Abstract
Intraoperative parathyroid hormone dosage allows real-time monitoring of the decrease in PTH levels during parathyroidectomy and verify procedure’s efficacy. Currently, none of the interpretative criteria used has absolute accuracy. The aim of this study is to evaluate diagnostic accuracy of the Rome criterion verifying diagnostic significance of the individual assays. A total of 205 patients with primary hyperparathyroidism from a single adenoma were retrospectively evaluated and monitored with baseline PTH, PTH at 10 min and PTH at 20 min after adenoma excision. The accuracy of the latter two assays compared with baseline was compared by ROC curves. In addition, was evaluated the influence on these data of localization diagnostics (ultrasounds and scintigraphy), definitive histology, and type of surgery performed. The ratio of 20-min sampling to baseline in the Rome criterion showed highest diagnostic significance. This finding was not influenced by the type of surgery performed, definitive histologic examination, or intraoperative localization of the adenoma. The Rome criterion has shown its high reliability in detecting persistence. The ratio of sampling at 20 min to baseline is by far the best performing. Further studies are needed to evaluate whether sampling at 10 min after adenoma excision can be considered not mandatory.
Similar content being viewed by others
Introduction
The need of parathyroid hormone (PTH) value measurement during parathyroidectomy has been highlighted since the late 1980s1,2. In fact, although parathyroidectomy (PTx) is successfully in 90% of cases of primary hyperparathyroidism (HPT1), in 10% the calcemia and PTH values return or become elevated as a result of an unidentified or inaccessible adenoma, multiglandular disease, insufficient excision of hyperplastic glands, difficulty in distinguishing between adenomatous tissue and hyperplastic gland3. In 1993, Irvin et al. developed the rapid intraoperative PTH assay4,5. The Quick intact intraoperative parathormone assay (ioPTH) is a technique that allows real-time monitoring of the decline in plasma PTH levels as the glands are removed during PTx6,7. At present, a PTH threshold that can predict 100% of cases of a persistent/recurrent disease is not well defined8,9. Therefore, several interpretative models of the ioPTH curve have been proposed10. Among these, at our institution we have been adopting for more than a decade the Rome criterion, which is based on a drop > 50% of ioPTH values compared to the highest pre-excision values and/or ioPTH value within the reference threshold, and/or ≤ 7.5 ng/L lower than the value at 10 min post-excision, 20 min after excision11,12.
The introduction of ioPTH and the optimization of its interpretative models, together with the refinement of techniques for localization of pathological parathyroid glands have allowed the implementation of focused approach for PTx13,14 and the extension of surgical indications, with an overall improvement of treatment optimization, especially in terms of complications of HPT115. In addition, ioPTH may be a useful tool in difficult settings, such as concurrent thyroid disease or unlocalized parathyroid gland16,17.
Overall, the routine use of ioPTH is justified by the usefulness shown in decision making in HPT1 surgery18.
Despite the effectiveness of ioPTH in optimizing results in HPT1 surgery, this practice results in increased costs, given by the combination of the cost of instruments, consumables, and the time to devote to each analysis19. The last two items are directly proportional to the number of samples analysed in each procedure.
The aim of our study is to verify, in the context of a procedure monitored according to the Rome criterion, which requires at least three intraoperative samplings, which one correlates most closely with the cure of HPT1, and whether this result alone can be judged sufficiently accurate to make the other unnecessary.
Methods
Study population
The Rome criterion has been used almost systematically since 2010 at all Surgical Units of our Department; however, we excluded from the study patients treated in the 3-year period 2010–2012 because we considered this period necessary for the development and internal validation of the protocol.
The prospectively collected medical records of a retrospective cohort of patients undergoing PTx from 2013 to 2020 at the three Surgical Units of the Department of Surgical, Oncological and Oral Sciences of the Policlinico Universitario “P. Giaccone”of Palermo involved in the treatment of endocrine diseases was evaluated in this study. Our tertiary hospital is a referral center for the treatment of endocrine disorders. The volume of parathyroidectomies performed in the last decade at our department, can be defined as intermediate, although it collects the largest proportion of PTx performed in western Sicily20,21,22.
We excluded from the study patients with secondary or tertiary hyperparathyroidism, redo- surgery, Multiple Endocrine Neoplasia, patients with incomplete records, missing data and/or ioPTH monitoring not in agreement with standards of Rome criterion.
We also excluded cases with double adenoma, which we considered a confounding factor because the timing of the samples could not be interpreted according to the Rome criterion.
In all patients undergoing surgery, vitamin D values were previously corrected to within the normal range (30–100 ng/ml). Patients with vitamin D values below the normal range were not evaluated for the study.
Surgical techniques
The patients included in this study underwent three different surgical techniques: conventional bilateral exploration, minimally invasive video-assisted parathyroidectomy (both under general anesthesia), focused open minimally invasive parathyroidectomy (under local anesthesia).
Bilateral conventional exploration was preferred in cases of doubtful or absent localization, or in most cases where an intrathyroid site of the parathyroid was suspected. This technique was also employed in the presence of mediastinal scintigraphic uptake. It was performed with a 3.5–4 cm Kocher incision, preparation of flap below the platysma, and access to the thyroid beds bilaterally after separation of the strap muscles on the midline. MIVAP was preferred in the presence of a parathyroid with probable localization (clear US image or scintigraphy uptake), or certain (the two imaging techniques concordant), in this case if the parathyroid was a superior one (PIV), given its location deep in the neck and anterior to the recurrent nerve. In addition, this technique was preferred in cases of patients not compliant with local anesthesia. Some patients with intrathyroid parathyroid, suspected at US and confirmed at scintigraphy, underwent video-assisted hemithyroidectomy necessary to remove enlarged parathyroid gland.
The focused technique under local anesthesia was chosen in the presence of concordance of imaging techniques, for lower, superficial, non-mediastinal parathyroid glands, in consenting and compliant patients.
Intraoperative parathyroid hormone monitoring
The total intact PTH assay was performed with immunoradiometric assay (IRMA). The blood samples were processed at the hospital's centralized laboratory. This allowed for the best possible standardization on results across the three clinical institutions involved in patient recruitment.
Regardless of the surgical technique used, a PTH drop considered insufficient in both 10' and 20' sampling led to a continuation of the dissection and, in some cases, the conversion from a focused or minimally invasive technique to a conventional technique, generally aimed at bilateral exploration.
Data collection
The clinical records of 241 patients suffering from hyperparathyroidism, enrolled for surgery at the Department of our Department from 2013 to 2020 were examined. We excluded 9 patients with secondary or tertiary hyperparathyroidism, 7 patients because the ioPTH monitoring was not in agreement with standards of Rome criterion, 5 patients undergoing reoperation, who had undergone the first surgical procedure in another hospital, 4 patients with double parathyroid adenoma, 11 patients who presented incomplete records. After case selection according to the inclusion/exclusion criteria, a total of 205 patients were included in the study (Fig. 1).
Demographics (age, gender, and year of operation) were taken into account, as well as baseline PTH (range: 15–65 pg/ml), PTH values 10 min after PTx, and PTH values 20 min after PTx. We also recorded the surgical technique adopted, the results of imaging (US, scintigraphy), and the concordance of results between the two imaging techniques, as well as the definitive histological diagnosis.
Surgical treatment outcome was recorded as a dichotomous variable (cure/persistence). We considered persistence as the increase of PTH levels above the upper normal limit (> 65 pg/mL) with any calcemia values (normal range: 8.6–10.0 mg/dL) and vitamin D values above the threshold of sufficiency (> 30 ng/ml). PTH and calcemia were evaluated on the first postoperative day and 30 days after surgery. In the latter sample, vitamin D was also evaluated.
The variables were recorded on an excel spreadsheet.
Outcomes
The primary outcome of the study was the significance of the result of each postoperative PTH assay, compared with baseline sampling, in predicting cure or persistence.
We also evaluated whether the surgical technique adopted, the histology, or the localization imaging results could in any way influence the outcome.
Statistical analysis
In a first step, a univariate analysis was performed. Fisher's exact test for categorical variables and the Mann–Whitney test for continuous variables were applied.
Next, ROC curves were generated in order to evaluate the accuracy of changes in PTH (T10 minutes postoperative) or PTH (T20 minutes postoperative) relative to baseline PTH as a predictor of the occurrence of disease persistence. These percentage changes were derived through the following formulas:
A multivariate logistic analysis was performed in which the following variables were included: Age, Sex, PTHT10-baseline PTH Ratio, PTHT20-baseline PTH Ratio, PTHT20-PTHT10 Ratio, US, Scintigraphy, US + scintigraphy, and Localization.
In addition, the Mann–Whitney test was applied to evaluate a possible relationship between the continuous variable PTHT20-baseline PTH Ratio with the result of scintigraphy, the only variable to be significant in both univariate and multivariate analysis, to assess their possible interrelation.
Statistical analyses were performed with RStudio software (version 3.4.1 of 2017–06-30) for R (version 2.1) (25, 26). The application software "pROC" was used to generate ROC curves.
The present study involved uman participants and was conducted in conformity with ethical and human principles of research according to the ethical standards of the Declaration of Helsinki of 1964 and its amendments.
Informed consent was obtained from all individual participants included in the study according to format of "Società Italiana di Endocrinochirurgia" (SIEC), "Club delle Unità di Endocrinochirurgia" (UEC) and, from 2017, "Società Italiana Unitaria di Endocrinochirurgia" (SIUEC).
Ethical Board approval was obtained by "Comitato etico del Policlinico Paolo Giaccone—Palermo".
Results
From the univariate analysis, the variables that seem to be risk factors for disease persistence are: sex (males seem to be more at risk compared to females), PTH-T10, PTH-T20, US (negative), Scintigraphy (negative), US + Scintigraphy (not in accordance) and localization (intrathyroid parathyroid gland) (Table 1).
When comparing the three ROC Curves, we see that the decrease rate in PTH-T10 versus baseline PTH appears to be a moderately accurate predictor of disease persistence with AUC = 0.87 and 95% CI (0.79–0.95) with a cut-off value of -58,4%, Specificity = 0.66 95% CI (0.59–0.73) and Sensitivity = 1 with 95% CI (1–1); whereas the decrease rate in PTH-T20 compared to baseline PTH appears to be a highly accurate predictor of disease persistence with AUC = 0. 98 and 95% CI (0.92–0.99) with a cut-off value of − 63.5%, Specificity = 0.95 95% CI (0.92–0.98) and Sensitivity = 0.92 with 95% CI (0.77–1) (Fig. 2).
Calculation with ROC curves of the relationship between sensitivity and specificity of the PTH T10/baseline PTH, PTH T20/PTH T10, and PTH T20/baseline PTH ratios. The latter curve includes the area below with the greatest extension, demonstrating the greater diagnostic significance of this detection compared with the others, although these also showed excellent performance.
Finally, the decrease rate in PTH-T20 versus PTH-T10 (PTH ratio) turns out to be a highly accurate predictor of disease persistence with AUC = 0. 92 and 95% CI (0.84–0.97) with a cut-off value of − 35.5%, Specificity = 0.79, 95% CI (0.73–0.89) and Sensitivity = 0.92 with a 95% CI (0.77–1).
In multivariate logistic analysis, the following variables were included: Age, Sex, Baseline_PTH-T20_PTH ratio, Scintigraphy and Localization. The model revealed that the decrease rate PTH-T20—baseline PTH and scintigraphy are risk factors for disease persistence with OR and 95%IC of 1.124 95%IC (1.067–1.219) (p value < 0.05) and 30.87 95%IC (2.684–1.05e+03) (p value < 0.05), respectively (Table 2).
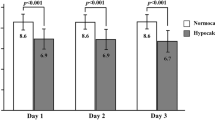
No correlation between categorical variables and the PTHT20-baseline PTH Ratio was shown. In particular, considering it reasonable to hypothesize a possible correlation between the outcome of scintigraphy (theoretically correlated in a directly proportional relationship to the metabolic activity of the parathyroid adenoma) and the extent of PTH decrease, we report in detail the relevant statistical evaluations. The groups of subjects with diagnostic scintigraphy (group 1) and those with non-diagnostic scintigraphy (group 2) were similar in terms of ratio (Fig. 3).
The indicators, for the two groups, were:
-
Group 1 M = − 79.38%; Median = − 82.00%; 1st Quartile = − 89.00%; 3rd Quartile = − 73.00%.
-
Group 2 M = − 74.93%; Median = − 80.00%; 1st Quartile = − 88.25%; 3rd Quartile = − 75.00%.
Discussion
Parathyroid surgery is considered a procedure whose strategic approach requires considerable specific expertise, especially in choosing the indication for surgery and the technique to use, as well as determining the extent of dissection3,8,22,23. The development of localization imaging has unquestionably improved the chances of correctly identifying hyperfunctioning parathyroid tissue2,3,13,23,24. IoPTH has attracted interest since its launch because of its capacity to validate, during the execution of surgery, the removal of all pathological parathyroid tissue or the incompleteness of the procedure4,5. In fact, the short half-life of PTH allows us to assess its kinetics in just a few minutes1,2,25. Standardized criteria for ioPTH monitoring have been proposed, but none of them has absolute diagnostic accuracy10,11,12. The criteria commonly suggested for the interpretation and application of ioPTH kinetics in clinical practice are essentially based on four cornerstones: the decrease rate from the maximum value achieved starting from the induction of anesthesia; the time span between samplings; the range of normality (whose maximum value is usually considered 65 pg/mL); and the absolute post-excision value considered safe. The first and second groups include the criteria of Miami (ioPTH drop ≥ 50% from any highest pre-excision level at 10 min after gland excision)26, Vienna (ioPTH drop ≥ 50% within 10 min following gland removal)27, and Rome (ioPTH drop > 50% from the highest pre-excision level, and/or ioPTH within the range of 20 min after gland removal, and/or ≤ 7.5 ng/L lower than the 10 min post removal value). The latter criterion has enhanced, among the rules, the achievement of the maximum threshold value of normality11. Finally, a recent study demonstrated the extremely low likelihood of disease persistence in patients in whom an ioPTH value of 40 pg/mL was reached within 15 min18.
We chose the Rome criterion rather than others because of the minimization of false positives, which protects against possible persistence of residual pathological tissue (i.e.: "sleeping double adenoma")10,11. The Rome criterion appears to provide the best success rate in avoiding persistence, although it could result in extended operating times and a greater number of intraoperative samplings required and, consequently, higher costs28. In fact, the authors who proposed this criterion showed that the predictive factors of disease persistence are a drop in ioPTH values that does not reach 50% after 20 min or an ioPTH value that remains, in the same time frame, above the maximum threshold (65 pg/mL). A third criterion introduced is the comparison of ioPTH values at 10 min, which could be significantly higher than at 20 min in the case of persistence11.
Several factors must be considered in support of extended monitoring: clinical conditions, such as renal failure, vitamin D deficiency, diabetes, and obesity, may require a prolongation of monitoring with an increase in the number of samples, either by modifying the kinetics of PTH or for other causes29,30,31,32.
Our results confirm the importance of extending the sampling up to 20 min and the significance of the ratio ioPTH T20-ioPTH T10. However, the latter does not appear to produce any additional accuracy compared to the ratio of ioPTH T20-baseline PTH. From these results, it that ioPTH is a good indicator to assess the recovery or possible persistence of the disease. However, among the various indicators, the most reliable appears to be the variation in PTH value detected at 20 min after surgery compared to baseline PTH. The detection of PTH at 10 min, according to our data, would lose its importance.
It could be noted that the prolongation of ioPTH monitoring to 20 min leads to an increase in costs. It has been estimated that the greatest impact on costs depends on the number of samples taken during an intervention rather than the time spent for monitoring33.
We emphasize that there is no interrelationship between the ratio ioPTH T20-baseline PTH and false negatives of localization imaging (scintigraphy). We found this finding to be interesting, because one might consider that increased parathyroid tissue activity, to which a more intense uptake might correspond, does not appear to be related to PTH kinetics. It also appears clear that the higher persistence rate with ectopic pathological parathyroid localizations (intrathyroid, mediastinal) refers to sporadic cases with a higher failure rate, which is consistent with literature data34,35,36.
This study has some limitations: the limited number of patients enrolled in the study; the exclusion of the cases of double adenoma, considered a confounding factor but which, nevertheless, constitutes the main context at risk of persistence more than all the others; and the relatively high number of procedures performed with bilateral exploration, prevalent especially in the early years of the study, compared with minimally invasive techniques or focused procedures. This is not, at present, the standard in our institution as well as in centers with medium or high volumes of activity. Finally, no distinction was made between the different baseline values of PTH, varying from 80 to about 1000 pg/ml: in this regard, we believe that such a wide variability includes subgroups that could express different kinetics of PTH.
However, the value of our data lies in their origin in a real scenario, in which the volume of activity is to be considered well above the threshold of low-volume centers, but not fully classifiable in high-volume centers, whose number, at least in Italy, is very limited and the minimum threshold considered is not achievable, at least at this time, in some areas of the country, such as Sicily.
Conclusion
The data emerging from our study in favor of extending ioPTH monitoring to 20 min after baseline detection appeared to be quite robust. Closer evaluation revealed the highest diagnostic significance of the later detection compared with the others.
However, the abolition of the 10-min sampling is not part of our routine, it is only a statistical evaluation carried out on our data, evaluated in any case according to the criterion of Rome, which at the moment, at our institution, continues to be the preferred for ioPTH monitoring.
However, we believe that an evaluation of a larger number of patients, possibly recruited for a multicentre study, could allow the validation of a simpler method in the evaluation of ioPTH monitoring with a small but significant cost reduction.
References
Nussbaum, S. R., Thompson, A. R., Hutcheson, K. A., Gaz, R. D. & Wang, C. A. Intraoperative measurement of parathyroid hormone in the surgical management of hyperparathyroidism. Surgery 104, 1121–1127 (1988).
Thompson, G. B. et al. Reoperative parathyroid surgery in the end of sestamibi scanning and intraoperative parathyroid hormone monitoring. Arch. Surg. 134(7), 699–704 (1999).
Guerin, C. et al. Persistent and recurrent hyperparathyroidism. Updates Surg. 69(2), 161–169 (2017).
Irvin, G. L. III. & Deriso, G. T. A new practical intraoperative parathyroid hormone assay. Am J Surg 168(5), 466–581 (1994).
Weber, C. J. & Ritchie, J. C. Retrospective analysis of sequential changes in serum intact parathyroid hormone levels during conventional parathyroid exploration. Surgery 126, 1139–1144 (1999).
Yamashita, H. et al. Comparison of parathyroid hormone levels from the intact and whole parathyroid hormone assays after parathyroidectomy for primary and secondary hyperparathyroidism. Surgery 135(2), 149–156 (2004).
Halevy, A. et al. Quick parathormone assay in the surgical management of hyperparathyroidism. Isr Med Assoc J 5(11), 775–777 (2003).
Perrier, N. D. et al. Parathyroid surgery: separating promise from reality. J. Clin. Endocrinol. Metab. 87, 1024 (2002).
Garbutt, L. et al. What is the most appropriate intraoperative baseline parathormone? A prospective cohort study. Int J Surg 25, 49–53 (2016).
Barczyński, M. et al. Evaluation of Halle, Miami, Rome, and Vienna intraoperative iPTH assay criteria in guiding minimally invasive parathyroidectomy. Langenbecks Arch. Surg. 394, 843–849 (2009).
Lombardi, C. P. et al. Intraoperative PTH monitoring during parathyroidectomy: The need for stricter criteria to detect multiglandular disease. Langenbecks Arch. Surg. 393, 639–645 (2008).
Di Stasio, E. et al. Parathyroidectomy monitored by intra-operative PTH: The relevance of the 20 min end-point. Clin. Biochem. 40, 595–603 (2007).
Asseeva, P. et al. Value of 123I/99mTc-sestamibi parathyroid scintigraphy with subtraction SPECT/CT in primary hyperparathyroidism for directing minimally invasive parathyroidectomy. Am. J. Surg. 217(1), 108–113 (2019).
Piccin, O. et al. Preoperative imaging workup for surgical intervention in primary hyperparathyroidism: A tertiary referral center experience. Am. J. Otolaryngol. 42(1), 102819 (2021).
Saponaro, F. et al. Clinical presentation and management of patients with primary hyperparathyroidism in Italy. J. Endocrinol. Investig. 41(11), 1339–1348 (2018).
Scerrino, G. et al. The coexistence of primary hyperparathyroidism and thyroid nodules: Should the preoperative work-up of the parathyroid and the thyroid diseases be specifically adjusted?. G Chir. 37(3), 123–129 (2016).
Bergenfelz, A., Van Slycke, S., Makay, Ö. & Brunaud, L. European multicentre study on outcome of surgery for sporadic primary hyperparathyroidism. Br. J. Surg. https://doi.org/10.1002/bjs.12025 (2020).
Claflin, E. et al. Intraoperative parathyroid hormone levels 40 pg/mL are associated with the lowest persistence rates after parathyroidectomy for primary hyperparathyroidism. Surgery 166, 50–54 (2019).
Badii, B. et al. Cost–benefit analysis of the intraoperative parathyroid hormone assay in primary hyperparathyroidism. Head Neck 39(2), 241–246 (2017).
Melfa, G. et al. Surgeon volume and hospital volume in endocrine neck surgery: How many procedures are needed for reaching a safety level and acceptable costs? A systematic narrative review. G Chir. 39(1), 5–11 (2018).
Scerrino, G. et al. Mapping the centers performing endocrine neck surgery in Italy. G Chir. 40(5), 389–397 (2019).
Iacobone, M., Scerrino, G. & Palazzo, F. F. Parathyroid surgery: An evidence-based volume-outcomes analysis: European Society of Endocrine Surgeons (ESES) positional statement. Langenbecks Arch. Surg. 404(8), 919–927 (2019).
Henry, J. F. et al. Endoscopic parathyroidectomy: Why and when?. World J. Surg. 32, 2509–2515 (2008).
Yalon, T. et al. The added value of technetium-99 m sestamibi scan in patients with primary hyperparathyroidism and positive ultrasound. World J. Surg. https://doi.org/10.1007/s00268-021-06066-8 (2021).
Miller, B. S. et al. Interpretation of intraoperative parathyroid hormone monitoring in patients with baseline parathyroid hormone levels of < 100 pg/mL. Surgery 140, 883–889 (2006) (discussion 889-890).
Caneiro, D. M., Solorzano, C. C., Nader, M. C., Ramirez, M. & Irvin, G. L. I. I. I. Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: Which criterion is the most accurate?. Surgery 134, 973–979 (2003).
Riss, P., Kaczirek, K., Heinz, G., Biglmayer, C. & Niederle, B. A “defined baseline” in PTH monitoring increases surgical success in patients with multiple gland disease. Surgery 142, 398–404 (2007).
Badii, B. et al. Cost-benefit analysis of the intraoperative parathyroid hormone assay in primary hyperparathyroidism. Head Neck 39(2), 241–246 (2017).
Their, M., Daudi, S., Bergenfeltz, A. & Almquist, M. Predictors of multiglandular disease in primary hyperparathyroidism. Langenbeck’s Arch. Surg. 403, 103–109 (2018).
Shawky, M. S. et al. Influence of common clinical variables on intraoperative parathyroid hormone monitoring during surgery for primary hyperparathyroidism. J. Endocrinol. Investig. 43, 1205–1212 (2020).
Roche, A. M., Brant, J. A. & Chai, R. L. Predictors of readmission and reoperation in patients undergoing parathyroidectomy for primary hyperparathyroidism. Otolaryngol. Head Neck Surg. 158(5), 828–834 (2018).
Sunkara, B. et al. Influence of concurrent chronic kidney disease on intra- operative parathyroid hormone monitoring during parathyroidectomy for primary hyperparathyroidism. Surgery https://doi.org/10.1016/j.surg.2017.09.014 (2017).
Riss, P. et al. Evaluating a shortened interpretation criterion for intraoperative parathyroid hormone monitoring in patients with primary hyperparathyroidism: A 5-minutes criterion in primary hyperparathyroidism and intraoperative algorithm. Head Neck 40(12), 2664–2669. https://doi.org/10.1002/hed.25453 (2018).
Navarro, A., Vassallo, J. & Galea, J. Excision of an elusive tiny ectopic parathyroid adenoma. Case Rep. Oncol. 10, 1105–1111 (2017).
Parikh, A. M., Suliburk, J. W. & Morón, F. E. Imaging localization and surgical approach in the management of ectopic parathyroid adenomas. Endocr. Pract. 24(6), 589–598 (2018).
Gawrychowski, J. et al. Surgical management of primary hyperparathyroidism. Clinicopathologic study of 1019 cases from a single institution. J. Clin. Med. 9, 3540 (2020).
Author information
Authors and Affiliations
Contributions
Material preparation was performed by G.S., S.C. and S.C.; data collection was performed by G.M., G.O., R.A., A.C. and M.P.P.; data analysis was performed by S.M.; The first draft of the manuscript was written by G.G. and G.S.; G.G., C.C., G.C. and G.S. contributed in study conception and design and final draft revision for final approval. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Graceffa, G., Cipolla, C., Calagna, S. et al. Interpretation of intraoperative parathyroid hormone monitoring according to the Rome criterion in primary hyperparathyroidism. Sci Rep 12, 3333 (2022). https://doi.org/10.1038/s41598-022-07380-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-07380-4
This article is cited by
-
Intraoperative parathyroid hormone measurement pitfalls: parathyroid hormone spikes with carboxyl-terminal parathyroid hormone fragments in primary hyperparathyroidism—a case report
Surgical Case Reports (2024)
-
Characteristics, management and outcomes of primary hyperparathyroidism from 2009 to 2021: a single centre report from South Africa
BMC Endocrine Disorders (2024)
-
Investigating the effectiveness of intraoperative rapid parathyroid hormone assay in parathyroidectomy surgery in patients with secondary hyperparathyroidism
BMC Endocrine Disorders (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.