Abstract
Pneumonia is one of the top 10 diseases by morbidity in Bhutan. This study aimed to investigate the spatial and temporal trends and risk factors of childhood pneumonia in Bhutan. A multivariable Zero-inflated Poisson regression model using a Bayesian Markov chain Monte Carlo simulation was undertaken to quantify associations of age, sex, altitude, rainfall, maximum temperature and relative humidity with monthly pneumonia incidence and to identify the underlying spatial structure of the data. Overall childhood pneumonia incidence was 143.57 and 10.01 per 1000 persons over 108 months of observation in children aged < 5 years and 5–14 years, respectively. Children < 5 years or male sex were more likely to develop pneumonia than those 5–14 years and females. Each 1 °C increase in maximum temperature was associated with a 1.3% (95% (credible interval [CrI] 1.27%, 1.4%) increase in pneumonia cases. Each 10% increase in relative humidity was associated with a 1.2% (95% CrI 1.1%, 1.4%) reduction in the incidence of pneumonia. Pneumonia decreased by 0.3% (CrI 0.26%, 0.34%) every month. There was no statistical spatial clustering after accounting for the covariates. Seasonality and spatial heterogeneity can partly be explained by the association of pneumonia risk to climatic factors including maximum temperature and relative humidity.
Similar content being viewed by others
Introduction
Pneumonia is a major cause of morbidity and mortality1. Each year, pneumonia accounts for over 12 million hospital admissions and 1.3 million deaths in children aged < 5 years worldwide2,3. In 2017, pneumonia was the second-leading cause of death in children aged < 5 years and it is estimated to remain the case through to 20404. Mortality is disproportionately higher in low-income and middle-income countries (LMICs), where 95–99% of pneumonia-specific < 5 deaths occur5. Children < 5 years in LMICs experience 0.28 episodes per child-year, with the highest rates and predominantly reported in South Asia and sub-Saharan Africa6,7.
Pneumonia is a potentially life-threatening illness with a particularly high burden in South Asia and sub-Saharan Africa3,8,9. It is not only a major cause of morbidity and mortality but is also associated with a substantial economic burden on healthcare systems10,11 and household income12. Pneumonia often has a complex aetiology involving multiple pathogens, including many that are transmitted person-to-person. Past time-series analyses have identified various pneumonia and influenza outcomes to be temporally seasonal, demonstrating highly consistent peaks in winter months and troughs in summer months13,14. Other studies have found that pneumonia admissions were highly spatially clustered15, driven by contact with infected people during indoor activities16.
Pneumonia continues to be an important communicable disease in Bhutan, located in the Eastern Himalayas17,18,19 (Fig. 1). In 2019, pneumonia was one of the top-ten ranked diseases in Bhutan, accounting for 19% of the overall disease burden20. In the financial year 2017–2018, 7.1% of the Bhutanese government’s health expenditure was spent on treating infectious respiratory diseases19,21. Despite the importance of pneumonia, and the infectious nature of the disease, there have been no previous studies to understand the underlying ecological drivers of pneumonia in Bhutan22,23. Understanding the spatial and temporal patterns of pneumonia will be important for prevention and preparedness through more efficient targeting of scarce healthcare resources. In this study, we investigated the trends of childhood pneumonia in Bhutan, identified potential high-risk geographical areas and quantified associations between disease risk and climatic risk factors.
Results
Descriptive analysis
A total of 83,315 paediatric pneumonia cases were reported in Bhutan during the study period (2010–2018). This corresponded to 71,807 and 11,508 cases in children aged < 5 years and 5–14 years, with an incidence of 143.57 and 10.01, respectively, per 1000 persons during the nine years (Table 1). In both age groups, incidence decreased from 173.18 and 82.28 cases per 1000 persons in 2010 to 11.32 and 6.62 cases per 1000 persons in 2018 for the < 5 years and 5–14 years age groups, respectively (Table 1). The seasonal and trend decomposition using loess (STL) of monthly pneumonia cases based on locale is illustrated in Fig. 2. The highest number of cases was reported in 2012, and pneumonia displayed a strong seasonal pattern, with peaks in May and September of each year (Supplementary Fig. 1 and 2). The average standardized morbidity ratio (SMR) of pneumonia at sub-district level was 9.6 (range: 0 to 49.8; Standard Deviation of 9.7). The SMR for Haa, Paro, Gasa, Bumthang and Wandue was lower than average, whilst for Chukha, Mongar, Samtse, Sarpang, Samdrup Jongkhar and Thimphu districts, the SMR was higher than average (Fig. 3).
Spatio-temporal model
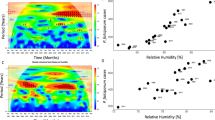
Model I, which contained the unstructured random effects, had the lowest deviation information criterion (DIC) (159.881.0), and was thus better fitting than Model II and Model III, which contained the spatially structured random effects. The incidence of pneumonia was 14 times (95% credible interval [CrI] 13.96, 14.59) higher in children aged < 5 years as compared to those 5–14 years. Females were 11.3% (95% CrI 10.0%, 12.5%) less likely to develop pneumonia compared to males. The burden of pneumonia decreased by 0.3% (95% CrI 0.26%, 0.34%) every month. Each 1 °C increase in the maximum temperature was associated with a 1.3% (95% CrI 1.27%, 1.4%) increase in pneumonia cases. Conversely, each 10% increase in relative humidity was associated with a 1.2% (95% CrI 1.1%, 12.5%) decrease in the incidence of pneumonia (Table 2).
There was no statistical evidence of spatial clustering after accounting for the covariates (Table 2 and Fig. 4). There was > 95% probability of a lower than the national average trend of pneumonia in 56/205 sub-districts, whereas 66/205 sub-districts had > 95% probability of a trend more than the national average. There was no clear spatial pattern, with sub-districts showing higher and lower average trends across all the 20 districts (Fig. 5).
Discussion
This is the first study to have explored the climatic and geographic effects on childhood pneumonia in Bhutan. Pneumonia was spatially and temporally heterogeneous across sub-districts of Bhutan during the study period. There was a decreasing trend in disease burden from 2010 through 2018, in addition to a strong seasonal pattern. Pneumonia mainly affected males and children aged < 5 years. Maximum temperature were associated with an increased incidence of pneumonia, while relative humidity was associated with a decreased incidence of disease.
In addition to climatic factors, spatial heterogeneity could be due to differences in the socio-demographic characteristics of sub-districts. Known risk factors responsible for exacerbation and spread of pneumonia in Bhutan include low birth weight, malnutrition, indoor air pollution, overcrowded households, lack of breastfeeding in infants, and poor personal and environmental hygiene24,25. This was evident from the two districts of Haa and Paro, which have the lowest poverty levels26, and also reported lowest SMR associated with pneumonia. Similar to the decreasing trend in the incidence of global childhood pneumonia6, the pneumonia trend in Bhutan decreased during the study period from 2015 onwards. This could be attributed to a decrease in exposure to key risk factors including poor housing conditions and overcrowding, incomplete immunisation and malnutrition6.
Pneumonia is the single largest infectious cause of death in children worldwide. It accounts for 15% of all deaths of children < 5 years27. In this study, children < 5 years were at a much higher risk of pneumonia compared to those 5–14 years old. Infants (aged between 0–11 months) were reported to contribute up to 24.2% of pneumonia cases in another study from Bhutan28. The WHO and United Nations Children’s Fund (UNICEF) initiated a global action plan for pneumonia and diarrhoea (GAPPD) to accelerate pneumonia control in children29. The GAPPD strategies include promoting: (1) exclusive breastfeeding and adequate complementary feeding to protect children from pneumonia; (2) vaccination; (3) hand hygiene; (4) reductions in household air pollution; (5) HIV prevention; (6) co-trimoxazole prophylaxis for HIV infected and exposed children; and (7) treatment of childhood pneumonia with antibiotics and oxygen. Strengthening GAPPD strategies should be considered in Bhutan, as is the case in other countries in South Asia (including Bangladesh and India). The introduction of pneumococcal conjugate vaccines (PCVs) in Bhutan in 2019 is timely in prevention of pneumonia, and the effect of introduction of PCV on the burden of childhood pneumonia in Bhutan must be evaluated21,30. Exclusive breastfeeding rates from birth until six months in Bhutan varies from 35.9 to 51.0%31,32. Increasing exclusive breastfeeding rates are likely to reduce pneumonia associated morbidity33.
Pneumonia incidence was highly seasonal, and was associated with climatic factors including temperature and relative humidity. The association of temperature with pneumonia has been reported in other studies34,35. A plausible explanation is the association of higher temperature with air pollution36 which in itself is known risk factor and cause of pneumonia7,37,38,39. Most industries are located in the southern parts of Bhutan where air pollution is expected to be higher as compared to other districts. This was reflected by these sub-districts having higher SMR for pneumonia. Additionally, traditional methods of cooking in rural Bhutan using fire wood could also contribute to respiratory illness such as pneumonia40,41.
The incidence of pneumonia tends to be higher during the rainy season but not so in this study42,43,44. Rainfall may trigger socio-ecological behavioural changes such as increased contact between people and the distribution of pathogens. Further, heavy rainfall during the monsoon is likely to pollute drinking water, particularly surface water from streams, which is the main drinking water source for rural populations45. Unsafe drinking water and sanitation are important drivers of pneumonia46. Relative humidity was associated with a decrease in pneumonia incidence in this study which is in concordance with other studies35,47. Higher relative humidity decreases the survival of lipid-enveloped viruses such as influenza A, influenza b and respiratory syncytial virus48,49.
There are a number of limitations that need to be considered when interpreting the results of this study. First, the study used routine case reports to measure pneumonia incidence. Known issues exist surrounding completeness and representativeness of such data. Secondly, the causal organisms of pneumonia were not available and the association could be different based on the organisms. Thirdly, there was no reconciliation to accommodate different levels of aggregation of the climate variables (district) and the disease data (sub-district), and the climate conditions were assumed to be homogeneous within a district. Lastly, unaccounted risk modifiers were not included in the modelling due to a lack of available data. These important unmeasured factors, such as immunization coverage, air pollution level, living standards and socio-economic status, crowding, smoking, access to safe drinking water and latrine usage might have resulted in confounding, which was not able to be quantified39,50,51.
Despite these limitations, the strengths of this study are the capacity to implement the spatial analysis at a relatively fine resolution, being the sub-district level, and over an extended time series (108 months). Traditionally, spatial patterns of infectious disease risk have been displayed at larger geographical units, such as a district, province, national, regional, and global scales45,52,53. Such low resolution can mask localized disease patterns due to averaging54.
Conclusion
Pneumonia is an important childhood disease and the introduction of PCVs to reduce the burden of this disease is timely. Pneumonia was highly seasonal and spatially heterogeneous across sub-districts. Seasonality can be explained by climatic factors including maximum temperature and relative humidity. The spatial and temporal variability of pneumonia should inform prevention and control efforts in Bhutan, through rational decision making and proper resources allocation.
Materials and methods
Study area
Bhutan, located in the Eastern Himalayas, borders China in the north and India in the east, south and west. The country is divided administratively into 20 districts and 205 sub-districts, with a total projected population of 735,553 (189,446 under 15 years) in 201755. Around 62.2% (452,178) of the population live in rural areas and practice subsistence farming. The altitude ranges from 75 m above sea level in the south to more than 7000 m in the Himalayas (Fig. 1).
Study design and data source
This is a retrospective study using secondary data on pneumonia from January 2010 to December 2018, stratified by sex and age (< 5 years and 5–14 years) at the sub-district level. The data were obtained from the National Acute Respiratory Infections surveillance system, hosted by the Bhutan Health Information and Management Systems (HIMS) under the Bhutan Ministry of Health. These data contain all pneumonia cases treated by health centres including hospitals and primary health care facilities and reported to the HIMS every month. Pneumonia is defined as “a patient with history of cough or reported breathing difficulty, and increased respiratory rate, (respiratory rate ≥ 50 breaths per minute in children aged two months or more and less than 12 months, or repiratory rate ≥ 40 breaths per minute in children aged 12 months or more and less than 60 months) or chest indrawing”56. Daily climatic variables (rainfall, relative humidity, minimum and maximum temperature) were obtained from the National Centre for Hydrology and Meteorology under the Ministry of Economic Affairs of Bhutan. Monthly average climatic variables were calculated at the district level because they were available only at the district level. Population estimates used in the study were obtained from the National Statistical Bureau, Bhutan57. Administrative boundary maps were downloaded from the DIVA-GIS website58.
Crude standardized morbidity ratios
An initial descriptive analysis of pneumonia incidence across the country was conducted. Crude SMR for each sub-district were calculated using the following formula:
where Y is the overall SMR in sub-district i, O is the total number of observed pneumonia cases over the entire study period in the sub-district and E is the expected number of pneumonia cases in the sub-district across the study period. The expected number was calculated by multiplying the national incidence by the average population for each sub-district over the study period.
Exploration of seasonal patterns and inter-annual patterns
The time series of pneumonia incidence was decomposed using STL weighted regression to show: the seasonal pattern, inter-annual patterns and the residual variability. The STL model was structured as follows:
where Yt represents numbers of local pneumonia cases with logarithmic transformation, St is the additive seasonal component, Tt is the trend, and Rt is the “remainder component”; t is time in months59,60.
Spatio-temporal model
A Bayesian statistical framework was deployed for spatial analysis. It provides a convenient framework for the simultaneous inclusion of covariates and spatial autocorrelation in a single model, while providing robust evaluation and expression of uncertainty. The posterior distributions can be used to quantify uncertainties in parameters of interest (e.g., covariate effects and spatial patterns of disease risk)61.
Initially, a preliminary bivariate Poisson regression of pneumonia cases was undertaken to select the covariates. The covariates were altitude and climatic variables including rainfall, minimum and maximum temperature and relative humidity without lag, and lagged up to 3 months. The covariates with a p-value of < 0.05 and the lowest Akaike's information criterion (AIC) were selected (Supplementary Table 1). The co-linearity of the selected climatic and environmental variables was tested using variance inflation factors (VIF) (Supplementary Table 2). In the final model, altitude, and rainfall, maximum temperature without lag and relative humidity lagged at 3 months were included.
Of the 83,315 observations stratified by sub-districts, age (< 5 and 5–14 years) and sex over an observation period of 108 months, there were 63,742 (72%) zero counts of pneumonia. Therefore, Zero-inflated Poisson (ZIP) regression was constructed in a Bayesian framework (Supplementary Table 3). The first model (Model I), assumed that spatial autocorrelation was not present in the relative risk of pneumonia. This model was developed with selected climatic factors (rainfall, maximum temperature and relative humidity), altitude, age (< 5 and 5–14 years) and gender as explanatory variables, and an unstructured random effect for sub-districts. The second model (Model II) contained a spatially structured random effect in addition to the aforementioned covariates. Model III, a convolution model, contained all of the components of the preceding two models. The model with the lowest DIC was selected as the final explanatory model.
Model III assumed that the observed counts of pneumonia, Y, for the ith sub-district (i = 1 … 205) in the jth month (January 2010–December 2018) followed a Poisson distribution with mean (μij), that is,
where the expected number of cases in sub-district i, month j (acting as an offset to control for population size) was represented by Eij and θij is the mean log relative risk (RR). The intercept (α), and coefficients for age (5–14 years as reference), sex (male as reference), monthly trend, altitude, rainfall, relative humidity and maximum temperature are β1, β2, β3, β4, β5, β6 and β7. The spatially unstructured and structured random effects are represented as ui and si, respectively, with ui excluded from Model II and si excluded from Model I. Spatiotemporal random effect with a mean of zero and variance of σw2 was denoted by wi as in other studies62,63.
A conditional autoregressive (CAR) prior structure was used to model the spatially structured random effect. Spatial relationships between the sub-districts were based on a ‘queen’ contiguity matrix64. A weight of 1 was assigned to sub-districts sharing a border and 0 otherwise. A flat prior distribution was specified for the intercept, whereas non-informative normal prior distributions (mean = 0.0, precision = 0.00001) were used for the coefficients. The priors for the precision of unstructured and spatially structured random effects were specified using non-informative gamma distributions with shape and scale parameters of 0.5, 0.001.
Markov Chain Monte Carlo simulation was used to estimate model parameters65. The models were run for an initial 10,000 iterations for burn in, which were then discarded. Subsequently, visual inspection of posterior density and history plots were used to note convergence at intervals of 20,000 iterations. Convergence occurred at approximately 100,000 iterations for all models. Following convergence, posterior distributions from model parameters were stored for inference. Summaries of parameters were calculated, including posterior mean and 95% CrI. In the Bayesian analyses, RR with 95% CrI that excluded 1 were considered statistically significant.
Seasonality decomposition was carried out using the R statistical software, version 3.3.166. The ZIP regression model was constructed using WinBUGS software, version 1.4.3 (MRC Biostatistics Unit 2008)67. ArcMap 10.5 software (ESRI, Redlands, CA) was used to generate maps of the posterior means of the unstructured and structured random effects and the spatiotemporal random effects.
Ethical approval and patient confidentiality
Administrative approval to use these datasets was provided by the Ministry of Health, Bhutan. This study was a low-risk study since the surveillance data did not contain identifying information on individual participants.
Data availability
The datasets of the current study will be made available from the corresponding author on reasonable request.
Change history
15 November 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41598-021-01075-y
References
WHO. Pneumonia, The Forgotten Killer of Children (UNICEF/WHO, 2006).
Nair, H. et al. Global and regional burden of hospital admissions for severe acute lower respiratory infections in young children in 2010: A systematic analysis. Lancet 381, 1380–1390. https://doi.org/10.1016/s0140-6736(12)61901-1 (2013).
WHO. Pneumonia. https://www.who.int/en/news-room/fact-sheets/detail/pneumonia (2019).
Institute for Health Metrics and Evaluation (IHME). Findings from the Global Burden of Disease Study (Institute for Health Metrics and Evaluation (IHME), 2018).
(IVAC), I. V. A. C. 1–42 (Johns Hopkins Bloomberg School of Public Health, 2015).
McAllister, D. A. et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: A systematic analysis. Lancet Glob. Health 7, e47–e57. https://doi.org/10.1016/s2214-109x(18)30408-x (2019).
Rudan, I., Boschi-Pinto, C., Biloglav, Z., Mulholland, K. & Campbell, H. Epidemiology and etiology of childhood pneumonia. Bull. World Health Organ. 86, 408–416. https://doi.org/10.2471/blt.07.048769 (2008).
Di Pasquale, M. F. et al. Prevalence and etiology of community-acquired pneumonia in immunocompromised patients. Clin. Infect. Dis. 68, 1482–1493. https://doi.org/10.1093/cid/ciy723 (2019).
Franco, J. Community-acquired pneumonia. Radiol. Technol. 88, 621–636 (2017).
Prina, E., Ranzani, O. T. & Torres, A. Community-acquired pneumonia. Lancet 386, 1097–1108. https://doi.org/10.1016/s0140-6736(15)60733-4 (2015).
Tan, K. K. et al. Burden of hospitalized childhood community-acquired pneumonia: A retrospective cross-sectional study in Vietnam, Malaysia, Indonesia and the Republic of Korea. Hum. Vaccin Immunother. 14, 95–105. https://doi.org/10.1080/21645515.2017.1375073 (2018).
Sabin, L. L. et al. Household costs associated with hospitalization of children with severe pneumonia in Quito, Ecuador. Am. J. Trop. Med. Hyg. 102, 731–739. https://doi.org/10.4269/ajtmh.19-0721 (2020).
Farrar, D. S. et al. Seasonal variation and etiologic inferences of childhood pneumonia and diarrhea mortality in India. Elife https://doi.org/10.7554/eLife.46202 (2019).
Nimbalkar, P. M. & Tripathi, N. K. Space-time epidemiology and effect of meteorological parameters on influenza-like illness in Phitsanulok, a northern province in Thailand. Geospat. Health. 11, 447. https://doi.org/10.4081/gh.2016.447 (2016).
Crighton, E. J., Elliott, S. J., Moineddin, R., Kanaroglou, P. & Upshur, R. E. An exploratory spatial analysis of pneumonia and influenza hospitalizations in Ontario by age and gender. Epidemiol. Infect. 135, 253–261. https://doi.org/10.1017/s095026880600690x (2007).
Paynter, S., Ware, R. S., Weinstein, P., Williams, G. & Sly, P. D. Childhood pneumonia: A neglected, climate-sensitive disease?. Lancet 376, 1804–1805. https://doi.org/10.1016/s0140-6736(10)62141-1 (2010).
MoH. (Ministry of Health, 2018).
MoH. (Ministry of Health, 2017).
MoH. (Ministry of Health, 2019).
MoH. (Ministry of Health, 2020).
Dorji, K. et al. Towards the introduction of pneumococcal conjugate vaccines in Bhutan: A cost-utility analysis to determine the optimal policy option. Vaccine. 36, 1757–1765. https://doi.org/10.1016/j.vaccine.2018.02.048 (2018).
Jullien, S., Pradhan, D. & Bassat, Q. Pneumonia in Bhutanese children: what we know, and what we need to know. Pneumonia 12, 1. https://doi.org/10.1186/s41479-019-0065-x (2020).
Jullien, S. et al. Pneumonia in children admitted to the national referral hospital in Bhutan: A prospective cohort study. Int. J. Infect. Dis. 95, 74–83. https://doi.org/10.1016/j.ijid.2020.04.017 (2020).
Wangchuk, S., Zangmo, S. & Thapa, B. Epidemiological analysis of Influenza–Like Illness and Severe Acute Respiratory Infection surveillance for 2011 6 (Public Health Laboratory, 2011).
Balaraman, K. Assignment Report on Acute Respiratory Infections in Bhutan: Review of the Magnitude of the Problem and Formulation of Strategies for Prevention and Control, 27 November 1985–7 January 1986. (1987).
RGoB. Bhutan Poverty Analysis Report 2017 (Royal Government of Bhutan, 2017).
WHO. Ending Preventable Child Deaths from Pneumonia and Diarrhoea by 2025 (WHO, 2013).
Sangay, N. Effects of indoor air pollution on risk of acute respiratory infection and other respiratory problem in children under five in Thimphu, Bhutan MPH Thesis thesis, College of Public Health, Chulalongkorn University, (2004).
WHO. End Preventable Deaths: Global Action Plan for Prevention and Control of Pneumonia and Diarrhoea (World Health Organization and United Nations Children’s Fund, 2013).
Ojal, J. et al. Sustained reduction in vaccine-type invasive pneumococcal disease despite waning effects of a catch-up campaign in Kilifi, Kenya: A mathematical model based on pre-vaccination data. Vaccine 35, 4561–4568. https://doi.org/10.1016/j.vaccine.2017.07.019 (2017).
Pokhrel, H. P., Pavadhgul, P. & Srisorrachatr, S. Factors associated with exclusive breastfeeding practices in western Bhutan. Bhutan Health J. 4, 13–22 (2018).
MoH. National Nutrition Survey. (Ministry of Health, RGoB, 2015).
Hanieh, S. et al. Exclusive breast feeding in early infancy reduces the risk of inpatient admission for diarrhea and suspected pneumonia in rural Vietnam: A prospective cohort study. BMC Public Health 15, 1166. https://doi.org/10.1186/s12889-015-2431-9 (2015).
Ho, N. T. et al. Retrospective analysis assessing the spatial and temporal distribution of paediatric acute respiratory tract infections in Ho Chi Minh City, Vietnam. BMJ Open 8, e016349. https://doi.org/10.1136/bmjopen-2017-016349 (2018).
Silva, D. R., Viana, V. P., Muller, A. M., Livi, F. P. & Dalcin Pde, T. Respiratory viral infections and effects of meteorological parameters and air pollution in adults with respiratory symptoms admitted to the emergency room. Influenza Other Respir. Viruses 8, 42–52. https://doi.org/10.1111/irv.12158 (2014).
Ayres, J. G. et al. Climate change and respiratory disease: European Respiratory Society position statement. Eur. Respir. J. 34, 295–302. https://doi.org/10.1183/09031936.00003409 (2009).
Nhung, N. T. T. et al. Short-term association between ambient air pollution and pneumonia in children: A systematic review and meta-analysis of time-series and case-crossover studies. Environ. Pollut. 230, 1000–1008. https://doi.org/10.1016/j.envpol.2017.07.063 (2017).
Gordon, S. B. et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2, 823–860. https://doi.org/10.1016/s2213-2600(14)70168-7 (2014).
Ruchiraset, A. & Tantrakarnapa, K. Time series modeling of pneumonia admissions and its association with air pollution and climate variables in Chiang Mai Province, Thailand. Environ. Sci. Pollut. Res. Int. 25, 33277–33285. https://doi.org/10.1007/s11356-018-3284-4 (2018).
Langbein, J. Firewood, smoke and respiratory diseases in developing countries: The neglected role of outdoor cooking. PLoS ONE 12, e0178631. https://doi.org/10.1371/journal.pone.0178631 (2017).
Juntarawijit, Y. & Juntarawijit, C. Cooking smoke exposure and respiratory symptoms among those responsible for household cooking: A study in Phitsanulok, Thailand. Heliyon 5, e01706. https://doi.org/10.1016/j.heliyon.2019.e01706 (2019).
Singh, V., Sharma, B. B., Patel, V. & Poonia, S. Clinical profile of pneumonia and its association with rain wetting in patients admitted at a tertiary care institute during pandemic of influenza A (H1N1) pdm09 virus infection. Indian J. Chest Dis. Allied Sci. 56, 21–26 (2014).
Paynter, S. et al. Sunshine, rainfall, humidity and child pneumonia in the tropics: Time-series analyses. Epidemiol. Infect. 141, 1328–1336. https://doi.org/10.1017/s0950268812001379 (2013).
Chowdhury, F. R. et al. The association between temperature, rainfall and humidity with common climate-sensitive infectious diseases in Bangladesh. PLoS ONE 13, e0199579. https://doi.org/10.1371/journal.pone.0199579 (2018).
Wangdi, K. & Clements, A. C. Spatial and temporal patterns of diarrhoea in Bhutan 2003–2013. BMC Infect. Dis. 17, 507. https://doi.org/10.1186/s12879-017-2611-6 (2017).
Gessner, B. D. Lack of piped water and sewage services is associated with pediatric lower respiratory tract infection in Alaska. J. Pediatr. 152, 666–670. https://doi.org/10.1016/j.jpeds.2007.10.049 (2008).
Tasci, S. S., Kavalci, C. & Kayipmaz, A. E. Relationship of meteorological and air pollution parameters with pneumonia in elderly patients. Emerg. Med. Int. 2018, 4183203. https://doi.org/10.1155/2018/4183203 (2018).
Schaffer, F. L., Soergel, M. E. & Straube, D. C. Survival of airborne influenza virus: Effects of propagating host, relative humidity, and composition of spray fluids. Arch. Virol. 51, 263–273. https://doi.org/10.1007/bf01317930 (1976).
Tellier, R. Aerosol transmission of influenza A virus: A review of new studies. J. R. Soc. Interface 6(Suppl 6), S783-790. https://doi.org/10.1098/rsif.2009.0302.focus (2009).
Amsalu, E. T., Akalu, T. Y. & Gelaye, K. A. Spatial distribution and determinants of acute respiratory infection among under-five children in Ethiopia: Ethiopian Demographic Health Survey 2016. PLoS ONE 14, e0215572. https://doi.org/10.1371/journal.pone.0215572 (2019).
Beninca, E., van Boven, M., Hagenaars, T. & van der Hoek, W. Space-time analysis of pneumonia hospitalisations in the Netherlands. PLoS ONE 12, e0180797. https://doi.org/10.1371/journal.pone.0180797 (2017).
Clements, A. C., Barnett, A. G., Cheng, Z. W., Snow, R. W. & Zhou, H. N. Space-time variation of malaria incidence in Yunnan province, China. Malar. J. 8, 180. https://doi.org/10.1186/1475-2875-8-180 (2009).
Hundessa, S. H. et al. Spatial and space-time distribution of Plasmodium vivax and Plasmodium falciparum malaria in China, 2005–2014. Malar. J. 15, 595. https://doi.org/10.1186/s12936-016-1646-2 (2016).
Haddow, A. D., Jones, C. J. & Odoi, A. Assessing risk in focal arboviral infections: Are we missing the big or little picture?. PLoS ONE 4, e6954. https://doi.org/10.1371/journal.pone.0006954 (2009).
NSB. 2017 Population and Housing Census of Bhutan: Natioanl Report. (2019).
WHO. (ed World Health Organization, 2014).
National Statistical Bureau. (2017).
DIVA-GIS. https://www.diva-gis.org/
Cleveland, R. B. STL: A Seasonal-Trend decomposition Prodecures Based on Loess. J. Off. Stat. 6, 3–73 (1990).
Wangdi, K., Clements, A. C. A., Du, T. & Nery, S. V. Spatial and temporal patterns of dengue infections in Timor-Leste, 2005–2013. Parasites Vectors 11, 9. https://doi.org/10.1186/s13071-017-2588-4 (2018).
Basanez, M. G., Marshall, C., Carabin, H., Gyorkos, T. & Joseph, L. Bayesian statistics for parasitologists. Trends Parasitol. 20, 85–91 (2004).
Wangdi, K. et al. A spatio-temporal analysis to identify the drivers of malaria transmission in Bhutan. Sci. Rep. 10, 7060. https://doi.org/10.1038/s41598-020-63896-7 (2020).
Wangdi, K. et al. Analysis of clinical malaria disease patterns and trends in Vietnam 2009–2015. Malar. J. 17, 332. https://doi.org/10.1186/s12936-018-2478-z (2018).
Rouamba, T., Samadoulougou, S., Tinto, H., Alegana, V. A. & Kirakoya-Samadoulougou, F. Bayesian spatiotemporal modeling of routinely collected data to assess the effect of health programs in malaria incidence during pregnancy in Burkina Faso. Sci. Rep. 10, 2618. https://doi.org/10.1038/s41598-020-58899-3 (2020).
Gelfand, A. E. & Smith, A. F. M. Sampling-based approaches to calculating marginal densities. J. Am. Stat. Assoc. 85, 398–409. https://doi.org/10.1080/01621459.1990.10476213 (1990).
Team & R. C. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2021).
Thomas, A., Best, N., Lunn, D., Arnold, R. & Spiegelhalter, D. GeoBUGS User Manual Version 1.2 (Medical Research Council Biostatistics Unit, 2004).
Acknowledgements
The authors would like to thank the Bhutan Ministry of Health for allowing to use these surveillance data.
Author information
Authors and Affiliations
Contributions
K.W. and K.P. were involved in the conception of the study. K.W. and T.T. undertook the analysis. K.P. and C.T. obtained the data. K.W. and K.P. drafted the manuscript. A.C.A.C., P.G. and D.J.G. critically reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in Figure 3 where the crude standardized morbidity ratios were incorrectly calculated, resulting in errors in the map and key. As a result, in the Results section under the subheading ‘Descriptive analysis’, “The average standardized morbidity ratio (SMR) of pneumonia at sub-district level was 44.72 (range: 1.55 to 1397.9; Standard Deviation of 102.05)” now reads: “The average standardized morbidity ratio (SMR) of pneumonia at sub-district level was 9.6 (range: 0 to 49.8; Standard Deviation of 9.7).” Additionally, “The SMR for Haa, Paro, Gasa, Bumthang and Wandue was lower than average, whilst for Bumthang, Chukha, Mongar, Samtse, Sarpang, Samdrup Jongkhar and Thimphu districts, the SMR was higher than average (Fig. 3)” now reads: “The SMR for Haa, Paro, Gasa, Bumthang and Wandue was lower than average, whilst for Chukha, Mongar, Samtse, Sarpang, Samdrup Jongkhar and Thimphu districts, the SMR was higher than average (Fig. 3).”
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wangdi, K., Penjor, K., Tsheten, T. et al. Spatio-temporal patterns of childhood pneumonia in Bhutan: a Bayesian analysis. Sci Rep 11, 20422 (2021). https://doi.org/10.1038/s41598-021-99137-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99137-8
This article is cited by
-
Spatial patterns and spatially-varying factors associated with childhood acute respiratory infection: data from Ethiopian demographic and health surveys (2005, 2011, and 2016)
BMC Infectious Diseases (2023)
-
Dynamic spatiotemporal correlation coefficient based on adaptive weight
Financial Innovation (2023)
-
How do temperature and precipitation drive dengue transmission in nine cities, in Guangdong Province, China: a Bayesian spatio-temporal model analysis
Air Quality, Atmosphere & Health (2023)
-
Identifying socio-ecological drivers of common cold in Bhutan: a national surveillance data analysis
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.