Abstract
Previous studies showed positive associations between specific types of social capital and child nutritional status. Our study examined whether improved food availability mediates the impact of maternal and child social support on child nutritional status in four low- and middle-income countries. We used data from the Young Lives cohort study, comprising 1,000 children aged 8 and 12 in Vietnam and Ethiopia, 1008 in India, and 714 in Peru. The outcome variables were the z-scores for height for age and body mass index (HAZ and BAZ, respectively). The causal mediation analysis framework was used. In Peru, above-median values of maternal social support and receiving child financial support were positively associated with HAZ at age 12. The level of maternal financial support was positively associated with BAZ among 12-year-old children in India. Peru was the only country where a positive association was found between food availability and maternal financial support among children aged 12. However, food availability did not mediate the effect of maternal financial support on HAZ at age 12. Strengthening social support to improve child nutritional status, especially by improving food availability, may not be a sufficient intervention in resource-poor settings because sources of support may lack sufficient food resources to share. However, more comprehensive measurements of social support and food security are necessary to better understand the mechanism of social support and child nutritional status.
Similar content being viewed by others
Introduction
Poor nutritional status in childhood has been linked to an elevated risk of mortality and morbidity later in life1. Not only does impaired physical growth hamper child development (defined as the attainment of gross motor and fine motor skills), psychosocial competencies, and cognitive abilities2,3, it also raises the risk of contracting infectious diseases4. However, the worldwide prevalence of child malnutrition, including stunting, underweight, and wasting, remains persistently high and is concentrated in low- and middle-income countries (LMICs). In 2020, stunting affected 32.3% and 32.5% of children aged 0–59 months in Eastern/Southern and West/Central Africa, respectively. The prevalence of stunting in East Asia (13.5%) and Middle/North Africa (15.6%) was far lower, but it was still three to four times greater than that in North America (3.2%)5. These findings highlight the importance of accelerating efforts to close this geographical gap in stunting.
According to the United Nations Children’s Fund report “Improving Child Nutrition,” household food insecurity is an important factor for child undernutrition, which is in turn affected by socioeconomic conditions and the national/global context6. Food insecurity leads to inadequate dietary intake, which directly affects height and weight and exerts indirect effects by promoting disease occurrence. This was empirically demonstrated by Humphries (2015), who established that children from chronically food-insecure households in Ethiopia, India, Peru, and Vietnam had significantly lower height for age Z-score (HAZ) values than children from households that were consistently food-secure7.
Social capital, defined as the resources embedded within social networks8, has been demonstrated to positively affect health. Social capital can be analyzed as an individual attribute (e.g., as an individual’s access to social support within a network) or as a collective property collective, (e.g., norms of mutual assistance within a group)9,10. Although social capital has long been discussed in the social sciences, the emergence of social capital as a concept of interest in research on health is relatively recent11. Several studies have found positive associations between maternal or household social capital and child nutritional status12,13,14,15. However, it is difficult to reach any definite conclusion because the characteristics of the sample and measures of social capital have varied from study to study, and the results have been mixed12,13,14,15.
Studies that found positive associations between social capital and child nutritional status suggested that increased food security may be the mechanism, whereby individuals share food resources within their network or gain access to knowledge of where to obtain cheap sources of food. A handful of studies have demonstrated associations between social capital and household hunger or food security. Martin et al. (2004) found a significant association between increased household- and community-level social capital and decreased household experience of hunger in the United States (US)16. Similarly, low community- and family-level social capital was associated with higher odds of reporting food insecurity among the elderly in the US17. However, most of these studies were conducted in high-income countries (HICs), where food availability is generally relatively high, and therefore, there are abundant sources of support from which food-insecure households can borrow food or receive food assistance. Only one study was conducted in the LMIC setting, and it found a positive association between social capital and food security in six sub-counties of Uganda, three of which participated in a food aid program18. Given the significant gap in economic and public health resources between the two settings, it is difficult to generalize the findings from HICs to LMICs19. Furthermore, no previous studies examined the mediating role of food security in the effect of social capital on child nutritional status.
The results of prior studies underscore the need to assess the role of food security or food availability in the association between social capital and child nutritional status in LMICs. Although school-age children are old enough to develop their own social networks or to participate in groups while they are still in a growth phase, no studies have evaluated the association between child’s social support and their nutritional status. Unfortunately, the Young Lives (YL) study we utilized does not have enough information to address the comprehensive concept of food security but has information on food availability. Thus, our study aimed to examine 1) whether maternal and child social support is associated with child nutritional status using two indicators: HAZ and body mass index (BMI)-for-age z-score (BAZ); and 2) whether these associations are mediated by food availability.
Methods
Study design
For this secondary analysis, data were obtained from the older cohort of the YL study, a longitudinal cohort survey performed in Ethiopia, India, Peru, and Vietnam20. The older cohort of the YL study originally comprised 1,000 children in Vietnam and Ethiopia, 1,008 in India, and 714 in Peru aged 8 years when recruited in 2002 (wave 1). Subsequent data were collected at the ages of 12 years in 2006 (wave 2), 15 years in 2009 (wave 3), 19 years in 2013 (wave 4), and finally 22 years in 2016 (wave 5). For our study, wave 1 and wave 2 were used. The YL survey for the older cohort consists of three sets of questionnaires that examine information on households, children, and communities and were administered in interviews with primary caregivers, children, and community key informants, respectively.
The YL survey employed a clustered multistage sampling strategy in each country. At the first stage, 20 sentinel sites were selected in each country by semi-purposive sampling with a slight oversampling of poor sites to serve the main study objective to explore the causes and consequences of childhood poverty20. For example, the most food-deficient areas encompassed the sampling universe in Ethiopia. In Peru, the richest 5% of districts were excluded from the sample. However, the final samples represent a wide range of regions, policy contexts, and living conditions7. The cohort in India consisted of households only from Andhra Pradesh state, while the cohorts in the other three countries were nationwide. At the second stage, all households with children of the right age within the sites were listed, from which 100 households were randomly selected at each site (Figure S1)21.
The response rate was above 90% in all countries. Data were collected from the child’s main caregiver by a standardized, interviewer-administered questionnaire. The data for our analysis were extracted from waves 1 and 2 and limited to the biological mother.
Study indicators
Child anthropometry
Child nutritional status was captured using anthropometric indicators for child height and BMI, which are affected by chronic and acute nutritional status, respectively22. In the YL survey, anthropometric indicators were measured by adequately trained staff members who utilized techniques according to the World Health Organization (WHO) guidelines7,23,24. Height was measured using stadiometers with standing plates and moveable headboards, which were locally made, and weight was measured by a calibrated digital balance (Soehnle)7. The HAZ and BAZ were calculated using the WHO 2007 standard25. Extreme z-scores deemed biologically implausible (< − 6 and > 6 for HAZ, and < − 5 and > 5 for BAZ) were dropped according to the WHO recommendation26.
Household food availability
Due to the lack of information available for constructing food security, we utilized information on food availability from the household dataset. Food availability was asked differently in waves 1 and 2. In wave 1, respondents were asked whether the household had gotten enough food to eat, while in wave 2, they were asked whether the household had experienced any food shortage in the last 12 months. Responses of “yes” in wave 1 and “no” in wave 2 were coded as 1, indicating that food was available in the household.
Social support
Different questions were used to capture social support across waves. In wave 1, only maternal social support was measured, while the survey used in wave 2 measured both maternal and child social support. Information on maternal and child social support was obtained from the household and child surveys, respectively. The Short Social Capital Assessment Tool (SASCAT) was used to measure maternal social capital in wave 1; the SASCAT is a shortened version of the Adapted Social Capital Tool (A-SCAT) that includes three aspects of structural social capital: membership of groups, involvement in citizenship activities, and social support. The SASCAT was validated in Vietnam and Peru27,28, and has been widely used in many LMICs14,29. We only utilized the social support items for our study. Support received from groups in which the mother participated (support from groups) as well as social support received from different types of individuals (support from individuals) were combined into an index of maternal social support. For support from groups, when respondents answered that they were members of any of seven different kinds of groups (trade unions, community association/co-ops, women’s groups, political groups, religious groups, credit/funeral groups, and sports groups), they were subsequently asked whether they had received any support from that group. For support from individuals, participants were asked whether they had received support from any of nine different types of individuals (e.g., family, neighbors, friends, and so on). A composite score of maternal social support was calculated by averaging the number of “yes” responses, resulting in a score ranging from 0 to 1 that was analyzed as a continuous variable. We also examined maternal support as a categorical variable using a median split (due to high skewness). In wave 2, only financial support, which is one type of tangible (or instrumental) social support, was examined for the mother, while overall social support was examined for the child. Specifically, mothers were asked how many people they could rely on in times of financial need, with seven response options (none, 1, 2, 3 ~ 5, 6 ~ 10, 11 ~ 15, 16 ~ 20, 12 ~ 30, and > 30). Responses were dichotomized into no (none) versus yes (all others). Children were asked whether there was someone who could help in six different types of situations (detailed questions were described in Table S1). The overall level of child support was calculated by averaging positive responses, resulting in a range of 0 ~ 1, which were also dichotomized using a median split. We additionally examined financial support for the child based on the question asking whether the child had someone who could help when they needed pocket money (Table S1).
Covariates
Child characteristics included gender (female vs. male), birth order (second, third, and fourth or higher vs. first), and child’s working status (yes vs. no). Information on child working status was derived from a question asking whether the child was involved in any work activities such as farm work or domestic chores. Maternal characteristics included age in 5-year bands (≥ 30 and < 35, ≥ 35 and < 40, and ≥ 40 vs. < 30), education level (completed vs. not completed primary school), and marital status (permanent partner vs. divorced, separated, single, or widowed). Household characteristics included household size (5 or 6, and > 6 vs. ≦4), residential location (rural vs. urban), and wealth quintiles (second, third, fourth and fifth vs. first). The wealth quintile was based on a wealth index ranging from 0 to 1, which was calculated by averaging three variables: housing quality, ownership of consumer durables, and access to services30.
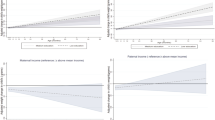
Statistical analyses
First, we reported descriptive statistics on the characteristics of the analytic sample and calculated the average HAZ and BAZ by each covariate (Table S2). We also presented the distribution of maternal and social support and the average HAZ and BAZ by the level of maternal and child social support for each of the four countries (Fig. 2). Next, the associations between the level of maternal or child social support and the child’s HAZ and BAZ at ages 8 and 12 were assessed using multivariable linear regression models. We introduced a community cluster effect (\(\varepsilon_{1, } \varepsilon_{2,} , \;{\text{and}}\;\varepsilon_{3}\)) to the model using the “cluster” option in the STATA package. The model can be specified as follows:
where X1 includes control variables except for food availability, and \(\varepsilon_{1 }\) is a community-level random effect.
To explore the mediating effect of food availability in the association between social support and child’s HAZ and BAZ, we fit a mediation model. We examined whether maternal or child social support, which showed a significant association with HAZ or BAZ in Eq. (1), is associated with the probability of food availability in the household, using the following reduced-form specification.
where \({\text{X}}_{2}\) includes control variables that showed strong associations with food availability (household size, mother’s education, and wealth level). For mediation to be present, \(\beta\) in Eq. (2) needs to be significantly different from 0. Finally, we introduced the food availability variable in Eq. (1).
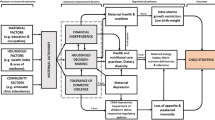
To demonstrate the presence of mediation, δ in (3) needs to be significantly different from 0 and \(\gamma^{\prime }\) in (3) must be either 0 or less than \(\gamma\) in (1) in absolute value. The relationships described above can be visualized in terms of the mediation model proposed by Baron and Kenny (Fig. 1)31.
However, this process does not fit well for non-linear mediators. Further, it is difficult to make a causal interpretation due to potential omitted variable bias. To address these issues, we used the potential outcome framework introduced by Imai et al. (2010), which uses counterfactuals to identify a causal effect and decomposes the total effect of a variable into direct and indirect (i.e., mediational) effects32,33. In the model of Imai et al., the total effect is γ in Eq. (1), which corresponds to the total effect of social support on HAZ or BAZ (without the food availability effect). The average direct effect is the mean difference between two counterfactual states of initial conditions, assuming no change in the mediator (\(\gamma^{\prime }\) in Eq. (3)), which is a direct effect of social support on HAZ or BAZ after taking into account the mediation (indirect) effect of food availability. Finally, the average causal mediation effects (ACME) is defined as the mean difference in effect between two counterfactual states of a mediator, assuming no change in the initial condition (total effect subtracted by direct effect: \(\gamma - \gamma^{\prime }\), which equals the product of \(\beta\) in Eq. (2) and δ in Eq. (3)). The mediation analysis was performed using the user-written code -medeff– in STATA 1434,35,36. Analyses were performed separately by wave (age 8 and age 12) and country.
Results
Our results were based on complete case analyses of 944, 813, 927, and 634 observations (mother—child dyads) in Vietnam, Ethiopia, India, and Peru respectively (Table S2). The proportion of missing values was less than 10%, except in Ethiopia (with 14.0% missing values in wave 1). However, the composition of the analytic and missing samples was assumed to be tolerably similar, such that the missing data did not lead to bias in our results (Table S3). The pattern of social support significantly differed between settings (Fig. 2). The average score of maternal social support was highest in Vietnam (0.15 in the lower 50% and 0.31 in the upper 50% group) and the lowest in Peru (0.03 in the lower 50% and 0.17 in the upper 50% group). In India, 91.5% of children responded that they had someone to help in all six situations. The relationship between the levels of maternal and child social support and the average HAZ and BAZ was not consistent across the countries.
Table S2 shows the descriptive statistics of the study samples in wave 1 from Vietnam, Ethiopia, India, and Peru, as well as the mean HAZ and BAZ for each category (the characteristics of study samples in wave 2 hardly changed from wave 1 because the YL study is a cohort survey). Generally, children with higher HAZ/BAZ were more likely to be from households with fewer household members, wealthier households, and households in an urban area. The average BAZ for the entire sample was remarkably high in Peru compared to other countries in both waves.
The results for the associations between maternal and child social support and HAZ in waves 1 and 2 without adjusting for food availability were mixed (Table 1). In wave 1, when the child was 8 years old, children of mothers in Vietnam whose overall level of social support belonged to the upper 50% were likely to have lower HAZ. No significant associations were found in the other three countries. In wave 2, only Peru showed a positive association between maternal financial support and HAZ. Child financial support was negatively associated with HAZ in Ethiopia, while it was positively associated in Peru. The overall level of child support showed no associations in any countries. As for BAZ, only the level of maternal financial support, operationalized both as a continuous and a binary variable, showed a positive association when a child was 12 years old in India (Table 1).
Table 2 shows results from logistic regression models examining the association between social support and food availability. As previously described in the Methods section, we limited the analyses only to the social support variables that showed significant associations with HAZ or BAZ (presented in Table 2). The only significant relationship that was observed was a positive association between the level of maternal financial support in Peru and the probability of having enough food in wave 2.
Finally, causal mediation analysis using the method of Imai et al. was performed only in Peru, since it was the only country to show a significant association between maternal financial support and food availability (Table 3). Our model testing the mediating role of food availability in linking maternal financial support to HAZ in Peru showed that the average causal mediation effect of the upper 50% of maternal financial support was less than zero and statistically non-significant at the 95% level, implying that food availability was not a significant mediator of the impact of maternal financial support on HAZ.
Discussion
Although extensive efforts have been made to elucidate whether social capital has any benefit on a child’s nutritional status, the results on the effect of maternal social capital have been mixed across studies depending on the type of social capital, child’s age, and geographical location. Furthermore, improved food security has been hypothesized as one of the key mechanisms explaining the positive effect of social capital on child anthropometry, but this hypothesis has never been examined empirically to our knowledge.
Our results do not support a strong or consistent relationship between maternal and child support a child nutritional status. A positive association between maternal and child financial support and HAZ was only found in Peru. However, negative associations were found for overall maternal social support and child financial support in Vietnam and Ethiopia, respectively. In De Silva’s study (2007), the associations between maternal social support and HAZ and weight-for-age z-score of children aged between 6 and 18 months also varied across four LMICs15. However, unlike our results, the direction was consistently positive. Although we need to be cautious in the interpretation of negative or non-significant associations between maternal/child social support and child nutritional status, it is postulated that child nutritional status at an earlier age or the nature of social capital as shaped by cultural differences among countries might have affected the results. First, our analyses targeted children aged 8 years old (wave 1) and 12 years old (wave 2), which are older ages than those analyzed by De Silva (2007). Height and weight are more sensitive to feeding status or growth stimulation at a younger age than at later stages of growth. Evidence shows that catch-up growth of preterm infants measured by weight or height mainly occurred from the 10th to 12th months of life37. Another study reported that the catch-up growth of malnutrition of institutionalized children who were adopted before the age of 12 months old was much larger than that of children adopted after 12 months old38. In light of this, children who suffered from poor nutritional status, such as stunting or low weight at an earlier age, especially before 12 months, would have had greater difficulties catching up to normal children, such that any help from sources of social support may have been inadequate to overcome their growth deficit. Second, since our results are from cross-sectional data, we cannot rule out the possibility of reverse causality (i.e., support is provided to mothers whose children are not growing properly)15. Third, there might have been a dark side of social capital—namely, participation in groups might have placed an additional burden on mothers39, interfering with their ability to care for their children15. A further exploration based on longitudinal data and qualitative studies may be necessary to address this research gap.
Several mechanisms have been proposed to explain the positive effect of social support on child nutritional status. Social support enables mothers to gain knowledge (e.g., how to feed their children for better nutritional status), and give better care (e.g., practicing hygiene habits or breastfeeding longer)40. This effect would be more marked in societies where mothers have low levels of education, and therefore, could not have obtained the necessary knowledge through schooling. Emotional support is beneficial for maternal mental health, which can also be linked to improved child growth41,42. Martin et al. (2004) provided another theory that social capital is associated with reduced odds of household hunger and food insecurity16. Availability and access to food can be enhanced by collectively sharing information and resources. In an LMIC context, sharing seeds and livestock breeds could be good examples. Further, in communities with strong ties, solidarity, and networks, people can share food itself during times of hunger18. However, our analyses revealed that child nutritional status was associated only with financial support both for the mother and child, and food availability was not a mediator.
There are several possible explanations for the lack of a mediation effect of food availability. First, the YL study over-sampled households from poor sites, and data from India were collected only in Andhra Pradesh, one of the poorest states. Therefore, food or sources of food (seed or livestock) might not have been sufficient across the community. Even if someone had social support, these sources of support might not have had enough food to share. In Cattel’s (2001) qualitative study, individuals who were part of homogeneous networks of poor households were less likely to receive effective support because other members were not able to provide the required assistance15,43. Second, since healthy growth requires a continuous supply of a well-balanced diet, one-off or sporadic support would not be linked to improvements in children’s anthropometric parameters. Cultural specificity of social networks may determine to what extent and how people can give and receive support from each other. Specifically, the type and the nature of social networks might vary across different cultural settings due to different norms15. For example, social networks based on religious groups might be stronger in some cultural settings than in others44,45. Depending on the cultural context, having someone to rely on in specific circumstances may or may not translate to the availability of long-term and stable support15. Questions about the strength of ties with the source of support or the frequency of receiving help from them would help uncover the practical contribution of social support to child nutritional status. Finally, having enough food in the household does not necessarily mean that the household members have consumed enough food. This information also does not reflect the nutritional value or quality of the food.
In light of the above considerations, we are faced with a challenging question: how can a positive association between child anthropometric indicators and financial support to mothers be explained other than through securing enough food? Although further explorations are needed, previous studies on mechanisms linking better economic status and improved nutritional status might provide some clues. For example, improved financial status makes it possible for mothers to access health care services when their children become ill46. Furthermore, environmental factors such as improved water, sanitation47,48, and cleaner fuel46,49 have been found to be associated with improvements in anthropometric indicators. Financial support might have been used to improve these environmental factors rather than to obtain food.
There are several limitations to consider when interpreting the results. First, although the YL study is a cohort survey, we could not exploit the longitudinal design for the analyses because social capital was not uniformly measured across the waves. The cross-sectional analysis limits our ability to draw causal inferences. Second, the levels of maternal and child social support were arbitrarily categorized. We classified the level of maternal and child social support as being in the upper or lower 50% using median cutoff values; this decision was made considering the high skewness and substantially different distributions of data across the countries. However, to reduce the possibility of bias from arbitrary operationalization of the variables, we presented results from models wherein social support was operationalized as a continuous or a binary variable. Third, child nutritional status can be affected not only by food availability, but also by food quality, which can be captured through the concept of food security. Fourth, although the effect of social support might vary depending on the type (e.g., tangible, informational, or emotional support)50, the YL study does not have information on the types of social support that mothers received. Fifth, paternal social support and characteristics might also affect food availability or child nutritional status. The lack of detailed information on food security, social support (i.e., measurements of the strength and frequency of support), or paternal characteristics limits the interpretation of our study results. Sixth, although the mother’s health status during ante- and intra-partum periods might affect the child’s nutritional status51,52, information on these periods was not gathered in the older cohort survey. This might have confounded our results. Finally, the data for the study are more than 15 years old, which may raise the question of whether the results remain valid in the present context of the study setting. However, the findings of our study still may offer implications to other LMICs currently experiencing similar contexts to those of the study countries in the survey years.
Despite its several limitations, the present study contributes to our understanding of whether interventions to boost maternal or child social support can be a practical approach of improving children’s growth status in a resource-poor setting. Our findings suggest that interventions to strengthen social support in anticipation of a positive effect on improving child nutritional status, especially through facilitating food availability in the household by sharing or supporting, may be unreliable in very poor communities. Furthermore, the observed variability across countries implies that a “one size fits all” approach for enhancing social support may not be appropriate. Future research should seek to examine the effect of social support on child nutritional status in various contexts, including those where food resources are abundant (e.g., communities participating in a food aid program), using the concept of food security.
Ethical approval and consent to participate
The Young Lives Study provides anonymous, secondary data that are publicly available for scientific use. We downloaded the data without identifiers; thus, the confidentiality of the information given by the participants was guaranteed. Therefore, ethical approval was not required. Participants provided signed informed consent before the study commenced and were assured of confidentiality.
Data availability
All methods were carried out in accordance with the relevant guidelines and regulations. Data are available from the UK Data Service website (at https://discover.ukdataservice.ac.uk/series/?sn=2000060). Users are required to register and apply for a password with the UK Data Service and sign a confidentiality agreement before getting access to the data. Users are also asked to inform the UK Data Service and Young Lives of any analysis or publication resulting from their work with the dataset.
References
Blossner, M., De Onis, M. & Prüss-Üstün, A. Malnutrition: quantifying the health impact at national and local levels: World Health Organization (2005).
Miller, A. C. et al. How consistent are associations between stunting and child development? Evidence from a meta-analysis of associations between stunting and multidimensional child development in fifteen low-and middle-income countries. J. Public Health Nutr. 19(8), 1339–1347 (2016).
Sudfeld, C. R. et al. Linear growth and child development in low-and middle-income countries: A meta-analysis. J. Pediatr. 135(5), e1266–e1275 (2015).
Black, R. E. et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet 382(9890), 427–451 (2013).
UNICEF/WHO/WB. UNICEF/WHO/World Bank joint child malnutrition estimates: global and regional Accessed through: https://data.unicef.org/topic/nutrition/malnutrition/. 2020.
UNICEF. Improving child nutrition: the achievable imperative for global progress (Accessed March 24, 2020. https://www.unicef.org/nutrition/index_68661.html). United Nations Children’s Fund, 2020.
Humphries, D. L. et al. Cross-sectional and longitudinal associations between household food security and child anthropometry at ages 5 and 8 years in Ethiopia, India, Peru, and Vietnam. J. Nutr. 145(8), 1924–1933 (2015).
Dubos, R. Social capital: Theory and research (Routledge, Abingdon, 2017).
Lin, N. Building a network theory of social capital. Connections 22(1), 28–51 (1999).
Forsman, A. K. et al. Structural and cognitive social capital and depression among older adults in two Nordic regions. Aging Ment. Health 16(6), 771–779 (2012).
Eriksson, M. Social capital and health–implications for health promotion. Glob. Health Action 4(1), 5611 (2011).
Vikram, K. Social capital and child nutrition in India: The moderating role of development. Health Place 50, 42–51 (2018).
Sujarwoto, S. & Tampubolon, G. Mother’s social capital and child health in Indonesia. Soc. Sci. Med. 91, 1–9 (2013).
Harpham, T., De Silva, M. J. & Tuan, T. Maternal social capital and child health in Vietnam. J. Epidemiol. Community Health 60(10), 865–871 (2006).
De Silva, M. J. & Harpham, T. Maternal social capital and child nutritional status in four developing countries. Health Place 13(2), 341–355 (2007).
Martin, K. S. et al. Social capital is associated with decreased risk of hunger. Soc. Sci. Med. 58(12), 2645–2654 (2004).
Dean, W. R., Sharkey, J. R. & Johnson, C. M. Food insecurity is associated with social capital, perceived personal disparity, and partnership status among older and senior adults in a largely rural area of central Texas. J. Nutr. Gerontol. Geriatr. 30(2), 169–186 (2011).
Sseguya, H., Mazur, R. E. & Flora, C. B. Social capital dimensions in household food security interventions: Implications for rural Uganda. Agric. Hum. Values 35(1), 117–129 (2018).
Bennett, I. M. et al. Maternal mental health, and child growth and development, in four low-income and middle-income countries. J. Epidemiol. Community Health 70(2), 168–173 (2016).
Barnett, I. et al. Cohort profile: The Young Lives study. J. Int. J. Epidemiol. 42(3), 701–708 (2013).
Young Lives group.Young lives methods guide: sampling (Available: http://www.younglives.org.uk/files/methods-guide/methods-guide-sampling).
Bailey, K. & Ferro-Luzzi, A. Use of body mass index of adults in assessing individual and community nutritional status. Bull. World Health Organ. 73(5), 673 (1995).
WHO. WHO child growth standards: training course on child growth assessment. 2008.
UN. How to weigh and measure children: assessing the nutritional status of young children in household surveys. New York.: UN, 1986.
Onis Md, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Org. 85, 660–67 (2007).
WHO. WHO reference 2007 STATA macro package.
De Silva, M. J. et al. Psychometric and cognitive validation of a social capital measurement tool in Peru and Vietnam. Soc. Sci. Med. 62(4), 941–953 (2006).
Tuan T, Harpham T, Huong N, et al. Measuring social capital and mental health in Vietnam: a validity study.Technical Report (Available at: https://researchonline.lshtm.ac.uk/id/eprint/19385). London, UK: Centre for Global Mental Health, 2005.
Thomas EPSC. Social capital and women's health in Sub-Saharan Africa. London South Bank University, 2004.
Briones K. How many rooms are there in your house? Constructing the young lives wealth index. Technical note 43. Oxford, UK: University of Oxford, 2017.
Baron, R. M. & Kenny, D. A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Person. Soc. Psychol. 51(6), 1173 (1986).
Imai, K., Keele, L. & Tingley, D. A general approach to causal mediation analysis. Psychol. Methods 15(4), 309 (2010).
Imai, K., Keele, L. & Yamamoto, T. Identification, inference and sensitivity analysis for causal mediation effects. Stat. Sci. 51–71 (2010).
Hicks, R. & Tingley, D. Causal mediation analysis. Stand. Genom. Sci. 11(4), 605–619 (2011).
MacKinnon, D. P., Lockwood, C. M. & Williams, J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivar. Behav. Res. 39(1), 99–128 (2004).
MacKinnon, D. P., Fairchild, A. J. & Fritz, M. S. Mediation analysis. Annu. Rev. Psychol. 58, 593–614 (2007).
Gong, Y.-H., Ji, C.-Y. & Shan, J.-P. A longitudinal study on the catch-up growth of preterm and term infants of low, appropriate, and high birth weight. Asia Pac. J. Public Health 2015;27(2):NP1421–NP31.
Van Ijzendoorn, M. H., Bakermans-Kranenburg, M. J. & Juffer, F. Plasticity of growth in height, weight, and head circumference: Meta-analytic evidence of massive catch-up after international adoption. J. Dev. Behav. Pediatr. 28(4), 334–43 (2007).
Villalonga-Olives, E. & Kawachi, I. The dark side of social capital: A systematic review of the negative health effects of social capital. Soc. Sci. Med. 194, 105–127 (2017).
Anderson, A. K. et al. Social capital, acculturation, and breastfeeding initiation among Puerto Rican women in the United States. J. Hum. Lact. 20(1), 39–45 (2004).
Patel, V. et al. Effect of maternal mental health on infant growth in low income countries: New evidence from South Asia. BMJ 328(7443), 820–823 (2004).
Harpham, T. et al. Maternal mental health and child nutritional status in four developing countries. J. Epidemiol. Community Health 59(12), 1060–1064 (2005).
Cattell, V. Poor people, poor places, and poor health: The mediating role of social networks and social capital. Soc. Sci. Med. 52(10), 1501–1516 (2001).
Koenig, H. G. et al. Modeling the cross-sectional relationships between religion, physical health, social support, and depressive symptoms. Am. J. Geriatr. Psychiatry 5(2), 131–144 (1997).
Krause, N., Ingersoll-Dayton, B. & Liang, J. et al. Religion, social support, and health among the Japanese elderly. J. Health Soc. Behav., 405–21 (1999).
Pongou, R., Ezzati, M. & Salomon, J. A. Household and community socioeconomic and environmental determinants of child nutritional status in Cameroon. BMC Public Health 6(1), 1–19 (2006).
Merchant, A. et al. Water and sanitation associated with improved child growth. Eur. J. Clin. Nutr. 57(12), 1562–1568 (2003).
Magnani, R. J. et al. Breast-feeding, water and sanitation, and childhood malnutrition in the Philippines. J. Biosoc. Sci. 25(2), 195–212 (1993).
Jeyaseelan, L. & Lakshman, M. Risk factors for malnutrition in south Indian children. J. Biosoc. Sci. 29(1), 93–100 (1997).
Cohen, S., Underwood, L. G. & Gottlieb, B. H. Social relationships and health. In: Social Support Measurement and Intervention. New York, NY: Oxford University Press, 3–28 (2000).
Steyn, N. P. et al. What is the nutritional status of children of obese mothers in South Africa?. Nutrition 27(9), 904–911 (2011).
Tigga, P. L. & Sen, J. Maternal body mass index is strongly associated with children-scores for height and BMI. J. Anthropol. 2016 (2016).
Acknowledgements
Min Kyung Kim is gratefully acknowledged for her professional English editing.
Funding
There was no funding to support this study.
Author information
Authors and Affiliations
Contributions
HYL conceived the idea. HYL, IHS, and IK designed the study. HYL analyzed the data and wrote the first draft. All authors interpreted the results. IHS and IK revised the manuscript critically. IK supervised the whole process. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, HY., Song, I. & Kawachi, I. Maternal and child social support and food availability in relation to child growth in four low- and middle-income countries. Sci Rep 12, 5910 (2022). https://doi.org/10.1038/s41598-022-09850-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-09850-1
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.