Abstract
The cuff leak test (CLT) has been widely accepted as a simple and noninvasive method for predicting post-extubation stridor (PES). However, its accuracy and clinical impact remain uncertain. We aimed to evaluate the reliability of CLT and to assess the impact of pre-extubation variables on the incidence of PES. A prospective observational study was performed on adult critically ill patients who required mechanical ventilation for more than 24 h. Patients were extubated after the successful spontaneous breathing trial, and CLT was conducted before extubation. Of the 191 patients studied, 26 (13.6%) were deemed positive through CLT. PES developed in 19 patients (9.9%) and resulted in a higher reintubation rate (8.1% vs. 52.6%, p < 0.001) and longer intensive care unit stay (8 [4.5–14] vs. 12 [8–30.5] days, p = 0.01) than patients without PES. The incidence of PES and post-extubation outcomes were similar in patients with both positive and negative CLT results. Compared with patients without PES, patients with PES had longer durations of endotracheal intubation and required endotracheal suctioning more frequently during the 24-h period prior to extubation. After adjusting for confounding factors, frequent endotracheal suctioning more than 15 times per day was associated with an adjusted odds ratio of 2.97 (95% confidence interval, 1.01–8.77) for PES. In conclusion, frequent endotracheal suctioning before extubation was a significant PES predictor in critically ill patients. Further investigations of its impact on the incidence of PES and patient outcomes are warranted.
Similar content being viewed by others
Introduction
Endotracheal intubation is an essential procedure for respiratory support in critically ill patients. However, complications resulting from mechanical trauma to the larynx by the endotracheal tube may lead to laryngeal edema1,2. Airflow through a narrowed upper airway manifests clinically as a post-extubation stridor (PES)3. The incidence of PES is 4–10% in patients who are endotracheally intubated for more than 24 h4,5. Patients with PES are likely to undergo increased reintubation6,7, which is associated with increased morbidity and mortality8,9,10.
To identify patients at risk of laryngeal edema, airway patency assessment before extubation has been evaluated. Since Miller and Cole evaluated 100 mechanically ventilated patients in 1996, the cuff leak test (CLT) has been widely used because of its noninvasiveness and avoidance of sophisticated equipment11,12,13,14,15. The cuff leak volume was defined as the tidal volume difference from before to after endotracheal tube (ETT) cuff deflation. The primary threshold of cuff leak volume of less than 110 mL was reported as the valid cut-off value for predicting PES with a positive predictive value of 0.80. Subsequent studies reported various cut-off values16,17,18. The other remarkable threshold, a cuff leak less than 10% of the tidal volume, was identified to predict PES or reintubation with a specificity of 96%19. In the previous meta-analyses of pooled studies on multiple CLT methods, the CLT displayed an accurate prediction for patients at high risk of the development of airway obstruction20,21,22 and is now widely used. However, some previous studies did not conduct a spontaneous breathing trial (SBT), which is the current standard weaning method, and there is concern that this may affect extubation outcomes. Indeed, recent studies have reported the poor diagnostic performance of the CLT in the current critical care settings7,23,24, and the diagnostic performance of CLT remains controversial.
Moreover, several studies related to baseline characteristics and airway management were performed to identify PES incidence risk factors. Important risk factors include female sex, body mass index (BMI), larger ETT diameter, and longer intubation duration3,12,25,26,27. However, each risk factor is insufficient to identify patients at high risk for PES when considered alone3, and the investigation of physiological or descriptive data at extubation is limited.
Accordingly, we aimed to determine the CLT value and the impact of pre-extubation variables for predicting PES among critically ill patients, based on the current standard and unified weaning readiness techniques.
Methods
Conduct of the study and selection criteria
This prospective study was performed in a multidisciplinary intensive care unit (ICU) of a tertiary care hospital between May 2017 and April 2019. The consecutive patients who had undergone invasive mechanical ventilation for more than 24 h and had been extubated following a successful SBT and assessment of the CLT were enrolled. Patients younger than 18 years of age, with a tracheostomy or unplanned extubation, who received palliative care or passed away under mechanical ventilation, and who passed away within 48 h after extubation were excluded. If patients received mechanical ventilation multiple times, the first extubation attempt after mechanical ventilation for more than 24 h was included.
This study was approved by the ethics review board of Osaka University Hospital (Approval Number: 19316), and the need for consent for research participation was waived. The study was performed in accordance with relevant guidelines and regulations.
Assessment before extubation
According to the weaning strategies with national consensus, patients were considered eligible for SBT when the underlying cause of respiratory failure was resolved. Sufficient oxygenation (SpO2 > 90% at FiO2 ≤ 0.5 and positive end-expiratory pressure [PEEP] ≤ 8 cmH2O) and inspiratory effort (tidal volume > 5 mL/kg; minute volume < 15 L/min; rapid shallow breathing index < 105 breaths/min/L; and pH > 7.25) were verified prior to SBT. Clinicians suspended SBT if a patient had any of the following: significant deterioration of oxygenation compared to before SBT, respiratory rate ≥ 30 breaths/min, heart rate ≥ 140 beats/min, arrhythmia, myocardial ischemia symptom, sustained increased blood pressure, or appearance of respiratory distress as defined by paradoxical breathing, use of accessory muscles, sweating, or agitation. Patients were extubated if they tolerated 30 min of spontaneous breathing on PEEP of 5 cmH2O with pressure support (PS) of 5 cmH2O.
The cuff pressure was continuously measured and maintained at 25 cmH2O during mechanical ventilation in all patients. Prior to endotracheal extubation, CLT was performed by the attending intensivists. The patient was suctioned intraorally and intratracheally and placed in the assist-control ventilation mode. With the ETT cuff inflated to the occlusion volume, the average mechanical exhaled volume over the three consecutive respiratory cycles was measured and recorded. Subsequently, the ETT cuff was deflated. The mechanical exhaled tidal volume was monitored over the next six consecutive respiratory cycles to ensure the exclusion of erroneous values. The average of the three lowest exhaled tidal volumes was recorded. The lost tidal volume on exhalation, the cuff leak volume, was calculated as the tidal volume difference between the inflated and deflated ETT cuffs. Moreover, the cuff leak volume was divided by the tidal volume before cuff deflation and multiplied by 10019; the resulting value was regarded as the percent cuff leak. The high risk of upper airway obstruction was determined as the positive cuff leak result, the cuff leak volume ≤ 110 mL, and/or the percent cuff leak ≤ 10%, before extubation11,19,21.
Data collection
Variables collected of each patient included age, sex, BMI, comorbidities, Acute Physiology and Chronic Health Evaluation (APACHE) II and III scores as indicators of disease severity on ICU admission, the reason for intubation, the size of the endotracheal tube, and the duration of mechanical ventilation. In addition, arterial blood gas values and ventilation data during successful SBT were recorded. Simultaneously, we collected information on patient management during the 24 h prior to extubation. Fluid balance, increased body weight when compared with the body weight prior to ICU admission, and as an indicator of tracheal–bronchial secretion, endotracheal suctioning, were recorded 24 h prior to extubation. Systemic steroid therapy was recorded if the patient was administered steroid ≥ 20 mg/day of methylprednisolone at least 4 h prior to extubation. Furthermore, the severity of organ dysfunction during extubation was assessed using the Sequential Organ Failure Assessment (SOFA) score28.
Moreover, the following data were recorded after extubation: reintubation and the incidence of PES within 48 h after extubation, ICU and hospital lengths of stay, and ICU and hospital mortality. Patients’ respiratory function and hemodynamics were closely monitored for 48 h after extubation. They were reintubated if they presented cardiac arrest, refractory hypoxemia, severe hemodynamic instability without response to fluids and vasoactive drugs, persistent inability to remove excessive secretions, upper airway obstruction, agitation, and loss of consciousness at the discretion of the intensivist in charge. A patient having PES was identified with the presence of respiratory distress with high-pitched inspiratory wheezing. The incidence of PES was assessed and recorded by clinicians and decisions concerning the medical treatment for PES were made by the attending intensivists.
Statistical analyses
Categorical data are presented as numbers and percentages. Distributed data are presented as medians and interquartile ranges. Differences in proportions were evaluated using the chi-square test or Fisher’s exact test, and differences in distributed data with the Mann–Whitney U test for the two groups. A multiple logistic regression analysis model was used to determine PES incidence risk factors. Covariates with p < 0.05 in the univariate analysis were included in the multivariate model. To adjust for potential confounding factors, sex, BMI (> 25 kg/m2), and positive CLT were added to the model. All statistical inferences were made with a 2-sided significance level of 5% and conducted with R version 4.0.1 (2020, R Foundation for Statistical Computing, Vienna, Austria).
Ethics declarations
This study was approved by the ethics review board of Osaka University Hospital (Approval Number: 19316), and the need for consent for research participation was waived.
Results
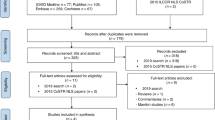
Over the 2-year study period, a total of 286 adult patients required invasive mechanical ventilation for more than 24 h. CLTs were not performed for 95 patients for the following reasons: tracheostomy (n = 21), palliative care or death under mechanical ventilation (n = 9), ICU discharge with mechanical ventilation (n = 14), unplanned extubation (n = 1), or omission of the CLT (n = 50). The remaining 191 adult patients were included in this study (Fig. 1). The characteristics of the study population are presented in Table 1. The median age was 65 years, and 67 (35.1%) patients were women. The main causes of ICU admission were surgical (75.9%). Reasons for mechanical ventilation included postoperative acute respiratory failure defined as ineligible decision for weaning and extubation in patients after surgery (n = 143; 74.9%), pneumonia (n = 16; 8.4%), cardiac failure (n = 10; 5.2%), and cardiac arrest (n = 8; 4.2%).
CLT result and its clinical impact
Twenty-six (13.6%) patients were determined to be positive through the CLT before extubation (Table 1). Positive CLT results were detected more often in female patients (18/67; 26.9%) than in male patients (8/124; 6.5%) (p < 0.001). Besides, patients with positive CLT results had a significantly larger BMI than their counterparts. The ETT diameter, duration of mechanical ventilation, and data from 24 h before extubation were similar regardless of CLT results (Tables 1, 2). The cuff leak volume and percent cuff leak were significantly smaller in patients with positive CLT results. All patients with positive CLT results had a cuff leak volume ≤ 110 mL; however, only 9 (34.6%) patients had a percent cuff leak ≤ 10%. The PES incidence was similar in the results of both CLT (negative: 9.7% vs. positive: 11.5%, p = 0.73) (Supplementary Table S1 shows this in more detail). Moreover, there were no differences in the reintubation rate, ICU and hospital lengths of stay, and ICU and hospital mortality according to the CLT results.
Comparison of patients with and without PES
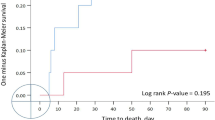
The overall incidence of PES was 9.9% (19/191). Table 3 compares the baseline characteristics of patients with and without PES. There were no significant differences in sex or BMI. The SOFA score at extubation, respiratory data, and the administration of systemic steroids during the 24-h period before extubation were similar in both groups (Table 4). Patients with PES had a longer duration of mechanical ventilation and required endotracheal suctioning more frequently than patients without PES. However, the CLT results were similar in both groups. As post-extubation outcomes, 8 (42.1%) patients with PES required reintubation for PES (Table 5). The reintubation rate for all causes was significantly higher in patients with PES than in those without PES (8.1% vs. 52.6%, p < 0.001). Moreover, the ICU length of stay was significantly longer for patients with PES than for those without PES (p = 0.01). There were no significant differences in hospital length of stay and ICU or hospital mortality.
Factors associated with PES
In the univariate logistic regression analysis, the positive result of CLT was not significantly associated with the incidence of PES, while there were differences in frequent endotracheal suctioning and prolonged mechanical ventilation (Table 6). After adjusting for confounding factors in the multivariate analysis, the frequent endotracheal suctioning more than 15 times during the 24-h period before extubation remained significant (adjusted odds ratio 2.97; 95% confidence interval [CI] 1.01–8.77).
Discussion
We conducted a prospective cohort study to evaluate the performance of CLT and the potential impact of pre-extubation variables on the incidence of PES in critically ill patients who were extubated after successful SBT under the unified ventilatory support setting. Though the patients with positive CLT results had significantly smaller cuff leak volumes and percent cuff leaks than those with negative CLT results, the performance of the CLT was insufficient for the accurate prediction of PES. The potential risk factors, female sex, and the larger BMI were associated with CLT results. However, these factors were not significantly associated with the incidence of PES. Frequent endotracheal suctioning during the 24-h period prior to extubation was independently associated with the incidence of PES.
As the direct visualization of laryngeal edema is difficult with an endotracheal tube in position, the CLT has been widely accepted to predict PES incidence. However, this study contributes to the limited and conflicting evidence regarding the predictive accuracy of CLT. The standard rate of patients deemed positive through the CLT (the cuff leak volume ≤ 110 mL) has been reported to be between 5 and 30% in critically ill adult settings11,20,23,27, which validates our finding of 13.6%. Simultaneously, the incidence of PES in this study was 9.9%, which was comparable to the results of previous studies with a lower rate than the positive CLT rate. Thus, the relatively low prevalence of PES has been regarded as a possible factor for the poor performance of the CLT in the identification of patients at high risk of PES occurrence3. Laryngeal edema should occur in most intubated patients with varying degrees. The quantity of data on airway stenosis regarding PES and respiratory distress incidence is limited29,30,31. Furthermore, after prolonged endotracheal intubation, bronchoscopy showed that the tracheal granulation tissue or ulcerations spread widely from the vocal cord to the previous ETT balloon cuff site17,32. As global guidelines have not standardized the ETT size based on the tracheal diameter33,34, our patients were provided a similar ETT size regardless of the CLT results. Mild laryngeal edema encompassing the ETT balloon cuff could be demonstrated by the CLT without significant clinical symptoms, leading to an insufficient interpretation of the test result24. Moreover, the cumulative evidence for the predictive accuracy of CLTs was based on a variety of mechanical ventilation modes and clinical settings during CLT22. Following the reference report by Miller et al.11, the assist-control ventilation mode was commonly used, just as in this study35. However, the fact that rigorous and reproducible CLT assessment may require firm sedation and paralysis to avoid erroneous measurement caused by coughing or agitation36 and the potential influence of glossoptosis on the head position are challenges for the current standard CLT method37.
Furthermore, systemic steroid therapy before elective extubation has been associated with significant PES incidence reductions5,25,38,39. A recent meta-analysis including 11 trials of 2472 participants revealed that prophylactic systemic steroid therapy was associated with a reduced incidence of post-extubation airway events (risk ratio [RR], 0.43; 95% CI 0.29–0.66) and reintubation (RR, 0.42; 95% CI 0.25–0.71) when compared with placebo or no treatment29,40. The authors also screened six trials that documented the adverse effects and concluded that the short duration of systemic steroid administration rarely resulted in severe adverse effects. There was no hyperglycemia or gastrointestinal bleeding incidence, and only one patient who received systemic steroids was recognized with the infection. Thus, the current guidelines indicate the use of prophylactic systemic steroids in patients with airway compromise12,41. In our cohort, patients received systemic steroid therapy for at least 4 h before extubation for all causes (7.3% and 15.4% of the patients with negative and positive CLT results, respectively). Systemic steroid therapy was not individually associated with PES incidence (p = 0.67); however, it may potentially treat laryngeal edema and influence patient outcomes.
Multiple investigations of the risk factors for the incidence of PES have been reported, with conflicting conclusions. In this study, female sex and larger BMI were associated with CLT results. Patients with PES had a longer duration of intubation and frequent endotracheal suctioning than those without PES. However, multivariate analysis revealed that frequent endotracheal suctioning during the 24-h period before extubation was independently associated with PES incidence in our patient population. The number of endotracheal suctioning indicates the amount of trachea-bronchial secretion. Excessive tracheal-bronchial secretions can lead to bronchial plugging and atelectasis, which can result in respiratory failure. Recent reports substantiated the significance of excessive tracheal-bronchial secretions before extubation as risk factors for reintubation8,42,43,44. In addition, the tracheal-bronchial secretions are relevant indicators of laryngeal edema because they are triggered simultaneously, and both are caused by airway inflammation45. Furthermore, acute venous congestion due to excessive fluid infusion could increase pulmonary congestion causing tracheal-bronchial secretions46,47; moreover, it could also increase the risk of laryngeal edema48. Subsequently, the procedure of endotracheal suctioning itself has been reported to potentially cause tracheal-bronchial inflammation49,50 and pulmonary edema51. Thus, laryngeal edema and tracheal-bronchial secretions are caused in conjunction with each other, however, their relative importance has not been sufficiently investigated. The only previous study to research the association between the number of endotracheal suctioning and laryngeal injury was in 1981, in a single prospective cohort of 150 critically ill patients who received mechanical ventilation with endotracheal intubation or tracheostomy2. Stauffer et al. reported that endotracheal suctioning frequency was not significantly associated with total laryngeal injury at autopsy. However, this analysis included 51 patients (34%) with a tracheostomy, and the liberation process was not standardized. According to the current clinical practice and the unified weaning readiness techniques, the present data provide a reasonable impact.
Our findings imply that a positive result of CLT is relatively common in critically ill patients who have undergone invasive mechanical ventilation for more than 24 h. However, they also imply that the CLT results are not significantly associated with PES incidence, which results in an increased reintubation rate and ICU length of stay. Despite the lack of a significant impact on demographic variables, we found that frequent endotracheal suctioning was an independent risk factor for PES incidence. This finding provides a rationale for further investigations of the risk management of upper airway obstruction.
Our study has several strengths. Relatively few studies have assessed the physiological or descriptive data at extubation as risk factors for PES incidence. Though the population we investigated was relatively small, our prospective cohort was representative, as the rate of positive results of CLT and the incidence of PES were comparable to those described in other recent studies. In addition, the rigorous SBT and CLT assessment revealed a robust evaluation of CLT and risk factors for the prediction of PES.
Some limitations of this study should be acknowledged. First, it is a single-center study, with all the limitations inherent in such a design. The results may not be generalizable to all geographical regions. Second, we employed the SBT method with pressure support ventilation (PSV) using low PS and PEEP levels, following the international guideline that recommends inspiratory pressure augmentation52. General SBT methods, both PSV and T-piece, were reported to have comparable predictive performance for successful extubation53. However, low level of assistance without PEEP has recently been recommended as a SBT method54, which is distinct from the method used in this study. Third, based on previous studies reporting PES rates of 4–10%, we conducted a 2-year observational study to obtain at least 10 patients presenting with PES in an ICU with approximately 50–150 eligible patients per year to clarify its predictive performance using binary logistic regression analysis. To detect the association between the CLT results and PES incidence with 95% certainty at 80% power, we assumed that a total of 184 patients would be required. This was based on CLT positivity and PES incidence rates of 18% and 4%, respectively, according the results of a previous study that included the largest number of patients27. We found that that 19 among 191 study patients had PES and could accumulate sufficient cases for analysis, however, the CLT positivity rate and the incidence of PES in this study suggested that a greater number of patients were warranted to determine the predictive ability of CLT for PES. Hence, our results should be examined in a meta-analysis and in a pooled analysis. In addition, this study included all patients with mechanical ventilation and not exclusively patients at high risk for PES, for which the guideline recommends CLT12. Furthermore, patients with unplanned extubation regarded as high risk for PES12 were not included in the study due to lack of SBT or CLT, and we did not identify any patient who was reintubated after unplanned extubation and then underwent planned extubation. Forth, the formal PES diagnosis was based on clinical symptoms and, therefore, relatively subjective. Fifth, although the assessment of SBT and CLT was standardized, the final decision of extubation, the administration of systemic steroids, the treatment of patients with PES, and the decision of reintubation were at the discretion of the clinician in charge of the patients without specific institutional protocols.
Conclusions
In the critically ill patients receiving mechanical ventilation, patients who required frequent endotracheal suctioning were at a high risk of developing PES. Though its impact on the incidence of PES and patient outcomes needs to be further explored, frequent endotracheal suctioning before extubation could be added to the usual prediction for PES.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Colice, G. L., Stukel, T. A. & Dain, B. Laryngeal complications of prolonged intubation. Chest 96, 877–884 (1989).
Stauffer, J. L., Olson, D. E. & Petty, T. L. Complications and consequences of endotracheal intubation and tracheotomy. A prospective study of 150 critically ill adult patients. Am. J. Med. 70, 65–76 (1981).
Pluijms, W. A., van Mook, W. N., Wittekamp, B. H. & Bergmans, D. C. Postextubation laryngeal edema and stridor resulting in respiratory failure in critically ill adult patients: Updated review. Crit. Care 19, 295 (2015).
Patel, A. B., Ani, C. & Feeney, C. Cuff leak test and laryngeal survey for predicting post-extubation stridor. Indian J. Anaesth. 59, 96–102 (2015).
Cheng, K. C. et al. Methylprednisolone reduces the rates of postextubation stridor and reintubation associated with attenuated cytokine responses in critically ill patients. Minerva Anestesiol. 77, 503–509 (2011).
Jaber, S. et al. Post-extubation stridor in intensive care unit patients. Risk factors evaluation and importance of the cuff-leak test. Intensive Care Med. 29, 69–74 (2003).
Schnell, D. et al. Cuff leak test for the diagnosis of post-extubation stridor: a multicenter evaluation study. J. Intensive Care Med. 34, 391–396 (2019).
Epstein, S. K. & Ciubotaru, R. L. Independent effects of etiology of failure and time to reintubation on outcome for patients failing extubation. Am. J. Respir. Crit. Care Med. 158, 489–493 (1998).
Frutos-Vivar, F. et al. Outcome of reintubated patients after scheduled extubation. J. Crit. Care 26, 502–509 (2011).
Seymour, C. W., Martinez, A., Christie, J. D. & Fuchs, B. D. The outcome of extubation failure in a community hospital intensive care unit: A cohort study. Crit. Care 8, R322–R327 (2004).
Miller, R. L. & Cole, R. P. Association between reduced cuff leak volume and postextubation stridor. Chest 110, 1035–1040 (1996).
Girard, T. D. et al. An Official American Thoracic Society/American College of Chest physicians clinical practice guideline: Liberation from mechanical ventilation in critically Ill adults. Rehabilitation protocols, ventilator liberation protocols, and cuff leak tests. Am. J. Respir. Crit. Care Med. 195, 120–133 (2017).
Baptistella, A. R. et al. Prediction of extubation outcome in mechanically ventilated patients: Development and validation of the extubation predictive score (ExPreS). PLoS ONE 16, e0248868 (2021).
Lewis, K. et al. The cuff leak test in critically ill patients: An international survey of intensivists. Acta Anaesthesiol. Scand. 65, 1087–1094 (2021).
Moran, J. V., Godil, S. A., Goldner, B., Godil, K. & Aslam, J. Post-extubation stridor complicating COVID-19-associated acute respiratory distress syndrome: A case series. Cureus 12, e10492 (2020).
Wang, C. L. et al. The role of the cuff leak test in predicting the effects of corticosteroid treatment on postextubation stridor. Chang. Gung. Med. J. 30, 53–61 (2007).
Chung, Y. H., Chao, T. Y., Chiu, C. T. & Lin, M. C. The cuff-leak test is a simple tool to verify severe laryngeal edema in patients undergoing long-term mechanical ventilation. Crit. Care Med. 34, 409–414 (2006).
Keeratichananont, W., Limthong, T. & Keeratichananont, S. Cuff leak volume as a clinical predictor for identifying post-extubation stridor. J. Med. Assoc. Thai. 95, 752–756 (2012).
Sandhu, R. S., Pasquale, M. D., Miller, K. & Wasser, T. E. Measurement of endotracheal tube cuff leak to predict postextubation stridor and need for reintubation. J. Am. Coll. Surg. 190, 682–687 (2000).
Zhou, T. et al. Cuff-leak test for predicting postextubation airway complications: A systematic review. J. Evid. Based Med. 4, 242–254 (2011).
Ochoa, M. E. et al. Cuff-leak test for the diagnosis of upper airway obstruction in adults: A systematic review and meta-analysis. Intensive Care Med. 35, 11711179 (2009).
Kuriyama, A., Jackson, J. L. & Kamei, J. Performance of the cuff leak test in adults in predicting post-extubation airway complications: A systematic review and meta-analysis. Crit. Care 24, 640 (2020).
Shin, S. H. et al. The cuff leak test is not predictive of successful extubation. Am. Surg. 74, 1182–1185 (2008).
Gros, A. et al. Intra-individual variation of the cuff-leak test as a predictor of post-extubation stridor. Respir. Care 57, 2026–2031 (2012).
Ho, L. I., Harn, H. J., Lien, T. C., Hu, P. Y. & Wang, J. H. Postextubation laryngeal edema in adults. Risk factor evaluation and prevention by hydrocortisone. Intensive Care Med. 22, 933–936 (1996).
Erginel, S., Ucgun, I., Yildirim, H., Metintas, M. & Parspour, S. High body mass index and long duration of intubation increase post-extubation stridor in patients with mechanical ventilation. Tohoku J. Exp. Med. 207, 125–132 (2005).
Kriner, E. J., Shafazand, S. & Colice, G. L. The endotracheal tube cuff-leak test as a predictor for postextubation stridor. Respir. Care 50, 1632–1638 (2005).
Ferreira, F. L., Bota, D. P., Bross, A., Melot, C. & Vincent, J. L. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286, 1754–1758 (2001).
Wittekamp, B. H., van Mook, W. N., Tjan, D. H., Zwaveling, J. H. & Bergmans, D. C. Clinical review: Post-extubation laryngeal edema and extubation failure in critically ill adult patients. Crit. Care 13, 233 (2009).
Mackle, T., Meaney, J. & Timon, C. Tracheoesophageal compression associated with substernal goitre. Correlation of symptoms with cross-sectional imaging findings. J. Laryngol. Otol. 121, 358–361 (2007).
Ding, L. W., Wang, H. C., Wu, H. D., Chang, C. J. & Yang, P. C. Laryngeal ultrasound: A useful method in predicting post-extubation stridor. A pilot study. Eur. Respir. J. 27, 384–389 (2006).
Kastanos, N., Estopa Miro, R., Marin Perez, A., Xaubet Mir, A. & Agusti-Vidal, A. Laryngotracheal injury due to endotracheal intubation: Incidence, evolution, and predisposing factors. A prospective long-term study. Crit. Care Med. 11, 362–365 (1983).
Higgs, A. et al. Guidelines for the management of tracheal intubation in critically ill adults. Br. J. Anaesth. 120, 323–352 (2018).
Quintard, H. et al. Experts’ guidelines of intubation and extubation of the ICU patient of French Society of Anaesthesia and Intensive Care Medicine (SFAR) and French-speaking Intensive Care Society (SRLF): In collaboration with the pediatric Association of French-speaking Anaesthetists and Intensivists (ADARPEF), French-speaking Group of Intensive Care and Paediatric emergencies (GFRUP) and intensive care physiotherapy society (SKR). Ann. Intensive Care 9, 13 (2019).
Lewis, K. et al. Cuff leak test and airway obstruction in mechanically ventilated ICU patients: A pilot randomised controlled trial. Ann. Am. Thorac. Soc. https://doi.org/10.1513/annalsats.202103-390oc (2021).
Pettignano, R., Holloway, S. E., Hyman, D. & LaBuz, M. Is the leak test reproducible? S. Med. J. 93, 683–685 (2000).
Goto, S., Ishikawa, J. Y., Idei, M. & Nomura, T. False-positive cuff leak test due to glossoptosis. Am. J. Respir. Crit. Care Med. https://doi.org/10.1164/rccm.202104-0820IM (2021).
Darmon, J. Y. et al. Evaluation of risk factors for laryngeal edema after tracheal extubation in adults and its prevention by dexamethasone. A placebo-controlled, double-blind, multicenter study. Anesthesiology 77, 245–251 (1992).
François, B. et al. 12-h pretreatment with methylprednisolone versus placebo for prevention of postextubation laryngeal oedema: A randomised double-blind trial. The Lancet 369, 1083–1089 (2007).
Kuriyama, A., Umakoshi, N. & Sun, R. Prophylactic corticosteroids for prevention of postextubation stridor and reintubation in adults: A systematic review and meta-analysis. Chest 151, 1002–1010 (2017).
Popat, M. et al. Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia 67, 318–340 (2012).
Salam, A., Tilluckdharry, L., Amoateng-Adjepong, Y. & Manthous, C. A. Neurologic status, cough, secretions and extubation outcomes. Intensive Care Med. 30, 1334–1339 (2004).
Mokhlesi, B. et al. Predicting extubation failure after successful completion of a spontaneous breathing trial. Respir. Care 52, 1710–1717 (2007).
Khamiees, M., Raju, P., DeGirolamo, A., Amoateng-Adjepong, Y. & Manthous, C. A. Predictors of extubation outcome in patients who have successfully completed a spontaneous breathing trial. Chest 120, 1262–1270 (2001).
Rogers, D. F. Physiology of airway mucus secretion and pathophysiology of hypersecretion. Respir. Care 52, 1134–1146 (2007).
Ngo, C., Dahlmanns, S., Vollmer, T., Misgeld, B. & Leonhardt, S. Object-oriented modeling of thoracic fluid balance to study cardiogenic pulmonary congestion in humans. Comput. Methods Progr. Biomed. 180, 104998 (2019).
Solymosi, E. A. et al. Chloride transport-driven alveolar fluid secretion is a major contributor to cardiogenic lung edema. Proc. Natl. Acad. Sci. U.S.A. 110, E2308–E2316 (2013).
Jan, R., Alahdal, A. & Bithal, P. K. Effect of two regimens of fluid administration on airway edema in prone-position surgery. Anesth. Essays Res. 14, 467–473 (2020).
Sole, M. L., Bennett, M. & Ashworth, S. Clinical indicators for endotracheal suctioning in adult patients receiving mechanical ventilation. Am. J. Crit. Care 24, 318–324 (2015).
Sackner, M. A., Landa, J. F., Greeneltch, N. & Robinson, M. J. Pathogenesis and prevention of tracheobronchial damage with suction procedures. Chest 64, 284–290 (1973).
Bhattacharya, M., Kallet, R. H., Ware, L. B. & Matthay, M. A. Negative-pressure pulmonary edema. Chest 150, 927–933 (2016).
Ouellette, D. R. et al. Liberation from mechanical ventilation: An official American College of Chest Physicians/American Thoracic Society Clinical Practice Guideline: Inspiratory pressure augmentation during spontaneous breathing trials, protocols minimizing sedation, and non-invasive ventilation immediately after extubation. Chest 151, 166–180 (2017).
Li, Y., Li, H. & Zhang, D. Comparison of T-piece and pressure support ventilation as spontaneous breathing trials in critically ill patients: A systematic review and meta-analysis. Crit. Care 24, 67 (2020).
Jung, B., Vaschetto, R. & Jaber, S. T. tips to optimize weaning and extubation success in the critically ill. Intensive Care Med. 46, 2461–2463 (2020).
Acknowledgements
We would like to thank all the staff of the participating ICU for the supervision of this project and the assistance with the data collection.
Author information
Authors and Affiliations
Contributions
Study concept and design: A.T., A.U. and Y.F. Data acquisition: A.T., Y.H., R.H., R.S., Y.K., H.E., T.Y., A.M., K.S., D.H., N.I. and N.O. Data processing and interpretation: A.T., Y.H., R.H., R.S., Y.K., H.E., T.Y., A.M., K.S., D.H., N.I. and N.O. Statistical analysis: A.T., A.U. and Y.F. Figure preparation: A.T. Drafting of the manuscript: A.T. Revision of the manuscript for important intellectual content: A.T., A.U., T.Y. and Y.F. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tanaka, A., Uchiyama, A., Horiguchi, Y. et al. Predictors of post-extubation stridor in patients on mechanical ventilation: a prospective observational study. Sci Rep 11, 19993 (2021). https://doi.org/10.1038/s41598-021-99501-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99501-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.