Abstract
In patients presented to emergency rooms, Pro hormone of Natriuretic Peptide (Pro BNP) essay is overly sensitive test to rule out heart failure but less specific in predicting outcomes in follow-ups, in this study we ought to find the added value of High Sensitivity cardiac Troponin I (Hs-cTn I), in patients presented acutely with heart failure and its impact on mortality when Pro BNP is highly elevated. Prospective cohort study, inclusion criteria were age above 18 and clearly positive NT Pro BNP > 1000 pg/ml, with 12 months follow up period, primary end point was mortality from heart failure, secondary endpoint was need for rehospitalization. 95 patients were enrolled, divided into overt and non-overt pulmonary edema groups. Mean (Pro BNP) was 6184 and 5927 pg/ml and mean (Hs-cTn I) were 19.27 and 0.17 ng/ml respectively, Mean Ejection fraction was 48 ± 7 and 47 ± 7 for each group sequentially. Mortality rate was 4 (13%) in the higher Hs-c Tn I group, and 1 (1.6%) in the low troponin level group p = .03, odd ratio was 8.5, 95% CI (0.9–80). Need for re-hospitalization was present in 12 (38%) Vs 7 (8%) patients, p = .0081, odd ratio 4.8, 95% CI (1.7–14.2). In COX proportional hazard analysis, only Hs-cTn I was a significant predictor of poor outcome in this high-risk cohort with p = 0.0001. Adding (Hs-cTrop I) assay to the panel of laboratory testing, in patients presented to ER with acute heart failure and with high Pro-BNP > 1000, may further predicts mortality and rehospitalization rate.
Similar content being viewed by others
Introduction
Acute cardiac pulmonary edema secondary to heart failure carries a bad prognosis. Beta natriuretic peptide (BNP) and N-terminal Pro BNP are the gold standard biomarkers used for diagnosis and prognosis, more novel biomarkers like Mid-Regional pro ADrenoMedullin (MR-proADM) Mid-Regional pro Atrial Natriuretic Peptide (MR-proANP), Highly sensitive cardiac Troponins (Hs-cTn), soluble Suppression of Tumorigenicity 2 (sST2), Growth Differentiation Factor (GDF)-15 and Galectin-3, may have a role to play in determining prognosis far and beyond the one established by natriuretic peptides, but their potential role in clinical care of patients with heart failure is yet to be fully determined1.
There are many studies that looked at the utility of using pro-BNP, the natural peptides produced by atria, due to stretching effect of elevated cavitary pressure, and its value in diagnosing pulmonary edema. It can discriminate cardiac from other causes of lung infiltrates like acute respiratory syndrome and pneumonia. Albeit very well studied2,3,4,5,6, BNP and Pro BNP still have some limitations particularly when they are used in follow ups as results of assays may be affected by several factors related to age, gender, body mass, renal function and exercise, all of which may limit its utility for accurately stratifying some patients with acute heart failure9,10,11,12,13,14.
(Hs-cTn) has been suggested to play a role in predicting early onset of heart failure in asymptomatic patients15,16 and as a marker of myocardial injury in patients with the first ever presentation of heart failure, based on the Biomarker for Cardiovascular Risk Assessment in Europe consortium (BIOMAReCare) Hs-cTn shows its independence for the prognosis of HF17,18,19,20.
In this study we ought to find the added value of Hs-cTn in patients presented acutely to the emergency room with dyspnea and highly elevated Pro BNP and its impact on predicting death and re-hospitalization over 12-month time.
Methods
Cohort prospective study with inclusion criteria of adults above the age of 18, with suspected acute pulmonary edema due to heart failure and elevated -Pro BNP > 1000 pg/ml. Study was approved by the Institutional Review Board (IRB) of Dr Sulaiman Alhabib Medical Group holding approval number HAP-01-R-082, all experiments were performed in accordance with relevant guidelines and regulations and was Health Insurance Portability and Accountability Act (HIPPA) complaint, an informed consent was obtained from all subjects and/or their legal guardian(s). After recruitment, Hs-cTn plasma level was assessed in addition to other laboratory investigations including creatinine, as well as hemoglobin level. All patients underwent chest Xray at presentation. X-rays were read independently by expert radiologists and patient were subclassified into overt pulmonary edema and non-overt pulmonary edema groups based on the reports’ results and were followed for 12 months. Mean of all variances were calculated and analysis of variance (ANOVA) was conducted for non-continuous variables, while (t-test was used for continuous non categorical variables, using 95% power level, looking for p < 0.05 of significance.
During follow up patient’s data were collected including echocardiographic findings, additional special interventions including aggressive medical therapy and revascularization with Percutaneous intervention (PCI) or Bypass surgery (CABG), primary end point was mortality from heart failure and secondary endpoint was need for rehospitalization. Patients who lost follow up were censored and results were not counted in the final analysis. (Fig. 1) explains the study design. Hs-cTns were measured using (Abbott Laboratories; Chicago, IL) with reference range values of (0.004–0.028 ng/ml) and the prohormone brain natriuretic peptide (Pro BNP) was assessed via Elisa immunoassay with 460 pg/ml been the cut value of elevated hormones, we used 1000 pg/ml to avoid borderline positive tests. We did not look at repeated levels of troponins or pro BNP in subsequent presentations as this demonstrated in previous study to be of less predictive value (Fig. 1).
Results
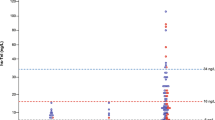
After 12 months follow up and a mean of 180 days, 95 patients were recruited of which 64 were with non-overt pulmonary edema (non-PE) and 31 with pulmonary edema (PE), mean age was 78 ± 6 and 68 ± 6, males were 51 and 50% on each group. Mean Pro BNP levels were 6148, 5927 pg/ml while Hs-cTn were 19.27 and 0.17 ng/ml respectively (baseline values for both biomarkers are depicted in Fig. 2), mean Body mass index (BMI) of 35 and 29.8, for each group. Other risk factors and clinical findings are depicted on (Table 1), of note there were more cases of atrial fibrillation in the non-overt pulmonary edema group compared to the overt pulmonary edema 41vs 19%. Mean creatinine and hemoglobin blood levels were comparable between both studied groups.
Baseline values of Pro-Bnp and high sensitivity troponin. (A) Baseline values of Pro Bnp. X axis represents Pro BNP range values, Y axis represents the number of subjects under each range. (B) Baseline values of Hs-CTnI. X axis represents Hs-cTn I range values, Y axis represents the number of subjects under each range.
Echocardiographic findings revealed no significant difference in overall ejection fraction with mean values around 47%, similarly the left atrial size, early diastolic to late diastolic mitral inflow doppler velocity (E/A) ratio, Tricuspid Regurgitation (TR) jet velocity were equivalent between both groups, two exceptions were observed including high Early mitral inflow velocity to early mitral tissue doppler annular velocity E/e’ of 30 compared to 7 in favor of PE group, and the regionality on resting echo was higher among patients in PE group in at least 50% of cases vs only 26% in the non PE (Table 2).
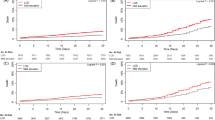
For endpoints, we identified 4 mortalities related to heart failure (cardiogenic shock) in the PE compared to 1 in non-PE cohorts, for secondary endpoint 12 cases were hospitalized in the span of 365 days in PE, compared to only 7 in the non-PE. The odd ratios were 8.5 and 4.8 m, p = 0.003 and 0.008 respectively (Table 3), in the COX proportional hazard regression covariate analysis, 7 (covariates) factors were suspected to predict poor outcomes including Pro BNP, Troponin, Creatinine, and diabetes mellitus in addition to E/e’ ratio regionalities and overt pulmonary edema on Xray at the time of presentation , Hs-cTn was the only significant predictor, Hs-cTn is more sensitive and specific compared to Pro BNP in layering the risk of death and accurately predicting poor outcomes, receiver operator curves were obtained for both and depicted on Figs. 3 and 4 with omnibus multivariate logistic regression statistic showed significant p = 0.001, cumulative survival and hazard risk with mean (Hs-cTnI) of 17 has been depicted in Fig. 5.
Furthermore, need for revascularization was assessed, with 3 vs 7 patients underwent Coronary artery bypass surgery (CABG) and 8 vs 12 patient had Percutaneous Coronary Intervention (PCI) in PE and Non-PE group, respectively. Risk of stroke were similar over all between PE and non-PE groups’ but higher in the subgroup of patient who underwent CABG at 2% compared to overall of 1%. Patients were placed on good medical therapy throughout the study with excellent rate of compliance of more than 85% of cases and were followed in heart function clinic. Patient with reduced ejection fraction < 45% or overt pulmonary edema were treated with diuretics & goal directed medical therapy to reduce mortality and rehospitalization using angiotensin receptor-neprilysin inhibitor (ARNI) or angiotensin blockers with maximum tolerated dose, in addition to beta blockers, aldosterone antagonists and sodium-glucose cotransporter-2 inhibitors. SGLT-2 inhibitors. Those with renal impairment were placed on combination therapy of hydralazine and long-acting nitrate.
Discussion
Although both were studied before, the added value of Hs-cTn to BNPs is an area that is still under scrutiny21,22,23. The study shed lights on the value of adding one to another in further predicting hard endpoints of heart failure related death and re-hospitalization. There are no “perfect” tests but in this scenario Hs-cTns were “perfect” with sensitivity of 96%. The depicted ROC (receiver operator curves) speaks to this effect very illustratively.
We believe the findings of this trial is unique and may be practice changing for treating patients with acute heart failure. We have selected extremely high-risk patients with quite elevated level of pro Bnp > 1000 and we further stratify them using Hs-cTns and radiological evidence of pulmonary edema, both biomarkers are measured in the laboratories and their blood levels are pathophysiologically explained. BNPs are produced due to stretching effect of the myocardial tissue while high sensitivity troponins are released in blood stream in response to direct damage to the myocardium24,25. Translating the laboratories finding to clinical practice was in keeping with the clinical outcomes of patients in this trial, as myocardial damage (measured by high sensitivity Troponins) is more of a surrogate marker compared to the stretching effect causing (Pro BNP elevation).
Despite the novel finding of the trial, there are quite few limitations of the study that need to be highlighted, including small numbers of patients in both groups leading to wide confidence intervals and reducing the power of the study, the selection bias related to open label protocol, and potential lab errors related to sample drawn. The number of patients is low but the events rate over one year, with the clinical characteristics reported, is high, could simply be a chance finding in a small cohort. We used only baseline level of troponin and Pro BNP to assess prognosis without follow-up values, as this has shown to be more predictive of poor outcomes in previous study26. We did not repeat cardiac troponin level in post recruitment presentations to avoid dilutional effect of intervention on blood level of pro BNPs and troponins.
The study seems to touch upon major factors of increasing risk of deaths in patients with heart failure including risk factors of ischemic heart disease, reduced ejection fraction, elevated filling pressure by echo criteria and radiological evidence of pulmonary edema, however the study was not powered to look at the impact of all these factors in the small size sample of patients recruited, making it very difficult to compare its utility in addition to Hs-cTns.
Focusing on predicting outcomes is important aspects of proper management of patient with heart failure as outlined in most recent guidelines, where class A is defined as patient at risk of heart failure but not yet diagnosed to have heart failure27, adding Hs-cTns to the paradigm of heart failure management may be of value to tailor more aggressive surveillance and more strict management protocol that will help improve survival and outcomes.
The trial served its purpose very well, the drop-out rate was 5%, and results were clinically significant even with the inherited limitations we have alluded to. Further study with large numbers of patients is needed to address the same question but in the setup of other factors or other novel markers, the later may be better in refining the risk assessment tool of patient with first time presentation of heart failure.
Conclusions
In this small cohort of patient with acute pulmonary edema due to heart failure, high sensitivity cardiac troponins were successful in predicting poor outcomes related to death and hospitalization, Hs-cTn has odd ratio of 8.5 and 4.3 in predicting both respectively despite equal mean level of PRO BNP and ejection fraction.
References
Gaggin, H. K. Biomarkers and diagnostics in heart failure. Biochim. Biophys. Acta. 1832(12), 2442–2450. https://doi.org/10.1016/j.bbadis.2012.12.014 (2013) ((Epub 2013 Jan 9)).
Zelt, J. G. E. et al. N-terminal Pro B-type natriuretic peptide and high-sensitivity cardiac troponin T levels are related to the extent of hibernating myocardium in patients with ischemic heart failure. Can. J. Cardiol. 33(11), 1478–1488. https://doi.org/10.1016/j.cjca.2017.06.012(Epub (2017).
Madan, N. et al. Relation of isolated systolic hypertension and pulse pressure to high-sensitivity cardiac troponin-T and N-terminal pro-B-type natriuretic peptide in older adults (from the atherosclerosis risk in communities study). Am. J. Cardiol. 124(2), 245–252. https://doi.org/10.1016/j.amjcard.2019.04.030 (2019).
Alawieh, H., Chemaly, T. E., Alam, S. & Khraiche, M. Towards point-of-care heart failure diagnostic platforms: BNP and NT-proBNP biosensors. Sensors 19(22), 5003. https://doi.org/10.3390/s19225003 (2019).
Martindale, J. L. et al. Diagnosing acute heart failure in the emergency department: A systematic review and meta-analysis. Acad. Emerg. Med. 23(3), 223–242. https://doi.org/10.1111/acem.12878 (2016) ((Epub 2016 Feb 13)).
Madamanchi, C., Alhosaini, H. & Sumida, A. Obesity and natriuretic peptides, BNP and NT-proBNP: Mechanisms and diagnostic implications for heart failure. Int. J. Cardiol. 176(3), 611–617. https://doi.org/10.1016/j.ijcard.2014.08.007 (2014) ((Epub 2014 Aug 9)).
Maisel, A. S., Duran, J. M. & Wettersten, N. Natriuretic peptides in heart failure: Atrial and B-type natriuretic peptides. Heart Fail Clin. 14(1), 13–25. https://doi.org/10.1016/j.hfc.2017.08.002 (2018).
Myhre, P. L. et al. B-type natriuretic peptide during treatment with sacubitril/valsartan: The PARADIGM-HF trial. J. Am. Coll. Cardiol. 73(11), 1264–1272. https://doi.org/10.1016/j.jacc.2019.01.018 (2019) ((Epub 2019 Mar 4)).
Hill, S. A. et al. Use of BNP and NT-proBNP for the diagnosis of heart failure in the emergency department: A systematic review of the evidence. Heart Fail Rev. 19(4), 421–438. https://doi.org/10.1007/s10741-014-9447-6 (2014) ((Erratum. In: Heart Fail Rev. 2014 Aug;19(4):565)).
Patel, A. N. BNP-response to acute heart failure treatment identifies high-risk population. Heart Lung Circ. 29(3), 354–360. https://doi.org/10.1016/j.hlc.2019.02.004 (2019) ((Epub 2019 Feb 26)).
Abuzaanona, A. & Lanfear, D. Pharmacogenomics of the natriuretic peptide system in heart failure. Curr. Heart Fail. Rep. 14(6), 536–542. https://doi.org/10.1007/s11897-017-0365-5 (2017).
Ibrahim, N. E. et al. Effect of neprilysin inhibition on various natriuretic peptide assays. J. Am. Coll. Cardiol. 73(11), 1273–1284. https://doi.org/10.1016/j.jacc.2018.12.063 (2019).
Zdrenghea, D. T. et al. NT-pro-BNP during isotonic and isometric exercise in heart failure patients with preserved LV ejection fraction. Clin. Lab. 60(12), 2055–2061. https://doi.org/10.7754/clin.lab.2014.140417 (2014).
van Kimmenade, R. R., Pinto, Y. M., Bayes-Genis, A., Lainchbury, J. G. & Richards, A. M. Usefulness of intermediate amino-terminal pro-brain natriuretic peptide concentrations for diagnosis and prognosis of acute heart failure. Am. J. Cardiol. 98(3), 386–390. https://doi.org/10.1016/j.amjcard.2006.02.043 (2006) ((Epub 2006 Jun 12)).
Myhre, P. L. et al. Cardiac troponin I and risk of cardiac events in patients with heart failure and preserved ejection fraction. Circ. Heart Fail. 11(11), e005312. https://doi.org/10.1161/CIRCHEARTFAILURE.118.005312 (2018).
Emdin, M. et al. sST2 predicts outcome in chronic heart failure beyond NT-proBNP and high-sensitivity troponin T. J. Am. Coll. Cardiol. 72(19), 2309–2320. https://doi.org/10.1016/j.jacc.2018.08.2165 (2018).
Yan, I. et al. High-sensitivity cardiac troponin i levels and prediction of heart failure: Results from the BiomarCaRE Consortium. JACC Heart Fail. 8(5), 401–411. https://doi.org/10.1016/j.jchf.2019.12.008 (2020) ((Epub 2020 Mar 11)).
Sato, Y., Fujiwara, H. & Takatsu, Y. Cardiac troponin and heart failure in the era of high-sensitivity assays. J. Cardiol. 60(3), 160–167. https://doi.org/10.1016/j.jjcc.2012.06.007 (2012) ((Epub 2012 Aug 4)).
Evans, J. D. W., Dobbin, S. J. H., Pettit, S. J. & Di Angelantonio, E. High-sensitivity cardiac troponin and new-onset heart failure: A systematic review and meta-analysis of 67,063 patients with 4,165 incident heart failure events. JACC Heart Fail. 6(3), 187–197. https://doi.org/10.1016/j.jchf.2017.11.003 (2018) ((Epub 2018 Jan 10)).
Nguyen, K. et al. N-terminal Pro B-type natriuretic peptide and high-sensitivity cardiac troponin as markers for heart failure and cardiovascular disease risks according to glucose status (from the multi-ethnic study of atherosclerosis [MESA]). Am. J. Cardiol. 125(8), 1194–1201. https://doi.org/10.1016/j.amjcard.2020.01.025 (2020) ((Epub 2020 Jan 30)).
Hall, C. Essential biochemistry and physiology of (NT-pro) BNP. Eur. J. Heart Fail. 6(3), 257–260. https://doi.org/10.1016/j.ejheart.2003.12.015 (2004).
Puelacher, C. et al. Combining high-sensitivity cardiac troponin and B-type natriuretic peptide in the detection of inducible myocardial ischemia. Clin. Biochem. 52, 33–40. https://doi.org/10.1016/j.clinbiochem.2017.10.014 (2018) ((Epub 2017 Nov 8)).
Garg, P. et al. Cardiac biomarkers of acute coronary syndrome: from history to high-sensitivity cardiac troponin. Intern. Emerg. Med. 12(2), 147–155. https://doi.org/10.1007/s11739-017-1612-1 (2017) ((Epub 2017 Feb 11)).
Debska-Kozlowska, A., Ksiazczyk, M. & Warchol, I. Clinical usefulness of N-terminal prohormone of brain natriuretic peptide and high sensitivity troponin T in patients with heart failure undergoing cardiac resynchronization therapy. Curr. Pharm. Des. 25(14), 1671–1678. https://doi.org/10.2174/1381612825666190621155718 (2019).
Pipikos, T. et al. Stronger correlation with myocardial ischemia of high-sensitivity troponin T than other biomarkers. J. Nucl. Cardiol. 26(5), 1674–1683. https://doi.org/10.1007/s12350-018-1199-6 (2019) ((Epub 2018 Jan 29)).
Zymliński, R. et al. Elevated troponin I level assessed by a new high-sensitive assay and the risk of poor outcomes in patients with acute heart failure. Int. J. Cardiol. 230, 646–652. https://doi.org/10.1016/j.ijcard.2017.01.012 (2017) ((Epub 2017 Jan 5)).
Yancy, C. W. et al. ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128(16), 1810–1852. https://doi.org/10.1161/CIR.0b013e31829e8807 (2013).
Author information
Authors and Affiliations
Contributions
I Dr Alhejily herein confirmed that I'm the main author for this manuscript and have contributed in the whole process of the research, including collecting data, writing the research paper with all its part to submitting it to your respected journal.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alhejily, W.A. High sensitivity Troponins In Patients with elevated prohormone of beta natriuretic peptide and acute heart failure (HIGH TRIP Trial). Sci Rep 12, 1838 (2022). https://doi.org/10.1038/s41598-022-05759-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-05759-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.