Abstract
Influenza-like illness (ILI), a disease caused by respiratory pathogens including influenza virus, is a major health concern in older adults. There is little information on changes and recovery dynamics of the nasopharyngeal (NP) microbiota of older adults associated with an ILI. Here, we compared the NP microbiota in older adults reporting (n = 240) or not (n = 157) ILI during the 2014–2015 influenza season at different times of the ILI event. A small but significant effect of the ILI was observed on the microbiota community composition and structure when compared to controls and samples collected at recovery. Corynebacterium was negatively associated with ILI and its abundance increased after recovery. Potential pathobionts such as Haemophilus, Porphyromonas and Gemella had higher abundances during acute-ILI. Stability and changes in the NP microbial community showed individual dynamics. Key core genera, Corynebacterium, Moraxella and Dolosigranulum exhibited higher inter-individual variability in acute-ILI, but showed comparable variability to controls after recovery. Participants in the ILI group with higher core microbiota abundances at the acute phase showed higher microbiota stability after recovery. Our findings demonstrate that acute-ILI is associated with alterations in the phylogenetic structure of the NP microbiota in older adults. The variation in the core microbiota suggests imbalances in the ecosystem, which could potentially play a role in the susceptibility and recovery of the NP microbiota after an ILI event.
Similar content being viewed by others
Introduction
Respiratory viral infections are a major cause for public health concern, especially due to their mode of transmission and high risk of morbidity and mortality in at risk populations such as older adults1. While vaccinations have the potential to prevent infections, their efficacy can vary based on several factors, such as ageing and the subsequent deterioration of the immune system2,3,4,5,6. Influenza-like illness (ILI) refers to a defined set of symptoms associated to the disease caused by respiratory bacterial or viral pathogens, including but not exclusively by influenza virus7. It is crucial to understand the factors that may play either a protective or pathogenic role in this respiratory disease, such as that of the commensal respiratory microbiome.
The respiratory tract harbors between 102 and 106 bacteria depending on the site, with the nasopharynx (NP) consisting of ~ 103 of bacteria8. The upper respiratory tract microbiota of older adults differs from that of middle-aged healthy adults9. These differences have been associated with, among others traits of ageing, immune-senescence, i.e., a dysregulation of the immune system occurring with age suggesting a potential role of the microbiota through interaction with the local immune response9,10,11,12. Commensal NP microbiota, can play an important role in inhibiting colonization and expansion of invading pathogens by exhibiting colonization resistance similar to what occurs in other host-associated niches13. E.g. for bacterial infections, colonization of Staphylococcus lugdunensis (a lugdunin producing bacterium) was shown to reduce Staphylococcus aureus carriage and could play a role in preventing staphylococcal infections14. Studies investigating the upper respiratory tract microbiota during influenza virus infection have identified differences between infected and non-infected individuals15,16. However, to our knowledge, information on changes in the NP microbiota during the onset of ILI and its dynamics during recovery after an ILI event in the ageing population remains under explored. A better understanding of microbiota dynamics may provide clues for potential microbial markers of recovery from ILI and susceptibility to secondary bacterial infections such as pneumonia, which is of special relevance in the ageing population.
We investigated the NP microbiota in older adults reporting an ILI event in comparison to NP microbiota in participants not reporting an ILI event throughout the 2014–2015 influenza season, considered as controls6. We used 16S rRNA gene sequencing to assess the composition of the NP microbiota in a subset of participants (n = 397) from the ILI cohort6. Controls were sampled throughout the season equally distributed over the different age groups at two timepoints, 14 days apart. Participants reporting an ILI event were sampled three times: at onset, at 14 days and at 7–9 weeks, considered as the recovery sampling phase. We observed differences in NP microbiota community composition between the ILI and control groups, indicating changes associated with acute infection. In longitudinal samples from ILI participants, the NP microbiota during recovery differed markedly from that observed during the acute phase. Our study highlights the need for further mechanistic and longitudinal studies to understand the role of the NP microbiota and its link with susceptibility as well as recovery from ILI in the ageing population.
Material and methods
Study design and participants
The participants (n = 397) in this study were part of the prospective surveillance cohort of individuals with influenza-like illness (ILI) which was previously described6,17. For this study, we included all individuals that had nasopharyngeal swabs available and reported ILI symptoms once during the 2014–2015 season as well as a control group consisting of participants with no ILI reported in the same season (see Supplementary Fig. 1). Detailed information of participants in this study is provided in Table 1. The differences in sex, age and body-mass index were tested using Fisher test, t-test, sum statistic (without blocking by stratum i.e., age and sex). For characteristics such as medications, comorbidities, presence of pathogens in the cohort we used Cochran-Mantel–Haenszel test with blocking per strata, where stratum is defined as the interaction of sex and age groups (5-year range between 60 and 90 years). Ethical clearance was obtained from the regional Medical Ethical Committee Noord Holland and written informed consent was provided by the participants. All methods including sample collection, data acquisition and analysis were performed in accordance with the relevant guidelines and regulations. This study is registered with the Netherlands Trial Registry, number NL4666.
Sample collection
Nasopharyngeal (NP) swabs were collected between Oct 1, 2014, and June 15, 2015, during the 2014–15 influenza season from participants registering an ILI event within 72 h of reporting symptoms (acute-ILI; visit-1), after 14 days (ILI-14 days; visit-2) and 7–9 weeks after the ILI event (recovery sample; visit-3). The Dutch Pel criteria was used to determine Influenza-like Illness, where having a fever (≥ 37·8 °C) with at least one other symptom such as headache, myalgia, sore throat, coughing, rhinitis, or chest pain was used to classify individuals into the ILI group6. Causative agents were identified using NP and oropharyngeal (OP) swabs by Multiplex ligation-dependent probe amplification (MLPA) or classical culture approaches (Supplementary Table 1). NP swabs were further used for microbiota profiling. Participants without any reported ILI event were used as controls and randomly sampled throughout the season (visit-1) and 14 days after their first visit (visit-2).
DNA extraction and sequencing
The DNA extraction protocol for low-biomass samples that was previously demonstrated to be robust was used to extract DNA from NP swabs with slight modifications18. We used the modified Agowa Mag DNA extraction kit (LGC genomics, Berlin, Germany). For each batch of DNA extraction, the ZymoBIOMICS Microbial Community Standard (Zymo catalog number: D6300) was 1000 × diluted and 200 µl of this diluted Zymo mock was included as positive control together with two negative controls containing only the lysis buffer. The NP FLOQSwabs® in Copan’s Liquid Amies Elution were thawed on ice and 200 µl vortexed for 10 s. For each sample, 600 µl of lysis buffer containing zirconium beads (diameter 0.1 mm, Biospec Products, Bartlesville, OK, USA) and 550 µl phenol (VWR International, Amsterdam, the Netherlands) were added. The bead-beating step was done twice for 2 min at 3500 oscillations/minute by bead beating (Mini-Beadbeater-24, Biospec Products). Between each bead-beating step, the tubes were transferred on ice for 2 min. The tubes were then centrifuged for 10 min at 4500 × g and the clear aqueous phase was pipetted and transferred to a new 2 ml Eppendorf tube that consisted of 1.3 ml binding buffer and 10 µl magnetic beads. The 2 ml Eppendorf tube was kept for shaking for 30 min at 900 RPM and then placed on a magnetic separation rack. The clear liquid was discarded and the magnetic beads were washed and dried for 15 min at 55 °C. The DNA was eluted in 35 µl elution buffer.
The rRNA V4 region of the 16S rRNA gene was amplified by dual-index PCR using the 515F (5′-GTG CCA GCM GCC GCG GTA A-3′) and 806R (5′-GGA CTA CHV GGG TWT CTA AT-3′) primers including the Illumina adapters and sample specific barcodes19,20. For PCR, we included additional DNA mocks, ATCC-MSA-2004 and an in-house DNA mock consisting of Haemophilus influenzae, Streptococcus pneumoniae, Streptococcus pyogenes (group B), Klebsiella oxytoca, Klebsiella pneumoniae, Hemolytic Streptococcus Group A, Pseudomonas aeruginosa, Staphylococcus epidermidis, Staphylococcus aureus and Moraxella catarrhalis pooled in equal ratios based on 16S rRNA gene qPCR data. Overall, DNA blanks, non-template controls (NTC), ZymoBIOMICS Microbial Community Standard (whole cell) and gDNA mocks were included in each PCR plate and sequenced alongside the samples sequenced (2 × 250 bp) with an Illumina MiSeq instrument (Illumina Inc., San Diego, CA, US) using MiSeq v2 (500 cycles) reagent kit following manufacturer’s recommendations.
Identification of amplicon sequence variants (ASVs)
All the bioinformatic analysis were done in R (v3.6.0) and RStudio (v1.1.383), unless otherwise stated21,22. For each sequencing run, raw reads were filtered, trimmed and denoised into amplicon sequence variants (ASVs) using the dada2 R package (v1.14.1)23 using default parameters, except for filterAndTrim for which we used following parameters (truncLen = c(200,150), trimLeft = c(20,22)). The creation of the ASV table was followed by removal of chimera and ASV tables were merged from individual sequencing runs.
The ASVs were assigned taxonomy using the RDP classifier and SILVA database v138 with assignTaxonomy (key parameters: minBoot = 80 and tryRC = TRUE). Species level assignments were done using the addSpecies function24,25. The resulting ASV table and taxonomic table were combined with sample data into a phyloseq (v1.30) object for downstream analysis26.
Removal of potential contaminant ASVs
In order to identify and deal with contamination from exogenous sources such as reagents, of special relevance in our low biomass samples, we included several positive and negative technical controls. The technical controls were as follows: (1) DNA extraction controls (n = 32). (2) PCR non-template controls (n = 13) and three different mock communities. Genomic DNA mixtures included an ATCC mock community (n = 15), and in-house mock community (n = 10) and the ZymoBiomics mock community (n = 53) including genomic DNA as well as whole-cell mixtures. As a first step to remove contaminant ASVs we used the prevalence methods (threshold 0.5) from the decontam R package function isNotContaminant()27. In contrast to the widely used, isContaminant approach, the isNotContaminant is stricter and focuses on identifying taxa that are not likely to be contaminants27. ASVs over-abundant in negative controls compared to true samples, and those classified as Cyanobacteria, Chloroflexi and Mitochondria were removed. Next, a co-abundance approach was used, by applying a correlation-based clustering approach for the identified blank-sample ASVs in all the data (technical controls plus NP samples). Optimal number of clusters of co-occurring taxa were identified using gap statistic with 500 permutations with fviz_nbclust() function in factoextra R package (v1.0.7) using the hcut method and visualized using aheatmap() function in the NMF R package (v0.22.0)28,29. To check for consistency in the 9 clusters that were identified, we split the data into training and test data by randomly subsampling 500 samples and testing clustering with mantel test function in vegan R package (v2.5.6)30.
Finally, to reduce extremely rare ASVs, we aggregated data at the phylum level and excluded the following phyla based on low abundance (< 0.02) and prevalence (< 25%) in all samples combined: Synergistota, Planctomycetota, Acidobacteriota, Spirochaetota, Bdellovibrionota, Verrucomicrobiota, Gemmatimonadota, Desulfobacterota, Myxococcota Crenarchaeota, Abditibacteriota, Euryarchaeota, Halobacterota, Armatimonadota, Fibrobacterota, Nitrospirota, Dependentiae. The Bacterial Diversity Metadatabase (BacDive; https://bacdive.dsmz.de/advsearch) was used to search for genus and species epithet for the most dominant/prevalent ASVs from Fusobacteriota and Campilobacterota to confirm the source of isolation of nearest cultured representative31. Despite being prevalent (63%) and constituting 0.15% of the reads, we removed (as a rational choice) phylum Deinococcota, because ASVs from this phylum belonged to the Deinococcus-Thermus group, identified as reagent contaminants in several studies32,33,34,35.
Microbial community analysis
Phylogenetic diversity, Simpson’s evenness and beta-diversity (Generalized UniFrac and unweighted Unifrac) analyses were performed on rarefied data subsampled at 1932 reads/sample (86.5% of ASVs were retained), using R packages picante (v1.8.1), microbiome (v2.1.1) and MiSPU (v1.0)36,37,38,39,40. Association between beta-diversity and health status was assessed using a non-parametric Analysis of similarities (ANOSIM, vegan R package) with 999 permutations. Within group differences in beta-diversity (divergence) and intra-individual stability (1-GUniFrac) in microbiota was calculated based on the GUniFrac with equal weights to low and high abundant ASVs (alpha = 0.5). Proportional variability (PV) in core genus relative abundances was calculated as described previously41,42. To avoid instances where values are divided by zero, due to either detection limit or true absence of taxa in samples, we add a small constant value (1% of mean relative abundance) to relative abundances of each taxon before calculating PV. For PV calculation, in the control group we selected participants with samples for both visits, and in the ILI group only participants with all three visits were included. To avoid biases resulting from differences in number of samples between groups, we sampled 80% of the samples in each group with 999 bootstrap iterations. Taxonomic compositions were visualized using microbiomeutilities (v1.00.12), pheatmap (v1.0.12) and ggplot2 (v3.3.3) R packages43,44. Between group alpha diversity, divergence and intra-individual stability were compared using the Wilcoxon tests within the stat_compare_means function in the R package ggpubr (v0.2.5)45.
Associations with microbiota
Associations between microbiota composition and variables such as ILI status, pathogen type (bacterial or viral), medications including antibiotics and co-morbidities were carried out using the procedure described in detail previously17. Briefly, ASVs were agglomerated to genus level and those genera with minimum 0.001 relative abundance in 10% of the samples were selected for testing associations mentioned above. We used sum-statistic for testing associations between genera relative abundances and variable of interests46. The R package coin (v1.3-1) was used for statistical testing47. To reduce the effect of confounding variables such as participant age and sex, these were stratified as blocks. The Benjamin-Hochberg procedure was applied for multiple testing (false discovery rate (FDR) < 20%) to each sub-study48. The age groups were defined as 5‐year range, covering ages from 60 to 90 years.
Pairwise comparison of microbiota stability (1-GUniFrac) between visits was done using Wilcoxon rank-sum test corrected for multiple testing. Relationship of stability (1-GUniFrac) and phylogenetic diversity and sum of relative abundances of core microbiota were tested using Spearman’s correlation.
Results
Cohort description
An overview of the study design and analysis is given in Supplementary Fig. 1. 397 participants, with a mean chronological age of 70.3 (± 6.2) years were selected for this study based on availability of nasopharyngeal swabs. Of these, 157 participants (approx. 40%) did not report an ILI-event throughout the 2014–2015 influenza season, and were therefore used as controls, and 240 reported an ILI event, and were considered as the ILI group. An overview of participant information is provided in Table 1. While the majority of participants in the control (89.2%) and ILI (77.9%) groups had no additional respiratory diseases (such as asthma or COPD) at the time of sampling for this study, these were significantly higher in the ILI group.
Participants from the control group had higher rates of influenza vaccination (78.3%) than the ILI group (67.1%). Comorbidities were more frequent in the ILI group, as well as use of antibiotics and analgesics (Table 1). The most common causative agents for ILI were Influenza virus (21.2%), Rhinovirus (17.5%), Haemophilus (15.4%), and coronavirus (7.9%) (Supplementary Table 1).
Microbial community composition in the NP in the ageing population
To investigate the composition of the NP microbial community of the study participants, we first removed contaminant sequences due to high prevalence of taxa previously reported as reagent contaminants, e.g., Ralstonia, Bradyrhizobium, Mesorhizobium, Comamonadaceae (Supplementary Figs. 2 and 3). After removing these contaminants, the top three most abundant phyla, namely Actinobacteriota, Firmicutes, and Proteobacteria, accounted for 97.8% of the total composition in all samples (Supplementary Table 2). The top five genera, Corynebacterium, Moraxella, Dolosigranulum, Staphylococcus and Haemophilus contributed to 83.8% of the total (Supplementary Table 3). ASVs unclassified at the genus level contributed to 3.11% of the total. Based on genus relative abundance across samples, Corynebacterium was dominant in 48.9% of the samples, Moraxella in 20.5%, Staphylococcus in 13.9%, Dolosigranulum in 5.2%, and Haemophilus in 4% of the samples (Supplementary Table 4). In 47% of the samples, a single ASV was contributing to more than 50% of the total abundance. This suggests that the majority of ASVs detected in an individual’s NP microbiota were of low abundance.
Effect of ILI on the NP microbiota diversity and structure
To assess differences in microbial diversity and community evenness, we compared the NP microbiota between controls and the ILI group throughout the different phases of the ILI. Comparison of phylogenetic diversity (Faith’s Phylogenetic diversity, PD) revealed higher diversity in samples 14 days after ILI (mean ± sd; 13.5 ± 5.8) when compared to controls (12.0 ± 5.6), acute-ILI (12.5 ± 6.0) and samples after recovery (12.5 ± 5.9) (Fig. 1A). We observed that the NP microbiota exhibited low evenness (Simpson’s evenness, Fig. 1A), supporting our previous observation of single ASVs dominance in the NP microbiota, with higher levels observed in controls (0.11 ± 0.08) when compared to samples from 14-day after ILI (0.08 ± 0.05). However, significance of these differences disappeared after correcting for multiple testing.
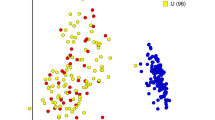
Comparison of diversity between groups. (A) Alpha diversity measures, phylogenetic diversity and evenness comparisons between groups. (B) Inter-individual variation in community composition based on generalized UniFrac distances between samples within a group. Statistical comparisons are based on Wilcoxon rank-sum test, corrected for multiple comparisons using Benjamini–Hochberg Procedure. (C) Comparison of beta-diversity between groups based on Unweighted, Generalized and Weighted UniFrac distances, with centroids and bars representing standard error across the two axis.
Within-group variation in the overall microbiota community composition and structure was different between controls and the ILI group at all time-points (Fig. 1B). This variation was higher in samples from the acute-ILI and at 14 days after when compared to controls and samples from the recovery phase. Due to the observed unevenness in the NP microbiota (Fig. 1A), we used three distance measures, i.e. unweighted, generalized and weighted UniFrac, to account for mono-dominance and rarity in NP microbiota. The microbiota composition and structure were significantly different between the control and ILI groups (Fig. 1C, Unweighted UniFrac, ANOSIM R = 0.007, Panosim = 0.02; GUniFrac, ANOSIM R = 0.08, Panosim = 0.014; Weighted UniFrac, ANOSIM R = 0.008, Panosim = 0.016), but in-line with the observed high inter-individual variation within the groups, the low values of R statistic (< 0.1) indicate that this was a small effect.
The within-group and overall high inter-individual variation observed in the beta diversity analysis (Fig. 1B, C) led us to do pairwise comparison of community dissimilarity between the control and ILI groups, as a means to control for high variability across all samples, and to potentially identify specific differences between groups. The microbiota of samples from the ILI group at the acute phase were significantly dissimilar to controls and recovery samples (Table 2). In addition, when compared to controls and recovery samples, samples from acute-ILI and ILI-14 days had significantly higher inter-individual variation in the NP microbiota (Wilcoxon rank-sum test, p.adj < 0.001, Fig. 1B). In general, in pairwise comparisons between groups, such as the control and ILI samples at the acute phase, the values of R statistic were higher than those obtained from comparisons within the ILI group, such as between recovery and acute samples (weighted Unifrac and GUnifrac). Overall, using different methods (see Table 2) these data suggest that the changes in NP microbiota during acute-ILI can be highly variable between individuals, and potentially indicative of an unstable environment, which is greatly reduced after recovery.
NP microbiota associations with ILI status
To identify compositional differences in microbial community members, we compared their relative abundances between the control and ILI groups. We observed high inter-individual variation in relative abundances of the dominant phyla, as seen in the distribution pattern for each of the groups (Fig. 2A). At the phylum level, when compared to the control group, the microbiota of acute-ILI and 14-day after ILI had lower abundance of Actinobacteriota (Wilcoxon rank-sum test, p.adj < 0.05, Fig. 2A). Proteobacteria were higher in samples from acute-ILI and ILI-14 day compared to controls, while samples from the recovery phase showed no significant differences when compared to controls.
Comparison of phylum level abundances and Corynebacterium/Moraxella ratio. (A) Relative abundances of the top four phyla were compared between groups using Wilcoxon rank-sum test, corrected for multiple comparisons using Benjamini–Hochberg Procedure. (B) Corynebacterium/Moraxella relative abundance ratio was compared between groups using Wilcoxon rank-sum test, corrected for multiple comparisons using Benjamini–Hochberg Procedure.
Overall, the two most dominant genera, Corynebacterium and Moraxella showed a negative correlation (Spearman’s rho = − 0.3728436, P ≤ 2.2e−16) potentially indicative of an anti-occurrence of these groups. Comparison of the Corynebacterium/Moraxella ratio suggested a significantly higher ratio in the control group when compared to acute-ILI and ILI-14 days but not with the ILI-recovery group (Fig. 2B).
We then tested for associations between the NP microbiota with having an ILI. Due to the intrinsic differences in our study groups, all associations were corrected for age and sex as potential confounders. Four genera were differentially abundant between the control samples and samples from acute-ILI. Among these, Corynebacterium showed a negative association, while Haemophilus, Gemella and Porphyromonas showed a positive association with acute-ILI (Fig. 3A, C). Corynebacterium, Haemophilus, and Gemella were not associated with other factors known to affect the upper respiratory tract microbiota, such as medication, smoking or other co-morbidities (including respiratory or cardiac disease(s), diabetes, kidney transplant, autoimmune diseases, asplenia, leukemia, lymphatic cancer and/or malignancies). However, Porphyromonas, positively associated with ILI, was negatively associated with use of alpha- & beta-blockers, other co-morbidities and respiratory diseases. Due to its association with medication and co-morbidities, its higher abundance in acute-ILI could not be directly associated with the acute-ILI event.
Haemophilus colonization (infection assessed by positive culture) was positively associated with Haemophilus 16S rRNA gene relative abundances at the acute-ILI phase, with colonized individuals showing high abundance even at the 14-day sample, and abundances after recovery were largely reduced (Supplementary Fig. 6).
NP microbiota associations with health-related parameters independent of ILI
Our study population consists of older adults who are diagnosed with a variety of disease/disorders and are using medications that could potentially act as confounders. Therefore, we investigated potential associations with NP microbiota and other health related parameters and medications. Staphylococcus abundances were negatively associated with Angiotensin receptor blocker, while Anaerococcus and Prevotellaceae were negatively associated with autoimmune disease. Several genera found negatively associated with statins had low prevalence in both ILI (acute phase) and control groups (Fig. 3B). Smoking in the last 3 months was positively associated with relative abundances of Streptococcus, Vellionella, Rothia, Prevotella and Leptotrichia, however, the latter had low prevalence in both groups. These data suggest the need for investigating potential interactions between medications and NP microbiota, of especial interest in at-risk populations such as older adults, with high prevalence of co-morbidities and polypharmacy.
Dynamics of the NP core microbiota during ILI
In host-associated microbial communities, members of the core microbiota can be viewed as stably-associated with the host. Since we observed high within-group variability in our study groups, we focused our analysis on the dynamics of the core-microbiota. We hypothesized that, in absence of ILI, the members of the core microbiota may exhibit lower inter-individual variability compared to acute-ILI, and can serve as a marker for recovery from the disease. For this analysis, we used paired samples of participants from the control (two visits, n = 78) and ILI group (3 visits, n = 81). This allowed us to investigate variability in core microbiota abundances between visits in each of the study groups. We identified 14 genera present in 75% of samples with at least 0.00001% relative abundance (Fig. 4A). Within the core genera members such as Anaerococcus, Peptoniphilus, Corynebacterium, Rothia and Prevotella, variation in abundances at the ASV level was observed between the ILI (acute phase) and control groups (Supplementary Fig. 7). To test whether core genera showed variation in their abundance depending on the disease status, we calculated the variation in relative abundance of each core genera within a group using proportional variability (PV). Comparison of PV of core genera between groups revealed higher variation in abundances of the more dominant and prevalent genera, i.e., Corynebacterium, Dolosigranulum, Haemophilus, Moraxella, and Rothia, during of the acute phase of the ILI event (Fig. 4B).
Notably, the PV values for Corynebacterium and Haemophilus genera within the ILI samples at the recovery phase were more similar to the control group. On the contrary, Staphylococcus and Streptococcus had lower variability in ILI groups when compared to controls. These data suggest that the onset of ILI is characterized by variation in abundances of the dominant core genera, which is largely restored after recovery from the disease.
Stability of the NP microbiota with and without ILI
Longitudinal stability of the microbiota is associated with resistance to pathogens and resilience to perturbations and is often suggested to have a positive association with diversity49. We therefore investigated the relationship between stability of the NP microbiota with disease status and phylogenetic diversity. To this end, we calculated stability, defined as 1- GUniFrac dissimilarity, between paired samples in the absence of ILI (n = 78) and during an ILI (n = 81). No significant difference in stability was observed between visits for the control and ILI groups (Fig. 5A). However, in both groups there was a large inter-individual variability in microbiota stability between visits (Fig. 5A, B). Notably, in the control group there was a negative correlation between phylogenetic diversity (PD) on the first visit and microbiota stability (Fig. 5C), also observed between samples from acute-ILI (v1) compared with 14 day and recovery visit microbiota.
Associations of stability and diversity. (A) Comparison of microbiota stability between visits. Here for control group, visits are randomly carried out throughout the influenza season, with 14 days intervals between first (v1) and second (V2) visit. For the ILI group, v1 is the acute-phase of ILI, v2 is 14 days later and v3 is visit between 7 and 9 weeks after v1. (B) Depicts individuals categorized into three groups based on the stability of microbiota between visits. Each line connects observations for an individual to demonstrate differences between visits. (C) Spearman’s correlation between stability (1-GUniFrac) and Phylogenetic diversity. (D) Spearman’s correlation between stability (1-GUniFrac) and relative abundance of core microbiota.
Analysis of proportional variability indicated that the acute-ILI was associated with higher variability in relative abundances of key core microbiota members compared to controls. We further investigated whether the observed microbiota stability was associated with the relative contribution of core members (core abundance) to the total community abundance. We observed that higher core abundance was associated with higher stability between visits in the control group, as well as between acute-ILI (visit-1) with 14 days (visit-2) and with recovery phase (visit-3) respectively (Fig. 5D). However, core abundances did not correlate with stability between 14 days (visit-2) and recovery stage (visit-3), indicative of a more unstable environment in the early phase of recovery from the disease.
Discussion
Here we studied the NP microbiota in older adults during an influenza-like illness event. We evaluated the differences in the NP microbiota in those not reporting an ILI event throughout the 2014–2015 influenza season with those reporting an ILI event, sampled during the acute phase of ILI (< 72 h after report), 14 days after and 7–9 weeks after the onset of ILI, considered as the recovery phase. Acute ILI was associated with differences in microbiota community and structure when compared to controls and recovery samples. The NP microbiota exhibited high inter-individual differences in dynamics from onset to recovery from ILI. Dominant core genera showed higher variability in acute-ILI and 14 days after ILI when compared to controls, indicative of an unstable microbiota environment in the early days of reporting an ILI event.
Micro-niches within the upper-respiratory tract are occupied by distinct microbial communities and diverse bacteria can co-exists in the NP8,9. Anatomically, the NP is located above the oral cavity and can be blocked during respiratory infections due to nasal congestion. Moreover, local changes in inflammatory responses may influence the habitability of NP by microbes. Thus, changes in these micro-niches can occur during respiratory infections thereby potentially impacting the commensal microbiota through proinflammatory responses or shortage of nutrients50,51. Acute-ILI was characterized by higher abundances of Proteobacteria and lower abundances of Actinobacteriota and Firmicutes. Similar observations have been previously reported in individuals with upper respiratory tract viral infections15. Notably, Actinobacteriota and Firmicutes had higher abundances after recovery from ILI, further suggesting that these phyla are negatively associated with ILI at the acute phase and are largely restored after disease52. At the genus level, the Haemophilus, Gemella and Porphyromonas genera were positively associated with acute-ILI. Haemophilus was more abundant in infected individuals compared to non-infected individuals within the ILI group at the acute phase. Haemophilus was also more abundant in samples collected 14 days after the acute-ILI and only reduced after recovery from the ILI, likely suggesting a reduction of the pathogenic variant at a later phase of recovery from ILI. Previously, Haemophilus influenzae was detected in samples collected at the recovery phase as well as in control samples in this cohort6. Species or strain typing for H. influenzae or H. haemolyticus is challenging using short-amplicon sequencing approaches as used in this study, however, the overall positive association confirms the biological signal captured in our analysis. The genus Gemella is widely considered as a commensal of the respiratory niche, however, there is evidence for it being a potential opportunistic pathogen in older adults53. Similarly the genus Porphyromonas, more abundant in acute-ILI compared to controls, has been associated with pro-inflammatory responses54,55. Notably, the gut microbiota of individuals with acute-ILI was previously reported to harbor a pro-inflammatory profile17. Overall, based on our observations we hypothesize that ILI might promote expansion of pro-inflammatory bacteria, as previously shown for the gut microbiota, also locally within the respiratory tract. In addition, previous studies have observed an association between the nasal microbiota and inflammatory responses during infections9,56. Therefore, future studies should investigate the dynamic interactions between immune system and the microbiome associated with ILI.
Corynebacterium, that belongs to the Actinobacteriota phylum, was the only genera that had a negative association with acute-ILI. Corynebacterium is proposed as one of the keystone species in the upper respiratory tract, mainly due to its positive association with health8,57. Majority of the previous studies of the NP microbiota included children and adults (< 65 years age), but a recent study during influenza virus infection across age-groups (including older adults, n = 66) observed a lower prevalence of Corynebacterium16. Our observation of lower abundances of Corynebacterium during ILI at the acute phase, and its increase after recovery from the disease in participants > 60 years of age, indicates a potential life-long key role for Corynebacterium and related species with health in the upper respiratory tract. Future studies investigating the mechanistic role of Corynebacterium in the upper respiratory tract are need to better understand the impact of this bacterium in human health.
Our study included a population of older adults (> 60 years of age) with high prevalence of polypharmacy and co-morbidities. While interactions between the nasopharyngeal microbiota and different medications is limited, recent studies on the impact of the gut microbiome on drug metabolism have highlighted its importance for human health58. Because of the high prevalence in polypharmacy and comorbidities in our cohort, we performed all association studies with these variables, and studied how these results would relate to those found for the ILI event. We did not observe any genera associated with antibiotics usage, which was significantly higher in ILI group. However, in this study we did not consider timing of antibiotic usage (i.e. either taken before or due to the ILI), which can have a potential impact on the recovery dynamics of the NP microbiota and therefore needs further investigation. Notably, statins usage (which was significantly higher in ILI group, Table 1), was negatively associated with four genera, none of which showed associations with the ILI after correcting for multiple testing (Fig. 3A). Statins have anti-inflammatory properties and are proposed to have a potential protective role on seasonal influenza patients59. We observed core genera such as Dolosigranulum negatively associated with a number of medications. However, the biological significance of these associations will require more mechanistic studies to better understand the NP microbiome-drug interactions, of especial relevance in the context of the aging population.
A previous study suggested that core upper respiratory tract microbiota is perturbed during influenza A virus infection15. The core microbiota represents taxa that are highly prevalent, likely due to their adaptation to a particular ecosystem, and could play a vital role in maintaining stability and therefore health60,61. Hence, any variation in the core microbiota could suggest imbalances in the ecosystem, leading to susceptibility for disease or simply serving as a biomarker of disease. Therefore, we compared the variability in the core microbiota in our cohort. To this end, we quantified the inter-group variability in core microbiota using a non-parametric measure, Proportional Variability (PV)41,42. PV can be a better estimate of variability for quantities undergoing very different dynamics, in our study, relative abundances of core bacterial taxa. Although it is difficult to estimate a range of abundance values for bacteria that can be considered as “healthy”, variability within groups can serve as markers for perturbation, as suggested in the analogy with Anna Karenina principle62. We observed higher variability within the ILI group at the early phases (acute and 14 days) for dominant and prevalent taxa such as Corynebacterium, Moraxella and Dolosigranulum, which have been previously associated with a “healthy” NP microbiota8. Lower variability of core genera such as Streptococcus and Staphylococcus was observed in the ILI group compared to the control group. This indicates that some core bacteria are strongly or similarly selected during ILI in the majority (if not all) of the diseased participants, thus showing lower variability within the diseased group. In addition, the differences in abundances we observed at ASV level likely indicate the importance of different clades of dominant groups e.g. Moraxella and Corynebacterium that may be associated with health or disease. Furthermore, pathogenic strains within Streptococcus and Staphylococcus genera can cause complications and exacerbate respiratory infection63. There is a need for investigating strain-level variation between pathogenic (non-core) strains and core strains of Streptococcus and Staphylococcus, which could illuminate the potential impact of strain variation on host-susceptibility to infection.
The longitudinal analysis of beta-diversity indicated that the stability (1- GUniFrac) of the overall microbial community was variable between visits, independently of the disease status. A negative association between phylogenetic diversity, a measure of biodiversity, and stability in the absence of ILI suggests that individuals with higher phylogenetic diversity exhibit a more variable microbiota composition. This is contrary to the widely reported diversity -stability relationship and requires further investigation in the context of upper respiratory microbiota and its importance in host-health. The abundance of core microbiota was associated with higher stability in controls and also between acute-ILI and other visits. This suggests that the core microbiota at the acute phase of ILI potentially plays a critical role in stability and therefore recovery of the NP microbiota, especially 7–9 weeks after the onset of ILI.
Conclusion
Investigation of the NP microbiota in the older adult population suggests that onset of ILI is accompanied by changes in the microbiota. Potential pro-inflammatory bacteria increase in abundances during acute-ILI. Some strains belonging to genera such as Haemophilus, Streptococcus and Staphylococcus consists of strains that are known causative agents of secondary infections related to complications of ILI in the aging population64. Increased abundances of Gemella and Prophyromonas in acute-ILI suggests that there is a need to investigate the role of these bacteria during ILI. Variability in core microbiota can be viewed as a potential biomarker of ILI, indicating that higher core microbiota abundance during onset of ILI is associated with higher resilience to changes during recovery stage. Future studies should focus on the role of core NP microbiota in determining the susceptibility to ILI and its influence on recovery. For this, a trans-domain integrated approach will be crucial to better understand the three-way interaction between core microbiota-host immune system-viral infection outcome.
Ethics declarations and consent to participate
Ethical clearance was obtained from the regional Medical Ethical Committee Noord Holland and written informed consent was provided by the participants. This study is registered with the Netherlands Trial Registry, number NL4666.
Data availability
Raw sequencing data analyzed in this study are deposited at European Nucleotide Archive database under the study accession number PRJEB46215. The R code and scripts used to analyze the data are available from the GitHub repository https://github.com/RIVM-IIV-Microbiome/ILI-Respiratory-Microbiota-2021. Information pertaining to participant data is available following institutional regulations.
References
Wood-Charlson, E. M. et al. The national microbiome data collaborative: Enabling microbiome science. Nat. Rev. Microbiol. 18, 313–314. https://doi.org/10.1038/s41579-020-0377-0 (2020).
Darvishian, M., Bijlsma, M. J., Hak, E. & van den Heuvel, E. R. Effectiveness of seasonal influenza vaccine in community-dwelling elderly people: A meta-analysis of test-negative design case-control studies. Lancet. Infect. Dis. 14, 1228–1239 (2014).
Nichol, K. L., Heilly, S. J., Greenberg, M. E. & Ehlinger, E. Burden of influenza-like illness and effectiveness of influenza vaccination among working adults aged 50–64 years. Clin. Infect. Dis. 48, 292–298 (2009).
Jefferson, T. et al. Efficacy and effectiveness of influenza vaccines in elderly people: A systematic review. The Lancet 366, 1165–1174 (2005).
Monto, A. S., Hornbuckle, K. & Ohmit, S. E. Influenza vaccine effectiveness among elderly nursing home residents: A cohort study. Am. J. Epidemiol. 154, 155–160 (2001).
Van Beek, J. et al. Influenza-like illness incidence is not reduced by influenza vaccination in a cohort of older adults, despite effectively reducing laboratory-confirmed influenza virus infections. J. Infect. Dis. 216, 415–424 (2017).
Fitzner, J. et al. Revision of clinical case definitions: Influenza-like illness and severe acute respiratory infection. Bull. World Health Organ. 96, 122 (2018).
Man, W. H., de Steenhuijsen Piters, W. A. & Bogaert, D. The microbiota of the respiratory tract. Nat. Rev. Microbiol. 15, 259–270 (2017).
Kumpitsch, C., Koskinen, K., Schöpf, V. & Moissl-Eichinger, C. The microbiome of the upper respiratory tract in health and disease. BMC Biol. 17, 87 (2019).
deSteenhuijsenPiters, W. A. et al. Dysbiosis of upper respiratory tract microbiota in elderly pneumonia patients. ISME J. 10, 97–108 (2016).
Whelan, F. J. et al. The loss of topography in the microbial communities of the upper respiratory tract in the elderly. Ann. Am. Thorac. Soc. 11, 513–521 (2014).
Franceschi, C. et al. Inflamm-aging: An evolutionary perspective on immunosenescence. Ann. N. Y. Acad. Sci. 908, 244–254 (2000).
Brugger, S. D., Bomar, L. & Lemon, K. P. Commensal–pathogen interactions along the human nasal passages. PLoS Pathog. 12, e1005633 (2016).
Zipperer, A. et al. Human commensals producing a novel antibiotic impair pathogen colonization. Nature 535, 511–516 (2016).
Kaul, D. et al. Microbiome disturbance and resilience dynamics of the upper respiratory tract during influenza A virus infection. Nat. Commun. 11, 1–12 (2020).
Ding, T. et al. Microbial composition of the human nasopharynx varies according to influenza virus type and vaccination status. MBio 10, e01296-e11219 (2019).
Fuentes, S. et al. Associations of faecal microbiota with influenza-like illness in participants aged 60 years or older: An observational study. Lancet Healthy Longevity 2, e13–e23 (2021).
Biesbroek, G. et al. Deep sequencing analyses of low density microbial communities: Working at the boundary of accurate microbiota detection. PLoS ONE 7, e32942 (2012).
Bosch, A. A. et al. Development of upper respiratory tract microbiota in infancy is affected by mode of delivery. EBioMedicine 9, 336–345 (2016).
Caporaso, J. G. et al. Global patterns of 16S rRNA diversity at a depth of millions of sequences per sample. Proc. Natl. Acad. Sci. 108, 4516–4522 (2011).
Racine, J. S. (JSTOR, 2012).
Team, R. C. R: A language and environment for statistical computing (2013).
Callahan, B. J. et al. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods 13, 581–583 (2016).
Wang, Q., Garrity, G. M., Tiedje, J. M. & Cole, J. R. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl. Environ. Microbiol. 73, 5261–5267 (2007).
Quast, C. et al. The SILVA ribosomal RNA gene database project: Improved data processing and web-based tools. Nucleic Acids Res. 41, D590–D596 (2012).
McMurdie, P. J. & Holmes, S. phyloseq: An R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE 8, e61217 (2013).
Davis, N. M., Proctor, D. M., Holmes, S. P., Relman, D. A. & Callahan, B. J. Simple statistical identification and removal of contaminant sequences in marker-gene and metagenomics data. Microbiome 6, 1–14 (2018).
Kassambara, A. & Mundt, F. Package ‘factoextra’. In Extract and Visualize the Results of Multivariate Data Analyses 76 (2017).
Gaujoux, R. & Seoighe, C. A flexible R package for nonnegative matrix factorization. BMC Bioinform. 11, 1–9 (2010).
Dixon, P. VEGAN, a package of R functions for community ecology. J. Veg. Sci. 14, 927–930 (2003).
Reimer, L. C. et al. Bac Dive in 2019: Bacterial phenotypic data for high-throughput biodiversity analysis. Nucleic Acids Res. 47, D631–D636 (2019).
Eisenhofer, R. et al. Contamination in low microbial biomass microbiome studies: Issues and recommendations. Trends Microbiol. 27, 105–117 (2019).
Karstens, L. et al. Controlling for contaminants in low-biomass 16S rRNA gene sequencing experiments. MSystems 4, e00290 (2019).
Salter, S. J. et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 12, 87 (2014).
Stinson, L. F., Keelan, J. A. & Payne, M. S. Identification and removal of contaminating microbial DNA from PCR reagents: impact on low-biomass microbiome analyses. Lett. Appl. Microbiol. 68, 2–8 (2019).
Kembel, S. W. et al. Picante: R tools for integrating phylogenies and ecology. Bioinformatics 26, 1463–1464 (2010).
Lahti, L. & Shetty, S. (2018).
Wu, C., Chen, J., Kim, J. & Pan, W. An adaptive association test for microbiome data. Genome Med. 8, 1–12 (2016).
Chen, J. et al. Associating microbiome composition with environmental covariates using generalized UniFrac distances. Bioinformatics 28, 2106–2113 (2012).
Lozupone, C., Lladser, M. E., Knights, D., Stombaugh, J. & Knight, R. UniFrac: An effective distance metric for microbial community comparison. ISME J. 5, 169–172 (2011).
Heath, J. P. & Borowski, P. Quantifying proportional variability. PLoS ONE 8, e84074 (2013).
Heath, P. Quantifying temporal variability in population abundances. Oikos 115, 573–581 (2006).
Kolde, R. & Kolde, M. R. Package ‘pheatmap’. R package 1, 790 (2015).
Wickham, H. ggplot2. Wiley Interdiscip Rev Comput Stat 3, 180–185 (2011).
Kassambara, A. & Kassambara, M. A. (2020).
Ferreira, J. A. & Fuentes, S. Some comments on certain statistical aspects of the study of the microbiome. Brief. Bioinform. 21, 1487–1494 (2020).
Zeileis, A., Wiel, M. A., Hornik, K. & Hothorn, T. Implementing a class of permutation tests: the coin package. J. Stat. Softw. 28, 1–23 (2008).
Ferreira, J. & Zwinderman, A. On the Benjamini–Hochberg method. Ann. Stat. 34, 1827–1849 (2006).
Sommer, F., Anderson, J. M., Bharti, R., Raes, J. & Rosenstiel, P. The resilience of the intestinal microbiota influences health and disease. Nat. Rev. Microbiol. 15, 630–638 (2017).
Raza, M., Blackwell, C., Elton, R. & Weir, D. Bactericidal activity of a monocytic cell line (THP-1) against common respiratory tract bacterial pathogens is depressed after infection with respiratory syncytial virus. J. Med. Microbiol. 49, 227–233 (2000).
Siegel, S. J., Roche, A. M. & Weiser, J. N. Influenza promotes pneumococcal growth during coinfection by providing host sialylated substrates as a nutrient source. Cell Host Microbe 16, 55–67 (2014).
Chaban, B. et al. Characterization of the upper respiratory tract microbiomes of patients with pandemic H1N1 influenza. PLoS ONE 8, e69559 (2013).
Jayananda, S., Gollol-Raju, N. S. & Fadul, N. Gemella species bacteremia and stroke in an elderly patient with respiratory tract infection. Case Rep. Med. https://doi.org/10.1155/2017/1098527 (2017).
Chen, Y. et al. Porphyromonas gingivalis induced inflammatory responses and promoted apoptosis in lung epithelial cells infected with H1N1 via the Bcl-2/Bax/Caspase-3 signaling pathway. Mol. Med. Rep. 18, 97–104 (2018).
Guilloux, C.-A., Lamoureux, C., Beauruelle, C. & Héry-Arnaud, G. Porphyromonas: A neglected potential key genus in human microbiomes. Anaerobe 68, 102230 (2020).
Lehtinen, M. J. et al. Nasal microbiota clusters associate with inflammatory response, viral load, and symptom severity in experimental rhinovirus challenge. Sci. Rep. 8, 1–12 (2018).
Pettigrew, M. M. et al. Upper respiratory tract microbial communities, acute otitis media pathogens, and antibiotic use in healthy and sick children. Appl. Environ. Microbiol. 78, 6262–6270 (2012).
Maier, L. et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature 555, 623–628 (2018).
Atamna, A. et al. Statins and outcomes of hospitalized patients with laboratory-confirmed 2017–2018 influenza. Eur. J. Clin. Microbiol. Infect. Dis. 38, 2341–2348 (2019).
Shade, A. & Handelsman, J. Beyond the Venn diagram: The hunt for a core microbiome. Environ. Microbiol. 14, 4–12 (2012).
Shetty, S. A., Hugenholtz, F., Lahti, L., Smidt, H. & de Vos, W. M. Intestinal microbiome landscaping: insight in community assemblage and implications for microbial modulation strategies. FEMS Microbiol. Rev. 41, 182–199 (2017).
Zaneveld, J. R., McMinds, R. & Thurber, R. V. Stress and stability: Applying the Anna Karenina principle to animal microbiomes. Nat. Microbiol. 2, 1–8 (2017).
Rynda-Apple, A., Robinson, K. M. & Alcorn, J. F. Influenza and bacterial superinfection: Illuminating the immunologic mechanisms of disease. Infect. Immun. 83, 3764–3770 (2015).
Miellet, W. R. et al. Influenza-like illness exacerbates pneumococcal carriage in older adults. Clin. Infect. Dis. 73(9), e2680 (2020).
Acknowledgements
We thank all participants for their invaluable contribution to this study.
Funding
This work was supported by the Dutch Ministry of Health, Welfare and Sport, and the Strategic Program of the National Institute for Public Health and the Environment (RIVM).
Author information
Authors and Affiliations
Contributions
D.vB. and J.vB. were responsible for the ILI study. D.vB., and S.F. conceived and designed respiratory microbiota experiments. T.B. coordinated and J.G. and S.K. performed laboratory work. S.A.S. performed the microbiota analysis. S.A.S. wrote the initial draft of the manuscript with inputs from S.F. All authors contributed to interpreting the results, critically revisions of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shetty, S.A., van Beek, J., Bijvank, E. et al. Associations and recovery dynamics of the nasopharyngeal microbiota during influenza-like illness in the aging population. Sci Rep 12, 1915 (2022). https://doi.org/10.1038/s41598-022-05618-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-05618-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.