypertrophic cardiomyopathy in Thailand. BMC Cardiovasc. Disord. 19(1), 1 (2019).
Choi, Y. J. et al. Validation of the hypertrophic cardiomyopathy risk-sudden cardiac death calculator in Asians. Heart 105(24), 1892–1897 (2019).
Geske, J. B. et al. Women with hypertrophic cardiomyopathy have worse survival. Eur. Heart J. 38(46), 3434–3440 (2017).
Wang, Y. et al. Female sex is associated with worse prognosis in patients with hypertrophic cardiomyopathy in China. PLoS ONE 9(7), e102969 (2014).
Rowin, E. J. et al. Impact of sex on clinical course and survival in the contemporary treatment era for hypertrophic cardiomyopathy. J. Am. Heart Assoc. 8(21), e012041 (2019).
Majidi, M., Eslami, V., Ghorbani, P. & Foroughi, M. Are women more susceptible to ischemic heart disease compared to men? A literature overview. J. Geriatr. Cardiol. 18(4), 289–296 (2021).
Reineck, E. et al. Physical activity and other health behaviors in adults with hypertrophic cardiomyopathy. Am. J. Cardiol. 111(7), 1034–1039 (2013).
Ommen, S. R. et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 76(25), e159–e240 (2020).
Park, J. B. et al. Obesity and metabolic health status are determinants for the clinical expression of hypertrophic cardiomyopathy. Eur. J. Prev. Cardiol. 27(17), 1849–1857 (2020).
Lee, H. J. et al. Novel oral anticoagulants for primary stroke prevention in hypertrophic cardiomyopathy patients with atrial fibrillation. Stroke 50(9), 2582–2586 (2019).
Lee, H. et al. Risk of end-stage renal disease in patients with hypertrophic cardiomyopathy: A nationwide population-based cohort study. Sci. Rep. 9(1), 14565 (2019).
Kim, M. et al. Sex differences in the prognosis of patients with hypertrophic cardiomyopathy. Sci. Rep. 11(1), 4854 (2021).
Lee, H. J. et al. Clinical impact of atrial fibrillation in a nationwide cohort of hypertrophic cardiomyopathy patients. Ann. Transl. Med. 8(21), 1386 (2020).
Funding
None.
Author information
Authors and Affiliations
Contributions
S.K.: conceptualization, methodology, software, validation, formal analysis, investigation, resources, data curation, writing—original draft, writing—review & editing, visualization. H.K.K.: conceptualization, methodology, formal analysis, investigation, resources, data curation, writing—review & editing, supervision, project administration, funding acquisition. B.K.: methodology, software, validation, formal analysis, investigation, resources, data curation. H.J.L.: conceptualization, writing—review & editing, supervision. K.D.H.: methodology, software, validation, formal analysis, investigation, resources, data curation, supervision, project administration. I.C.H., Y.E.Y., S.P.L., G.Y.C., Y.J.K.: conceptualization, writing—review & editing, supervision. J.B.P., H.L.: methodology, conceptualization, writing—review & editing, supervision.
Corresponding author
Ethics declarations
Competing interests
H.K.K reports research grants from Johnson & Johnson, Handok Pharm, GSK, Dae-Woong Pharm, Yuhan, Hanmi, ChongKunDang Pharm, Boryung Pharm, and JW Pharm. The remaining authors have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kwon, S., Kim, HK., Kim, B. et al. Comparison of mortality and cause of death between adults with and without hypertrophic cardiomyopathy. Sci Rep 12, 6386 (2022). https://doi.org/10.1038/s41598-022-10389-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10389-4
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.