Abstract
Weight loss through behavioral modification is central to treating non-alcoholic fatty liver disease (NAFLD). To achieve this, patients need to accurately self-perceive their health behaviors. We aimed to identify predictors of concordance between self-perception and objective measures of body weight, physical activity (PA) and dietary behaviors. We used data from the Harris County NAFLD Cohort, an ongoing prospective study in a regional safety-net healthcare system. Patients completed self-administered baseline questionnaires on demographics, diet, PA, and self-perceptions. We assessed concordance between actual and self-perceived body weight and energy-balance behaviors. Multivariable logistic regression identified predictors of concordance. Patients (n = 458; average age 46.5 years) were 90% Hispanic and 76% female. PA and fruit/vegetable intake guidelines were met among 37% and 9%, respectively. Most (89%) overweight/obese patients accurately perceived themselves as such. However, 41% of insufficiently-active and 34% of patients not meeting fruit/vegetable intake guidelines inaccurately self-perceived their behaviors as “just right”. Women were 3 times more likely to accurately self-perceive weight status (adjusted odds ratio [AOR] 3.24; 95% CI 1.68–6.25) but 51% less likely to accurately self-perceive PA levels than men (AOR 0.49; 95% CI 0.29–0.81). Lower acculturation was associated with higher odds of accurate PA self-perception. Patients with prediabetes or diabetes vs normoglycemia were more likely to accurately self-perceive their fruit/vegetable intake. Most NAFLD patients accurately self-perceived their body weight. A third or more of those not meeting fruit/vegetable intake or PA guidelines had inaccurate perceptions about their behaviors. Our findings highlight key areas to target in NAFLD-specific behavioral modification programs.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a significant public health concern in the U.S. It is the second leading indication for liver transplantation1, a rising cause for hepatocellular carcinoma2,3, and associated with adverse cardiovascular outcomes4. Excess body fat is the central pathogenic mechanism underlying NAFLD5. Its prevalence has grown rapidly in parallel with obesity, to a current estimate of 25%6. Hispanics have a 57% higher risk of NAFLD than non-Hispanic Whites (NHW) and women have a higher risk of advanced NAFLD fibrosis than men7.
Behavioral modification with the goal of weight loss through changes in diet and physical activity (PA) is central to NAFLD treatment8,9,10. Weight loss of 5%, 7%, and 10% from baseline is associated with meaningful reductions in hepatic steatosis, steatohepatitis, and hepatic fibrosis, respectively9. Reductions in total calorie and sugar intake, increased fruit/vegetable intake and increased aerobic PA are each independently associated with reductions in liver fat and improvements in insulin resistance8. As such, clinical guidelines emphasize weight loss, dietary changes, and increased PA11.
Behavioral change is a complex process, influenced by multiple cognitive and social determinants. A key initial step toward achieving behavioral change, according to the Transtheoretical Model of Behavior Change12, is for patients to transition from having no intention to change to intending to take action through self-reflection and personal reassessment. Patients must believe it is necessary to lose weight and modify their behaviors. While several additional factors ultimately influence the likelihood of behavioral change success, this belief is paramount; without it, patients they are less likely to take action13. Thus, an important aspect to assisting patients achieve successful behavior change is to understand if patients’ self-perceptions of body weight and lifestyle behaviors align with objective measures. This is particularly important among Hispanic patients who have the highest rates of NAFLD14 and also have, irrespective of NAFLD status, greater weight misperception than NHW15,16.
This study aimed to identify the demographic and clinical predictors of concordance between objective measures and self-perception of body weight status, PA, and dietary behaviors among a predominantly Hispanic population of patients with NAFLD at their baseline hepatology clinic visit. The overarching purpose was to elucidate the rates and predictors of discordance in behavioral self-perception, which could serve as targets for counseling. Based on prior research conducted among non-NAFLD populations, we hypothesized that there would be differences in discordance rates based on sex, education level, and acculturation status17,18,19,20. In addition, we performed an exploratory analysis to characterize clinically significant weight loss, as a proxy for behavioral change, by patients’ baseline concordance between objective measures and self-perception of PA and fruit/vegetable intake.
Methods
Study design and population
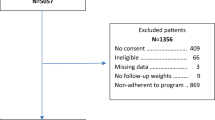
We conducted a cross-sectional study among patients participating in the Harris County NAFLD Cohort (HCNC) from 2015 to 2019. The HCNC is an ongoing prospective cohort study that includes consecutive adult patients with NAFLD referred to a multidisciplinary clinic staffed by both a hepatologist and an endocrinologist within the Harris Health System, the main regional safety-net healthcare system for residents of Houston, Texas. The inclusion criteria were age ≥ 18 years and presence of NAFLD. The exclusions were presence of alternative liver disease etiologies (described below), decompensated cirrhosis, or hepatocellular carcinoma at baseline. The study was approved by the Baylor College of Medicine and Harris Health System institutional review boards. All research procedures were performed in accordance with relevant guidelines and regulations and in accordance with the Declaration of Helsinki. All participants provided written informed consent.
At the baseline visit, patients completed self-administered questionnaires. Subsequently, patients underwent clinical evaluation that included a detailed liver disease and metabolic assessment.
NAFLD was uniformly diagnosed across the patient population using the following criteria: presence of hepatic steatosis detected by abdominal ultrasound performed within 1 year of the baseline visit and exclusion of patients with chronic excessive alcohol consumption (> 14 and > 21 standard drinks/week on average for ≥ 2 years among women and men, respectively)11, viral hepatitis, hemochromatosis, Wilson’s disease, cholestasis, autoimmune disease, drug induced liver injury, or medications associated with hepatic steatosis.
All patients received standard of care management of NAFLD which included clinic based lifestyle modification counseling delivered by both the hepatologist and endocrinologist. The counseling emphasized caloric restriction and a dietary pattern aligned with the MyPlate method which encourages a shift to more vegetable and fruit intake, less added sugars, and a shift away from saturated fats and toward mono-unsaturated fats21. Counseling also emphasized moderate intensity aerobic physical activity of at least 150 min weekly22. In addition, all patients were referred to a dietitian for continued counseling and returned to the clinic for regular care at 3–6 month intervals. Patients enrolled in the study are being followed over time for changes in weight and development of clinically significant liver disease complications (i.e., hepatic decompensation, hepatocellular carcinoma, or death) and changes in weight. We collected the information at baseline, and ascertained changes in weight prospectively.
Variables and measures
Demographic characteristics and clinical parameters
At baseline, we collected demographic characteristics including age, sex, race/ethnicity, education, primary language, country of birth, and if born outside the U.S., age moved to the U.S. Three proxy acculturation variables were used: primary language spoken, country of birth, and duration living in the U.S. We classified prediabetes or type 2 diabetes based on the presence or absence of a pre-existing diagnosis reported by the patient or documented in the electronic medical record.
Current alcohol use was assessed using two items. The first assessed whether a participant currently consumed alcohol. If the response was affirmative, then frequency and quantity of alcohol use over the prior 1 year was assessed using the Alcohol Use Disorders Identification Test-C (AUDIT-C)23. Scores of < 3 in women and < 4 in men were classified as non-risky; scores ≥ 3 in women and ≥ 4 in men were classified as risky. Smoking was assessed with the National Health Interview Survey standard single-item measure assessing if a participant had smoked ≥ 100 cigarettes in their lifetime and then classifying patients as never, current or former users.
Body weight
Each patient’s weight and height were measured at the baseline visit and used to calculate body mass index (BMI). Patients were classified as underweight/normal weight (BMI < 25 kg/m2) or overweight/obese, which included anyone who met World Health Organization Weight Status criteria for overweight to obese class III (i.e. BMI ≥ 25 kg/m2)24. We assessed weight change among patients who had their weight measured during follow-up clinic visits 9 to 24 months post-baseline (median = 15 months).
Physical activity measures
We used the Rapid Assessment of Physical Activity Scale (RAPA), a 7-item questionnaire validated among both Spanish and English speaking samples that asks participants how physically active they are25,26. Using standard scoring procedures, participants were classified as active or insufficiently active. Active was defined as moderate-intensity PA for ≥ 30 min/day for ≥ 5 days/week or vigorous-intensity PA for ≥ 20 min/day for ≥ 3 days/week per American College of Sports Medicine guidelines27; insufficiently active was defined as all other responses.
Dietary variables
We used the modified version of the National Cancer Institute’s FLASHE screener (26 items) to capture daily intake of dietary factors commonly consumed in the U.S.28, including fruits, vegetables, sugar-sweetened beverages (SSB) and sweet foods. Daily fruit/vegetable intake was quantified using two items that assessed the average number of servings consumed each day. Because dietary guidelines specific to NAFLD do not exist, we applied national dietary guidelines that are widely applicable. These indicate that adult women need at least 1½ cups of fruit and 2½ cups of vegetables and adult men need at least 2 cups of fruit and 3½ cups of vegetables daily29. We classified patients as either meeting or not meeting these guidelines.
Daily SSB intake was calculated using 4 items capturing frequency of consuming sweetened fruit drinks and teas, regular soda/pop, sports drinks, and pure fruit juice. Daily sugary food intake was calculated with 4 items capturing frequency of consuming candy or chocolate, sugary baked items, frozen desserts, and sugary cereals. We converted responses based on frequency to average daily intake and summed the 4 relevant items to determine daily SSB and sugary food intake30.
Self-perceptions of body weight, dietary patterns, and exercise behaviors
At baseline, a series of single-items were used to assess how patients perceived their own body-weight status, dietary patterns and PA. To assess self-perception of weight status, participants were asked whether they considered themselves to be “overweight” versus “underweight or about right”31,32,33,34. Using yes/no responses, participants were also asked if they felt like they needed to lose weight, thought that they should eat healthier, considered themselves to be physically activity, and wanted to be more physically active. Three items assessed whether participants thought they ate the right amount of or needed to eat 1) more fruits/vegetables, 2) less fat, and 3) less sugar35.
Statistical analyses
We used descriptive statistics to assess demographic and behavioral characteristics and tested sex differences. Baseline concordance was calculated between (1) measured BMI vs. participant perception of being overweight/obese or underweight/about right, (2) fruit/vegetable intake measured by the FLASHE dietary screener vs. participant perception of eating the right amount or needing to eat more fruits and vegetables, and (3) PA level measured by the RAPA vs. participant perception of being active or not. We compared the demographic and clinical characteristics between people with discordant versus concordant perceptions of weight status, fruit/vegetable intake, and physical activity status using chi square analysis and student t test.
Univariable and multivariable analyses assessed the cross-sectional association of demographic and clinical characteristics with accuracy of (1) weight status, (2) PA levels and (3) fruit/vegetable intake. The multivariable models included all characteristics from univariable analysis.
Lastly, we explored differences in demographic and clinical characteristics, as well as baseline accuracy of PA and fruit/vegetable intake perceptions between those who did and did not achieve clinically significant weight loss (CSWL) defined as ≥ 5% weight loss one year later. Given the limited sample size and the exploratory nature of this aim, we did not perform tests of statistical significance. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
The study population’s (n = 458) average age was 46.5 years; 76.0% were women, 90.0% were Hispanic, and 53.5% had diabetes. Overall, 96.5% of the study population were overweight or obese: 21.8% met WHO criteria for overweight status, 35.2% for obesity I, 19.4% obesity II, and 20.1% obesity III (Table 1). Approximately 9.0% of patients met or exceeded the fruit/vegetable intake guidelines and 36.7% were physically active (Table 2). Most reported that they needed to lose weight (88.7%) and wanted to be more physically active (89.7%). While 91.9% reported that they could eat healthier in general, only 60.5% thought that they should eat more fruits/vegetables, 69.2% thought that they should eat less fat and 65.1% thought they should eat less sugar.
There was high concordance (88.4%) between objective measures and self-perceptions of weight status among the overall study population (Table 3). However, there was less concordance between actual and self-perceived PA levels or fruit/vegetable intake (Table 3). Overall, only 65.8% and 62.8% of all patients concordantly self-perceived their PA levels and fruit/vegetable dietary intake, respectively. Table 4 presents concordance between objective measures and self-perceptions among the patients with the highest risk behavior profiles: 88.5% of overweight/obese, 59.1% of insufficiently active, and 65.8% of those who did not meet fruit/vegetable intake thresholds concordantly self-perceived their status.
Table 5 and Supplementary Table S1 present the associations between patient characteristics and accuracy of self-perceptions. In the multivariable model, women were three-fold more likely as men to concordantly perceive their weight status (adjusted OR (AOR) 3.24, 95% CI 1.68–6.25). Hispanic ethnicity was associated with three-fold greater odds of concordantly self-perceiving weight status on univariable analysis (OR 3.04, 95% CI 1.49–6.21); this association was attenuated and no longer statistically significant on multivariable analysis (AOR 1.87, 95% CI 0.54–6.51). Women were 51% less likely than men to concordantly self-perceive their PA levels (AOR 0.49, 95% CI 0.29–0.81). Lower acculturation was also independently associated with 2.5-fold higher odds of concordant self-perceived PA levels: Spanish vs. English/bilingual (AOR 2.55, 95% CI 1.35–4.80). Those with prediabetes or diabetes had 2.6-fold greater odds of concordantly perceiving the adequacy of their fruit/vegetable intake than those with normoglycemia (AOR 2.63, 95% CI 1.61–4.31).
Among the 322 patients with available follow-up weight data, 51 (16%) experienced clinically significant weight loss (i.e., ≥ 5% of baseline weight) (Table 6). We observed no differences in baseline characteristics between patients who did and did not experience clinically significant weight loss (Supplementary Table S2). Among the 4 PA concordance groups, the highest proportion of clinically significant weight loss was observed among patients who were active at baseline but had a discordant self-perception (i.e., felt they needed more physically activity: 38% of 24 patients). Among the 4 fruit/vegetable intake concordance groups, the highest proportion of clinically significant weight loss was observed among patients who accurately self-perceived their fruit/vegetable intake. Specifically, 25% of 12 patients who met daily fruit/vegetable intake guidelines with concordant self-perceived dietary habits, and 21% of 82 patients who did not meet daily fruit/vegetable intake guidelines with concordant self-perceived dietary habits had ≥ 5% weight loss.
Discussion
Behavioral change leading to dietary modifications, increased PA and weight loss, is central to NAFLD treatment. Prior research has shown that there are multiple determinants of behavioral change that need to be targeted to help patients achieve healthy habits and weight loss. Unfortunately, there is a paucity of research characterizing behavioral determinants among patients with NAFLD, which is important for formulating improved strategies. Our study is the first to provide insight into NAFLD patients’ perceptions regarding their own lifestyle behaviors, which is one of many determinants of behavioral change, upon first presentation to a hepatology clinic. Among a predominantly Hispanic population, we found that most felt they needed to lose weight and overweight/obese patients accurately self-classified their weight status. To achieve and sustain weight loss, it is important to change both PA and dietary behaviors36. Therefore it is less reassuring that approximately 34% of patients with inadequate fruit/vegetable intake and 41% of inactive patients believed their behaviors as adequate. These high discordance rates highlight a need to correct patients’ perceptions of these behaviors as a first step toward influencing patients’ readiness for change37. It is vital that clinicians and healthcare teams who engage in lifestyle counseling understand patients’ self-perceptions of their current behaviors.
Our findings demonstrate that patients with NAFLD need targeted and detailed counseling regarding specific dietary components. Only 10% of the overall study population actually had adequate fruit/vegetable intake. The fact that only 33% of the study population nevertheless felt their fruit/vegetable intake was “just right” coupled with the large proportion of patients who inaccurately perceived themselves as having adequate fruit/vegetable intake points to the importance of targeting this dietary component during dietary counseling sessions. Fruit/vegetable intake is an important component of the Mediterranean diet, which is associated with reductions in liver fat and widely recommended for patients with NAFLD38,39. Fruits/vegetables may be associated with lower hepatocellular carcinoma risk and have beneficial effects on insulin resistance40,41. It is notable that a baseline diagnosis of pre-diabetes/diabetes was associated with a 2.6-greater likelihood of accurate self-perceived fruit/vegetable intake. Given that prediabetic/diabetic patients are more likely to have discussed diet with a dietician or physician prior to presenting to a NAFLD clinic, this finding may reflect the importance of teaching patients and correcting misperceptions about adequate daily fruit/vegetable intake. Expanded counseling from a dietician, with a potential focus on improving misperceptions and increasing knowledge, may be key to moving NAFLD patients toward behavioral change.
Our findings also demonstrate that a second high-yield area for nutritional targeting is sugar. The Mediterranean diet also emphasizes reductions in added sugars and intake of mono-unsaturated over saturated fats42,43. Across the entire study population, 97% expressed that they could eat healthier but only 65% thought that they should eat less sugar. We did not assess the concordance between actual and self-perceived sugar intake because while national guidelines recommend reductions in and specific thresholds for added sugar, they do not provide specific daily intake thresholds for all dietary sugar. However, it is well established that simple sugar and fructose intake are important to avoid as they drive NAFLD pathogenesis through de novo lipogenesis and insulin resistance44,45. Given the relatively high sugary food and beverage intake observed across the study population, it is concerning that 28% felt they were eating the “right” amount of sugar and did not identify a need for reduction. Sugar intake, thus, may represent a high-yield area for targeted intervention.
We examined differences in perceptions by various demographic characteristics, finding that there were differences by gender. Given that women have a higher risk of NAFLD progression than men7, it is encouraging that women with NAFLD were three times as likely as men to accurately identify their weight status. It is disconcerting, however, that women were less likely to accurately recognize insufficient PA levels. It is also concerning that 20% of overweight/obese men underestimated their weight status. Central obesity is the strongest risk factor for cirrhosis among Hispanic men in Texas46, and inaccurate weight status perception among those who are overweight or obese has been associated with fewer attempts to lose weight15. The observed gender disparity in self-awareness regarding weight status may reflect differences in body image perceptions among men versus women and warrants further qualitative study47. The immediate clinical implication is that discussions on lifestyle modifications among men with NAFLD may need to begin with a greater emphasis on defining what it is to be medically overweight or obese. Discussions among women should define and emphasize PA recommendations.
We also examined differences in perceptions by acculturation. With greater exposure to new lifestyles, diets, beliefs, and environments, Hispanic immigrants to the U.S. become more “acculturated” which is associated with a higher prevalence of NAFLD risk factors and potentially with transformed perceptions of their own lifestyle habits48. We found that one proxy of lower acculturation, namely Spanish-language preference, was associated with nearly 3 times higher odds of accurately self-perceiving PA levels. In other words, Hispanics with greater acculturation were more likely to misperceive their low PA levels as being sufficient and vice versa. This finding may reflect a social desirability bias among highly acculturated Hispanics. More highly acculturated Hispanics tend to engage in higher levels of leisure-time PA49,50; thus, they may also be more aware of the expectation of performing leisure-time PA in the U.S. and consequently misrepresent engaging in high levels of PA to their healthcare providers. Given this possibility, exercise counseling administered to highly acculturated Hispanic NAFLD patients (i.e., born in the U.S. and/or prefer English) should emphasize the minimum PA recommendations outlined by the U.S. PA Guidelines for Americans and the medical importance of adhering to them.
Study limitations
To our knowledge, this is the first study to provide insight into the concordance between actual and self-perceived patterns of weight status, PA and fruit/vegetable intake among patients with NAFLD at baseline, prior to receiving specialty care in a hepatology clinic. However, certain limitations must be acknowledged. Because this was a cross-sectional study, casual links between the study variables and concordance between actual and self-perceived behaviors cannot be established. Several survey questions were single items, limiting our ability to capture the entirety of the construct measured. We used validated and well-recognized dietary and PA questionnaires. Nevertheless, as in any study investigating dietary and PA behavior, misclassification, recall, and social desirability biases are potential limitations51,52. The use of a monitor-based PA measure, for example a pedometer, may have provided greater objectivity than self-report, but was not feasible. Although we used validated dietary and PA questionnaires, the PA levels and fruit/vegetable intake were also based on self-report and could have overestimated concordance between these exposures and self-perceptions. Limitations in the available data prevented an assessment of associations between prior dietitian counseling encounters and patients’ self-perceptions. The study population was representative of a safety net outpatient hepatology clinic in Texas, and predominantly, immigrant, Hispanic and lower than high school educational attainment and representative. We recognize that these characteristics limit the generalizability of this study’s finding; at the same time, the study population represents a high risk NAFLD population, understudied in the field of NAFLD, and are important to target with improved dietary interventions.
Future directions
There is a pressing need for more research addressing the determinants of behavioral change in patients with NAFLD; to date, only eight papers on the topic have been published53,54,55,56,57,58,59,60. This study was a focused investigation into the rates and predictors of one behavioral determinant- self-perception- among patients with NAFLD, prior to receiving specialty care in a hepatology clinic. Our exploratory analysis describing the relationship between baseline concordance and follow up weight loss, as a proxy for behavioral change, was limited by sample size. However, given the complexity of behavioral change, we do not expect that concordance in self-perception, alone, will be predictive of weight loss. Therefore, future studies should examine additional behavioral determinants—for example self-efficacy, perceived barriers, and/or outcome expectations—in patients with NAFLD and how they associate with behavioral change over time. In addition, more proximal behavioral outcomes, such as dietary change or increases in physical activity, should be assessed.
Conclusion
In summary, while most patients with NAFLD accurately self-recognize their weight status, approximately one-third do not recognize inadequate dietary or PA behaviors. A diagnosis of NAFLD may represent a catalyst for behavior change among patients who are overweight/obese and/or have features of the metabolic syndrome. Recent international collaborative efforts on renaming NAFLD as metabolic associated fatty liver disease (MAFLD) is potentially a step in this direction by reframing the liver disease as a consequence of systemic metabolic dysfunction61. In addition to helping patients better understand their liver disease, promoting weight loss and healthy behaviors among patients with NAFLD/MAFLD requires well-designed interventions. Our findings provide a starting point for assessing patients’ readiness for behavioral change and key areas to target in NAFLD/MAFLD-specific behavioral modification programs.
References
Wong, R. J. et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 148(3), 547–555 (2015).
Makarova-Rusher, O. V. et al. Population attributable fractions of risk factors for hepatocellular carcinoma in the United States. Cancer 122(11), 1757–1765 (2016).
Younossi, Z. M. et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009. Hepatology 62(6), 1723–1730 (2015).
Stepanova, M. & Younossi, Z. M. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin. Gastroenterol. Hepatol. 10(6), 646–650 (2012).
Friedman, S. L., Neuschwander-Tetri, B. A., Rinella, M. & Sanyal, A. J. Mechanisms of NAFLD development and therapeutic strategies. Nat. Med. 24(7), 908–922 (2018).
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64(1), 73–84 (2016).
Balakrishnan M, Patel P, Dunn-Valadez S, et al. Women have lower risk of nonalcoholic fatty liver disease but higher risk of progression vs men: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. (2020).
Keating, S. E., Hackett, D. A., George, J. & Johnson, N. A. Exercise and non-alcoholic fatty liver disease: A systematic review and meta-analysis. J. Hepatol. 57(1), 157–166 (2012).
Vilar-Gomez, E. et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology 149(2), 367–378 (2015).
Marchesini, G., Petta, S. & Dalle, G. R. Diet, weight loss, and liver health in nonalcoholic fatty liver disease: Pathophysiology, evidence, and practice. Hepatology 63(6), 2032–2043 (2016).
Chalasani, N. et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67(1), 328–357 (2018).
Marshall, S. J. & Biddle, S. J. The transtheoretical model of behavior change: A meta-analysis of applications to physical activity and exercise. Ann. Behav. Med. 23(4), 229–246 (2001).
Prochaska, J. O., Redding, C. A. & Evers, K. E. The transtheoretical model and stages of change. In Health behavior: Theory, research, and practice 5th edn (eds Glanz, K. et al.) 125–148 (John Wiley & Sons, Inc, 2015).
Rich, N. E. et al. Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the United States: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 16(2), 198–210 (2018).
Dorsey, R. R., Eberhardt, M. S. & Ogden, C. L. Racial and ethnic differences in weight management behavior by weight perception status. Ethn. Dis. 20(3), 244 (2010).
Kuchler, F. & Variyam, J. N. Mistakes were made: misperception as a barrier to reducing overweight. Int. J. Obes. 27(7), 856–861 (2003).
Cui, Z. et al. Prediction of body mass index using concurrently self-reported or previously measured height and weight. PLoS ONE 11(11), 7288 (2016).
Lemon, S. C. et al. Municipal officials’ participation in built environment policy development in the United States. Am. J. Health Promot. 30(1), 42–49 (2015).
Langellier, B. A., Glik, D., Ortega, A. N. & Prelip, M. L. Trends in racial/ethnic disparities in overweight self-perception among US adults, 1988–1994 and 1999–2008. Public Health Nutr. 18(12), 2115–2125 (2015).
Ahluwalia, I. B., Ford, E. S., Link, M. & Bolen, J. C. Acculturation, weight, and weight-related behaviors among Mexican Americans in the United States. Ethn. Dis. 17(4), 643 (2007).
DeSalvo, K. B., Olson, R. & Casavale, K. O. Dietary guidelines for Americans. JAMA 315(5), 457–458 (2016).
Piercy, K. L. et al. The physical activity guidelines for Americans. JAMA 320(19), 2020–2028 (2018).
Babor, T.F., Higgins-Biddle, J.C., Saunders, J.B., & Monteiro, M.G. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care. World Health Organization (2001).
World Health Organization. Obesity: Preventing and managing the global epidemic: Report of a WHO consultation 9241208945 (World Health Organization, 2000).
Topolski, T. D. et al. Peer reviewed: The Rapid Assessment of Physical Activity (RAPA) among older adults. Prev. Chronic. Dis. 3(4), 1 (2006).
Vega-López, S., Chavez, A., Farr, K. J. & Ainsworth, B. E. Validity and reliability of two brief physical activity questionnaires among Spanish-speaking individuals of Mexican descent. BMC. Res. Notes 7(1), 29 (2014).
American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription 10th edn. (Lippincott Williams & Wilkins, 2017).
Smith, T. M. et al. Using secondary 24-hour dietary recall data to estimate daily dietary factor intake from the FLASHE study dietary screener. Am. J. Prev. Med. 52(6), 856–862 (2017).
U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. December 2015.
National Cancer Institute. 2014 Family Life, Activity, Sun, Health and Eating (FLASHE) Survey Data. In. Rockville, MD: U.S. Department of Health and Human Services, National Cancer Institute.
Gleason, P., Rangarajan, A., Olson, C.M. Dietary intake and dietary attitudes among food stamp participants and other low-income individuals. Mathematica Policy Research, Incorporated (2000).
Obayashi, S., Bianchi, L. J. & Song, W. O. Reliability and validity of nutrition knowledge, social-psychological factors, and food label use scales from the 1995 Diet and Health Knowledge Survey. J. Nutr. Educ. Behav. 35(2), 83–92 (2003).
Capps, O., Cleveland, L. & Park, J. Dietary behaviors associated with total fat and saturated fat intake. J. Am. Diet. Assoc. 102(4), 490–502 (2002).
U.S. Department of Agriculture ARS. Diet and Health Knowledge Survey 1994–1996. https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/csfii-1994-1996-1998-and-dhks-1994-1996/. Accessed May 18 2015.
Oppen, M., Sugerman, S., & Foerster, S. Fruit and vegetable consumption in California adults: Ten-year highlights from the california dietary practices surveys 1989–1999. In Sacramento, CA: California Department of Health Services, Cancer Prevention and Nutrition Section (2002).
Johns DJ, Hartmann-Boyce J, Jebb SA, Aveyard P, Group BWMR. Diet or exercise interventions vs combined behavioral weight management programs: A systematic review and meta-analysis of direct comparisons. J. Acad. Nutr. Diet. 114(10), 1557–1568 (2014).
Jansink, R. et al. Misperception of patients with type 2 diabetes about diet and physical activity, and its effects on readiness to change. J. Diabetes 4(4), 417–423 (2012).
Liver EAftSot, Diabetes EAftSo. EASL-EASD-EASO Clinical practice guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 64(6), 1388–1402 (2016).
Eslam, M. et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol. Int. 1, 1–31 (2020).
Bamia, C. et al. Fruit and vegetable consumption in relation to hepatocellular carcinoma in a multi-centre, European cohort study. Br. J. Cancer 112(7), 1273–1282 (2015).
Yang, Y. et al. Increased intake of vegetables, but not fruit, reduces risk for hepatocellular carcinoma: A meta-analysis. Gastroenterology 147(5), 1031–1042 (2014).
Akhlaghi, M., Ghasemi-Nasab, M. & Riasatian, M. Mediterranean diet for patients with non-alcoholic fatty liver disease, a systematic review and meta-analysis of observational and clinical investigations. J. Diabetes Metab. Disord. 19(1), 575–584 (2020).
Guveli, H., Kenger, E. B., Ozlu, T., Kaya, E. & Yilmaz, Y. Macro-and micronutrients in metabolic (dysfunction) associated fatty liver disease: Association between advanced fibrosis and high dietary intake of cholesterol/saturated fatty acids. Eur. J. Gastroenterol. Hepatol. 33, 390 (2021).
Vos, M. B. & Lavine, J. E. Dietary fructose in nonalcoholic fatty liver disease. Hepatology 57(6), 2525–2531 (2013).
Lim, J. S., Mietus-Snyder, M., Valente, A., Schwarz, J.-M. & Lustig, R. H. The role of fructose in the pathogenesis of NAFLD and the metabolic syndrome. Nat. Rev. Gastroenterol. Hepatol. 7(5), 251 (2010).
Jiao, J. et al. Cirrhosis and advanced fibrosis in Hispanics in Texas: The dominant contribution of central obesity. PLoS ONE 11(3), 1 (2016).
Gardner, R. M. Weight status and the perception of body image in men. Psychol. Res. Behav. Manag. 7, 175 (2014).
Balakrishnan, M., Kanwal, F., El-Serag, H. B. & Thrift, A. P. Acculturation and nonalcoholic fatty liver disease risk among hispanics of mexican origin: Findings from the National Health and Nutrition Examination Survey. Clin. Gastroenterol. Hepatol. 15(2), 310–312 (2017).
Crespo, C. J., Smit, E., Carter-Pokras, O. & Andersen, R. Acculturation and leisure-time physical inactivity in Mexican American adults: results from NHANES III, 1988–1994. Am. J. Public Health. 91(8), 1254–1257 (2001).
Abraido-Lanza, A. F., Chao, M. T. & Florez, K. R. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc. Sci. Med. 61(6), 1243–1255 (2005).
Adams, S. A. et al. The effect of social desirability and social approval on self-reports of physical activity. Am. J. Epidemiol. 161(4), 389–398 (2005).
Prince, S. A. et al. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 5(1), 56 (2008).
Centis, E. et al. Stage of change and motivation to healthier lifestyle in non-alcoholic fatty liver disease. J. Hepatol. 58(4), 771–777 (2013).
Dhaliwal, H. S. et al. Perception of illness and its association with treatment willingness in patients with newly diagnosed nonalcoholic fatty liver disease. Dig. Dis. Sci. 66, 1–11 (2021).
Frith, J. et al. Potential strategies to improve uptake of exercise interventions in non-alcoholic fatty liver disease. J. Hepatol. 52(1), 112–116 (2010).
Heredia, N.I., Thrift, A.P., & Balakrishnan, M. Perceived barriers to weight loss among hispanic patients with non-alcoholic fatty liver disease. Hisp. Health Care Int. 15404153211043885 (2021).
O’Gorman, P. et al. Determinants of physical activity engagement in patients with nonalcoholic fatty liver disease: The need for an individualized approach to lifestyle interventions. Phys. Ther. 101(2), 195 (2021).
Stewart, K. E. et al. Readiness for behaviour change in non-alcoholic fatty liver disease: Implications for multidisciplinary care models. Liver Int. 35(3), 936–943 (2015).
Stine, J. G. et al. Breaking down barriers to physical activity in patients with nonalcoholic fatty liver disease. Dig. Dis. Sci. 1, 1–8 (2020).
Zelber-Sagi, S. et al. Role of illness perception and self-efficacy in lifestyle modification among non-alcoholic fatty liver disease patients. World J. Gastroenterol. 23(10), 1881 (2017).
Eslam, M. et al. A new definition for metabolic associated fatty liver disease: An international expert consensus statement. J. Hepatol. 1, 1 (2020).
Acknowledgements
We thank Gary Deyter for his editorial assistance.
Funding
This work was supported in part by National Institutes of Health grant P30 DK056338, which supports the Texas Medical Center Digestive Diseases Center. N.H. was supported, in part, by the Cancer Prevention and Research Institute of Texas (RP170259) and MD Anderson's Cancer Center Support Grant (CA016672) funded by the National Cancer Institute. F.K. is a core investigator at the Center for Innovations in Quality, Effectiveness and Safety (CIN 13–413), Michael E. DeBakey VA Medical Center, Houston, TX.
Author information
Authors and Affiliations
Contributions
N.H.: analysis, results interpretation, manuscript writing; Y.L.: data analysis; S.J., R.G., M.R., M.R.: data collection; H.E.S., F.K.: results interpretation, manuscript editing; A.P.T.: data collection, analysis, results interpretation, manuscript editing and critical revision for intellectual content; M.B.: study conception and design, data collection, analysis, manuscript writing, editing and critical revision for intellectual content, study supervision. All authors approved the final draft submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heredia, N.I., Gaba, R., Liu, Y. et al. Perceptions of weight status and energy balance behaviors among patients with non-alcoholic fatty liver disease. Sci Rep 12, 5695 (2022). https://doi.org/10.1038/s41598-022-09583-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-09583-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.