Abstract
It is widely acknowledged that efficiency of pediatric critical care transport plays a vital role in treatment of critically-ill children. In developing countries, most critically-ill children were transported by ambulance, and a few by air, such as a helicopter or fixed airplane. High-speed train (HST) transport may be a potential choice for critically-ill children to a tertiary medical center for further therapy. This is a single-center, retrospective cohort study from June 01, 2016 to June 30, 2019. All the patients transported to the Pediatric Intensive Care Unit (PICU) of PLA general hospital were divided into two groups, HST group and ambulance group. The propensity score matching method was performed for the comparison between the two groups. Finally, a 2:1 patient matching was performed using the nearest-neighbor matching method without replacement. The primary outcome was hospital mortality. Secondary outcomes included duration of transport, transport cost, hospital stay, and hospitalization cost. A total of 509 critically-ill children were transported and admitted. Of them, 40 patients were transported by HST, and 469 by ambulance. The hospital mortality showed no difference between the two groups (p > 0.05). The transport distance in the HST group was longer than that in the ambulance group (1894.5 ± 907.09 vs. 902.66 ± 735.74, p < 0.001). However, compared to the HST group, the duration of transport time by ambulance was significantly longer (p < 0.001). No difference in vital signs, blood gas analysis, and critical illness score between groups at admission was noted (p > 0.05). There was no death during the transport. There was no difference between groups regarding the transport cost, hospital stays, and hospitalization cost (p > 0.05). High-quality tertiary medical centers are usually located in megacities. HST transport network for critically-ill children could be established to cover most regions of the country. Without increasing financial burden, HST medical transport can be a potentially promising option to improve the outcomes of critically-ill children in developing countries with developed HST network.
Clinical Trial Registration: This study was registered at http://www.chictr.org.cn/index.aspx (chiCTR.gov; Identifier: ChiCTR2000032306).
Similar content being viewed by others
The vital role of pediatric critical care transport has been widely acknowledged in the past 30 years with evidence showing that a pediatric transport team can improve the outcomes of critically-ill children1,2. Currently, most critically-ill children are transported by ambulance and a few by air, such as helicopters or fixed airplanes. Lack of air transport service is a big challenge to the health system in some remote regions. The advantages of ambulance transport include low cost, point to point, and no need for a parking apron like for a helicopter. However, the shortcoming is also apparent, such as longer duration, due to road and weather conditions3. Air medical transport is quite common in developed countries, which is faster and free from traffic jams. In the case of transport of over 500 km, air medical transport is the best choice4. However, the cost of air medical transport is unaffordable for many families in developing countries, like China, as it is not covered by the National Insurance System. It is urgent to develop an innovative way to transport critically-ill children for over 500 km. High-speed trains (HST) has been developing rapidly in China in recent years. As of in 2019, the HST system has covered almost all parts of China except some remote areas in the west, with a total railway distance of over 35,000 km5. The speed of the HST in China could reach up to 350 km per hour, and the HST network has connected most of the regional medical centers in China, making it a promising innovative modality for long-distance transport6. Although this innovative transport modality has been carried out in China for a few years, its safety and efficacy have not been well defined. This study aimed to clarify whether transportation by HST has superior outcomes compared to ambulance transport.
Methods
Ethical approvals
The study was approved by the Ethics Committee of the People’s Liberation Army general hospital (No.2016-039) (Beijing, China), and registered in ChiCTR (ChiCTR2000032306). Written informed consent was obtained from the parents. The methodology in this study was in accordance with the relevant guidelines and regulations.
Study design
This is a single-center, retrospective cohort study, conducted from June 01, 2016 to June 30, 2019. A total of 509 pediatric patients under 14 years old, who were transported to a tertiary medical center, were recruited in this study. All the children were confirmed with an indication of transport7. Of them, 40 children were transported by HST, and 469 children by ambulance.
HST carriage for medical transport
A modification of the HST carriage was necessary to fit the requirement of critically-ill children's transport. Business-class of HST has enough space to accommodate a medical stretcher and other equipment. Under special conditions, the business-class seat could be regulated to make room for a stretcher for patients. The necessary equipment during transport includes a ventilator, infusion pumps, cardiopulmonary monitor, blood gas analyzer, vacuum extractor, intubation supplies, oxygen cylinder or oxygen generator et al. (Figs. 1 and 2).
Clinical management
Our HST transport program was set up in 2016. All the medical care was provided by our pediatric/neonatal critical care transport team (CCTT). In this program, CCTT was composed of a neonatal and pediatric intensivist and a registered nurse. A checklist of HST transport was reviewed before leaving. During transport, routine management mainly includes intravenous administration of medication, and respiratory supports, including oxygen supply and mechanical ventilation. The choice of respiratory support during transport was dependent upon the comprehensive clinical evaluation. Prostaglandin E1 is considered for some children with patent ductus arteriosus dependent congenital heart disease.
The vital signs, including heart rate, respiratory rate, blood pressure, and peripheral oxygen saturation, were closely monitored during transport. End-tidal carbon dioxide (ETCO2) was placed on the children who needed invasive mechanical ventilation. The vital signs and relevant clinical conditions were regularly recorded in the transportation sheet, and blood gas analysis was obtained immediately at admission to the referral hospital. The critical illness score was assessed and recorded after admission.
Outcomes
The primary outcome was hospital mortality. Secondary outcomes included duration of transport, transport cost, hospital stay and hospitalization cost.
Data collection
All data encompassing demographic data, vital signs, medication, procedure, diagnosis, and other relevant information were extracted from the transport record database. Blood gas analysis was retrospectively read from the hospital information systems.
Statistical analysis
To minimize the effect of confounding factors and potential bias between the ambulance and HST groups, the propensity score was calculated using logistic regression, and a 2:1 patient matching was performed using the nearest-neighbor matching method without replacement. Variables in the matching model were gender, age, body weight, diagnosis, respiratory supports, the pediatric risk of mortality III (PRISMIII), and Score for neonatal acute physiology II (SNAPII). The median of continuous and ordinal variables and the exact conditional maximum likelihood estimation of binary variables were calculated. The characteristics and outcomes of each pair were compared based on the exact sign tests and 95% confidence intervals for the median and estimation.
Results
Working flow and patients’ selection
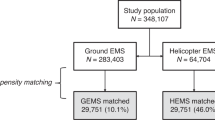
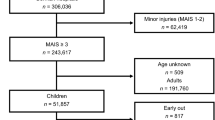
A total of 509 children were transported to PICU between June 01, 2016 and June 30, 2019. Among them, 40 cases were transported by HST, and 469 by ambulance. Propensity score matching (PSM) of 1:2 was performed, and 40 cases in the HST group and 80 cases in the ambulance group were eligible for the analysis in this study. Among them, six and ten children were dead in the HST group and the ambulance group respectively (Fig. 3).
Basic information of HST and ambulance group after PSM
After matching, covariates showed a fine balance for all matched variables. The demographic characteristics, including gender, age and body weight did not show any difference between the HST and ambulance group (p > 0.05), nor did the diagnosis and respiratory supports during transport (p > 0.05). The critical illness scores, including pediatric risk of mortality III (PRISMIII) score and Score for neonatal acute physiology II (SNAPII), also showed no difference between the two groups (p > 0.05). However, as the distance between the referring hospital and the receiving hospital differed greatly (1894.5 ± 907.09 vs. 902.66 ± 735.74, p < 0.001), the transport distance between the two groups was not included for the calculation of propensity score.
Vital signs, blood gas analysis and critical illness score at admission
Vital signs, including heart rate, respiratory rate, systolic pressure, diastolic pressure, and rectal temperature showed no difference between HST and the ambulance group (p > 0.05). The vital parameters of blood gas analysis, including pH, PaO2, PaCO2, and BE, also showed no difference between groups at admission (p > 0.05). The level of lactate in the ambulance group was higher than that in the HST group (2.73 ± 2.76 mmol/L vs.1.66 ± 1.21 mmol/L, p = 0.006). There was no difference in the critical illness score between groups at admission (p > 0.05) (Table 1).
Outcomes
There was no death during transport in both groups. The hospital mortality rate was 12.5% in the ambulance group, compared to 15.0% in the HST group without significant difference (p = 0.704). There was no difference in transport cost, hospital stays and hospitalization cost between HST and ambulance groups (p > 0.05). Compared to the HST group, the duration of transport by ambulance was significantly longer than that of HST (p < 0.001).
Discussion
To our knowledge, this is the first clinical study on HST transport for critically-ill pediatric patients. To our knowledge, most critically-ill pediatric patients were transported by ambulance in developing countries, like China. Due to the limitation of ambulance transport and the high cost of air medical transport, long-distance transport of critically-ill children is still a challenge in developing countries. In this study, our findings suggest that critically-ill children can be transported by HST safely and efficiently, without increasing mortality rate and cost. HST can play an essential role on critically-ill children transport in developing countries and countries with the HST network.
A total of 509 children were transported to our PICU from June 01, 2016 to June 30, 2019, but only 40 cases were transported by the HST. HST transport was not suitable for all children. Firstly, the distance between the two hospitals would limit the use of HST. In regards to patients living close to Beijing, the use of HST would spend much more time than transport by ambulance as the transport between the hospital and the HST station need extra time. As shown in Fig. 4B, transport by HST follows the “referring hospital-ambulance-HST-ambulance-receiving hospital” mode, which needs good coordination and more transfer time between different nodes. Secondly, patients receiving treatment have to be in a city with an HST station. The hospital requesting the transportation service should be close to an HST station so that the patients could be transported timely by ambulance to catch the targeted HST immediately.
(A) China HST Network Map (updated on December 2019). The map was created with Adobe Illustrator CS5 (US), https://www.adobe.com/cn/products/illustrator.html. (B) Door-to-door travel time between San Francisco and Los Angeles by different transports. (C) Door-to-door travel time by different distances between high-speed train and airplane.
It is also convenient for the children to be transported to a tertiary hospital after the HST arrived. The written consent of HST transport should be obtained from parents before CCTT go out. After CCTT arrived at the local hospital and took over the children, an HST with the business-class should be notified immediately. The business-class carriage is the best choice for HST transport as it can provide enough space to accommodate the medical equipment, and for CCTT to perform some medical procedures during transport in case the patient’s condition is not stable. As HST cannot stop unless arriving at a station, so the CCTT cannot call for emergency help during transport. The CCTT should check all the equipment, medication, supplies before they leave the referring hospital. A complete and practical checklist is necessary for HST transport, which can improve CCTT-oriented workflow through both routine and unexpected situations for good outcomes8. During air medical transport, checklists can improve team performance through the prevention of errors and complications9. Meanwhile, it is essential for CCTT to make adequate communication with the crew of HST before initiation of transport. CCTT can refer to them for help during transport if necessary.
This study showed that HST transport was safe for critically-ill children. The vital signs after admission, including heart rate, respiratory rate, blood pressure and rectal temperature, showed no difference in both groups. The result of blood gas analysis and critical illness score at admission was almost no difference. Only the serum lactate in the ambulance group was higher than that in the HST group (Table 1). The underlying cause may be that the children in the ambulance group needed more time for medical transport; they could not receive further therapy timely in the tertiary center. The speed of HST ranges from 250 to 350 km/h in China, which can make medical transport more quickly over the ambulance. In China, the HST network is developing quite well, and many prefecture-level cities have high-speed railway stations (Fig. 4A)6. In addition, another evident advantage of HST transport is that CCTT can be rapidly delivered to the referring hospital by HST so that the critically-ill children could be under the management of CCTT as soon as possible. A recent study was against the “golden hour” in critically-ill children transport, continuing to emphasize the timely delivery of proper care over the speed of transfer10. Some studies have shown that specialized teams for transport could improve outcomes for proper treatment during transport2,11,12. Although sending a specialized team might be time-consuming and delay the critically-ill patients arriving at the tertiary care centers, robust evidence still shows that such teams should be worthy to consider for transport when available.
It is essential to highlight that this study confirmed that the mortality of children in the HST group showed no difference compared with the ambulance group. Proper care provided by CCTT for critically-ill children was critical to the consequence after transporting the children to the tertiary center13. In this study, the comprehensive life support on the HST ensured the stability of critically-ill children during transport. The children in HST could receive all necessary life support that is available in an ambulance, including oxygen therapy, intravenous infusion, invasive ventilation, and vital signs monitoring. The children in need of invasive ventilation were given routine ETCO2 monitoring during HST transport. Continuous ETCO2 monitoring followed by an arterial blood gas measurement of the PaCO2 would allow for a correlation of the PaCO2/ETCO2 concerning dead space ventilation. Some studies have shown that ETCO2 and PaCO2 are approximately correlated within 2 to 5 mmHg in healthy patients, but chronic disease states can cause this difference to increase, leading to ventilation errors14,15. The American Association of Respiratory Care clinical practice guidelines recommends ETCO2 as a method to guide ventilator management16. Our data also indicated that HST transport was more efficient and economical than the ambulance (¥ 2787.5 (1790, 4240) versus 2295(2208.75, 2380.5), p > 0.05, Table 2). Even longer transport distance and business class fare, there was still significantly less time-consuming, and less cost in the HST group. The critical point of pediatric critical transport is to deliver proper medical services and initialize life support for the children as soon as possible. Based on our data, HST transport has achieved this goal, which can offer quality specialty services more efficiently, and does not increase financial burden.
In China, high-quality tertiary medical centers are mainly located in megacities, such as Beijing, Guangzhou and Shanghai17. These cities usually are the centers of HST network as well. HST transport network for critically-ill children could be established to cover most regions of this country. Without increasing financial burden, HST medical transport can be a potentially promising option to improve the outcomes of critically-ill children in developing countries or those countries with developed HST network.
References
Day, S. et al. Pediatric interhospital critical care transport: consensus of a national leadership conference. Pediatrics 88(4), 696–704 (1991).
Orr, R. A. et al. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics 124(1), 40–48 (2009).
Nagata, I., Abe, T., Nakata, Y. & Tamiya, N. Factors related to prolonged on-scene time during ambulance transportation for critical emergency patients in a big city in Japan: a population-based observational study. BMJ Open 6(1), e009599 (2016).
Loyd, J. W. & Swanson, D. Aeromedical Transport (StatPearls, Treasure Island (FL), 2020).
Li, L. S. Z., Yang, F. X. & Cui, C. High-speed rail and tourism in China: An urban agglomeration perspective. Int. J. Tour. Res. 21(1), 45–60 (2019).
Cao, W., Feng, X., Jia, J. & Zhang, H. Characterizing the structure of the railway network in China: a complex weighted network approach. J. Adv. Transp. 2019, 3928260 (2019).
Warren, J. et al. Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med 32(1), 256–262 (2004).
Powell-Dunford, N., McPherson, M. K., Pina, J. S. & Gaydos, S. J. Transferring aviation practices into clinical medicine for the promotion of high reliability. Aerosp. Med. Hum. Perform. 88(5), 487–491 (2017).
Davidson, L. A., Utarnachitt, R. B., Mason, A. & Sawyer, T. Development and testing of a neonatal intubation checklist for an air medical transport team. Air Med. J. 37(1), 41–45 (2018).
Stroud, M. H., Prodhan, P., Moss, M. M. & Anand, K. J. Redefining the golden hour in pediatric transport. Pediatr. Crit. Care Med. 9(4), 435–437 (2008).
Ajizian, S. J. & Nakagawa, T. A. Interfacility transport of the critically ill pediatric patient. Chest 132(4), 1361–1367 (2007).
Lowe, C. G. Pediatric and neonatal interfacility transport medicine after mass casualty incidents. J. Trauma 67(2 Suppl), S168–S171 (2009).
Bigham, M. T. More than a bus ride: quality and outcomes of paediatric specialty transport. Acta Paediatr. 105(11), 1335 (2016).
Greene, M. J. 2010 critical care transport workplace and salary survey. Air Med. J. 29(5), 222–235 (2010).
Giardino, A. P. et al. A longitudinal view of resident education in pediatric emergency interhospital transport. Pediatr. Emerg. Care 26(9), 653–658 (2010).
Long, B., Koyfman, A. & Vivirito, M. A. Capnography in the emergency department: a review of uses, waveforms, and limitations. J. Emerg. Med. 53(6), 829–842 (2017).
Wei, T., Shi, F. & Xu, G. Estimation of time-varying passenger demand for high speed rail system. Complexity 2019, 1568941 (2019).
Funding
This present study was supported by Capital’s Funds for Health Improvement and Research (2020–2-5093), Key logistics research projects of Chinese PLA (BLJ18J006).
Author information
Authors and Affiliations
Contributions
Professor X.H. and Professor Z.F. were responsible for the concept, design. Z.Z. and Y.L. were responsible for the data analysis, interpretation. Z.Z. and Y.L. were responsible for preparation and manuscript review. B.Y., H.Z., X.L. and Y.Z. contributed importantly to data acquisition, manuscript preparation and final approval.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhao, Z., Liu, Y., Yang, B. et al. The safety and efficacy of high-speed train transport for critical children: a retrospective propensity score matching cohort study. Sci Rep 11, 19293 (2021). https://doi.org/10.1038/s41598-021-98944-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98944-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.