Abstract
This study was aimed to compare the risk of pneumonia between patients with chronic rhinosinusitis (CRS) and those without CRS (control) in a Korean population. The population aged 40 years or over was included from the Korean National Health Insurance Service-Health Screening Cohort. Participants with CRS (n = 6393) and controls (n = 25,572) were selected by 1:4 matching for age, sex, income, region of residence, and history of pneumonia for the previous 1 year. The index date (ID) of the controls was set as the treatment date of their matched CRS participants. The incidence of pneumonia after the ID was measured from 2003 to 2015. Simple and multiple linear regressions were performed to calculate estimated values (EVs) and 95% confidence intervals (CIs) for 1-y post-ID pneumonia, 2-y post-ID pneumonia, and 3-y post-ID pneumonia in CRS participants compared to controls. Statistical significance was noted in the 3-y post-ID period (EV = 0.017, 95% CI = 0.002–0.031, P = 0.030). In the subgroup analyses according to age and sex, statistical significance was seen in the younger age group (< 60 years old) in the 3-y post-ID period and in the female group in the 1-y and 3-y post-ID periods. This study revealed an increased risk for pneumonia following a diagnosis of CRS.
Similar content being viewed by others
Introduction
Pneumonia is a form of acute respiratory infection caused by viruses, bacteria, and fungi and a major cause of morbidity and mortality globally. According to the World Health Organization (WHO)’s 2019 Global Health Estimates, pneumonia and other lower respiratory infections were ranked as the fourth leading cause of death and disability-adjusted life years1. In Korea, deaths due to pneumonia have continued to increase since 2000, and in 2019, the death rate for pneumonia stood at 45.1 per 100,000 population, ranking as the third leading cause of deaths2. In a recent study in Korea, the hospitalization rate due to bacterial pneumonia was reported to be 161.5 per 10,000 population over the age of 653. Several risk factors, such as diabetes, cardiovascular disease, smoking, asthma, and chronic obstructive pulmonary disease (COPD), have been shown to increase the likelihood of the development of pneumonia4.
Chronic rhinosinusitis (CRS) is a chronic upper airway inflammation that can greatly influence the health-related quality of life of patients and the socioeconomic burden5. Several epidemiological studies have shown that CRS is associated with lower airway diseases such as asthma6, bronchiectasis7, and COPD8. This interdependence of the upper and lower respiratory tracts has led to the concept of the “unified airway”, which considers the upper and lower airways to be a single functional unit9.
Despite the correlations between the upper and lower airways, few studies have evaluated the association of CRS and pneumonia. A retrospective study using X-ray findings reported that the frequency of sinusitis was found to be 84% among patients with pneumonia10. A previous study in the U.S. showed an association between community-acquired pneumonia and CRS with sphenoid involvement (odds ratio [OR] = 19.76, 95% confidence interval [CI] = 8.78–44.47)11. Furthermore, population-based studies evaluating the risk of pneumonia in patients with CRS are lacking.
This study aimed to compare the incidence of pneumonia between patients with CRS and those without CRS (control) using a national sample cohort from the Korean population. An understanding of the association between CRS and pneumonia will contribute to disease prevention.
Results
Table 1 shows the general characteristics of the participants. Age, sex, income, region of residence, and 1-y pre-index date (ID) pneumonia showed no difference between the CRS and control groups due to matching (standardized difference = 0.00). Total cholesterol level, systolic blood pressure (SBP)/diastolic blood pressure (DBP), fasting glucose level, obesity, smoking status, alcohol consumption, and Charlson Comorbidity Index (CCI) scores were similar in the CRS total group and controls (standardized difference < 0.20), while the prevalence rates of asthma and COPD were different between the two groups (standardized difference ≥ 0.20).
The adjusted estimated value (EV) of the incidence of post-ID pneumonia did not reach statistical significance at 1-y (P = 0.059) and 2-y (P = 0.310) post-ID. However, the adjusted EV showed statistical significance at 3-y post-ID (EV = 0.017, 95% CI = 0.002–0.031, P = 0.030) (Table 2).
In the subgroup analyses according to age and sex, statistical significance was seen in the younger age group (< 60 years old) at 3-y post-ID (EV = 0.025, 95% CI = 0.011–0.038, P < 0.001) and the female group at the 1-y (EV = 0.037, 95% CI = 0.012–0.062, P = 0.004) and 3-y (EV = 0.022, 95% CI = 0.000–0.044, P = 0.046) post-ID periods (Table 2).
When analyzing the CRS with nasal polyps (CRSwNP) (Table 3) and CRS without nasal polyps (CRSsNP) (Table 4) groups separately, an association between CRS and pneumonia was found in the 1-y (EV = 0.035, 95% CI = 0.010–0.060, P = 0.007) and 3-y (EV = 0.037, 95% CI = 0.014–0.061, P = 0.002) post-ID periods in the CRSsNP group only.
Discussion
This study showed the association between CRS and pneumonia. This association was seen only in the younger age, female sex, and CRSsNP subgroups.
The concept of “united airway disease” or “one linked airway disease” has emerged, and allergic rhinitis, sinusitis, and asthma are expressed in different parts of the respiratory tract as one pathological process that is inflammatory in nature12. In addition, the concept has expanded beyond asthma, and an association with CRS has been reported in other lung diseases, including bronchiectasis7,13 and COPD8. In a systematic review, the pooled prevalence of CRS in adults with bronchiectasis was 62%, and CRS was associated with a greater degree of bronchiectasis severity, poorer quality of life, reduction in olfactory detection, and elevated levels of inflammatory markers7. A large retrospective study in a U.S. population found that almost half of the patients with bronchiectasis had comorbid CRS13. In a Taiwanese population-based study, COPD was associated with CRSsNP8.
On the other hand, there have been few studies on the association between CRS and pneumonia. Previous studies have mainly reported the incidence of sinusitis and pneumonia in intensive care unit (ICU) patients14,15,16. A meta-analysis on ventilator-associated sinusitis showed that 41% of patients with ICU-derived sinusitis also developed hospital-acquired pneumonia17. They showed that the same pathogen was isolated from culture specimens of the lung and sinuses in 59% of patients17. However, few studies have evaluated the association of CRS and pneumonia in the general population.
We hypothesize that there are several possible mechanisms underlying the association between CRS and pneumonia. First, the nasal cavities constitute the first barrier of the whole airway system that has immunological functions against bacteria, viruses, and other pathogens. Several studies have indicated that CRS is associated with a failure of the mechanical and immunological barriers across the nasal mucosa18,19. Furthermore, patients with CRS have been shown to have impaired mucociliary function20, which increases susceptibility to respiratory infections21. Second, there is biological plausibility for a relationship between CRS and pneumonia. Haemophilus influenzae, Moraxella catarrhalis, and Streptococcus pneumoniae are the primary respiratory tract pathogens involved in both acute and chronic rhinosinusitis22. Staphylococcus aureus, S. epidermidis, and anaerobic Gram-negative bacteria predominate in CRS23. Moreover, these are the main causative pathogens of community-acquired and hospital-acquired pneumonia24. Third, the effectiveness of the pneumococcal vaccination may be reduced in patients with CRS. CRS is known to be one of the most common manifestations of humoral immunodeficiency25. Specific antibody deficiency (SAD) is a primary immune deficiency associated with a qualitative defect in antibody function. SAD is defined as a poor antibody response to polysaccharide antipneumococcal vaccine, such as Pneumovax®, in the presence of recurrent or chronic sinopulmonary infections26. A meta-analysis reported a high prevalence of humoral immune deficiency in CRS, with 8–34% of subjects diagnosed with SAD27. Last, an increase in cytokines induced by CRS-related inflammation may promote systemic inflammation, including in the lung. However, it is necessary to determine whether CRS directly causes pneumonia, or whether both diseases are simply different manifestations of common pathophysiology.
The association between CRS and pneumonia was seen only in the younger age, female sex, and CRSsNP subgroups. Since the risk of pneumonia increases with age and the presence of comorbidities24,28, the effects of other risk factors, such as CRS, may be emphasized in the younger age group. A study showing increased odds of having community-acquired pneumonia in CRS with severe sphenoid involvement attributed this association to the posterior location with the possibility of postnasal drainage into the lower respiratory tract11. One of the explanations for the linkage between the upper and lower airways includes postnasal drainage of inflammatory material into the lower airway. A previous study evaluating sex-specific differences in CRS patients showed that women reported more problems with postnasal drainage than men29. While CRSwNP is characterized by eosinophil-related inflammation, Asian CRSsNP patients show prominent neutrophil-related inflammation30. Although neutrophils are essential components of the immune response to pulmonary infection, they can also be harmful to host tissue. Excessive neutrophil activation results in severe tissue damage as a result of the exacerbated release of toxic agents, including proteinases, cationic polypeptides, cytokines, and reactive oxygen species31. However, further studies may be required to clarify the pathophysiology behind this finding.
The present study has some limitations. First, the incidence of pneumonia was relatively low and there may be potential for diagnostic misclassification. However, in Korea, the National Health Insurance system covers almost the entire population and is characterized by cost effectiveness and easy access to medical institutions. Given the distinct clinical characteristics of lower respiratory tract infection, misclassification of patients with signs and symptoms of pneumonia into the nonpneumonic diagnostic category is unlikely32. Second, there was a possibility of unadjusted covariates because there were no data about pneumococcal vaccination, details of medication use such as corticosteroid or antibiotics, immunosuppression status, atopy, and allergies. However, we adjusted for several confounding factors, including asthma, COPD, and other comorbidities that could affect the risk of pneumonia. We used CCI, which is widely used to classify various comorbid conditions and underlying diseases, including diabetes, renal failure, any malignancy, and AIDS/HIV33. Third, the incidence rates of community-acquired and hospital-acquired pneumonia cannot be investigated separately. Nevertheless, the strength of this study is that it is a population-based study that revealed the relationship between CRS and pneumonia.
In conclusion, CRS patients were more likely to have pneumonia. Physicians should be aware of the possible risk of pneumonia in patients with CRS.
Materials and methods
Study population
We used data from the Korean National Health Insurance Service-Health Screening Cohort for this study, and a comprehensive explanation for this cohort is provided elsewhere34. This study was performed in accordance with relevant guidelines/regulations and approved by the Institutional Review Board (IRB) of Hallym University (IRB No: 2019-10-023). The need for written informed consent was waived due to its minimal risk involved in the retrospective analysis.
Participant selection
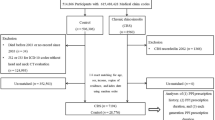
Among the 514,866 participants with 615,488,428 medical claim codes, participants were selected as the CRS total group (n = 8,560) according to the definition in our previous study35. Participants without a history of CRS were selected as a control group (n = 506,306). Participants in the CRS total group who diagnosed with CRS in 2002 were removed (n = 1,366) to calculate the history of pneumonia from the date of first diagnosis of CRS (ID) to the date 1 year prior (pre-ID pneumonia for 1 year). In the control group, participants who died before 2003 or had no records after 2003 (n = 34) and those diagnosed with J32 (chronic rhinosinusitis) or J33 (nasal polyps) using the ICD-10 code at least once (n = 124,993) were excluded. If the participants were treated for the first time from 2013 to 2015, they were excluded from the CRS total group to count the diagnosis of pneumonia for 3 years following the ID (n = 801). The participants with CRS were 1:4 matched with the controls for age, sex, income, and region of residence. The CRS total and control groups were additionally matched by pneumonia incidence for 1 year pre-ID (0 times; ≥ 1 time). To minimize selection bias, the controls were selected with random number order. The ID of the controls was set as the ID of their matched participant with CRS. Therefore, each CRS participant and his or her matched controls had the same ID. During the matching process, 355,707 control participants were excluded. Finally, 6,393 of the total CRS participants were 1:4 matched with 25,572 control participants. Additionally, the final selected participants were classified into CRSwNP (n = 3,304) with matched controls (n = 13,216) and CRSsNP (n = 3,089) with matched controls (n = 12,356) (Fig. 1).
A schematic illustration of the participant selection process that was used in the present study. Of a total of 514,866 participants, 6,393 of the total CRS participants were matched with 25,572 control participants for age, sex, income, region of residence, and pneumonia for 1 year prior to the index date. Additionally, the final participants were further classified into two groups: CRS with nasal polyps (n = 3,304) with matched controls (n = 13,216) and CRS without nasal polyps (n = 3,089) with matched controls (n = 12,356).
Chronic rhinosinusitis (Exposure)
CRS with/without nasal polyps were defined using ICD-10 codes (J32, chronic sinusitis; J33, nasal polyp) and head and neck computed tomography evaluations following our previous study35, 36.
Pneumonia (Outcome)
Pneumonia was identified based on ICD-10 codes (J12 to J18). Patients with these codes, who underwent chest X-ray (claim codes: G2101-G2105, G2111, G2112, G2121, G2201, G2301-G2305, G2322) or chest CT (claim codes: HA424, HA434, HA444, HA454, HA464, HA474) were defined as having pneumonia. Pneumonia for 1 year period pre-ID was categorized as 0 times and ≥ 1 time. The number of pneumonia diagnoses was counted from the ID to the date after the first year period (1-y post-ID pneumonia), second year period (2-y post-ID pneumonia), and third year period (3-y post-ID pneumonia).
Covariates
Age groups were divided by 5-year intervals into 10 groups. Income groups were classified into 5 classes (class 1 [lowest income] – 5 [highest income]). The region of residence was grouped into urban and rural areas according to our previous study37. Tobacco smoking, alcohol consumption, and obesity were categorized in the same way as in our previous study38. Total cholesterol (mg/dL), SBP (mmHg), DBP (mmHg), and fasting blood glucose (mg/dL) were measured. The CCI39 score ranged from 0 (no comorbidities) to 29 (multiple comorbidities) except for COPD. Asthma and COPD were defined following our previous studies40, 41.
Statistical analyses
The general characteristics of the CRS total and control groups were compared using standardized differences. Simple and multiple linear regressions were analyzed to calculate estimated values and 95% CIs for 1-y post-ID pneumonia, 2-y post-ID pneumonia, and 3-y post-ID pneumonia in the CRS total, CRSwNP, and CRSsNP groups compared to each matched control group. Both simple and multiple linear regressions were stratified by age, sex, income, and region of residence. In multiple linear regression, we used 2 models for analyses. Model 1 was adjusted for obesity, smoking status, alcohol consumption, total cholesterol, SBP, DBP, fasting blood glucose, CCI score, asthma history, and COPD history. Model 2 was adjusted for model 1 plus 1-y pre-ID pneumonia. For the subgroup analyses, we divided participants by age (< 60 years old and ≥ 60 years old) and sex (males and females). Simple and multiple linear regressions were calculated. All analyses were two tailed, and significance was defined as P-values less than 0.05. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses.
Data availability
Data in this study were from the Korean National Health Insurance Service-Health Screening Cohort. Releasing of the data by the researcher is not allowed legally. All of data are available from the database of National Health Insurance Sharing Service (NHISS) (https://nhiss.nhis.or.kr/). NHISS allows all data for any researcher who promises to follow the research ethics with some cost. If you want to access the data of this article, you could download it from the website after promising to follow the research ethics.
References
World Health Organization. Global Health Estimates. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates (2019).
Statistics Korea. Causes of Death Statistics in 2019. http://kostat.go.kr/portal/eng/pressReleases/8/10/index.board?bmode=read&aSeq=385629&pageNo=&rowNum=10&amSeq=&sTarget=&sTxt= (2020).
Kim, A. M., Kang, S., Park, J. H., Yoon, T. H. & Kim, Y. A spatial analysis of geographic variation and factors associated with hospitalization for bacterial pneumonia in Korea. BMC Pulm. Med. 19, 1–8 (2019).
Torres, A., Blasi, F., Dartois, N. & Akova, M. Which individuals are at increased risk of pneumococcal disease and why? Impact of COPD, asthma, smoking, diabetes, and/or chronic heart disease on community-acquired pneumonia and invasive pneumococcal disease. Thorax 70, 984–989 (2015).
Metson, R. B. & Gliklich, R. E. Clinical outcomes in patients with chronic sinusitis. Laryngoscope 110, 24–28 (2000).
Pan, Y. & Zang, H. Association of chronic rhinosinusitis with bronchial asthma and its severity: a protocol for systematic review and meta-analysis. Medicine 100, e24772 (2021).
Handley, E., Nicolson, C. H., Hew, M. & Lee, A. L. Prevalence and clinical implications of chronic rhinosinusitis in people with bronchiectasis: a systematic review. J. Allergy Clin. Immunol. Pract. 7, 2004-2012. e2001 (2019).
Chien, C.-Y., Tai, S.-Y., Wang, L.-F. & Lee, C.T.-C. Chronic obstructive pulmonary disease predicts chronic rhinosinusitis without nasal polyps: a population-based study. Am. J. Rhinol. Allergy 29, e75–e80 (2015).
Krouse, J. H. The unified airway—conceptual framework. Otolaryngol. Clin. North Am. 41, 257–266 (2008).
Özbay, B. & Arslan, H. Frequency of sinusitis in the patients with pneumonia. Clin. Imaging 26, 92–94 (2002).
McQuitty, R., Bui, R. & Chaaban, M. R. Retrospective study: association of chronic sphenoid rhinosinusitis with community acquired pneumonia. Am. J. Rhinol. Allergy 33, 751–756 (2019).
Grossman, J. One airway, one disease. Chest 111, 11S-16S (1997).
Somani, S. N. et al. Prevalence and characterization of chronic rhinosinusitis in patients with non-cystic fibrosis bronchiectasis at a tertiary care center in the United States. Int Forum Allergy Rhinol. 9, 1424–1429 (2019).
Huyett, P., Rowan, N. R., Ferguson, B. J., Lee, S. & Wang, E. W. The relationship of paranasal sinus opacification to hospital-acquired pneumonia in the neurologic intensive care unit patient. J. Intensive Care Med. 34, 844–850 (2019).
Holzapfel, L. et al. A randomized study assessing the systematic search for maxillary sinusitis in nasotracheally mechanically ventilated patients: influence of nosocomial maxillary sinusitis on the occurrence of ventilator-associated pneumonia. Am. J. Respir. Crit. Care Med. 159, 695–701 (1999).
Holzapfel, L. et al. Influence of long-term oro-or nasotracheal intubation on nosocomial maxillary sinusitis and pneumonia: results of a prospective, randomized, clinical trial. Crit. Care Med. 21, 1132–1138 (1993).
Agrafiotis, M., Vardakas, K. Z., Gkegkes, I. D., Kapaskelis, A. & Falagas, M. E. Ventilator-associated sinusitis in adults: systematic review and meta-analysis. Respir. Med. 106, 1082–1095 (2012).
Kern, R. C. et al. Perspectives on the etiology of chronic rhinosinusitis: an immune barrier hypothesis. Am. J. Rhinol. 22, 549–559 (2008).
Pothoven, K. L. et al. Oncostatin M promotes mucosal epithelial barrier dysfunction, and its expression is increased in patients with eosinophilic mucosal disease. J. Allergy Clin. Immunol. 136, 737–746734 (2015).
Gudis, D., Zhao, K.-Q. & Cohen, N. A. Acquired cilia dysfunction in chronic rhinosinusitis. Am. J. Rhinol. Allergy 26, 1–6 (2012).
Kuek, L. E. & Lee, R. J. First contact: the role of respiratory cilia in host-pathogen interactions in the airways. Am. J. Physiol. Lung Cell. Mol. Physiol. 319, L603–L619 (2020).
Gwaltney, J. M. Jr., Scheld, W. M., Sande, M. A. & Sydnor, A. The microbial etiology and antimicrobial therapy of adults with acute community-acquired sinusitis: a fifteen-year experience at the University of Virginia and review of other selected studies. J. Allergy Clin Immunol 90, 457–462 (1992).
Brook, I. Microbiology of chronic rhinosinusitis. Eur. J. Clin. Microbiol. Infect. Dis. 35, 1059–1068 (2016).
Lanks, C. W., Musani, A. I. & Hsia, D. W. Community-acquired pneumonia and hospital-acquired pneumonia. Med. Clin. 103, 487–501 (2019).
Keswani, A. et al. The clinical significance of specific antibody deficiency (SAD) severity in chronic rhinosinusitis (CRS). J. Allergy Clin. Immunol Pract. 5, 1105–1111 (2017).
Fried, A. J. & Bonilla, F. A. Pathogenesis, diagnosis, and management of primary antibody deficiencies and infections. Clin. Microbiol. Rev. 22, 396–414 (2009).
Schwitzguébel, A.J.-P., Jandus, P., Lacroix, J.-S., Seebach, J. D. & Harr, T. Immunoglobulin deficiency in patients with chronic rhinosinusitis: Systematic review of the literature and meta-analysis. J. Allergy Clin. Immunol. 136, 1523–1531 (2015).
Millett, E. R., Quint, J. K., Smeeth, L., Daniel, R. M. & Thomas, S. L. Incidence of community-acquired lower respiratory tract infections and pneumonia among older adults in the United Kingdom: a population-based study. PLoS ONE 8, e75131 (2013).
Lal, D., Rounds, A. B. & Divekar, R. in International forum of allergy & rhinology. 278–286 (Wiley Online Library).
Kim, D. W., Eun, K. M., Roh, E. Y., Shin, S. & Kim, D.-K. Chronic rhinosinusitis without nasal polyps in Asian patients shows mixed inflammatory patterns and neutrophil-related disease severity. Mediators Inflamm. 2019, 7138643 (2019).
Pechous, R. D. With friends like these: the complex role of neutrophils in the progression of severe pneumonia. Front. Cell. Infect. Microbiol. 7, 160 (2017).
Ives, D. G., Samuel, P., Psaty, B. M. & Kuller, L. H. Agreement between nosologist and cardiovascular health study review of deaths: implications of coding differences. J. Am. Geriatr. Soc. 57, 133–139 (2009).
Quan, H. et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 43, 1130–1139 (2005).
Seong, S. C. et al. Cohort profile: the national health insurance service-national health screening cohort (NHIS-HEALS) in Korea. BMJ Open 7, e016640 (2017).
Wee, J. H. et al. Association between Dyslipidemia and Chronic Rhinosinusitis in a Korean Population. Diagnostics 11, 26 (2021).
Choi, H. G. & Lee, H. J. Increased risk of psoriasis in patients with chronic rhinosinusitis without nasal polyps: a longitudinal follow-up study using Korean national sample cohort. Eur. Arch. Otorhinolaryngol. 276, 3105–3111 (2019).
Kim, S. Y., Min, C., Oh, D. J. & Choi, H. G. Bidirectional association between GERD and asthma: two longitudinal follow-up studies using a national sample cohort. J. Allergy Clin. Immunol. Pract. 8, 1005-1013. e1009 (2020).
Kim, S. Y., Oh, D. J., Park, B. & Choi, H. G. Bell’s palsy and obesity, alcohol consumption and smoking: a nested case-control study using a national health screening cohort. Sci. Rep. 10, 1–8 (2020).
Quan, H. et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 173, 676–682 (2011).
Kim, S. Y., Oh, D. J. & Choi, H. G. Tonsillectomy does not reduce asthma in children: a longitudinal follow-up study using a national sample cohort. Sci. Rep. 9, 1–8 (2019).
Kim, S.-Y., Lee, C.-H., Yoo, D.-M., Min, C.-Y. & Choi, H.-G. Association between chronic obstructive pulmonary disease and ménière’s disease: a nested case-control study using a national health screening cohort. Int. J. Environ. Res. Public Health 18, 4536 (2021).
Acknowledgements
This study was supported by the research fund of National Research Foundation of Korea (Choi HG, grant number NRF-2021-R1C1C1004986; Wee JH, grant number NRF-2020-R1G1A1005390). The funding organization did not contribute to the design or conduct of this study, preparation, review, approval, or decision to submit this manuscript for publication.
Author information
Authors and Affiliations
Contributions
B.P. and H.G.C. conceived and designed the study. J.H.W., C.M., and H.J.J. performed the experiments. J.H.W. and C.M. analysed the data, wrote the paper, and drew all the figures in this manuscript. M.W.P., B.P., and H.G.C. critically revised and edited the paper. All authors have read and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wee, J.H., Min, C., Jung, H.J. et al. Association between chronic rhinosinusitis and pneumonia: a longitudinal follow-up study using a national health screening cohort. Sci Rep 12, 5498 (2022). https://doi.org/10.1038/s41598-022-09552-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-09552-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.