Abstract
Shorter people are at risk for cardiovascular disease (CVD), but data remain limited. This study sought to determine whether height loss is associated with an increased incidence of CVD. From the Korean National Health Insurance Service—Senior database (2002–2015), data of 134,952 individuals with available information on height loss was obtained. Height loss as percentages was measured 3–5 years from the baseline height. To assess hazard ratios for CVD incidence, multivariable Cox proportional hazard regression models were used before and after applying propensity score matching. The unmatched cohort consisted of 109,546 participants without height loss (< 1%): 20,208 participants with 1–2% height loss, and 5126 participants with ≥ 2% height loss. During a median follow-up period of 6.5 years (interquartile range, 3.7–8.5 years), 21,921 were newly diagnosed with CVD. Adults with height loss of > 2% had a greater risk of incident CVD than those with no height loss. This finding was statistically significant both in the original- and propensity score-matched cohorts. The increased risk for ischemic stroke was significant in the male subgroups, in line with degree of height loss. Overall, height loss is associated with an increased risk of subsequent ischemic stroke in Korean men.
Similar content being viewed by others
Introduction
There is solid evidence regarding the increased risk of cardiovascular disease (CVD) in shorter people1; however, further studies are warranted to elucidate the underlying mechanism. Several prospective investigations with a sufficient number of cases and/or long follow-up periods have been conducted, but they do not draw a clear conclusion regarding the relationship between height loss and CVD incidence. The relationship is further complicated by the shared pathophysiology between CVD and osteoporosis2.
To explore this issue, longitudinal studies with sequential height measurements are warranted. One study3 followed 4213 men in the UK aged between 60 and 79 years. The researchers measured participants’ height changes after a period of 20 years. After a mean follow-up period of 6 years, compared to the group with a height loss of < 1 cm, the group with a height loss of ≥ 3 cm had a higher risk of CVD mortality (P = 0.02) and incidence of CVD (P = 0.03). Another study from the UK4 analyzed the data of 3802 men and 1615 women (aged 45 to 69 years) who had their height remeasured after an interval of 12 years. During the mean follow-up of 7.4 years, 69 cases of coronary heart diseases had occurred in the male participants and were associated with greater height loss (95% confidence interval [CI], 1.00–1.53). Recently, a Japanese study with 2498 atomic bomb survivors reported that marked height loss in middle age was an independent predictor for CVD mortality5.
The aforementioned studies had the following limitations. First, the data was only just within the limits of statistical significance, meaning no clear relationship between amount of height loss and CVD was described. Second, the researchers did not consider any osteoporotic events that may have critically impacted height loss. Third, they did not guarantee the generalizability in terms of sex, age, or health compared to the general population or other ethnic populations. Thus, this study aimed to investigate the relationship between height loss and CVD in a nationally representative large cohort from the Korean National Health Insurance Service database, with consideration of potential confounders including osteoporosis.
Methods
Study design and participants
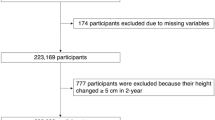
We used the National Health Insurance Service-Senior (NHIS-Senior) cohort6, provided by the Korean NHIS. The NHIS-senior cohort consists of a 10% random sample based on national claims data over 60 years old since 2002 in Korea, and has been tracked until 2015. The NHIS manages the national public health insurance program in which all health-care providers need to submit medical claims for reimbursement. NHIS subscribers receive biennial, mandatory health examinations starting from the age of 40 years. The NHIS data records demographic profile, health insurance claims, the death and disability registries, and national health check-up data. The International Classification of Diseases-10th Revision (ICD-10) was used to identify cases of morbidity and mortality. Representative 14-year (2002–2015) longitudinal data are provided to public health researchers if approved by the official review committee. We selected 174,030 individuals aged over 60 years, who had available data on height change over a period of 3–5 years. Among these, we excluded patients who had a history of osteoporotic vertebral fracture (ICD codes, M48.4, M48.5, S22.0, S22.1, S32.0; n = 14,704) or major CVD (i.e., acute myocardial infarction or any stroke; n = 32,866). Finally, 134,925 participants were enrolled as the unmatched whole cohort in this study (Fig. 1).
Ethical approval statement
The Korean National Health Insurance Corporation provided anonymized data to the researchers after approving the study protocol (No. NHIS-2020–2-004). This study was approved by the Institutional Review Board of Gachon University Gil Medical Center (IRB No. GCIRB2019-370). Participant consent was waived by the ethics committee because the data involved routinely collected medical data that was processed anonymously at all stages. All study methods were carried out based on the Declaration of Helsinki.
CVD outcomes and covariates
The primary outcome of this study was a newly diagnosed CVD during the follow-up period which was from the index date. The index date was recorded as the time of the second height measurement that was used to calculate height loss. Incidence of CVD included cases of acute myocardial infarction (ICD code, I21) and any stroke (ICD codes, ischemic, I63; hemorrhagic, I60–62) (Supplementary Table 1). Cases of CVD were defined as at least one outpatient visit or admission > 1, with the main or 1st subcode as one of the diagnoses.
In Korea, regular national checkups are performed every 1–2 years. At 3–5 years from the first screening, height measurements are made at the screening, and cases in which a decrease in height was confirmed were categorized and defined as within 1%, 1–2%, or > 2%. We used relative height loss, which was calculated as a percentage from the baseline height, because baseline height is associated with CVD risk1. Regarding information from the health checkup data, the most recent data (nearest the index date) were selected; these included height, weight, low income (medical aid benefits), and self-reported smoking status (never, ex-, or current). Body mass index (BMI, kg/m2) was calculated, and comorbidities such as hypertension and osteoporosis (ICD codes, M80–M82) were also assessed (Supplementary Table 1). The Charlson Comorbidity Index (CCI) was used to control for comorbid conditions7 (Supplementary Table 2).
Propensity score matching (PSM)
We also used propensity score matching to reduce potential confounders and to balance the baseline covariates of the groups8. The propensity score is the probability that an individual will lose height, based on their individual characteristics. Individual propensities for height loss were estimated by performing a logistic regression analysis of age, sex, coverage for low income, hypertension, osteoporosis, smoking status, CCI, and BMI. A ‘‘greedy nearest-neighbor’’ algorithm was used to match patients in the groups in a 1:1:1 ratio9. Adequacy of matching was assessed by comparing propensity score densities, distribution, and standardized mean differences (Supplementary Table 3). This approach calculates the mean population differences of the groups and is more meaningful than assessing P values from t tests10. After propensity score matching, there were 5122 adults with no height loss (< 1%) and matched adults with some height loss (5097 with 1–2% height loss and 5126 with ≥ 2% height loss) (Fig. 1).
Statistical analysis
Cohorts were followed up from the index date, until outcomes occurred or until the study period ended on December 31, 2015. Cox proportional hazards regression models were applied to calculate the hazard ratios (HRs) and 95% CIs for the CVD outcomes11. We used a global goodness-of-fit test proposed by Schoenfeld to test the proportional hazard assumption12. Adjusted curves for cumulative hazards were estimated using the multivariable Cox Proportional Hazard model for CVD outcomes and height loss in three categories. In the multivariable analysis, the covariates presented above were used. For stroke outcomes, the CHA2DS2–VASc score13 was applied in the Cox models, instead of the CCI score (Supplementary Table 4). Two-sided P values < 0.05 were considered statistically significant. Statistical tests were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Participant characteristics in relation to degree of height loss are described in Table 1. Individuals with greater height loss were more likely to be women, ≥ 75 years old, receive medical aid, have osteoporosis, and present a high CCI score.
The result of the minimally adjusted model is presented in Supplementary Table 5. Table 2 shows the association between height loss and incident CVD. During a median follow-up period of 6.5 years (interquartile range, 3.7–8.5 years), 21,921 participants were newly diagnosed with CVD (2,577 acute myocardial infarctions, 1916 hemorrhagic strokes, and 17,575 ischemic strokes). Compared to individuals with no height loss (< 1% height loss), those with height loss ≥ 2% had an increased risk of CVD in both the original (HR, 1.11; 95% CI, 1.04–1.19) and PSM cohorts (HR, 1.93; 95% CI, 1.73–2.16). However, this association was only statistically significant in regard to ischemic stroke (Table 3 and Fig. 2). Further, risk for incident ischemic stroke was significantly correlated with degree of height loss among men (Table 3).
Risk of incident ischemic stroke by degree of height loss. Adjusted for age (continuous), sex, hypertension, osteoporosis, coverage for low income, smoking status, CHA2DS2–VASc score (continuous), and body mass index (continuous). Created using SAS software (version 9.4; SAS Institute Inc., Cray, NC, USA).
Discussion
Prevention of CVD is a major public concern due to its increasing prevalence and resulting social burden14, and the need for better stratification of CVD risks prevails. Among the CVD risk factors, height is recently focused upon as it is known to be inversely associated with CVD outcomes1. Additionally, a number of studies have suggested that it is simple and economically viable for clinicians to monitor a patient’s change in height as a measure of health problems15. In this nationwide large-scale population-based study, we found that height loss is associated with CVD morbidity. These results suggest that height shrinkage is an informative, and easy to measure, indicator of worsening cardiovascular health at the population level, when more detailed measures might not be available.
Although age-related decline in height is a common observation, its possible association with CVD outcomes has rarely been studied. In prior studies3,4,5 on this issue, the small number of cases with height loss, outcome events, or lack of a clearly specified population could give rise to aberrant results, which must therefore be considered and interpreted cautiously. Of note, height shrinkage is greatest among taller individuals—who are known to be at low risk of CVD—as well as older age groups and women16. Thus, a lack of consideration of baseline height leads to an attenuation bias in the height-CVD association. We believe that despite the great height loss and/or long-term follow-up duration, a lack of significant results in previous studies was due to the dilution effect between greater height loss and lower baseline CVD risk in tall people. We analyzed a large-scale, nationwide cohort, which included both men and women, as well as young and elderly people, using a proportional indicator for height loss.
The causality between height loss and CVD outcomes remains to be further elucidated2, but longitudinal designs as used in the present study indicate that height loss might be a direct cause rather than a result of CVD. Given that osteoporotic consequences are highly linked to height loss17, we excluded a priori patients with vertebral fracture and only considered those with osteoporosis during the follow-up. Thus, our study included a limited number of cases of height loss caused by intervertebral disc degeneration; osteoarthritic conditions of the spine, hip, or knee; or weakness of the back muscles18. Paravertebral muscle weakness may reflect sarcopenia19. The increased risk of CVD associated with height loss may reflect poor muscular strength and skeletal muscle mass loss, both of which have been shown to be predictors of mortality20. Moreover, it has been established that women experience a greater degree of height decline over time than men, with one of the reasons being their vulnerability to osteoporosis and/or broken bones, and while height loss in women reflects the decrease in bone density, the cause of height loss in men has not yet been reported21.
Significance of height loss in cases of ischemic stroke was partially explained by the outstanding incidence of ischemic stroke in our cohort, compared with that of hemorrhagic stroke or myocardial infarction. Additionally, from the traditional mechanistic perspective, higher luminal pressure and increased shearing stress from height loss, particularly in the cerebral artery, may accelerate the progression of atherosclerosis22, which leads to ischemic stroke. Our subgroup analysis further showed that the correlation between height loss and incident ischemic stroke remained robust among men, which could be partially explained by the relative contribution of height loss to incident stroke (Supplementary Table 6). Our results suggest that height loss in elderly men could be an indicator of impending ischemic stroke and should be an important consideration for physicians. Furthermore, future research considering body composition would be helpful to elucidate the possible mechanism of the relationship between height loss and CVD and gender difference of this association.
Several limitations in the present study should be acknowledged. First, given that recruitment was based on the database of health examinations (the overall participation rate was 65.3%), the generated data cannot be considered free from potential healthy-user bias. If people who had not received a health screen had been included in the analysis, the significance of the results would be rather more remarkable because they would be more vulnerable to height loss and CVD development. This phenomenon might also be applied for underdiagnosis of osteoporosis in older men. Second, there may have been measurement inconsistencies as height was measured at different institutions. However, this non-differential misclassification of height loss would rather dilute the real effect. Third, some unmeasured confounding factors could remain. Early-life conditions, particularly nutrition, have been established to play an important role in shaping subsequent cardiovascular health23. Moreover, spine misalignment that can have an impact on the association24 was not considered in this study. A hospital-based study or expansion of clinical trial cohort that could capture those detailed clinical data is needed to confirm our findings.
Despite the limitations, this study contributes to the literature with its large-scale cohort sample and examination of detailed nation-wide health data. To clarify the association between height loss and cardiovascular events, a genetic or twin-track approach is needed. Further interventional research is needed to disentangle the effects of height loss prevention strategies (e.g., weight bearing exercises or anti-osteoporotic agents) on CVD incidence. Serial measurements of stature are highly feasible in clinical practice and may be useful as an indicator of cardiovascular health in the primary care setting, particularly in men.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nuesch, E. et al. Adult height, coronary heart disease and stroke: a multi-locus Mendelian randomization meta-analysis. Int. J. Epidemiol. 45(6), 1927–1937. https://doi.org/10.1093/ije/dyv074 (2016).
Laroche, M. et al. Osteoporosis and ischemic cardiovascular disease. Joint Bone Spine 84(4), 427–432. https://doi.org/10.1016/j.jbspin.2016.09.022 (2017).
Wannamethee, S. G., Shaper, A. G., Lennon, L. & Whincup, P. H. Height loss in older men: associations with total mortality and incidence of cardiovascular disease. Arch. Int. Med. 166(22), 2546–2552. https://doi.org/10.1001/archinte.166.22.2546 (2006).
Batty, G. D. et al. Height loss and future coronary heart disease in London: the Whitehall II study. J. Epidemiol. Community Health. 65(5), 461–464. https://doi.org/10.1136/jech.2009.103986 (2011).
Masunari, N. et al. Height loss starting in middle age predicts increased mortality in the elderly. J. Bone Miner Res. 27(1), 138–145. https://doi.org/10.1002/jbmr.513 (2012).
Lee, J., Lee, J. S., Park, S. H., Shin, S. A. & Kim, K. Cohort profile: the national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 46(2), e15. https://doi.org/10.1093/ije/dyv319 (2017).
Hwangbo, Y. et al. Incidence of diabetes after cancer development: a Korean national cohort study. JAMA Oncol. 4(8), 1099–1105. https://doi.org/10.1001/jamaoncol.2018.1684 (2018).
Austin, P. C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav. Res. 46(3), 399–424. https://doi.org/10.1080/00273171.2011.568786 (2011).
Franklin, J. M., Eddings, W., Austin, P. C., Stuart, E. A. & Schneeweiss, S. Comparing the performance of propensity score methods in healthcare database studies with rare outcomes. Stat. Med. 36(12), 1946–1963. https://doi.org/10.1002/sim.7250 (2017).
Roumie, C. L. et al. Association of treatment with metformin vs sulfonylurea with major adverse cardiovascular events among patients with diabetes and reduced kidney function. JAMA 322(12), 1167–1177. https://doi.org/10.1001/jama.2019.13206 (2019).
Lau, B., Cole, S. R. & Gange, S. J. Competing risk regression models for epidemiologic data. Am. J. Epidemiol. 170(2), 244–256. https://doi.org/10.1093/aje/kwp107 (2009).
Moreau, T., O’Quigley, J. & Mesbah, M. A global goodness-of-fit statistic for the proportional hazards model. Appl. Stat. 34(3), 212–218. https://doi.org/10.2307/2347465 (1985).
January, C. T. et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation 130(23), 2071–2104. https://doi.org/10.1161/CIR.0000000000000040 (2014).
Virani, S. S. et al. Heart disease and stroke statistics-2021 update: a report from the american heart association. Circulation 143(8), e254–e743. https://doi.org/10.1161/CIR.0000000000000950 (2021).
Kim, Y. H. et al. Gender differences in the relationship between socioeconomic status and height loss among the elderly in South Korea: Korean National Health and Nutrition Examination Survey 2008–2010. Medicine (Baltimore) 96(34), e7131. https://doi.org/10.1097/MD.0000000000007131 (2017).
Jain, U. & Ma, M. Height shrinkage, health and mortality among older adults: evidence from Indonesia. Econ. Hum. Biol. 37, 100863. https://doi.org/10.1016/j.ehb.2020.100863 (2020).
Chen, R. et al. The Value of historical height loss for detecting vertebral fractures in postmenopausal women in China. Endocr. Res. 46(1), 14–19. https://doi.org/10.1080/07435800.2020.1827263 (2021).
Roberts, S. et al. Ageing in the musculoskeletal system. Acta Orthop. 87(363), 15–25. https://doi.org/10.1080/17453674.2016.1244750 (2016).
Kim, W. J. et al. Sarcopenia and back muscle degeneration as risk factors for degenerative adult spinal deformity with sagittal imbalance and degenerative spinal disease: a comparative study. World Neurosurg. 148, E547–E555. https://doi.org/10.1016/j.wneu.2021.01.053 (2021).
Wilkinson, D. J., Piasecki, M. & Atherton, P. J. The age-related loss of skeletal muscle mass and function: measurement and physiology of muscle fibre atrophy and muscle fibre loss in humans. Ageing Res. Rev. 47, 123–132. https://doi.org/10.1016/j.arr.2018.07.005 (2018).
Rinonapoli, G. et al. Osteoporosis in men: a review of an underestimated bone condition. Int. J. Mol. Sci. https://doi.org/10.3390/ijms22042105 (2021).
Dumor, K., Shoemaker-Moyle, M., Nistala, R. & Whaley-Connell, A. Arterial stiffness in hypertension: an update. Curr. Hypertens. Rep. https://doi.org/10.1007/s11906-018-0867-x (2018).
Zhang, J. Y. & Lu, N. The association between childhood conditions and heart disease among middle-aged and older population in China: a life course perspective. Bmc Geriatr. https://doi.org/10.1186/s12877-021-02134-9 (2021).
Kado, D. M. et al. Hyperkyphosis predicts mortality independent of vertebral osteoporosis in older women. Ann. Int. Med. 150(10), 681–687. https://doi.org/10.7326/0003-4819-150-10-200905190-00005 (2009).
Acknowledgements
This study was supported by grants from the Gachon University Gil Medical Center (grant numbers, FRD2019-11 and FRD2021-14). The sponsor of the study was not involved in the study design, analysis, and interpretation of data; writing of the report; or the decision to submit the study results for publication.
Author information
Authors and Affiliations
Contributions
Drs J.J. and R.L. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. I.C.H. and J.J. contributed to the study concept and design, also study supervision. I.C.H., S.J.C., R.L. and Y.N. contributed to the acquisition, analysis, or interpretation of data. I.C.H., S.J.C. and R.L. Drafted of the manuscript. S.J.C., R.L., Y.N., I.C.H. and J.J. critically revised the manuscript. Statistical analysis run by R.L., I.C.H. and J.J. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, S.J., Lee, R., Na, Y. et al. Association between height loss and cardiovascular disease in the Korean elderly. Sci Rep 12, 2551 (2022). https://doi.org/10.1038/s41598-022-06594-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-06594-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.