Abstract
Clopidogrel, an antiplatelet drug, is frequently prescribed to patients diagnosed with ischemic diseases such as those suffering from acute coronary syndromes or ischemic stroke. Despite the drug being effective in majority of the patients, some still experience ischemic events early in the treatment which might be due to poor platelet inhibition. This study aims to investigate the association of cytochrome P450 2C19 (CYP2C19) loss-of-function polymorphisms, haplotypes as well as a wide range of clinical and demographic variables with platelet aggregation phenotypes to clopidogrel in a Pakistani cohort. The study comprised of a total of 120 patients diagnosed with cardiovascular diseases and were treated with clopidogrel. Antiplatelet response to clopidogrel was monitored by Helena AggRAM (HL-2-1785P) and patients with maximal platelet aggregation more than 50% were categorized as low responders and those with less than 50% as high responders. Our results show that 56.6% of patients were homozygous for the CYP2C19 wild-type allele, 38.3% of patients possessed one copy of the CYP2C19*2 allele and 5% of patients possessed both CYP2C19*2 alleles. No CYP2C19*3 allele was found in our patient cohort. There was no statistically significant difference between the high and low responder groups to clopidogrel in terms of extensive, intermediate and poor metabolizer genotypes. However, haplotype (H1), leukocyte count, random blood glucose, and history of diabetes mellitus was associated with the antiplatelet response to clopidogrel. The prevalence of clopidogrel resistance in our population was in line with that reported for other regional and global populations.
Similar content being viewed by others
Introduction
Clopidogrel, an antiplatelet drug which targets thienopyridine P2Y12 receptor, is frequently employed in patients who have been diagnosed with ischemic heart disease, ischemic stroke and acute coronary syndrome (ACS)1,2,3. Clopidogrel functions as an irreversible antagonist of the receptor and is effective in majority of the patients. However, a significant patient population with ACS who are concomitantly treated with aspirin and clopidogrel faces the recurrence of an acute ischemic event early in the treatment4. This ‘resistance’ to the therapeutic effect of clopidogrel might be due to the poor platelet inhibition by the drug which is likely to result in the poor therapeutic response to the antiplatelet therapy5.
Several studies investigating the clopidogrel ‘resistance’ report a prevalence of 15.9% to 49.5%, indicating a huge population-based variation6. This high variability among various populations suggests that environmental and genetic difference may play important roles in determining clopidogrel resistance. Genetic variation in the cytochrome P4502C19 gene has been previously found associated with high ADP-induced platelet aggregation in clopidogrel treated patients7,8. However, it is unlikely that CYP2C19 genetic variation is the only responsible factor for the observed clopidogrel resistance. Various environmental factors may also lead to clopidogrel resistance which may or may not be dependent on the bioavailability of clopidogrel9,10. The choice of blood preservative and the tests used to measure platelet aggregation also influence the clopidogrel’s antiplatelet response11.
Clopidogrel is absorbed in intestinal cells as prodrug, and then transported to hepatocyte where it is converted to active metabolite under the action of different isoforms of CYP enzymes, in a two-step oxidation. CYP2C19 is the principle contributor in both these steps12. Consequently, genetic variations in the CYP2C19 gene bring about variations in the therapeutic responses of both patients and healthy volunteers to clopidogrel13,14,15,16,17. CYP2C19 gene harbors up to 35 known variations or star alleles (CYP2C19 *1–35) as per pharmacogene variation consortium or PharmVar18. In contrast to individuals possessing the wild-type CYP2C19 allele, a reduction in the inhibition of platelet aggregation is observed in clopidogrel treated patients carrying a single or both copies of the defective CYP2C19 allele14. These defective alleles are involved in the inter-individual variation with respect to clopidogrel response13,19. Phenotypic consequence of most of these alleles can range from reduced effect to complete functional loss. Among these, CYP2C19*2 and *3 are considered defining variations. CYP2C19*2 (rs4244285) was the first variant discovered that induces an aberrant splice site in exon 5 (c.681G>A)20 while CYP2C19*3 (rs4986893) leads to a termination codon in place of one for tryptophan (c.636G>A, p.W212X)21. The decreased anti-platelet activity post clopidogrel administration is due to reduced levels of its active metabolite in carriers of at least one of the low activity alleles, CYP2C19*2 or *322. Furthermore, differential clopidogrel response is observed in populations with high prevalence of CYP2C19*2 allele23. An increased risk of heart attack, stroke or high mortality is likely in patients carrying reduced function alleles of CYP2C19 due to their inability to completely convert clopidogrel to its active metabolite. Therefore, a suitable strategy of pharmacogenetic testing for CYP2C19 genetic variants has been recommended for determining patients who may be subjected to a higher risk of adverse events24.
The principal objective of present study is to find out the prevalence of resistance to clopidogrel therapy in Pakistani patients who are taking clopidogrel for various indications and to investigate its relationship with CYPC19*2 and *3 variants and haplotypes. Impact of several other clinical and demographic variables was also explored.
Results
The demographic and basic clinical data of the patients who participated in this study is provided in the Table 1. The average age of our patient cohort was 60 ± 11 years with the patients in the low clopidogrel response group being slightly younger (58 ± 12) than those in the high response group (61 ± 11). The magnitude of platelet aggregation was measured as a percentage, with patients having a maximal platelet response of 0–50% were categorized as “High” responders and those patients having a maximal platelet response of > 50% were regarded as “Low” responders to clopidogrel. Out of the 120 patients 82.5% showed a high level of platelet inhibition. About three fifth of the patients were male. Specifically, in the low responder’s group, 81% (n = 17) patients were male; while 55% (n = 55) male patients were present in the high responders group.
Patients exhibited co-morbidities and various risk factors, mainly diabetes (43%), hypertension (67%), frequent cigarette smoking (31%) and a familial history of coronary artery disease (62%). The majority of the patients were prescribed clopidogrel for ACS (53%), followed by coronary artery disease (16%), ischemic heart disease (9%), and congestive cardiac failure (5%). The concurrent medications used by the patients include statins, 64% (n = 77), angiotensin converting enzyme (ACE) inhibitors 2.5%, (n = 3), clexane 47.5% (n = 57), and beta-blockers 17.5% (n = 21). Clopidogrel indication, the use of concurrent medications, or co-morbidities were found to have no significant association with platelet response to clopidogrel (Table 1).
In all those patients who were administered clopidogrel, the association between the antiplatelet response to clopidogrel and the various biochemical markers was investigated as provided in the Table 2. Multiple parameters such as prothrombin time, activated partial thromboplastin time, hemoglobin, leukocyte count, platelet count, random glucose, urea, creatinine, and fasting blood sugar were measured. Overall, no statistically significant association was observed between the high responders to clopidogrel and most of the studied parameters. However, a significant association was detected between the high responders to clopidogrel and total leukocyte count with high responders having significantly lower leukocyte count.
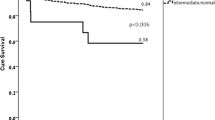
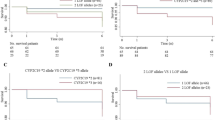
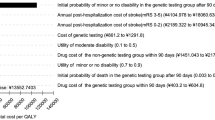
No CYP2C19*3 allele was observed in our cohort. The frequency of CYP2C19*2 allele was 0.241. The prevalence of the extensive metabolizer genotype (CC) in our patient cohort was 0.56 (n = 68), intermediate metabolizer genotype (CT) was 0.38 (n = 46), and poor metabolizer genotype (TT) was 0.05 (n = 6). It was observed that 87% (n = 59) of the patients with extensive metabolizer genotype (CC) exhibited high platelet inhibition as compared to 13% (n = 9) in the low response group (Table 2). With respect to the intermediate (CT) and poor metabolizer genotype (TT), the combined results showed that 77% or 40 of the 52 patients were in high response group while the rest demonstrated a low platelet inhibition response to clopidogrel (Table 2 and Fig. 1). These results suggest that there is no statistically significant difference between low and high responders to clopidogrel and studied genotypes.
CYP2C19*2 diplotype assignment was performed, and was categorized into 4 sub-haplotypes (denoted as H1-H4). Two haplotypes H1 and H2 were found with high frequency in this study. H1 was found with the highest frequency and was also associated with high antiplatelet response to clopidogrel (Table 2). It was observed that 48% (n = 10) of low responders had H1 haplotype while among the high responders, 77% (n = 76) had H1 haplotype. In patients exhibiting high response, 18% (n = 17) had H2 haplotype whereas among the low responders 24% patients (n = 5) possessed H2 haplotype. H3 and H4 were present with a minimum frequency of one each in our patient cohort (Fig. 2).
Correlations between antiplatelet response to clopidogrel and various laboratory and clinical laboratory parameters are presented in Table 3. A significant correlation (p = 0.025) was detected between the high clopidogrel responders and patient gender. No statistically significant correlation or significant difference was observed with regards to age, body mass index, concomitant diseases, and risk factors such as diabetes, hypertension, smoking, CAD familial history, and concurrent medications of the investigated patient cohort and the high responders to clopidogrel. A significant difference and a slight negative correlation were exhibited between leukocyte count and high responders to clopidogrel (R = − 0.206, p = 0.024). Furthermore, a significant correlation was established with regards to random glucose levels and high responders to clopidogrel (R = − 0.218, p = 0.017). No significant difference and no correlation could be established between high responders and the other remaining laboratory findings. The distribution of extensive, intermediate, and poor metabolizer genotypes was similar in high and low responder groups and no statistically significant correlation was found between the two groups in terms of these genotype. However, a negative correlation (R = − 0.233, p = 0.011) between the H1 haplotype and high responders to clopidogrel was observed. No such correlation was detected for the H2 haplotype.
Several risk factors and variables were subjected to a bivariate regression analysis in order to elucidate the predictors of clopidogrel resistance (Table 4). Factors such as age, smoking status, and hypertension did not differentiate between low and high responders to clopidogrel while the presence of H1 haplotype, and diabetes mellitus were significant predictors of clopidogrel response (Table 4).
As mentioned earlier, four haplotypes (H1-H4) with haplotype diversity (0.3542) were identified in the current study. The frequencies of these haplotypes are given in the Fig. 2. Due to the significant association observed between the high responders to clopidogrel and H1, haplotypes were investigated further. The pairwise genetic distances between haplotypes on the basis of AMOVA revealed that the H2 has substantial genetic differences against H3 and H4. On the other hand, H3 displayed high genetic distinction against H4, while H4 has significant distinction against H3 (Fig. 3). During the haplotype network analysis, the median-joining method revealed that H2 is a distinct individual group and highly distant form the H3 and H4 (Fig. 4).
Discussion
The present study is the first of its kind that has investigated the relationship between clinical and demographical variables together with, more importantly, loss-of-function polymorphisms within the CYP2C19 gene, and haplotypes and resistance to clopidogrel therapy in a Pakistani population. Previous studies throughout different regional and global populations exhibited a high variability when it comes to the prevalence of clopidogrel resistance, ranging from as low as approximately 5% to about 45% in German and Spanish populations respectively25,26. In the present investigation, 17.5% of patients in our cohort showed low response to clopidogrel. Wide interethnic variation in different populations such as from 20 to 65% in multiple populations in relation to the frequency of CYP2C19-reduced function genotypes has also been reported27,28. In our patient cohort, the frequency of the reduced function genotypes was 43%.
A total of 3 main CYP2C19 genetic variants—*2, *3, and *17—with important influence on the bioavailability of clopidogrel, have been previously demonstrated29. The bioavailability of active clopidogrel in poor metabolizers is very low. Intermediate metabolizers, albeit having a reduced bioavailability, still exhibit inhibition of platelet activity, when administered with higher than normal doses of clopidogrel30. The majority of the population possess the (*1*1) alleles and are termed as extended metabolizers. Individuals possessing the (*1/*17) and (*17/*17) alleles referred to as rapid and ultra-rapid metabolizers respectively, have also been described, but we were unable to investigate *17 allele in the current study. Furthermore, the number of individuals possessing *17 allele in the general population is much smaller30.
In our investigation, there was no statistically significant correlation between the high and low responders to clopidogrel in terms of extensive, intermediate and poor metabolizer genotypes (Table 2). This might be due to the fact that we found no *3 allele in our genotyped samples, and a low prevalence of *2 allele. These findings are in line with previous reports13, where correlation between clopidogrel resistance and the status of intermediate metabolizers failed to reach statistical significance. Bhatt et al. proposed that the presence of loss-of-function allele could be linked to fewer bleeding complications but without a significant increase in the number of ischemic events31. However, our findings are slightly different from several previous studies30,32, some of which suggest that CYP2C19*2 allele is implicated in conferring resistance to clopidogrel therapy in multiple populations.
In the present study, we observed that low responder group had a significantly higher leukocyte count. This finding is in accordance with recent publications. Osmancik et al. reported that for individuals having a higher leukocytic count, there were increased incidences of high on treatment platelet reactivity33. It seems that the inflammatory mediators such as C-reactive protein, P-selectin, platelet soluble CD40 ligand, and interleukin 6, are able to enhance thrombocyte reactivity33. Interestingly, it has been postulated that high leukocyte counts could, in part, be responsible for conferring the controversial aspirin resistance as well34. Thrombocyte count and clopidogrel response were not significantly correlated in our cohort. These findings are in line with previous studies35,36.
Baseline characteristics indicated a slight difference in creatinine levels between the two groups; however, the difference was insignificant. Previous studies have also linked a wide variety of laboratory and clinical parameters to altered patient responses to clopidogrel therapy. Reduced thrombolytic activity has been observed in individuals diagnosed with and suffering from type 2 diabetes mellitus37,38. On the other hand, lower values of hematocrit have been related to high platelet reactivity39. Our data set shows that, apart from diabetes mellitus, none of these factors have significant difference in both low and high responders to clopidogrel. Similar results have been reported previously40,41.
Regarding concomitant administration of hydroxy methyl glutaryl CoA reductase inhibitors (statins), we found no difference, in terms of clopidogrel resistance, between those on or without such treatment. This is in line with most of the published data42,43. However, it is important to note that detrimental effects of statin treatment (with special consideration to those metabolized by CYP3A4) have been suggested44,45. A residual high on-treatment platelet reactivity was observed with the co-administration of rosuvastatin, which is chiefly metabolized by CYP2C9 with little involvement of CYP3A446. It appears that the data obtained from ex vivo studies disagree with each other, suggesting different levels of interaction. Also, a clinically relevant finding is yet to be reported. Henceforth, it would be safe to suggest that a possible decreased clopidogrel response as a result of statin use, could have a significant impact particularly in high-risk patients.
It is well-known that cigarette smoking induces CYP1A2 enzyme which is responsible for the initial activation of clopidogrel47. Therefore, smoking status of a patient may affect antiplatelet response to clopidogrel. The explanation put forth for this smokers’ ‘paradox’ is that by enhancing the first step in the conversion of clopidogrel, the ‘induced’ CYP1A2 enhances the availability of active metabolites, thus decreasing the proportion of pro-drug excreted without activation47. However, in the present study, no association was found between the smoking status of the patients and the antiplatelet response to clopidogrel (Table 4).
Limitations of our study are that only ‘associations’ could be observed due to its cross-sectional design. Relevant survival profiles could not be created as the lack of clinical outcome data for most of the patients prevented us from doing so. The small sample size for the patients may have lowered the study’s statistical power. Concentrations of clopidogrel and its active metabolite within the plasma were not detected in the present study; thus, individual interviews were used to assume the correct administration of the drug.
The main findings of this study can be summarized as follows: low antiplatelet response to clopidogrel was found in 17.5% of our patients, and more than 43% of the patient population investigated had genotypes for the reduced function CYP2C19 enzyme. Carrying one or both variant alleles of CYP2C19*2 does not appear to significantly enhance the risk of having low response to clopidogrel. H1, the most frequent of the haplotypes, was associated with higher antiplatelet response with respect to clopidogrel. Low antiplatelet response to clopidogrel was associated with a higher leukocyte count. Higher random glucose levels were associated with lower antiplatelet response. Statins, beta-blockers or ACE inhibitor treatment, body mass index, or hematocrit levels didn’t significantly influence clopidogrel response in our data set but patients with diabetes mellitus did show differential response to clopidogrel treatment. Future studies, ideally with larger population samples, should investigate and assess additional clinical parameters and genomic mutations to evaluate and better foresee clopidogrel resistance.
Material and method
Data collection
The Institutional Review Board and Ethics Committee of Shifa Tameer-e-Millat University, Islamabad, Pakistan sanctioned the study. All the methods and procedures were performed in accordance with the relevant guidelines and regulations. All individuals were mandated to provide an informed consent to partake in the investigation. The study cohort comprised of 120 patients taking 75 mg clopidogrel at the time of inclusion in the study. Five milliliters venous blood was taken in the EDTA tube and stored at 4 °C. Gen Jet Genomics DNA extraction Kit (ThermoScientific) was used to isolate the genomic DNA. A 1% agarose gel electrophoresis was used to quantify the genomic DNA. Genomic DNA was stored at − 20 °C and was used later for further processing.
Sequences and PCR information
From purified genomic DNA, the CYP2C19 region containing significant and important variants was targeted for sequencing. The PCR products were purified and submitted to Tsingke Biotechnology, China, for commercial DNA sequence services. For sequence validation, each of the samples was sequenced into triplicates (3×). Data presented in the results contains variations on the reverse strand.
Quality checking and filtration
The accuracy of the DNA sequences was assessed by the Staeden package and Finch. TV v1.4 (Geospiza, Inc; Seattle, WA, United States). High quality of the sequences has been assembled by the Lasergene package v1.7 (DNASTAR, Inc; USA).
Genetic structure analysis
The good quality sequences of CYP2C19 were aligned with the Reference Human Genome (GRch38)48. The SNP positions were identified against the Reference Genome. In Addition, the DnaSP v6 package49 was used to determine the haplotypes in the test sequences . The population statistical analyses like haplotypes distances and frequencies within the individuals, were performed by the Arlequin software v1.350. The network of the haplotypes was drawn by the NETWORK v10 package51 using the median-joining method.
Platelet aggregation
Whole blood aggregometry was used to investigate antiplatelet activity where ADP as platelet aggregation inducing agonist52. Within 30-min to 5-h of placing the blood samples in clean test tubes, comprising of 3.2% sodium citrate anticoagulant (9:1), patient blood samples were tested at a temperature of 37 °C with 1200 rpm stirring speed. Following manufacturer guideline, equivalent amount (volume) of normal saline was used to dilute 500 µL of citrated blood. The response (platelet aggregation) was recorded after placing the electrode in the cuvette where platelet aggregation was induced by ADP (10 µM). For up-to 6 min, recordings were obtained as a measure of electrical impedance in ohms. Percent mean platelet inhibition, after obtaining values from 3 to 4 individual experiments, was calculated.
Statistical analysis
All data were recorded and analyzed using IBM Statistical Package for Social Sciences SPSS, version 23.0. Categorical variables were presented as frequency and percentage whereas for continuous variables, mean and standard deviation or median and interquartile range were calculated for normally distributed and non-normally distributed variables respectively. Normality was tested using Shapiro–Wilk test.
The study participants were categorized on the basis of their response to clopidogrel; maximal platelet aggregation of greater than 50% was characterized as low response and lower than 50% as high response. Comparison of the baseline variables (continuous) via independent samples T-test (or Mann–Whitney U test for non-normally distributed continuous variables) was performed for both response groups. For comparison of categorical variables, chi-square test (or Fisher exact test where expected count per cell is less than 5) was applied.
Correlation analysis was performed in order to study the association between independent variables and platelet inhibition. Pearson correlation (or Spearman’s rank correlation for non-normally distributed continuous variables) was applied to study correlation between continuous independent variables and percentage platelet inhibition. For categorical variables, phi correlation coefficient was calculated taking high response and low response groups as dependent variable. p ≤ 0.05 was regarded as statistically significant.
References
Amsterdam, E. A. et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130, 2354–2394 (2014).
Kernan, W. N. et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45, 2160–2236 (2014).
Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 33, 2569–2619 (2012).
Parodi, G. et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA 306, 1215–1223 (2011).
Papathanasiou, A., Goudevenos, J. & Tselepis, A. D. Resistance to aspirin and clopidogrel: Possible mechanisms, laboratory investigation, and clinical significance. Hellenic J. Cardiol. 48, 352–363 (2007).
Mallouk, N. et al. Prevalence of poor biological response to clopidogrel: A systematic review. Thromb. Haemost. 107, 494–506 (2012).
Wei, Y.-Q., Wang, D.-G., Yang, H. & Cao, H. Cytochrome P450 CYP 2C19*2 associated with adverse 1-year cardiovascular events in patients with acute coronary syndrome. PLoS ONE 10, e0132561 (2015).
Jia, D. et al. CYP2C19 polymorphisms and antiplatelet effects of clopidogrel in acute ischemic stroke in China. Stroke 44, 1717–1719 (2013).
Berger, J. S. et al. Smoking, clopidogrel, and mortality in patients with established cardiovascular disease. Circulation 120, 2337 (2009).
Silvain, J. et al. High on-thienopyridine platelet reactivity in elderly coronary patients: The SENIOR-PLATELET study. Eur. Heart J. 33, 1241–1249 (2012).
Labarthe, B., Théroux, P., Angioï, M. & Ghitescu, M. Matching the evaluation of the clinical efficacy of clopidogrel to platelet function tests relevant to the biological properties of the drug. J. Am. Coll. Cardiol. 46, 638–645 (2005).
Sangkuhl, K., Klein, T. E. & Altman, R. B. Clopidogrel pathway. Pharmacogenet. Genomics 20, 463–465 (2010).
Hulot, J.-S. et al. Cytochrome P450 2C19 loss-of-function polymorphism is a major determinant of clopidogrel responsiveness in healthy subjects. Blood 108, 2244–2247 (2006).
Brandt, J. T. et al. Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J. Thromb. Haemost. 5, 2429–2436 (2007).
Giusti, B. et al. Cytochrome P450 2C19 loss-of-function polymorphism, but not CYP3A4 IVS10 + 12G/A and P2Y12 T744C polymorphisms, is associated with response variability to dual antiplatelet treatment in high-risk vascular patients. Pharmacogenet. Genomics 17, 1057–1064 (2007).
Trenk, D. et al. Cytochrome P450 2C19 681G>A polymorphism and high on-clopidogrel platelet reactivity associated with adverse 1-year clinical outcome of elective percutaneous coronary intervention with drug-eluting or bare-metal stents. J. Am. Coll. Cardiol. 51, 1925–1934 (2008).
Fontana, P., Senouf, D. & Mach, F. Biological effect of increased maintenance dose of clopidogrel in cardiovascular outpatients and influence of the cytochrome P450 2C19*2 allele on clopidogrel responsiveness. Thromb. Res. 121, 463–468 (2008).
Gaedigk, A. et al. The pharmacogene variation (PharmVar) consortium: Incorporation of the human cytochrome P450 (CYP) allele nomenclature database. Clin. Pharmacol. Ther. 103, 399–401 (2018).
Sibbing, D. et al. Cytochrome P450 2C19 loss-of-function polymorphism and stent thrombosis following percutaneous coronary intervention. Eur. Heart J. 30, 916–922 (2009).
de Morais, S. M. et al. The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans. J. Biol. Chem. 269, 15419–15422 (1994).
Botton, M. R. et al. PharmVar GeneFocus: CYP2C19. Clin. Pharmacol. Ther. 109, 352–366 (2021).
Ferreiro, J. L. & Angiolillo, D. J. Clopidogrel response variability: Current status and future directions. Thromb. Haemost. 102, 7–14 (2009).
Chan, M. Y. Clopidogrel pharmacogenetics of east, south and other Asian populations. Eur. Heart J. Suppl. 14, A41–A42 (2012).
Abid, L. et al. Impact of cytochrome P450 2C19*2 polymorphism on the clinical cardiovascular events after stent implantation in patients receiving clopidogrel of a southern Tunisian region. World J. Cardiovasc. Dis. 3, 4–10 (2013).
Müller, I. et al. Prevalence of clopidogrel non-responders among patients with stable angina pectoris scheduled for elective coronary stent placement. Thromb. Haemost. 89, 783–787 (2003).
Angiolillo, D. J. et al. Identification of low responders to a 300-mg clopidogrel loading dose in patients undergoing coronary stenting. Thromb. Res. 115, 101–108 (2005).
Varenhorst, C. et al. Genetic variation of CYP2C19 affects both pharmacokinetic and pharmacodynamic responses to clopidogrel but not prasugrel in aspirin-treated patients with coronary artery disease. Eur. Heart J. 30, 1744–1752 (2009).
Mărginean, A., Bănescu, C., Scridon, A. & Dobreanu, M. Anti-platelet therapy resistance—Concept, mechanisms and platelet function tests in intensive care facilities. J. Crit. Care Med. 2, 6–15 (2016).
Mega, J. L. et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N. Engl. J. Med. 360, 354–362 (2009).
Rath, P. C. et al. A study on the impact of CYP2C19 genotype and platelet reactivity assay on patients undergoing PCI. Indian Heart J. 67, 114–121 (2015).
Bhatt, D. L. et al. The relationship between CYP2C19 polymorphisms and ischaemic and bleeding outcomes in stable outpatients: The CHARISMA genetics study. Eur. Heart J. 33, 2143–2150 (2012).
Kim, K. A., Park, P. W., Hong, S. J. & Park, J.-Y. The effect of CYP2C19 polymorphism on the pharmacokinetics and pharmacodynamics of clopidogrel: A possible mechanism for clopidogrel resistance. Clin. Pharmacol. Ther. 84, 236–242 (2008).
Osmancik, P., Paulu, P., Tousek, P., Kocka, V. & Widimsky, P. High leukocyte count and interleukin-10 predict high on-treatment-platelet-reactivity in patients treated with clopidogrel. J. Thromb. Thrombolysis 33, 349–354 (2012).
Mannini, L. et al. Erythrocyte deformability and white blood cell count are associated with aspirin resistance in high-risk vascular patients. Clin. Hemorheol. Microcirc. 35, 175–181 (2006).
Li, L. et al. Clopidogrel resistance of patients with coronary artery disease and its correlation with platelet count and mean platelet volume. Zhonghua Yi Xue Za Zhi 93, 916–920 (2013).
Uzun, F. et al. Antiplatelet resistance and the role of associated variables in stable patients treated with stenting. Postepy Kardiol Interwencyjnej 11, 19–25 (2015).
Angiolillo, D. J. & Suryadevara, S. Aspirin and clopidogrel: Efficacy and resistance in diabetes mellitus. Best Pract. Res. Clin. Endocrinol. Metab. 23, 375–388 (2009).
Ertugrul, D. T. et al. Aspirin resistance is associated with glycemic control, the dose of aspirin, and obesity in type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 95, 2897–2901 (2010).
Cecchi, E. et al. Effect of blood hematocrit and erythrocyte deformability on adenosine 5′-diphosphate platelet reactivity in patients with acute coronary syndromes on dual antiplatelet therapy. Am. J. Cardiol. 104, 764–768 (2009).
Zaccardi, F., Pitocco, D., Willeit, P. & Laukkanen, J. A. Efficacy and safety of P2Y12 inhibitors according to diabetes, age, gender, body mass index and body weight: Systematic review and meta-analyses of randomized clinical trials. Atherosclerosis 240, 439–445 (2015).
Ibrahim, O. et al. Evaluation of aspirin and clopidogrel resistance in patients with acute coronary syndrome by using adenosine diposphate test and aspirin test. Pak. J. Med. Sci. 29, 97–102 (2013).
Ojeifo, O. et al. Concomitant administration of clopidogrel with statins or calcium-channel blockers: Insights from the TRITON-TIMI 38 (trial to assess improvement in therapeutic outcomes by optimizing platelet inhibition with prasugrel-thrombolysis in myocardial infarction 38). JACC Cardiovasc. Interv. 6, 1275–1281 (2013).
Mitsios, J. V. et al. Atorvastatin does not affect the antiplatelet potency of clopidogrel when it is administered concomitantly for 5 weeks in patients with acute coronary syndromes. Circulation 109, 1335–1338 (2004).
Lau, W. C. et al. Atorvastatin reduces the ability of clopidogrel to inhibit platelet aggregation: A new drug-drug interaction. Circulation 107, 32–37 (2003).
Brophy, J. M., Babapulle, M. N., Costa, V. & Rinfret, S. A pharmacoepidemiology study of the interaction between atorvastatin and clopidogrel after percutaneous coronary intervention. Am. Heart J. 152, 263–269 (2006).
Verdoia, M. et al. Impact of atorvastatin or rosuvastatin co-administration on platelet reactivity in patients treated with dual antiplatelet therapy. Atherosclerosis 243, 389–394 (2015).
González, A. et al. Effect of CYP2C19 polymorphisms on the platelet response to clopidogrel and influence on the effect of high versus standard dose clopidogrel in carotid artery stenting. Eur. J. Vasc. Endovasc. Surg. 51, 175–186 (2016).
Cunningham, F. et al. Ensembl 2019. Nucleic Acids Res. 47, 745–751 (2019).
Rozas, J. et al. DnaSP 6: DNA sequence polymorphism analysis of large data sets. Mol. Biol. Evol. 34, 3299–3302 (2017).
Excoffier, L., Laval, G. & Schneider, S. Arlequin (version 3.0): An integrated software package for population genetics data analysis. Evol. Bioinform. Online 1, 47–50 (2007).
Bandelt, H. J., Forster, P. & Röhl, A. Median-joining networks for inferring intraspecific phylogenies. Mol. Biol. Evol. 16, 37–48 (1999).
Bauriedel, G. et al. Antiplatelet effects of angiotensin-converting enzyme inhibitors compared with aspirin and clopidogrel: A pilot study with whole-blood aggregometry. Am. Heart J. 145, 343–348 (2003).
Author information
Authors and Affiliations
Contributions
S.A., S.U.S. and A.H. conceptualized the study, S.G., and S.A. carried out the bench work, S.A., S.S., K.J., F.S.S., H.K., and M.H.H. did the analysis, wrote the original draft as well as the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, S., Gul, S., Siraj, S. et al. Antiplatelet response to clopidogrel is associated with a haplotype in CYP2C19 gene in Pakistani patients. Sci Rep 12, 6171 (2022). https://doi.org/10.1038/s41598-022-09679-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-09679-8
This article is cited by
-
Genetic variability in stroke patients: CYP2C19 polymorphisms unraveled
BMC Medical Genomics (2024)
-
Electrochemical peptide nucleic acid functionalized α-Fe2O3/Fe3O4 nanosheets for detection of CYP2C19*2 gene
Microchimica Acta (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.