Abstract
Despite a large body of literature on the association between the dietary inflammatory index (DII) and various chronic diseases, limited knowledge is available regarding the association between DII and migraine. Therefore, we assessed the relationship between the DII and migraine characteristics, including duration, frequency, and severity of migraine headaches, Headache Impact Test-6 (HIT-6), and serum levels of nitric oxide (NO). This population-based cross-sectional study was conducted from August 2019 to June 2020 among 262 patients (38 men and 224 women; 20–50 years). A 168-item semiquantitative food frequency questionnaire (FFQ) was gathered to evaluate dietary intake, and subsequently, an energy-adjusted DII score was calculated. After controlling for potential confounders, an increase of 3.48 in headache frequency was observed when the DII score increased from − 4.04 to − 1.83 (β = 3.48; 95% CI 1.43, 5.54). In the crude model, headache duration tended to be inversely associated with DII in the subjects with the pro-inflammatory diet compared to those with the anti-inflammatory diet (β = − 0.22; 95% CI − 0.46, 0.02). After adjustment for confounders, those with the highest DII values were at a higher risk of severe headaches than those with the lowest values (OR = 2.25; 95% CI 1.17, 4.32). No other significant results were found in terms of the association between DII and HIT-6 or serum NO levels. We found evidence suggesting that higher adherence to a diet with anti-inflammatory properties was significantly and inversely related to headache frequency. Furthermore, our results suggest that the DII score is substantially related to migraine severity.
Similar content being viewed by others
Introduction
Migraine is a chronic neurological disorder defined by unilateral repeated episodes of headaches, sometimes accompanied by nausea, vomiting, phonophobia, and photophobia1. Functional disorders following headaches are seen in 90% of patients, which can eventually affect various aspects of daily life such as work, social, and family relationships2,3,4,5. Furthermore, migraine has many indirect and direct costs for patients and society6,7,8. According to the World Health Organization (WHO) report, migraine is the seventh most debilitating disease worldwide9,10, and it is more commonly seen among women. In fact, migraines are two to three times more common in women than men, with a global prevalence of 14.7% for both sexes11.
Migraine pathology is not fully understood; however, previous research has indicated that the etiology of migraine could be composed of both environmental and genetic factors12. Migraine attacks can be prompted by vascular inflammation, corticotropin-releasing hormone, neurogenic and trigeminovascular system activation, degranulation of mast cells located in the dura, and nitric oxide (NO)-like trinitroglycerin13,14,15. Previous work has shown that NO has an important role in trigeminovascular inflammation occurring during migraine attacks16. Earlier studies have illustrated that a migraine headache is significantly related to systemic inflammation and oxidative stress13,17,18,19.
Dietary factors have a significant role in the modulation of chronic inflammation20. Studies have shown the relationship between specific eating patterns and neurological disorders; notably, the intake of foods with anti-inflammatory properties (e.g., beans, fruits, and vegetables) is correlated with a lower risk of Alzheimer’s disease21, Parkinson’s disease22, and multiple sclerosis23. In contrast, a Western dietary pattern24, full of nutrients or foods with pro-inflammatory effects, has been correlated with a higher risk of depression25.
The Dietary Inflammatory Index (DII) has been a useful tool used in nutritional research to evaluate inflammatory potential by considering pro-inflammatory and anti-inflammatory attributes of special foods or dietary compounds, such as macronutrients, vitamins, minerals, and flavonoids26,27. Although previous studies indicated that inflammation and oxidative stress triggered a migraine headache28, the association between DII and migraine was not assessed in these studies. One previous cross-sectional study including 266 women has shown that there was an association between headache frequency and DII. However, no relation was observed between headache duration or migraine severity and the DII score after adjusting for traditional risk factors29. Therefore, the current study was designed to further explore associations between migraines and DII using additional indices including the Headache Impact Test-6 (HIT-6) and NO. Given the limited information and the small number of studies considering the association between DII and migraine, the present cross-sectional study aimed to assess the association between DII and migraine characteristics including duration, frequency, and severity of headache as well as HIT-6 and serum levels of NO in an Iranian population diagnosed with migraine.
Materials and methods
Participants
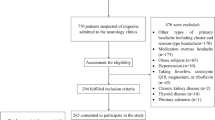
The present cross-sectional study was conducted from August 2019 to June 2020 in Isfahan, Iran. The study population was migraine patients who were admitted to the Imam Musa Sadr and Khorshid neurology clinics both affiliated with Isfahan University of Medical Sciences. Upon predefined inclusion and exclusion criteria and using a simple random sampling method, a total of 262 patients (38 men and 224 women; 20–50 years) were eligible to be enrolled in the current study. Prior to the enrollment, patients were informed regarding the aims, study procedures, and potential outcomes and their participation was voluntary (Fig. 1). Included patients suffer from migraines as defined by expert neurologic diagnosis using the International Classification of Headache Disorders (ICHD–3) criteria30. Patients were included in the study if they met the following inclusion criteria: (1) a Body Mass Index (BMI) between 18.5 and 30.0 kg/m2 and (2) diagnosis of migraines by a neurologist (F.K) based on the aforementioned criteria. Exclusion criteria included: (1) patients with a history of hypertension, diabetes, thyroid disease, cardiovascular disease, renal disease, cancer, hepatic disease, or other neurological disorders; (2) use of herbal and nutritional supplements including feverfew, coenzyme Q10, magnesium, or riboflavin; or (3) daily energy consumption outside the range of 800–4200 kcal/day (3347–17,573 kJ/day)31. The study protocol was approved by the Isfahan University of Medical Sciences Research Ethics Committee (IR.MUI.RESEARCH.REC.1398.352). Written informed consent forms were received from all participants. All study protocols were conducted according to the Declaration of Helsinki, and results were reported based on the strengthening the reporting of observational studies in epidemiology (STROBE) statement for cross-sectional studies.
Dietary intake assessment
A 168-item semi-quantitative Food Frequency Questionnaire (FFQ), a Willett-format questionnaire modified for Iranian foods, was used to evaluate the study participants' usual dietary consumption; the validity and reliability of this questionnaire have been established in a prior study32. All questionnaires were administered by a skilled dietitian. The FFQ contained a list of foods with a standard serving size for each. On a daily, weekly, or monthly basis, participants were requested to report their frequency of consumption of each food item over the previous year. Using home measurements, the portion sizes of consumed foods were estimated in grams33. The reported frequencies of intake of the various foods and beverages were then coded and analyzed for daily energy and nutrient content using Nutritionist 4 software (First Databank, Hearst Corp., San Bruno, CA, USA), which has been modified for Iranian foods.
Calculation of DII
The method previously reported by Shivappa et al. for calculating DII was used in the current analysis26. Out of 45 food items proposed by Shivappa et al., the DII score was calculated using 32 dietary parameters including energy; carbohydrate; protein; fat; cholesterol; fiber; monounsaturated fatty acids (MUFAs); polyunsaturated fatty acids (PUFAs); saturated fatty acids (SFAs); trans fatty acids (TFA); omega-3 fatty acids; omega-6 fatty acids; vitamin B12; folic acid; pyridoxine (B6); niacin (B3); riboflavin (B2); thiamin (B1); vitamins A, C, D, and E; beta carotene; magnesium; zinc; selenium; iron; caffeine; pepper; garlic; onion; and green/black tea. The energy-adjusted amounts of all nutrients were calculated via the residual technique34. Then, to get the z-score, the “standard global mean” was subtracted from the quantity of food and divided by the “global standard deviation” (SD). Standard global means and SDs for each dietary item were obtained from the article by Shivappa et al.26. To decrease skewness, this value was converted to a centered percentile score and was multiplied by the effect score for each of the food items using the numbers reported by Shivappa et al.26. Finally, we added the DII scores from all dietary components of individual participants to get the total energy-adjusted DII score for each subject. Positive values (higher DII scores) indicate a diet with pro-inflammatory properties, whereas negative values (lower DII scores) indicate a diet with anti-inflammatory properties.
Assessment of migraine
The HIT-6 tool, a 6-item validated questionnaire35, was employed to determine if migraine affects the quality of life of participants. This questionnaire contains 6 questions with 5 options for each ranging from never (scored as 6) to always (scored as 13) with a total score of 36–78. The overall score was categorized as little or no impact (≤ 49), some impact (50–55), substantial impact (56–59), and severe impact (≥ 60)36.
A 30-day headache diary was given to all participants with written and verbal instructions for completion. Participants were required to record clinical features of migraine, including headache severity, duration, and frequency for a month. The severity of headaches was evaluated using the visual analog scale (VAS) questionnaire (ranged from 0 to 10, with “0” meaning no pain and “10” the worst imaginable pain) and the overall score was categorized as mild (1–3), moderate (4–7), and severe (8–10) headache pain as suggested by previous studies37. The number of attacks per month (frequency) and mean duration of headache attacks per month (duration) were also examined.
NO was measured via the Griess method using a serum sample of patients which was taken after 8 h of fasting (Kiazist Life Sciences, Iran). Blood sampling was done the next day after the completion of the questionnaires.
Assessment of other variables
Demographic characteristics including sex, age, smoking status, marital status, number of family members, and medications were obtained using a questionnaire. Participants reported their level of physical activity using a validated version of the International Physical Activity Questionnaire (IPAQ) for 7 days38. A mercury sphygmomanometer (Riester, Germany) was used to measure blood pressure. Weight was measured in minimal clothing with a digital scale (Omron BF511, Omron Corp., Kyoto, Japan) to the nearest 100 g. Height was measured in a standing position without shoes by a wall tape meter to the nearest 1 mm. The BMI was calculated using weight (kg) divided by squared height (m2).
Statistical analysis
Mean ± standard error (SE) and number (percent) were used to express the quantitative and qualitative variables, respectively. The tertiles of the DII score were used to categorize the subjects. The Chi-square test for qualitative variables and analysis of variance (ANOVA) for quantitative variables were applied to compare general features of study subjects across tertiles of DII score. Participants' energy-adjusted food intakes were compared using ANOVA across tertiles of DII scores. Energy adjustment was done using the residual approach that was explained previously by Willett et al.39. For calculating energy-adjusted dietary intakes, each of the dietary components is regressed on their total energy intake and residual values were added to their actual mean intake to estimate energy-adjusted values. Multiple linear regression analyses were applied to analyze the relationship between DII and headache frequency, duration, and serum NO levels, and the beta (β) estimate with the associated 95% confidence intervals (CIs) were reported. The relationship between DII and migraine severity and HIT-6 was assessed using multivariable logistic regression, and the odds ratios (OR) with corresponding 95% CIs were provided. Different confounders were controlled in this study. Model 1 was adjusted for age (continuous) and sex; then, marital status (single/married), smoking status (current smoker/non-current smoker), migraine characteristic (with aura/without aura), family history (yes/no), mean arterial pressure (continuous), and physical activity (continuous) were added. Finally, BMI (continuous) was added to Model 2, resulting in the creation of the third model. SPSS version 26 (SPSS Inc., Chicago, IL, USA, www.ibm.com) was used for all analyses (IBM Corp, Armonk, NY, USA). P values < 0.05 were considered statistically significant. The sample ample size was estimated on the basis of similar studies and suggested formula for a cross-sectional design using α = 0.05, β = 0.95, r = 0.25, and drop-out rate of 10% that yielded 265 subjects29.
Ethics approval and consent to participate
The research ethics committee of Isfahan University of Medical Sciences approved the protocol of the current study on 26 August 2019 (IR.MUI.RESEARCH.REC.1398.352).
Results
A total of 770 patients were evaluated and finally, 265 patients met our inclusion criteria and consented to be enrolled in this study. The further exclusion was made for 3 subjects, since their total energy intake, on the basis of FFQ, was outside the range of 800–4200 kcal/day. The flow chart of the participants’ selection process was shown in Fig. 1. The mean (SE) of BMI, age, and DII of the study population were 25.55 (0.21) kg/m2, 36.1 (0.53) years, and − 2.96 (0.06), respectively. The general features of the study population across tertiles of DII score are given in Table 1. Compared to individuals with the lowest DII scores, those with the highest values had augmented severity of headaches, increased headache frequency, and a greater probability of migraines without aura. No other significant differences were observed for studied parameters across tertiles of DII (all P values < 0.05).
The energy-adjusted dietary intakes of participants across tertiles of DII are presented in Table 2. Compared to the lowest DII values, individuals with the highest DII scores consumed significantly higher amounts of energy, solid oils, fat, and sweets, as well as lower amounts of protein, carbohydrate, total fiber, potassium, magnesium, riboflavin, fruits, vegetables, nuts and seeds, fish, and legumes (all P values < 0.05).
The β estimates and 95% CIs for the association between DII and serum NO, headache frequency, and duration are shown in Table 3. The crude model showed that individuals with a pro-inflammatory diet (as evidenced by higher values of DII) had increased headache frequency (β = 3.32; 95% CI 1.28, 5.35) compared to those with an anti-inflammatory diet. This association remained significant after controlling for age, sex, smoking status, marital status, family history, migraine characteristics, MAP, and physical activity (β = 3.49; 95% CI 1.44, 5.55). After further adjustment for BMI, an increase of 3.48 in headache frequency was observed when the DII score increased from − 4.04 to − 1.83 (β = 3.48; 95% CI 1.43, 5.54). Headache duration tended to be inversely associated with DII when comparing subjects in the third tertile of DII to those in the first tertile (β = − 0.22; 95% CI − 0.46, 0.02). However, controlling for potential confounders attenuated the findings (β = − 0.20; 95% CI − 0.44, 0.04). Moreover, no significant association was detected between DII and serum NO levels either before or after adjustment for confounders.
In Table 4, the OR and 95% CIs for headache severity and HIT-6 across tertiles of the DII are indicated. The crude model revealed that individuals with the highest adherence to a pro-inflammatory diet had a higher likelihood of severe headache (OR = 2.53; 95% CI 1.36, 4.71) compared to those with the lowest adherence. Furthermore, after adjusting for age and sex, participants with the greatest DII score had higher odds of severe headache (OR = 2.32; 95% CI 1.23, 4.36) than those with the lowest DII values. Additional adjustments for marital status, migraine characteristics, family history, smoking status, MAP, and physical activity revealed that individuals in the third tertile of DII had a higher risk of severe headaches (OR = 2.25; 95% CI 1.17, 4.32) than those in the first tertile. Finally, when we added BMI as a confounder, a significant association was observed similar to the previous model (OR = 2.25; 95% CI 1.17, 4.32). No significant association was observed in terms of DII and HIT-6.
Discussion
The current study showed a significant positive relationship between DII score and headache frequency. However, the results did not present a significant relationship between headache duration or nitric oxide and DII after adjusting for confounders. Also, diets with higher pro-inflammatory properties, which are associated with higher serum inflammatory markers, were significantly correlated with an increased risk of severe migraine headaches. However, no significant relationship was seen between DII and HIT-6. To the best of our knowledge, this study was one of the first to investigate the association between DII and migraine.
In the current study, various possible confounders were selected to be adjusted in the regression models including age, sex, marital status, smoking status, migraine characteristic, family history, mean arterial pressure, physical activity, and BMI. The logic for using these variables was mostly based on similar studies and also literature search40,41,42. Moreover, due to the substantial role of adiposity in migraine43,44, BMI was added in a separate model to detect an adiposity independent association.
Previous research has indicated that some food patterns consistent with lower DII scores are associated with fewer migraine headache-related parameters. For example, the Dietary Approaches to Stop Hypertension (DASH) diet, which has low DII, was previously correlated with reduced headache severity and duration among migraine patients45. The majority of studies investigating the effects of nutrition on migraines have focused on the association between different types of foods and nutrients. Studies suggest that consumption of anti-inflammatory food items, including seafood46, ginger47, pepper, garlic, and onions48, is associated with improved clinical findings in patients suffering from migraine headaches. Moreover, the DII has previously been associated with other neurological disorders including dementia49, memory function50, and cognitive function51. Few studies have directly evaluated the association between migraine parameters and DII scores. One study considering the effects of the DII score on headaches among 266 Iranian women aged 18–45 years (DII score range − 4.22 to + 5.19) indicated a direct association between the DII score and headache frequency after adjustment for potential confounders. However, no relationship was found between headache duration or migraine severity and DII score45. Furthermore, a few studies have demonstrated increased inflammatory markers throughout the episodes of a migraine attack52,53,54. However, other studies have found no association between inflammatory markers and migraine headache severity or duration55. The discrepancy in results may be due to differences in study design, sample size, geographic area, and method of calculating the DII.
Migraines are described as a headache disorder with a significant effect on the quality of life and are prevalent in both developing and developed countries56. The mechanisms underlying migraine headaches are unresolved but are hypothesized to involve a degree of inflammation. The DII score is an index that reflects potential dietary inflammatory properties based on six inflammatory biomarkers, including Interleukins (IL)-1β, IL-6, IL-4, IL-10; Tumor Necrosis Factor (TNF)-α; and C-Reactive Protein (CRP)57. Secretion of Calcitonin Gene-Related Peptide (CGRP) leads to enhancement in the activity of NO synthase induction (iNOs), generation of NO expression, the activity of the cyclooxygenase-2 (COX-2) enzyme, and cytokine secretion of inflammatory factors such as IL-6, TNF-α, and IL-1β58. It has been established that cytokines, through enhanced permeability and cell-to-cell interaction, have been shown to play a major role in the pathogenesis of inflammation and pain associated with migraines59. In patients experiencing migraines, vascular disorder leads to endothelial activation and increased generation of factors such as inflammatory cytokines, intercellular adhesion molecule (ICAM), and vascular cell adhesion molecule-1 (VCAM). Pro-inflammatory cytokines, such as TNF-α, are vasodilators and induce the expression of ICAM and VCAM. Greater expression of these factors is related to microglia, which activates neuropathic inflammation and pain in the brain60,61,62. Also, some studies have indicated an association between consumption of magnesium63, riboflavin64 fruits, and vegetables65 and migraine. Our results showed that individuals in the lowest tertile of DII consumed significantly higher amounts of magnesium, riboflavin, fruits, and vegetables. As a result, higher consumption of these items may be a potential reason to explain migraine-related improvements in the present study.
We implemented a rigorous methodology in terms of patients’ selection, diagnosis of migraine, and use of valid and reliable questionnaires to improve the internal validity of the current study. Additionally, lots of possible confounders were controlled to show that the association was independent of confounders. However, due to residual confounders and some known questionnaire-based bias, this issue should be taken into account while interpreting the internal validity. In terms of external validity (generalizability), the findings of the current study can be generalized to the Iranian population with migraine headache which is independent of their sex, age, BMI, marital status, smoking, migraine characteristic, family history, MAP, and physical activity. However, the result must be generalized with caution to other populations.
The present study has several strengths. Various potential confounders were controlled for in this analysis, leading to unbiased risk estimates in this study. A validated FFQ was applied for the evaluation of dietary intakes. Nevertheless, limitations are also present. Notably, the cross-sectional design does not allow for the exploration of causative relationships between the DII and migraine. The FFQ is a memory-based questionnaire that is approximate in nature; therefore, another limitation is the potential overestimation or underestimation of dietary intake. Furthermore, residual confounders cannot be excluded, even when the model is adjusted for multiple probable confounders. While the socio-economic status of the study population was representative of the general Iranian population, generalizing these results to other populations should be done cautiously. In another word, the current study population may differ from others in terms of specific habits, culture, tradition, and geographical location that can influence our findings and diminish the generalizability of our results to other study populations. Moreover, patients were asked to refer to the laboratory for blood sampling on a headache-free day; however, it is possible that all of them were not headache free that this issue can influence our findings.
Conclusion
In conclusion, we found evidence showing that higher adherence to a diet with anti-inflammatory properties was significantly and inversely related to headache frequency. Furthermore, our results suggest that the DII score is significantly associated with the severity of migraines. More studies with larger sample sizes are needed to confirm these findings.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Butt, J. H., Franzmann, U. & Kruuse, C. Endothelial function in migraine with aura—a systematic review. Headache J. Head Face Pain 55, 35–54 (2015).
Lipton, R. B., Stewart, W. F., Diamond, S., Diamond, M. L. & Reed, M. Prevalence and burden of migraine in the United States: Data from the American Migraine Study II. Headache J. Head and Face Pain 41, 646–657 (2001).
Dueland, A. N., Leira, R., Burke, T. A., Hillyer, E. V. & Bolge, S. The impact of migraine on work, family, and leisure among young women—a multinational study. Curr. Med. Res. Opin. 20, 1595–1604 (2004).
Lipton, R. B., Stewart, W. F. & Von Korff, M. Burden of migraine: Societal costs and therapeutic opportunities. Neurology 48, 4S-9S (1997).
Dahlöf, C. G. & Solomon, G. D. The burden of migraine to the individual suffer: A review. Eur. J. Neurol. 5, 525–533 (1998).
Goetzel, R. Z. et al. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting US employers. J. Occup. Environ. Med. 46, 398–412 (2004).
Edmeads, J. & Mackell, J. A. The economic impact of migraine: An analysis of direct and indirect costs. Headache J. Head Face Pain 42, 501–509 (2002).
Ferrari, M. D. The economic burden of migraine to society. Pharmacoeconomics 13, 667–676 (1998).
Steiner, T. J., Stovner, L. J. & Birbeck, G. L. (Wiley Online Library, 2013).
Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 386, 743–800 (2015).
Vos, T. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196 (2012).
Andress-Rothrock, D., King, W. & Rothrock, J. An analysis of migraine triggers in a clinic-based population. Headache J. Head Face Pain 50, 1366–1370 (2010).
Martami, F. et al. The serum level of inflammatory markers in chronic and episodic migraine: A case–control study. Neurol. Sci. 39, 1741–1749 (2018).
Waeber, C. & Moskowitz, M. A. Migraine as an inflammatory disorder. Neurology 64, S9–S15 (2005).
Xanthos, D. N. et al. Central nervous system mast cells in peripheral inflammatory nociception. Mol. Pain 7, 1744 (2011).
Sarchielli, P. et al. Chemokine levels in the jugular venous blood of migraine without aura patients during attacks. Headache J. Head Face Pain 44, 961–968 (2004).
Dahri, M., Tarighat-Esfanjani, A., Asghari-Jafarabadi, M. & Hashemilar, M. Oral coenzyme Q10 supplementation in patients with migraine: Effects on clinical features and inflammatory markers. Nutr. Neurosci. 22, 607–615 (2019).
Conti, P. et al. Progression in migraine: Role of mast cells and pro-inflammatory and anti-inflammatory cytokines. Eur. J. Pharmacol. 844, 87–94 (2019).
Dini, E. et al. Plasma levels of oxidative stress markers, before and after BoNT/A treatment, in chronic migraine. Toxins 11, 608 (2019).
Hermsdorff, H. H. M., Zulet, M. Á., Puchau, B. & Martínez, J. A. Fruit and vegetable consumption and proinflammatory gene expression from peripheral blood mononuclear cells in young adults: A translational study. Nutr. Metab. 7, 1–11 (2010).
Sofi, F., Macchi, C., Abbate, R., Gensini, G. F. & Casini, A. Effectiveness of the Mediterranean diet: Can it help delay or prevent Alzheimer’s disease?. J. Alzheimers Dis. 20, 795–801 (2010).
Maraki, M. I. et al. Mediterranean diet adherence is related to reduced probability of prodromal Parkinson’s disease. Mov. Disord. 34, 48–57 (2019).
Sedaghat, F., Jessri, M., Behrooz, M., Mirghotbi, M. & Rashidkhani, B. Mediterranean diet adherence and risk of multiple sclerosis: A case–control study. Asia Pac. J. Clin. Nutr. 25, 377 (2016).
Hosseinzadeh, M. et al. Empirically derived dietary patterns in relation to psychological disorders. Public Health Nutr. 19, 204–217 (2016).
Li, Y. et al. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 253, 373–382 (2017).
Shivappa, N., Steck, S. E., Hurley, T. G., Hussey, J. R. & Hébert, J. R. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 17, 1689–1696 (2014).
Tabung, F. K. et al. Construct validation of the dietary inflammatory index among postmenopausal women. Ann. Epidemiol. 25, 398–405 (2015).
Borkum, J. M. Migraine triggers and oxidative stress: A narrative review and synthesis. Headache J. Head Face Pain 56, 12–35 (2016).
Khorsha, F. et al. Association between diet and migraine characteristics: The role of dietary inflammatory index. Curr. J. Neurol. 19, 67–75 (2020).
Olesen, J. Headache Classification Committee of the International Headache Society (IHS) the international classification of headache disorders, asbtracts. Cephalalgia 38, 1–211 (2018).
Estruch, R. et al. Effects of dietary fibre intake on risk factors for cardiovascular disease in subjects at high risk. J. Epidemiol. Community Health 63, 582–588 (2009).
Esfahani, F. H., Asghari, G., Mirmiran, P. & Azizi, F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. J. Epidemiol. 20, 150–158 (2010).
Ghaffarpour, M., Houshiar-Rad, A. & Kianfar, H. The manual for household measures, cooking yields factors and edible portion of foods. Tehran Nashre Olume Keshavarzy 7, 42–58 (1999).
Willett, W. & Stampfer, M. J. Total energy intake: Implications for epidemiologic analyses. Am. J. Epidemiol. 124, 17–27 (1986).
Rendas-Baum, R. et al. Validation of the Headache Impact Test (HIT-6) in patients with chronic migraine. Health Qual. Life Outcomes 12, 1–10 (2014).
Yang, M., Rendas-Baum, R., Varon, S. F. & Kosinski, M. Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia Int. J. Headache 31, 357–367. https://doi.org/10.1177/0333102410379890 (2011).
Price, D. D., McGrath, P. A., Rafii, A. & Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 17, 45–56 (1983).
Hagströmer, M., Oja, P. & Sjöström, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 9, 755–762 (2006).
Willett, W. C., Howe, G. R. & Kushi, L. H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 65, 1220S-1228S (1997).
Hajjarzadeh, S., Mahdavi, R., Shalilahmadi, D. & Nikniaz, Z. The association of dietary patterns with migraine attack frequency in migrainous women. Nutr. Neurosci. 23, 724–730 (2020).
Bakırhan, H., Yıldıran, H. & Uyar Cankay, T. Associations between diet quality, DASH and Mediterranean dietary patterns and migraine characteristics. Nutr. Neurosci. 20, 1–11 (2021).
Fernández-de-Las-Peñas, C. et al. Population-based study of migraine in Spanish adults: Relation to socio-demographic factors, lifestyle and co-morbidity with other conditions. J. Headache Pain 11, 97–104 (2010).
Halaiko, D. A., Faro, P., Levis, A. A. & Netto, B. D. M. The association between obesity and migraine and possible mechanisms of action: An integrative literature review. Headache Med. 20, 16–22 (2021).
Hatami, M., Soveid, N., Lesani, A., Djafarian, K. & Shab-Bidar, S. Migraine and obesity: Is there a relationship? A systematic review and meta-analysis of observational studies. CNS Neurol. Disord. -Drug Targets 20, 863–870 (2021).
Mirzababaei, A. et al. Associations between adherence to dietary approaches to stop hypertension (DASH) diet and migraine headache severity and duration among women. Nutr. Neurosci. 23, 335–342 (2020).
Tajmirriahi, M. et al. The effects of sodium valproate with fish oil supplementation or alone in migraine prevention: A randomized single-blind clinical trial. Iran. J. Neurol. 11, 21 (2012).
Martins, L. B. et al. Double-blind placebo-controlled randomized clinical trial of ginger (Zingiber officinale Rosc.) addition in migraine acute treatment. Cephalalgia 39, 68–76 (2019).
D’Andrea, G., Cevoli, S. & Cologno, D. Herbal therapy in migraine. Neurol. Sci. 35, 135–140 (2014).
Hayden, K. M. et al. The association between an inflammatory diet and global cognitive function and incident dementia in older women: The Women’s Health Initiative Memory Study. Alzheimers Dement. 13, 1187–1196 (2017).
Frith, E. et al. Dietary inflammatory index and memory function: Population-based national sample of elderly Americans. Br. J. Nutr. 119, 552 (2018).
Shin, D. et al. Inflammatory potential of diet is associated with cognitive function in an older adult Korean population. Nutrition 55, 56–62 (2018).
Theodoropoulos, D. et al. Allergen-specific sublingual immunotherapy in the treatment of migraines: A prospective study. Eur. Rev. Med. Pharmacol. Sci. 15, 1117–1121 (2011).
Meng, W. et al. Clinical research on treatment of migraine with pine needle moxibustion. Zhongguo Zhen jiu Chin. Acupuncture moxibustion 32, 519–522 (2012).
Güzel, I., Taşdemir, N. & Çelik, Y. Evaluation of serum transforming growth factor β1 and C-reactive protein levels in migraine patients. Neurol. Neurochir. Pol. 47, 357–362 (2013).
Tanik, N., Celikbilek, A., Metin, A., Gocmen, A. Y. & Inan, L. E. Retinol-binding protein-4 and hs-CRP levels in patients with migraine. Neurol. Sci. 36, 1823–1827 (2015).
Maleki, N., Kurth, T. & Field, A. E. Age at menarche and risk of developing migraine or non-migraine headaches by young adulthood: A prospective cohort study. Cephalalgia 37, 1257–1263 (2017).
Wirth, M. et al. Association of a dietary inflammatory index with inflammatory indices and the metabolic syndrome among police officers. J. Occup. Environ. Med. Am. Coll. Occup. Environ. Med. 56, 986 (2014).
Durham, P. & Papapetropoulos, S. Biomarkers associated with migraine and their potential role in migraine management. Headache J. Head Face Pain 53, 1262–1277 (2013).
Longoni, M. & Ferrarese, C. Inflammation and excitotoxicity: Role in migraine pathogenesis. Neurol. Sci. 27, s107–s110 (2006).
Hamed, S. A. The vascular risk associations with migraine: Relation to migraine susceptibility and progression. Atherosclerosis 205, 15–22 (2009).
Rodríguez-Osorio, X. et al. Endothelial progenitor cells: A new key for endothelial dysfunction in migraine. Neurology 79, 474–479 (2012).
Saegusa, H. & Tanabe, T. N-type voltage-dependent Ca2+ channel in non-excitable microglial cells in mice is involved in the pathophysiology of neuropathic pain. Biochem. Biophys. Res. Commun. 450, 142–147 (2014).
Sun-Edelstein, C. & Mauskop, A. Role of magnesium in the pathogenesis and treatment of migraine. Expert Rev. Neurother. 9, 369–379 (2009).
Thompson, D. & Saluja, H. Prophylaxis of migraine headaches with riboflavin: A systematic review. J. Clin. Pharm. Ther. 42, 394–403 (2017).
Narula, A. et al. (AAN Enterprises, 2021).
Acknowledgements
The authors wish to thank all participants who kindly contributed to the study.
Funding
This study was funded by Isfahan University of Medical Sciences, Isfahan, Iran.
Author information
Authors and Affiliations
Contributions
Conception and design: A.A., G.A., F.K. Acquisition of data: A.A., S.M.G., F.K. Analysis and interpretation of data: A.A., H.M. Drafting the manuscript: A.A., S.M.G. Revising manuscript for intellectual content: A.A., G.A., F.K.K., H.M., S.M.G., M.S.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ghoreishy, S.M., Askari, G., Mohammadi, H. et al. Associations between potential inflammatory properties of the diet and frequency, duration, and severity of migraine headaches: a cross-sectional study. Sci Rep 12, 2878 (2022). https://doi.org/10.1038/s41598-022-06819-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-06819-y
This article is cited by
-
Association of dietary and lifestyle inflammation score (DLIS) with chronic migraine in women: a cross-sectional study
Scientific Reports (2024)
-
Ethnopharmacology of medicinal plants used in choman community, Hewler (Erbil), Kurdistan Region, Iraq
Genetic Resources and Crop Evolution (2024)
-
Sex-specific metabolic profiling to explain the increased CVD risk in women with migraine: a narrative review
The Journal of Headache and Pain (2023)
-
Risk factors for migraine disease progression: a narrative review for a patient-centered approach
Journal of Neurology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.