Abstract
A comprehensive analysis of clinical information in patients with chronic low back pain (CLBP) was performed to clarify the clinical characteristics of geriatric LBP from the perspective of body composition, spinal alignment, and blood findings related to senescence. We enrolled 203 patients with an average age of 79.0 years (77 men and 126 women), with non-specific CLBP as a single-center prospective cohort study, the patients were compared with age- and sex-matched controls without CLBP using a propensity score-matching. We performed laboratory analysis, radiographic evaluations for global spinal parameter and lumbar degeneration, and body composition analysis using whole-body dual-energy X-ray absorptiometry. We observed a higher red blood cell distribution width (RDW) (p < 0.001), which is an index of aging, as well as a lower vitamin D level (p = 0.002), skeletal muscle mass index (p = 0.045) and a higher fat mass (p = 0.007) in patients with CLBP. Moreover, patients with geriatric CLBP had significantly lower lumbar lordosis (p = 0.024), and higher sagittal vertical axis (p = 0.006) was correlated with lower extremity and trunk muscle mass (p < 0.001), independent of lumbar degeneration. Geriatric patients with CLBP have sarcopenic fat accumulation and spinal sagittal malalignment with senescent status, such as elevated RDW and hypovitaminosis D.
Similar content being viewed by others
Introduction
Low back pain (LBP) is one of the most frequently encountered complaints in clinical setting, and is the most common type of chronic musculoskeletal pain in Japan1. The prevalence and associated burden of LBP increase with age2; however, research on LBP has primarily focused on youths and adults, and little attention is given to the elderly population3. LBP is classified as idiopathic in approximately 85% of patients with LBP4,5 considered as non-specific LBP, irrespective of common symptoms and socioeconomic burden6. The National Institute for Health and Care Excellence defines non-specific LBP as tension, soreness, and/or stiffness of unknown etiology in the low back region with joint, disc, and connective tissue involvement potentially contributing to symptoms7. However, these lumbar spine degenerative changes are highly prevalent with age, and the mechanism whereby they cause LBP remains poorly understood. Alternatively, sagittal alignment of the whole spinal balance to maintain standing postural stability has been recognized for spinal deformity, and related research has been widely conducted8,9. Sagittal malalignment has been considered important for the pathophysiology of LBP10,11. The relationship between spinal alignment and LBP has been investigated in many clinical studies; however, there are limited and conflicting data on the effects of malalignment on LBP12, particularly for geriatric LBP with age-related degeneration of various spinal components. The aging spine, which is characterized by an anterior imbalance of the spine related to the degenerative process requires more energy leading to higher incidence of functional disorders, poor health conditions and earlier mortality13. Aging loss of skeletal muscle mass is related to spinal sagittal imbalance14. Decreased skeletal muscle mass to support the trunk and changes in the standing posture of the sagittal plane are extremely important as reasons for the high prevalence of LBP in the elderly. Therefore, it is necessary to evaluate the body composition including skeletal muscle and spinal alignment that change with aging in the study of geriatric LBP. Changes in body composition with aging in conclude a decrease in skeletal muscle mass and an increase in fat mass, and the underlying mechanism is that these changes are part of inflammation-based aging15,16.
Recent systematic reviews regarding the association between chronic inflammation and non-specific LBP have been published, suggesting that inflammatory cytokines such as TNF-α and IL-6 may be biomarkers of inflammation in the pathogenesis of non-specific LBP17,18. Chronic inflammation is well known as a senescence-associated secretory phenotype (SASP), which produces numerous proinflammatory cytokines leading to age-related inflammation (“inflammaging”)19. Age-related low muscle mass (sarcopenia) and/or intramuscular fat deposition (sarcopenic obesity), which are associated with geriatric LBP20,21, are considered part of systemic inflammation15,16. Biobank-based approaches are necessary to elucidate the senescent mechanisms of geriatric LBP; thus, Japanese Cohort Study and Biobank for Non-specific Chronic Pain (J-BINC) has been developed at the National Center for Geriatrics and Gerontology since 2018. This project was established based on clinical data systematically collected by orthopedic specialist (spine and joint surgeon) and biobanking regarding non-specific chronic pain, including LBP, neck pain, and knee pain in the elderly. Regarding chronic LBP (CLBP), most of the research reports describe the potential causes and clinical impacts from the viewpoint of spinal degeneration and malalignment22, and there are no studies that address the pathological conditions peculiar to the elderly, such as aging and sarcopenia. We conducted a comprehensive analysis of clinical information in patients with chronic LBP to clarify the clinical characteristics of geriatric CLBP from a perspective of body composition, spinal alignment and blood findings related to senescence.
Materials and methods
The study protocol was approved by the institutional review board at the National Center for Geriatrics and Gerontology (Approval Number 1229), and carries out in accordance with relevant guidelines and regulations. Written informed consent was obtained from all patients.
Patients enrollment and eligibility
This observational survey was carried out from January 2018 to April 2020 in our institute from a prospectively collected database in the J-BINC, which is a single-center prospective cohort study recruiting patients from the National Center for Geriatrics and Gerontology to assess whether non-specific chronic pain in geriatric patients shows genetic overlap with clinical findings by the discovery analysis from genome-wide association study. Individuals from both the discovery and replication samples were of Japanese background to limit biases resulting from ethnic disparities, and the clinical database of individuals from the discovery samples was drawn for this study. This cohort was a patient-based study that openly recruited individuals aged ≥ 65 years with non-specific chronic pain lasting for more than 6 months, including LBP, neck pain and knee pain. Non-specific CLBP in this study was defined as follows: (1) LBP with visual analogue scale (VAS) score for LBP ≥ 3; (2) persistent pain localized below the costal margin and above the inferior gluteal folds for more than 6 months; (3) the absence of specific spinal pathology such as infection, tumors, and vertebral fractures on both plain radiographs and lumbar magnetic resonance imaging (MRI); (4) the absence of dominant leg pain caused by radicular and cauda equina disorders; (5) the absence of prominent instability such as spondylolysis, isthmic spondylolisthesis, and degenerative spondylolisthesis more than grade II; (6) no previous lumbar and/or thoracolumbar spine surgery. Degenerated lumbar structures such as the vertebral disc, facet joint, and sacroiliac joint were omitted from the inclusion criteria because available diagnostic procedures for these conditions are inaccurate22. In addition to patients who did not meet the above inclusion criteria, we excluded patients who were unable to stand unsupported, could not evaluate VAS due to dementia and did not agree with participation in the present study.
Age/sex-matched control
The retrospective collection was conducted with data from a prospectively maintained database of Sarcopenia Study for Elderly Patient for patients who underwent whole-body dual-energy X-ray absorptiometry (DXA) and evaluated skeletal muscle mass. Registration in this database requires that whole spine radiograph, lumbar MRI, and blood data be performed within 1 year of DXA. Of 2390 patients (65–100 year, averaged 78.7 years, male 1014 patients, female 1376 patients), 1195 patients excluding lumbar degenerative disease, 683 without complaint of LBP were recruited as control participants.
Laboratory measurements
Upon enrollment, we collected fasting venous blood samples from patients in the non-specific CLBP and control groups. We recorded complete blood count parameters such as hemoglobin, mean corpuscular volume, white blood cell (WBC) count, lymphocyte count, and red blood cell distribution width (RDW). The RDW is an automated measure of the heterogeneity of red blood cell sizes due to inflammation and senescence of erythropoietic cells in the bone marrow23. Additional covariates included albumin, C-reactive protein (CRP), total cholesterol, creatinine, estimated glomerular filtration rate, and 25-hydroxyvitamin D (25-OHD). Serum 25-OHD levels were determined using electrochemiluminescence immunoassay, and 25-OHD concentration was classified as sufficient, insufficient, and deficient for values ≥ 30 ng/mL, 21–29 ng/mL, and ≤ 20 ng/mL, respectively24.
Radiographic evaluation (Fig. 1)
Spinal parameters on standing radiograph. Thoracic kyphosis (TK) and lumbar lordosis (LL) are defined as the angle between the cranial endplate of Th1 and the caudal endplate of Th12, the cranial endplate of L1 and the caudal endplate of L5, respectively. Sacral slope is defined as the angle between the sacral endplate and the horizontal plane. Sagittal vertical axis (SVA) is distance from C7 plumb line from the center of the C7 to the posterior edge of the upper sacral endplate. Pelvic tilt (PT) is defined as the angle is between the line connecting the midpoint of S1 endplate to the center of the femoral head and the vertical line of S1 endplate. Pelvic incidence (PI) is defined as the angle between the line perpendicular to the middle of the cranial sacral endplate and the line joining the middle of the cranial sacral endplate to the center of the femoral head axis.
All patients underwent conventional radiography in the standing position. For lateral films, the patients stood with their knees locked, with feet shoulder-width apart, and looking straight ahead. Measured parameters of interest included coronal Cobb angle between the superior edge of L1 and S1, lumbar lordosis (LL), thoracic kyphosis (TK), S1 slope (SS), sagittal vertical axis (SVA), pelvic tilt (PT), pelvic incidence (PI), the presence of spondylolisthesis (anterior slip > 3 mm), and the lumbar range of motion (ROM) defined as the difference in lumbar lordosis angle between flexion and extension. Spinopelvic mismatch was determined when PI-LL is more than 10°25.
Body composition analysis
Body composition was assessed using DXA (Lunar iDXA, GE-Healthcare, Tokyo, Japan). Osteoporosis was evaluated using the young adult mean on the lumbar spine (L2-4). Sarcopenia was evaluated using the appendicular lean mass derived from the sum of lean mass in the upper and lower extremities with bone mineral content removed, and skeletal muscle mass index (SMI) was calculated using height squared (kg/m2)26.
MRI evaluation
Axial T2-weighted slices at L1/2 and L4/5 were obtained to measure the cross-sectional area (CSA) of the lumbar multifidus and erector spinae muscles for the levels of L1/2 and L4/5. Paraspinal muscle CSAs for both the right and left side were added together for each participant. The CSAs were measured using an area calculation software (SYNAPSER, FUJIFILM MEDICAL, Tokyo, Japan). Vertebral endplate and intervertebral disc degeneration were evaluated based on Modic changes27 and Pfirrmann classification28. End plate and disc degeneration were defined as Modic type I, II, and III (except for type 0), and Pfirrmann grade IV and V, respectively.
Statistical analysis
We determined that a minimum sample of 394 (197 per group) would be required for a power of 90% to detect a clinically importance between-group difference of 0.35 points (with CLBP vs without CLBP in the elderly patients) in the SMI value. Assumptions for the SMI included a two-sided alpha level of 0.05 and a mean standard deviation of 1.07 points18.
Proportions and means with standard deviations (SD) for normally distributed data and median with minimum and maximum values for not normally distributed data were calculated for covariates and demographic information, moreover, categorical variables were expressed as frequencies or percentages. The chi-square or Fisher exact test was used to assess differences in categorical variables, and means were compared using independent t-test and Mann–Whitney U test for normally and non-normally distributed data, respectively. Normality was checked using the Kolmogorov–Smirnov test. To minimize the effects of potential confounding influences of measured covariates in the 2 study groups (CLBP vs. control), a propensity score-matched analysis for age and sex was applied. Finally, patients were matched 1:1 without replacement using a nearest-neighbor approach with caliper restrictions set at 0.2. A propensity score was calculated for each patient using the results of this model, regardless of the statistical significance of the independent variables in the model. The correlation between skeletal muscle mass and spinal sagittal alignment parameters were analyzed using simple linear regression analysis (Pearson correlation coefficient). Statistical analyses were performed using the EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan). A p value less than 0.05 was considered statistically significant.
Ethical approval
The device(s)/drug(s) is/are FDA approved or approved by the corresponding national agency for this indication. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. Ethical approval was given by National Center for Geriatrics and Gerontology Ethics Committee.
Results
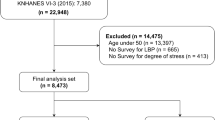
We enrolled 203 patients with CLBP with average age of 79.0 ± 6.04 years, comprising 126 (62.1%) women and 77 (37.9%) men. Among patients with CLBP, 203 patients were matched (1:1) for age and sex to control subjects (Fig. 2).
Laboratory measurements
Demographic and laboratory data of propensity score matching analysis are shown in Tables 1 and 2. There were no significant differences in anthropometry, cytometry, renal function, and nutritional condition. The RDW and the prevalence of elevated RDW were significantly higher in patients in the CLBP group than in those in the control group; however, there were no significant differences in CRP level. Serum 25-OHD levels were significantly lower in patients in the CLBP group than in those in the control group.
Body composition analysis
A comparison of body composition is shown in Table 3. Extremity muscle mass, SMI, and trunk muscle CSAs were significantly lower in patients with CLBP than in those with the control. Lower extremity fat mass and body fat ratio were significantly higher in patients with the CLBP than in those with the control.
MRI evaluation
In reference to lumbar degeneration in patients with CLBP, the frequency of lumbar spondylolisthesis was equal to that in the control and the prevalence of end plate and disc degeneration was lower in patients with CLBP than in the control group. (Table 4).
Radiographic evaluation
A comparison of spinal sagittal alignment is shown in Table 5. LL was significantly lower in patients with the CLBP than in those with the control, whereas SVA, PT, and PI-LL were significantly higher in patients with the CLBP than in those with the control group. Spinopelvic mismatch was significantly higher in patients with the CLBP group than in those in the control group. Muscle mass in both legs and trunk was negatively correlated with PT, whereas only trunk muscle mass was negatively correlated with SVA. Muscle mass in both legs and trunk was negatively correlated with PI-LL; however, trunk muscle mass was more correlated with PI-LL compared with lower extremity muscle mass. (Fig. 3).
Correlation between skeletal muscle mass and spinal sagittal alignment. Lower muscle mass in both legs and trunk was negatively correlated with PT, whereas only trunk muscle mass was negatively correlated with SVA. Muscle mass in both legs and trunk was negatively correlated with PI-LL; however, trunk muscle mass had stronger correlation with PI-LL compared with lower extremity muscle mass. The total number of plots was obtained by summing 203 cases in the CLBP group and 683 cases in the control group excluding 512 cases with LBP. PT: pelvic tilt, SVA: sagittal vertical axis, LL: lumbar lordosis, PI: pelvic incidence, PI-LL: PI minus LL.
Discussion
In the present study, high RDW related to senescence such as chronic inflammation, oxidative stress, which present in the elderly, were observed in patients with CLBP. Moreover, low lower extremity and trunk muscle mass with high body fat were observed in geriatric patients with CLBP. Previous studies have also reported an association with skeletal muscle mass reduction and LBP in the elderly18,19; thus, sarcopenia may have some impact on geriatric LBP development. However, it is unclear how lower extremity muscle mass reduction, which occurs before trunk muscle mass reduction with age29, causes LBP in the elderly. Although the relationship between trunk muscle atrophy and LBP has been previously highlighted30,31,32, it has not been concluded whether trunk muscle atrophy is the cause or result of LBP. There is a view that trunk muscle atrophy is caused by disuse, denervation, reflex suppression33,34, and there is conflicting evidence for a relationship between the morphological changes in the lumbar muscles and LBP. Age-related skeletal muscle mass reduction originates from type II fibers35; therefore, it is known that trunk muscles containing more type I fibers develop sarcopenic changes later than those in the lower extremities29. Currently, international guidelines for sarcopenia evaluation, define skeletal muscle mass as the skeletal muscle mass index (SMI), which is dependent on the muscle volume of the extremities36. The key to investigating the cause of non-specific LBP in the elderly from the perspective of aging musculature is to proceed with the analysis of geriatric LBP focusing on lower limb skeletal muscle.
Considering the pathophysiological condition of age-related skeletal muscle loss from the molecular biological mechanism of aging, senescence is associated with advanced aging in humans. Senescent cells involving irreversibly proliferative arrest can develop the SASP, consisting of proinflammatory cytokines and extracellular matrix-degrading proteins, which function as deleterious paracrine and systemic mild inflammation37. Thus, “inflammaing” is considered as a pervasive feature of aging tissue in age-related diseases17. One of the most important organs of locomotor senescence is the skeletal muscle, and sarcopenia, which is an age-related loss of muscle mass, is also considered to be a pathology associated with chronic inflammation mediated by immunosenescence38. RDW, which was significantly higher in elderly patients with CLBP in the present study, has been attracting attention as a prognostic factor for various acute and chronic diseases in recent years. This is because it represents the red blood cell size variation and reflects changes in circulatory half-life due to chronic inflammation39,40,41,42. Elevated RDW is associated with an increased risk of age-related diseases and mortality; moreover, RDW reflects overall inflammation because it is associated with overall and disease-specific mortality risk41,42. Veeranna43 and Wei44 performed comparative analyses of RDW and CRP for mortality prediction in patients with coronary heart disease and infectious endocarditis, respectively. They concluded that RDW, and not CRP, was associated with mortality, independent of traditional risk factors. They also suggested that RDW may be a stronger biomarker for morbidity and mortality. In our study, RDW, and not CRP, was associated with CLBP occurrence in the elderly. This suggests that CLBP may develop in the elderly based on chronic inflammation and RDW may be useful as a biomarker of chronic pain that does not reflect acute inflammation. In addition to chronic inflammation, oxidative stress is another significant mechanism that may explain the elevated RDW. Oxidative damage is an inducer of irreversible cellular senescence mediated by DNA damage, thereby leading to cell survival reduction45. Cellular senescence is an irreversible process. Unlike traditional biomarkers of acute inflammation, RDW is a valid indicator of senescence because it is not affected by cases of acute inflammation, such as infectious diseases; more so, it increases over time without large fluctuation, and it has a low reversibility43,44. The study results indicate that age-related physical changes in body composition, such as skeletal muscle loss and fat accumulation, are mechanisms of senescence that occur based on chronic inflammation. Thus, senescence might play a role in the development of CLBP in the elderly.
Additionally, recent studies have linked vitamin D, which is known to be effective in preventing falls in the elderly46, with chronic pain development47. Furthermore, the action of vitamin D is mediated by receptors within muscle cells and bone tissue. Vitamin D is one of the essential elements for the development and maintenance of the musculoskeletal metabolic system, thereby predisposing the patients to sarcopenia48. Conversely, vitamin D has anti-inflammatory properties, and pro-inflammatory cytokines are produced during vitamin D deficiency49. Vitamin D deficiency causes increased nociceptive skeletal muscle innervation, even before muscle or bone pathology occurs50. Moreover, patients with chronic pain and low vitamin D levels are have elevated central hypersensitivity, namely, increased mechanical pain sensitivity and somatic symptom severity51. In our study, skeletal muscle mass and 25-OHD levels decreased without bone density loss in patients with geriatric CLBP, which is a noteworthy mechanism of chronic pain mediated by the skeletal muscle system.
The feasibility of application to treatment for geriatric LBP in consideration of the involvement of senescence in the elderly with chronic pain is significant; however, the relationship between inflammation and pain is merely an issue of the pain threshold52, and the pathological conditions that trigger the occurrence of LBP are essential. Spinal sagittal alignment, which was significantly different in elderly patients with CLBP in this study, is also one of the most important factors influencing mechanical LBP in elderly patients. Progressive sagittal imbalance is strongly associated with health-related quality of life8. Skeletal muscle is important for maintaining sagittal spinal balance; thus, it is conceivable that sagittal imbalance occurs in elderly patients due to age-related muscle mass reduction and/or atrophy other than vertebral fracture. Since patients with vertebral fractures were excluded from this study, the increase in SVA in patients with CLBP was attributed to a decrease in skeletal muscle mass. Although a significant association between skeletal muscle mass reduction and high PT was found in both limbs and trunk, an association between SVA increase and skeletal muscle mass reduction was found only in the trunk. Considering that the decrease in skeletal muscle mass with aging occurs from the lower extremities, it is assumed that the subsequent decrease in trunk muscles accelerates the increase in SVA following pelvic posterior tilt due to skeletal muscle reduction in the extremities. The effect of skeletal muscles on pelvic tilt in our study is consistent with the findings of Hiyama, which demonstrated that pelvic tilt is the sagittal parameter most closely related to skeletal muscle mass in patients with spinal degeneration disease14. Studies evaluating LBP and skeletal muscle mass19,20,53,54 have reported the effect of skeletal muscle on sagittal spinal balance14,55,56; however, our study is the first to analyze the relationship between skeletal muscle reduction and spinal sagittal balance in elderly patients with CLBP. There is no other way than highly invasive surgical treatment to correct spinal deformity in the elderly, and there is no better treatment for sarcopenia. Given the fact that the underlying solution for mechanical LBP is practically challenging, thus it could make sense to seek other treatments to improve geriatric CLBP from an anti-inflammatory and/or anti-senescent perspective.
Our study has a limitation because we used data from heterogeneous patient database of Sarcopenia Study for Elderly Patient for patients who underwent DXA without CLBP as a control. It is unclear whether similar results can be obtained by comparing patients with CLBP and healthy elderly persons. In addition, the cross-sectional study design of our study prevents renders our findings inclusive regarding the role of skeletal muscle mass and spinal alignment in the development of CLBP. Longitudinal investigations on changes in skeletal muscle and spinal parameters in the elderly are needed to clarify the cause of geriatric CLBP.
In conclusion, RDW, which is an index of aging, was high in elderly patients with CLBP. Moreover, geriatric CLBP is associated with vitamin D deficiency, which affects the pain threshold, and triggers CLBP due to the age-related loss of skeletal muscle mass and spinal sagittal malalignment.
References
Nakamura, M., Nishiwaki, Y., Ushida, T. & Toyama, Y. Prevalence and characteristics of chronic musculoskeletal pain in Japan. J. Orthop. Sci. 16, 424–432. https://doi.org/10.1007/s00776-011-0102-y (2011).
Hoy, D. et al. The global burden of low back pain: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 73, 968–974. https://doi.org/10.1136/annrheumdis-2013-204428 (2014).
Woolf, A. D. & Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 81, 646–656 (2003).
Deyo, R. A., Rainville, J. & Kent, D. L. What can the history and physical examination tell us about low back pain?. JAMA 268, 760–765 (1992).
White, A. A. & Gordon, S. L. Synopsis: Workshop on idiopathic low-back pain. Spine 7, 141–149. https://doi.org/10.1097/00007632-198203000-00009 (1982).
Vos, T. et al. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators: Global burden of disease, injury incidence, prevalence collaborators—Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries. Lancet 388, 1545–1602. https://doi.org/10.1016/S0140-6736(16)31678-6 (2015).
Savigny, P., Watson, P. & Underwood, M. Guideline Development group: Early management of persistent non-specific low back pain: summary of NICE guidance. BMJ 338, 1805. https://doi.org/10.1136/bmj.b1805 (2009).
Glassman, S. D. et al. The impact of positive sagittal balance in adult spinal deformity. Spine 30, 2024–2029. https://doi.org/10.1097/01.brs.0000179086.30449.96 (2005).
Schwab, F. et al. Scoliosis research society-schwab adult spinal deformity classification: A validation study. Spine 37, 1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2,Pubmed:22045006 (2012).
Chaléat-Valayer, E. et al. Sagittal spino-pelvic alignment in chronic low back pain. Eur. Spine J. 20(Supplement), 5. https://doi.org/10.1007/s00586-011-1931-2 (2011).
Ogon, I. et al. Association between spinopelvic alignment and lumbar intervertebral disc degeneration quantified with magnetic resonance imaging T mapping in patients with chronic low back pain. Spine Surg. Relat. Res. 4, 135–141. https://doi.org/10.22603/ssrr.2019-0051 (2020).
Chun, S. W., Lim, C. Y., Kim, K., Hwang, J. & Chung, S. G. The relationships between low back pain and lumbar lordosis: A systematic review and meta-analysis. Spine J. 17, 1180–1191. https://doi.org/10.1016/j.spinee.2017.04.034 (2017).
Kado, D. M. et al. Factors associated with kyphosis progression in older women: 15 years’ experience in the study of osteoporotic fractures. J. Bone Miner. Res. 28, 179–187. https://doi.org/10.1002/jbmr.1728 (2013).
Hiyama, A. et al. Correlation analysis of sagittal alignment and skeletal muscle mass in patients with spinal degenerative disease. Sci. Rep. 8, 15492. https://doi.org/10.1038/s41598-018-33867-0 (2018).
Tsujinaka, T. et al. Interleukin 6 receptor antibody inhibits muscle atrophy and modulates proteolytic systems in interleukin 6 transgenic mice. J. Clin. Invest. 97, 244–249. https://doi.org/10.1172/JCI118398 (1996).
Haddad, F., Zaldivar, F., Cooper, D. M. & Adams, G. R. IL-6-induced skeletal muscle atrophy. J. Appl. Physiol. 98, 911–917. https://doi.org/10.1152/japplphysiol.01026.2004 (2005).
Lim, Y. Z. et al. Association between inflammatory biomarkers and non-specific low back pain: A systematic review. Clin. J. Pain. 26, 379–389 (2020).
Morris, P., Ali, K., Merritt, M., Pelletier, J. & Macedo, L. G. A systematic review of the role of inflammatory biomarkers in acute, subacute and chronic non-specific low back pain. BMC Musculoskelet. Disord. 21, 142. https://doi.org/10.1186/s12891-020-3154-3 (2020).
Franceschi, C. & Campisi, J. Chronic inflammation (Inflammaging) and its potential combination to age-associated diseases. J. Gerontol. A. Biol. Sci. Med. Sci. 69, S4–S9 (2014).
Sakai, Y. et al. Sarcopenia in elderly patients with chronic low back pain. Osteoporos. Sarcopenia. 3, 195–200. https://doi.org/10.1016/j.afos.2017.09.001 (2017).
Tanishima, S., Hagino, H., Matsumoto, H., Tanimura, C. & Nagashima, H. Association between sarcopenia and low back pain in local residents prospective cohort study from the GAINA study. BMC Musculoskelet. Disord. 18, 452. https://doi.org/10.1186/s12891-017-1807-7 (2017).
Steffens, D. et al. Does magnetic resonance imaging predict future low back pain? A systematic review. Eur. J. Pain. 18, 755–765. https://doi.org/10.1002/j.1532-2149.2013.00427.x (2014).
Salvagno, G. L., Sanchis-Gomar, F., Picanza, A. & Lippi, G. Red blood cell distribution width: A simple parameter with multiple clinical applications. Crit. Rev. Clin. Lab. Sci. 52, 86–105. https://doi.org/10.3109/10408363.2014.992064 (2015).
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practical guideline. J. Clin. Endocr. Metab. 96, 1911–1930 (2011).
Schwab, F., Patel, A., Ungar, B., Farcy, J. P. & Lafage, V. Adult spinal deformity-postoperative standing imbalance: How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 35, 2224–2231. https://doi.org/10.1097/BRS.0b013e3181ee6bd4 (2010).
Baumgartner, R. N. et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am. J. Epidemiol. 147, 755–763. https://doi.org/10.1093/oxfordjournals.aje.a009520 (1998).
Modic, M. T., Steinberg, P. M., Ross, J. S., Masaryk, T. J. & Carter, J. R. Degenerative disk disease: Assessment of changes in vertebral body marrow with MR imaging. Radiology 166, 193–199. https://doi.org/10.1148/radiology.166.1.3336678 (1988).
Pfirrmann, C. W., Metzdorf, A., Zanetti, M., Hodler, J. & Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26, 1873–1878. https://doi.org/10.1097/00007632-200109010-00011 (2001).
Abe, T., Loenneke, J. P., Thiebaud, R. S. & Fukunaga, T. Age-related site-specific muscle wasting of upper and lower extremities and trunk in Japanese men and women. Age 36, 813–821. https://doi.org/10.1007/s11357-013-9600-5 (2014).
Parkkola, R., Rytökoski, U. & Kormano, M. Magnetic resonance imaging of the discs and trunk muscles in patients with chronic low back pain and healthy control subjects. Spine 18, 830–836. https://doi.org/10.1097/00007632-199306000-00004 (1993).
Hultman, G., Nordin, M., Saraste, H. & Ohlsèn, H. Body composition, endurance, strength, cross-sectional area, and density of MM erector spinae in men with and without low back pain. J. Spinal Disord. 6, 114–123. https://doi.org/10.1097/00002517-199304000-00004 (1993).
Danneels, L. A., Vanderstraeten, G. G., Cambier, D. C., Witvrouw, E. E. & De Cuyper, H. J. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur. Spine J. 9, 266–272. https://doi.org/10.1007/s005860000190 (2000).
Hides, J. A., Richardson, C. A. & Jull, G. A. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine 21, 2763–2769. https://doi.org/10.1097/00007632-199612010-00011 (1996).
Hodges, P., Holm, A. K., Hansson, T. & Holm, S. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine 31, 2926–2933. https://doi.org/10.1097/01.brs.0000248453.51165.0b (2006).
Lexell, J., Taylor, C. C. & Sjöström, M. What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15 to 83 year-old men. J. Neurol. Sci. 84, 275–294. https://doi.org/10.1016/0022-510x(88)90132-3 (1988).
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European working group on sarcopenia in older people. Age. Ageing. 39, 412–423. https://doi.org/10.1093/ageing/afq034 (2010).
Shaw, A. C., Goldstein, R. & Montgomery, R. R. Age-dependent dysregulation of innate immunity. Nat. Rev. Immunol. 13, 875–887. https://doi.org/10.1038/nri3547 (2013).
Wilson, D. et al. Frailty and sarcopenia: The potential role of an aged immune system. Ageing Res. Rev. 36, 1–10. https://doi.org/10.1016/j.arr.2017.01.006 (2017).
Hu, L. et al. Prognostic value of RDW in cancers: A systematic review and meta-analysis. Oncotarget 8, 16027–16035. https://doi.org/10.18632/oncotarget.13784 (2017).
Felker, G. M. et al. Red cell distribution width as a novel prognostic marker in heart failure: Data from the CHARM program and the Duke databank. J. Am. Coll. Cardiol. 50, 40–47. https://doi.org/10.1016/j.jacc.2007.02.067 (2007).
Lippi, G. et al. Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Arch. Pathol. Lab. Med. 133, 628–632. https://doi.org/10.5858/133.4.628 (2009).
Bazick, H. S., Chang, D., Mahadevappa, K., Gibbons, F. K. & Christpher, K. B. Red cell distribution width and all-causes mortality in critically ill patients. Crit. Care Med. 39, 1913–1921. https://doi.org/10.1097/CCM.0b013e31821b85c6 (2011).
Veeranna, V., Zalawadiya, S. K., Panaich, S., Patel, K. V. & Afonso, L. Comparative analysis of red cell distribution width and high sensitivity C-reactive protein for coronary heart disease mortality prediction in multi-ethnic population: Findings from the 1999–2004 NHANES. Int J. Cardiol. 168, 5156–5161. https://doi.org/10.1016/j.ijcard.2013.07.109 (2013).
Wei, X. B. et al. Combined efficacy of C-reactive protein and red blood cell distribution width in prognosis of patients with culture-negative infective endocarditis. Oncotarget 8, 71173–71180. https://doi.org/10.18632/oncotarget.16888 (2017).
Kiefer, C. R. & Snyder, L. M. Oxidation and erythrocyte senescence. Curr. Opin. Hematol. 7, 113–116. https://doi.org/10.1097/00062752-200003000-00007 (2000).
Richy, F., Dukas, L. & Schacht, E. Differential effects of D-hormone analogs and native vitamin D on the risk of falls: A comparative meta-analysis. Calcif. Tissue. Int. 82, 102–107. https://doi.org/10.1097/00062752-200003000-00007 (2008).
Vos, T., Allen, C. & Arosa, M. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet 390, 1211–1259 (2017).
Uchitomi, R., Oyabu, M. & Kamei, Y. Vitamin D and sarcopenia: Potential of vitamin D supplementation in sarcopenia prevention and treatment. Nutrients 12, 3819. https://doi.org/10.3390/nu12103189 (2020).
Müller, K. et al. 1,25-Dihydroxvitamin D3 inhibits cytokine production by human blood monocytes at the post-transcriptional level. Cytokine 4, 506–512. https://doi.org/10.1016/1043-4666(92)90012-g (1992).
Tague, S. E. et al. Vitamin D deficiency promotes skeletal muscle hypersensitivity and sensory hyperinnervation. J. Neurosci. 31, 13728–13738. https://doi.org/10.1523/JNEUROSCI.3637-11.2011 (2011).
Von Känel, R., Müller-Hartmannsgruber, V., Kokinogenis, G. & Egloff, N. Vitamin D and central hypersensitivity in patients with chronic pain. Pain Med. 15, 1609–1618. https://doi.org/10.1111/pme.12454 (2014).
de Goeij, M. et al. Systemic inflammation decreases pain threshold in humans in vivo. PLoS ONE 8, e84159. https://doi.org/10.1371/journal.pone.0084159 (2013).
Nakagawa, M. et al. Influence of sarcopenia on the effect of exercise therapy for elderly patients with chronic low back pain. Spine Surg. Relat. Res. 4, 247–255. https://doi.org/10.22603/ssrr.2019-0116 (2020).
Wada, T., Tanishima, S., Osaki, M., Nagashima, H. & Hagino, H. Relationship between sarcopenia and pain catastrophizing in patients with lumbar spinal stenosis: A cross-sectional study. Osteoporos. Sarcopenia 5, 132–136. https://doi.org/10.1016/j.afos.2019.12.001 (2019).
Park, J. S., Park, Y. S., Kim, J., Hur, J. & Choe, D. H. Sarcopenia and fatty degeneration of paraspinal muscle associated with increased sagittal vertical axis in the elderly: A cross-sectional study in 71 female patients. Eur. Spine J. 29, 1353–1361. https://doi.org/10.1007/s00586-020-06416-5 (2020).
Ohyama, S. et al. Sarcopenia is related to spinal sagittal imbalance in patients with spinopelvic mismatch. Eur. Spine J. 28, 1929–1936. https://doi.org/10.1007/s00586-019-06066-2 (2019).
Acknowledgements
The authors would like to thank Editage (http://www.editage.co.kr) for English language editing.
Author information
Authors and Affiliations
Contributions
Y. S., N. W., H. M., T. W., H. I., and K. W. Made substantial contributions to the conception and design of the work. Y. S., N. W., H. M., T. W., and H. I. Collected the patient data and reviewed the radiographs. H. M. and T. W. Performed the statistical analysis. Y. S., N. W., H. M., T. W., H. I., and K. W. Contributed to the interpretation of data. Y. S. and K. W. Supervised the work. All authors reviewed the submitted version of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakai, Y., Wakao, N., Matsui, H. et al. Clinical characteristics of geriatric patients with non-specific chronic low back pain. Sci Rep 12, 1286 (2022). https://doi.org/10.1038/s41598-022-05352-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-05352-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.