Abstract
Postpartum depression is common; however, little is known about its relationship to social support and postpartum depression. This study examined the association between them among South Korean women within one year of childbirth. This study was based on the 2016 Korean Study of Women’s Health-Related Issues (K-Stori), a cross-sectional survey employing nationally-representative random sampling. Participants were 1,654 postpartum women within a year of giving birth. Chi-square test and logistic regression analysis were conducted to analyze the associations between social support (and other covariates) and postpartum depression. Among participants, 266 (16.1%) had postpartum depression. Depending on the level of social support, 6.0%, 53.9%, and 40.1% of them had low, moderate, and high social support, respectively. Women with moderate or low social support were more likely to have postpartum depression (OR = 1.78, 95% CI = 1.26–2.53; OR = 2.76, 95% CI = 1.56–4.89). This trend was observed in participants with multiparity, pregnancy loss, obese body image, and employed women. Social support was associated with a decreased likelihood of postpartum depression, indicating the importance of social support, especially for women experiencing multiparity, pregnancy loss, negative body image, as well as for employed women.
Similar content being viewed by others
Introduction
One of the most important turning points in a woman’s life is pregnancy and childbirth1. Women at the prenatal and postpartum periods commonly experience mental health problems2. The onset of mental health problems can cause devastation and dissension in a woman’s life3. Depression at the prenatal and postpartum periods is a common and debilitating psychiatric disorder, prevalent in South Korea and worldwide4,5. Incidence of depression is approximately two times higher in women than in men, and is particularly common among women of child-bearing age6. In Korea, social burden due to mental disorders have significantly increased. The proportion of those who suffered from mental disorders at least once in their lifetime was 30.2% in 2006 and 27.6% in 20117. The consequences of depression during the postpartum period are considerably more deleterious because a woman faces the added responsibility of being a caregiver for her newborn infant3.
Postpartum depression (PPD) is the most common complication of childbearing, affecting approximately 10–22% of woman in childbearing age8. Women usually experience PPD within the first six weeks following delivery, and recover from it six months postpartum; however, it may continue through the first and second years postpartum9. PPD is closely linked with negative outcomes for women and infants, such as maternal suicide, weak maternal interaction with her infant, early termination of breastfeeding, and delay in the child’s development10,11. Previous studies identified the following risks factors as predictors of PPD: low social support2,10,12, prenatal depression13,14, prenatal anxiety15, pregnancy loss experience16,17, perceived body image15,18,19, child care stress20, parity21,22,23, marital relationship24, socioeconomic status13, and currently employed status25,26,27.
Although PPD is undetected or inadequately treated, it may be remedied by both, behavioral and pharmacological treatments28. However, pharmacological therapy was unsuitable for postpartum mothers, particularly those who wished to breastfeed, as antidepressant compounds may be passed onto the infant via breastmilk29,30. Thus, prevention is the best method against the onset of depression rather than relying on these treatments. While the cause of PPD remains unclear, social support has been shown to be effective in helping women cope with postpartum depression12,31. Social support is defined as an exchange of resources among people perceived by the provider or recipient to be intended to improve the lifestyle of the recipient32. Social support includes both practical and emotional supports that are provided to an individual through social network. Sources of such supports are the individual’s family, friends, or significant others33. Social support can be measured in the form of perceived social support, which subjectively measures an individual's beliefs about the available support. It reflects an individuals' feeling that they are accepted, loved, and valued by other members of their social network34,35.
Previous studies have investigated the relationship between PPD and social support2,10,12 However, there was relatively little consideration for factors affecting social support and postpartum depression. Therefore, the aim of this study was to estimate the prevalence of PPD in postpartum women in South Korea, and investigate the relationship between PPD and social support.
Results
A total of 1,654 postpartum women were included in the analysis, of which 266 (16.1%) had PPD and 1,388 (83.9%) did not. The demographic and health characteristics of the study participants are summarised in Table 1. Statistically significant differences were observed between social support and having PPD. There were a greater number of women with PPD in groups with low social support.
Table 2 shows the social support status among participants: 6.0% of women had low, 53.9% had moderate and 40.1% had high social support. Overall, women who responded that social support was low had a low level of education and income, were employed, and faced high parenting burden during the previous month (p < 0.001). In addition, women with lower level of social support had relatively higher level of stress, with a history of depression and smoking (p < 0.001). Meanwhile, women with high social support had high breastfeeding percentages and high level of subjective health status (p < 0.001). Univariate and multiple logistic regression were conducted to determine the association between PPD and social support while controlling for potential covariates (Table 3). In univariate logistic regression analyses, the women with moderate (OR = 2.66, 95% CI = 1.93–3.67) and low (OR = 6.89, 95% CI = 4.22–11.24) level of social supports had increased likelihood for PPD compared to the women with high level of social support. In multivariate logistic regression analyses, the women with moderate and low social support levels were 1.78 (95% CI = 1.25–2.52) and 2.73 (95% CI = 1.54–4.83) times more likely to develop PPD, respectively, as compared to the women with high social support levels. Further, women who were employed, breastfed, faced high parenting burdens during the previous month, had poor subjective health status, high stress level, and a past depression diagnosis were more likely to develop PPD.
The results of subgroup analyses on social support and PPD with covariates are summarised in Table 4. Among women with multiparity, those with moderate and low levels of social support were 2.85 (95% CI = 1.68–4.82) and 4.90 (95% CI = 2.14–11.23) times more likely to develop PPD, respectively; but there were no statistical differences in women with primiparity. Further, in women who experienced pregnancy loss, those with lower levels of social support were 10.26 times more likely to develop PPD compared to women receiving high levels of social support. Among women who reported their body image as normal or obese, women with moderate and low levels of social support were more likely to develop PPD. In addition, women with jobs and low levels of social support showed the highest likelihood of PPD (OR = 10.34, 95% CI = 2.34–45.64).
Figure 1 presents the relationship between the level of social support in each scale of the development of PPD, and shows that the lower the social support level in all subscales, the higher the odds ratios (ORs) of PPD. The results showed a high degree of association in order of family, significant others, and friends.
Discussion
The World Health Organization (WHO) noted that mental health problems such as depression and anxiety are common during pregnancy and after childbirth26. However, there was limited information on which women develop PPD. Therefore, this study was conducted to investigate the associated factors of PPD, especially how social support affects depression in postpartum women. Our findings show that postpartum women with low social support had 4.63-fold higher odds of PPD compared with postpartum women with high social support. Further, women who are employed or breastfeeding, or have heavy parenting burden, poor subjective health status, high stress level, and were diagnosed with depression in the past were more likely to develop PPD. Furthermore, this study also showed that higher levels of social support may buffer against probability of PPD after adjusting for confounding variables. Given our results, postpartum women need a high level of social support from family, close friends, and significant others.
Interestingly, the subgroup analysis showed that women with multiparity had a five times higher risk of PPD if their social support was low. Multiparity could increase the level of maternal stress and depression because women need to also care for their previous children and infants. Women with multiparity may not receive the same level of social support as they received during their first time of childbearing because they are considered to be child-care experts despite their need of extra social support to take care of their new-born babies. Thus, the results suggest that as women with multiparity are more likely to have PPD, better social support is needed for preventing PPD27.
Another interesting finding in the current study is that women with low social support and previous experience of pregnancy loss were 10 times more likely to develop PPD. Our result is in line with previous studies in which previous pregnancy loss served as an effect modifier between social support and PPD. Pregnancy loss is an event which makes bereaved women particularly prone to depression, mood disorders, dramatic mental health disorder, and even suicide36. According to previous research, women who have lost their babies were seven to nine times more vulnerable to depression than women without a pregnancy loss37. These results indicate that postpartum women with history of pregnancy loss need higher level of social support to prevent PPD.
Body image also acts as an effect modifier between social support and PPD. Similar to adolescence, the period surrounding childbirth is accompanied by unique and rapid changes in not only body shape and size, but also psychological dimensions. Prior studies suggested that about 85% of women during pregnancy experience body image dissatisfaction38. In recent years, an increasing number of women reported to be concerned about their weight gain and appearance during pregnancy and postpartum period39,40. Body image may influence depression and health behaviours in postpartum women41. The current study results suggest that social support is an important factor that improves mental health of women with negative body image during postpartum period.
Several countries have implemented paid leave to help working parents42. Despite policies like paid leaves, women continue working for reasons such as career, being worried about losing their jobs, financial burden, and negative attitudes in the workplace. Women who have to multitask by having a job and having to rear child are especially vulnerable PPD43. Similarly, the current study results showed that employed women were 2.8 times more likely to develop PPD. Job strain often cannot be decreased or relieved, but social support in workplace can buffer the negative effect of overwork and role ambiguity25,43. In addition to workplace support, social support from their partner, family, and friends also decrease job stress in postpartum women44.
The strength of the study is that the findings are based on a nationwide survey. This ensures that the data is representative of Korean women, and comprehensively assesses depressive symptoms of the postpartum period.
Limitations
Several limitations to the present study could influence the interpretation of our findings. First, the cross-sectional design of K-stori could not show the direction of the causal relationship for the identified association between social support and PPD. Second, this study primarily relied on self-report measures from K-stori. Thus, questions on the dependent and other independent variables may contribute to recall bias. Third, depression was measured based on a self-report. Previous research has shown that self-reported survey can be under or overestimated depending on individual characteristics. Though all the responses were anonymous, quite a few individuals may not indicate their true levels of depression45.
This study provided a cross-sectional estimate of PPD within one year of childbirth in South Korean women. Social support was also positively associated with a lower likelihood of PPD in women with multiparity, pregnancy loss experience, negative body image, and jobs. Postpartum women should receive a high level of social support from family, friends, and significant others to prevent PPD and improve their maternal health, aided by health professionals.
Method
Study population
This cross-sectional study was based on the Korean Study of Women’s Health-Related Issues (K-Stori) in 2016. It was approved by the Institutional Review Board of the National Cancer Center, Korea (Approval no: NCC2016-0062). The K-Stori is a nationwide survey designed to investigate a broad area of health issues among Korean women according to five stages in the life cycle of a woman (adolescence: 14–17 years; childbearing: 19–44 years; pregnancy and postpartum: 19–44 years; menopause: 45–64 years; and old adulthood: 65–79 years)46. An approved study description was provided to all eligible participants. The study description covered the research purpose, subject, content, duration, voluntary participation, withdrawal of consent, expected risks and benefits from participating in the research, publication of the study results, and confidentiality. If the subjects agreed to participate in the study after reading the study description, participants were asked to provide written informed consent46. All methods were carried out in accordance with approved guidelines and regulations.
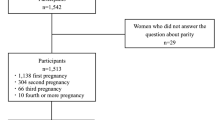
The participants of this study were women within a year of giving birth. From the total pregnant and postpartum women (n = 3000), pregnant women (n = 1,346) were excluded, and thus 1,654 women aged 19–44 years were included in the study. To recruit the participants, the interviewers planned to visit obstetrics and gynecology, or post-partum care centers. In order to select the same survey area as the other life cycle stages, a systematic data extraction method was used to identify local obstetrician and post-partum care centers, for pregnant and post-partum women, based on the same sample design area for the household survey participants.
Measures
The main outcome variable of this study was PPD, which was evaluated using the Edinburgh Postnatal Depression Scale (EPDS)47. The EPDS is a validated 10 questions screening tool, and is the most widely used screening questionnaire asking mothers how they have felt in the past seven days for PPD (Appendix 1). Participants answered the questionnaires and the answers were scored from 0–3 points (or 3–0 in case of a reverse score) with a total score of 0 to 30. A threshold score of ≥ 10 was used to classify postpartum women with a probable major depression who needed further medical examination based on the Korean version of the EPDS13,48,49.
The Multidimensional Scale of Perceived Social Support (MSPSS) was used to measure individual perceived social supports from three sources: friends (Item 6, 7, 9, and 12), family (Item 3, 4, 8, and 11) and significant others (Item 1, 2, 5, and 10)50. Participants were asked to indicate their agreement with the statements on a five-point Likert scale ranging from 0 = very strongly disagree to 4 = very strongly agree. The total score was calculated as the mean of 12 scores. The subscale total scores were the sum of the scores for the four questions related to the subscale. Total scores ranging from 12 to 24 were classified as low social support, from 25 to 36 as moderate social support and from 37 to 48 as high social support.
Further, information on age, living area, education level, household income, current job, number of parities, pregnancy loss experience, current breastfeeding status, degree of parenting burden within the last month, subjective health status, perceived body image, stress, past diagnosis of depression, and smoking experience was collected.
Statistical analyses
Descriptive analysis was conducted to compare the characteristics of study participants according to postpartum depression level. Multiple logistic regression was used to determine the association between PPD and social support while controlling for potential covariates. The OR and 95% confidence interval (95% CI) of having PPD were estimated. P values < 0.05 were considered statistically significant. Furthermore, subgroup analyses were conducted to assess the influence of social support on the risk of having PPD according to groups with different characteristics. In the subgroup analyses, the Cochran-Armitage test was used to assess the association between PPD and each variable, and the awareness of nutrition labelling. P values < 0.05 were considered to be statistically significant. All statistical analyses were performed using SAS version 9.4 (Cary, NC, USA).
Change history
04 March 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41598-022-08119-x
References
Gingnell, M. et al. Emotional anticipation after delivery–a longitudinal neuroimaging study of the postpartum period. Sci. Rep. 7, 1–6 (2017).
Gao, L. L., Chan, S. W. C. & Mao, Q. Depression, perceived stress, and social support among first-time Chinese mothers and fathers in the postpartum period. Res. Nurs. Health 32, 50–58 (2009).
Misri, S., Kostaras, X., Fox, D. & Kostaras, D. The impact of partner support in the treatment of postpartum depression. Can. J. Psychiatry 45, 554–558 (2000).
Husain, N. et al. Social stress and depression during pregnancy and in the postnatal period in British Pakistani mothers: A cohort study. J. Affect. Disord. 140, 268–276 (2012).
Kim, H. S. & Park, K. J. Latent growth model of maternal depressive symptoms: Predictors and effects on infant’s developmental outcomes. Child Stud. Asia-Pac. Contexts 4, 27–45 (2014).
Andersson, L., Sundström-Poromaa, I., Wulff, M., Åström, M. & Bixo, M. Depression and anxiety during pregnancy and six months postpartum: a follow-up study. Acta Obstet. Gynecol. Scand. 85, 937–944 (2006).
Cho, M. et al. The epidemiological survey of mental disorders in Korea 2011. Ministry of Health and Welfare Academic Research Services Business Report. (2011).
McCurdy, A. P., Boulé, N. G., Sivak, A. & Davenport, M. H. Effects of exercise on mild-to-moderate depressive symptoms in the postpartum period: a meta-analysis. Obstet. Gynecol. 129, 1087–1097 (2017).
Cornish, A. M. et al. Postnatal depression and infant cognitive and motor development in the second postnatal year: The impact of depression chronicity and infant gender. Infant Behav. Dev. 28, 407–417 (2005).
Morikawa, M. et al. Relationship between social support during pregnancy and postpartum depressive state: A prospective cohort study. Sci. Rep. 5, 1–9 (2015).
Rotheram-Borus, M. J., Tomlinson, M., Le Roux, I. & Stein, J. A. Alcohol use, partner violence, and depression: a cluster randomized controlled trial among urban South African mothers over 3 years. Am. J. Prev. Med. 49, 715–725 (2015).
Howell, E. A. et al. Reducing postpartum depressive symptoms among black and Latina mothers: A randomized controlled trial. Obstet. Gynecol. 119, 942 (2012).
Park, J.-H., Karmaus, W. & Zhang, H. Prevalence of and risk factors for depressive symptoms in Korean women throughout pregnancy and in postpartum period. Asian Nurs. Res. 9, 219–225 (2015).
Robertson, E., Grace, S., Wallington, T. & Stewart, D. E. Antenatal risk factors for postpartum depression: A synthesis of recent literature. Gen. Hosp. Psychiatry 26, 289–295 (2004).
Beck, C. T. Predictors of postpartum depression: An update. Nurs. Res. 50, 275–285 (2001).
Kersting, A. & Wagner, B. Complicated grief after perinatal loss. Dialogues Clin. Neurosci. 14, 187 (2012).
Maghade, M. A. et al. A study of depressive features and perceived social support in patients with miscarriage. Indian J. Mental Health 5, 412–418 (2018).
Carter-Edwards, L. et al. Body image and body satisfaction differ by race in overweight postpartum mothers. J. Womens Health 19, 305–311 (2010).
Boothe, A. S., Brouwer, R. J., Carter-Edwards, L. & Østbye, T. Unmet social support for healthy behaviors among overweight and obese postpartum women: Results from the active mothers postpartum study. J. Womens Health 20, 1677–1685 (2011).
Tambağ, H., Turan, Z., Tolun, S. & Can, R. Perceived social support and depression levels of women in the postpartum period in Hatay, Turkey. Niger. J. Clin. Pract. 21, 1525–1530 (2018).
Nakamura, Y. et al. Comfort with motherhood in late pregnancy facilitates maternal role attainment in early postpartum. Tohoku J. Exp. Med. 235, 53–59 (2015).
Desai, N., Mehta, R. & Ganjiwale, J. Study of prevalence and risk factors of postpartum depression. Natl. J. Med. Res. 2, 194–198 (2012).
Sagami, A., Kayama, M. & Senoo, E. The relationship between postpartum depression and abusive parenting behavior of Japanese mothers: a survey of mothers with a child less than one year old. Bull. Menninger Clin. 68, 174–187 (2004).
Azad, R. et al. Prevalence and risk factors of postpartum depression within one year after birth in urban slums of Dhaka, Bangladesh. PloS one 14, e0215735 (2019).
McGovern, P. et al. Postpartum health of employed mothers 5 weeks after childbirth. Ann. Fam. Med. 4, 159–167 (2006).
Surkan, P. J., Patel, S. A. & Rahman, A. Preventing infant and child morbidity and mortality due to maternal depression. Best Pract. Res. Clin. Obstet. Gynaecol. 36, 156–168 (2016).
Zaidi, F., Nigam, A., Anjum, R. & Agarwalla, R. Postpartum depression in women: a risk factor analysis. J. Clin. Diagn. Res.: Jcdr 11, QC13 (2017).
Horowitz, J. A. & Goodman, J. H. Identifying and treating postpartum depression. J. Obstet. Gynecol. Neonatal. Nurs. 34, 264–273 (2005).
Weissman, A. M. et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am. J. Psychiatry 161, 1066–1078 (2004).
Stephens, S., Ford, E., Paudyal, P. & Smith, H. Effectiveness of psychological interventions for postnatal depression in primary care: a meta-analysis. Ann. Fam. Med. 14, 463–472 (2016).
Ohara, M. et al. Social support helps protect against perinatal bonding failure and depression among mothers: A prospective cohort study. Sci. Rep. 7, 1–8 (2017).
Chen, C. M., Kuo, S. F., Chou, Y. H. & Chen, H. C. Postpartum Taiwanese women: their postpartum depression, social support and health-promoting lifestyle profiles. J. Clin. Nurs. 16, 1550–1560 (2007).
Kim, Y. S., Sharma, B., Jung, Y., Kim, D. & Nam, E. W. Perceived social support among women of reproductive age attending a public health facility in a poor area of Northern Lima, Peru. J. Glob. Health Sci. 1:1 (2019).
Cheng, C. Role of perceived social support on depression in Chinese adolescents: A prospective study examining the buffering model. J. Appl. Soc. Psychol. 27, 800–820 (1997).
Kuhirunyaratn, P., Pongpanich, S., Somrongthong, R., Love, E. J. & Chapman, R. S. Social support among elderly in Khon Kean province, Thailand. Southeast Asian J. Trop. Med. Public Health 38, 936 (2007).
Cacciatore, J. in Seminars in Fetal and Neonatal Medicine. 76–82 (Elsevier).
Vance, J. C. et al. Early parental responses to sudden infant death, stillbirth or neonatal death. Med. J. Aust. 155, 292–297 (1991).
Hicks, S. & Brown, A. Higher Facebook use predicts greater body image dissatisfaction during pregnancy: The role of self-comparison. Midwifery 40, 132–140 (2016).
Skouteris, H. Body image issues in obstetrics and gynecology. (2011).
Oken, E., Taveras, E. M., Popoola, F. A., Rich-Edwards, J. W. & Gillman, M. W. Television, walking, and diet: associations with postpartum weight retention. Am. J. Prev. Med. 32, 305–311 (2007).
Lancaster, C. A. et al. Risk factors for depressive symptoms during pregnancy: a systematic review. Am. J. Obstet. Gynecol. 202, 5–14 (2010).
Kim, E. J. The relationship between female education and total fertility rate, and the role of paid leave entitlements available to mothers. J. Popul. Soc. Stud. [JPSS] 28, 361–382 (2020).
McGovern, P. et al. Mothers’ health and work-related factors at 11 weeks postpartum. Ann. Fam. Med. 5, 519–527 (2007).
Munro, L., Rodwell, J. & Harding, L. Assessing occupational stress in psychiatric nurses using the full job strain model: The value of social support to nurses. Int. J. Nurs. Stud. 35, 339–345 (1998).
Kalibatseva, Z., Lyke, J. & Martino, S. Are “Superwomen" without social support at risk for postpartum depression and anxiety? Molly S. Arnold Stockton University.
Cho, H. N. et al. The Korean study of women’s health-related issues (K-Stori): Rationale and study design. BMC Publ. Health 17(1), 609 (2017).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150, 782–786 (1987).
Kim, Y.-K., Hur, J.-W., Kim, K.-H., Oh, K.-S. & Shin, Y.-C. Clinical application of korean version of edinburgh postnatal depression scale. J. Kor. Neuropsychiatr. Assoc. 47, 36–44 (2008).
Kim, M. W., Yang, H. S. & Kim, J. R. A study on agreements among screening tests and related factors with postpartum depression. Kor. J. Obst. Gynecol. 52, 1133–1143 (2009).
Zimet, G. D., Dahlem, N. W., Zimet, S. G. & Farley, G. K. The multidimensional scale of perceived social support. J. Pers. Assess. 52, 30–41 (1988).
Acknowledgements
This study was funded by the Korea Center for Disease Control and Prevention (Grant number: 2015ER630300), and a Grant-in-Aid for Cancer Research and Control from the National Cancer Center, Korea (#2210772).
Author information
Authors and Affiliations
Contributions
All authors were involved in the study conception and design. All authors were involved in the study conception and design. H.C. and K.L. contributed to drafting and writing the manuscript. H.N.C., E.C., and B.P. contributed to participate in the initial design of the study and revising the article. M.S. contributed to revising the article and statistical methodology. H.C., Y.R., and K.S.C. contributed to editing, reviewing, and final approval of article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the Acknowledgments section. “This study was funded by the Korea Center for Disease Control and Prevention (Grant number: 2015ER630300), and a Grant-in-Aid for Cancer Research and Control from the National Cancer Center, Korea (#1910231).” now reads: “This study was funded by the Korea Center for Disease Control and Prevention (Grant number: 2015ER630300), and a Grant-in-Aid for Cancer Research and Control from the National Cancer Center, Korea (#2210772).”
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, H., Lee, K., Choi, E. et al. Association between social support and postpartum depression. Sci Rep 12, 3128 (2022). https://doi.org/10.1038/s41598-022-07248-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-07248-7
This article is cited by
-
Prevalence and risk factors of postpartum depression among women attending primary healthcare centers in northern of West Bank/ Palestine: a cross-sectional study, 2022
BMC Women's Health (2024)
-
The mediating effect of psychological resilience between social support and anxiety/depression in people living with HIV/AIDS–a study from China
BMC Public Health (2023)
-
Women’s experience of perinatal support in a high migrant Australian population during the COVID-19 pandemic: a mixed methods study
BMC Pregnancy and Childbirth (2023)
-
Home-visiting programs based on the Brazelton approach: a scoping review
European Journal of Pediatrics (2023)
-
Pregorexia: a systematic review and meta-analysis on the constructs of body image dissatisfaction and eating disturbances by gestational age in the peripartum
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.