Abstract
To investigate the associations between hemoglobin (Hb) concentration and hematocrit (Hct), and blood pressure (BP) in children and adolescents. The study population consisted of 7950 subjects total (4229 boys and 3721 girls) aged 10–18 years who participated in the Korea National Health and Nutrition Examination Surveys conducted between 2007 and 2017. The prevalence of hypertension was 19.19% (21.51% for boys and 16.5% for girls) among the study population, and the prevalence of obesity was 9.59% (10.5% for boys and 8.6% for girls). Hb count and Hct tended to increase with the degree of obesity and BP elevation. Systolic BP (SBP) and diastolic BP (DBP) positively correlated with Hb count and Hct in both sexes. Following multiple linear regression analysis, Hb count and Hct presented a positive association with SBP and DBP after adjusting for age, BMI SDS, alcohol consumption, smoking status, physical activity, rural residence, household income, diagnosis of T2DM, hypertension, and dyslipidemia. Hb count and Hct were positively associated with SBP and DBP in children and adolescents 10–18 years old.
Similar content being viewed by others
Introduction
Hypertension (HTN) is an important risk factor for cardiovascular disease1 and a large contributor to the global burden of disease2,3. HTN in childhood often leads to HTN in adulthood, as childhood BP predicts adult BP4,5,6,7. It is a growing health problem that is often overlooked8,9.
In children younger than 13 years old, elevated blood pressure (BP) is defined as BP in the 90th percentile or higher considering age, height, and sex, and HTN is defined as BP in the 95th percentile or higher10. In adolescents 13 years or older, elevated BP is defined as 120 to 129 mm Hg systolic BP and less than 80 mm Hg diastolic BP, and HTN is defined by a BP of 130/80 mm Hg or higher10. HTN in childhood may contribute to premature atherosclerosis and the early development of cardiovascular disease (CVD). Therefore, identifying the prevalence of HTN and determining its potential risk factors in children and adolescents would be useful for understanding its pathophysiology and improving its treatment and prevention. Obesity is known as a risk factor for childhood HTN11; in turn, childhood HTN is increasing alongside obesity prevalence as it reaches epidemic proportions worldwide. Chronic kidney disease and sleep disorders are also attributed to the development of HTN12,13. Family history of HTN or CVD, male sex, low birth weight, and maternal smoking during pregnancy are additional risk factors, whereas children who were breastfed have a reduced risk for HTN14,15. Also, the risk of HTN varies according to race and ethnicity; Hispanic and black children are known to have a greater risk16.
Abnormalities in blood viscosity have been implicated in a number of CVDs17,18. Hemoglobin (Hb) is the most important determinant of whole blood viscosity19, and high Hb levels could be a potential risk factor to increase BP. Several studies have reported that Hb concentrations are elevated in humans with HTN. However, only a limited number of large-population studies have shown an association between Hb concentration and BP20,21,22,23. Also, such population studies conducted in childhood are rare. Therefore, the current study investigated the prevalence of HTN and obesity and the associations between Hb count and hematocrit (Hct), and BP in children and adolescents using data from the 2007–2017 Korea National Health and Nutrition Examination Survey (KNHANES).
Results
A total of 7950 subjects were included in the final analysis. Among them, 4229 were boys (53.2%), and 3721 were girls. The subjects were categorized into three groups according to body mass index (BMI, kg/m2); 3343 of the boys were normal weight (NW, 79.0%), 443 were overweight (OW, 10.5%), and 443 were obese (OB, 10.5%), and 3059 of the girls were normal weight (82.2%), 342 were overweight (9.2%), and 320 were obese (8.6%).
Table 1 presents the clinical characteristics of the study population. The SDSs of height and waist circumference were significantly higher for boys than for girls. Systolic BP (SBP), diastolic BP (DBP), and serum glucose concentrations were higher for boys, and concentrations of TC, TG, HDL-C, and LDL-C were higher for girls. Alcohol consumption, smoking, and physical activity were more common in boys. None of the participants were previously diagnosed with HTN. However, this study has shown that 1526 adolescents did, in fact, have HTN (910 boys and 616 girls). The prevalence of HTN in childhood (10–18 years) was about 19.19% (21.5% for boys and 16.5% for girls). In the NW group, the prevalence of HTN was about 19.3% in boys and 15.2% in girls. In the OW group, the prevalence of HTN was about 26.1% in boys and 18.7% in girls. In the OB group, the prevalence of HTN was about 32.9% in boys and 26.8% in girls. Mean Hb count (g/dL) was 14.59 ± 1.13 in boys and 13.27 ± 0.94 in girls, and mean Hct (%) was 43.40 ± 3.33 in boys and 40.09 ± 2.56 in girls. Figure 1a reveals mean Hb count and Hct according to BMI group. Mean Hb and Hct increased significantly in boys between NW, OW, and OB groups. The mean Hb count (g/dL) was 14.57 ± 1.11 (NW), 14.61 ± 1.16 (OW), and 14.78 ± 0.01 (OB) in boys (p < 0.001), and the mean Hct (%) was 43.28 ± 3.31(NW), 43.58 ± 3.41(OW), and 44.09 ± 3.30 (OB) in boys (p < 0.001). The mean Hb count (g/dL) was 13.27 ± 0.95(NW), 13.30 ± 0.85(OW), and 13.31 ± 0.89 (OB) in girls (p = 0.587). Mean Hct (%) was 40.05 ± 2.58 (NW), 40.25 ± 2.44 (OW), and 40.34 ± 2.43 (OB) in girls (p = 0.079). Mean Hb count and Hct tended to increase among BMI groups, but there was no statistical significance in girls.
(a) Hemoglobin count and hematocrit according to BMI group in boys and girls. *p < 0.05,***p < 0.001. (b). Hemoglobin count and hematocrit according to hypertension status in boys and girls. ***p < 0.001. (c). Hemoglobin count according to BMI group, and hypertension status in boys and girls. *p < 0.05, **p < 0.005, ***p < 0.001, NS, p > 0.05. (d). Hematocrit according to BMI group, and hypertension status in boys and girls. *p < 0.05; **p < 0.005; ***p < 0.001; NS, p > 0.05.
Figure 1b reveals mean Hb count and Hct according to HTN status. The mean Hb count (g/dL) was significantly higher in subjects with HTN than in boys (14.90 ± 1.1 vs. 14.44 ± 1.0, p < 0.001) or girls (13.43 ± 0.93 vs. 13.21 ± 0.93, p < 0.001) with normal BP. Mean Hct (%) was also significantly higher in subjects with HTN than in boys (44.31 ± 3.28 vs. 42.95 ± 3.26, p < 0.001) or girls (40.55 ± 2.56 vs. 39.91 ± 2.53, p < 0.001) with normal BP.
Mean Hb count and Hct according to sex, BMI group, and presence of HTN are shown in Table 2 and Fig. 1c,d. In boys, when analyzed in all groups according to BMI group, Hb count and Hct were significantly higher in those with HTN than in those with normal BP (p < 0.001). In girls in the NW group, Hb count and Hct were significantly higher in those with HTN than in those with normal BP (p < 0.001). In girls in the OW group, Hb count was significantly higher in those with HTN (p < 0.05), but Hct was not (p = 0.083). In girls in the OB group, Hb count and Hct were high in those with HTN, but there was no statistically significant difference (p = 0.295 and p = 0.054, respectively).
Table 3 presents the correlation between Hb count and Hct, and BP in all subjects. Hb count and Hct were both positively correlated with SBP and DBP in boys and girls before and after adjusting for age.
Table 4 presents the multiple linear regression between Hb count and Hct, and BP in boys and girls. The mean SBP and DBP increased alongside Hb count and Hct in both sexes. Model 2 demonstrated that Hb count and Hct were significantly associated with BP after adjusting for age, BMI SDS, alcohol consumption, smoking status, physical activity, rural residence, household income, diagnoses of type 2 diabetes mellitus (T2DM), HTN, and dyslipidemia. In boys, SBP increased by 1.3 mm Hg with every 1 g/dL increase in Hb concentration. SBP in girls increased by 0.5 mm Hg with every 1 g/dL increase in Hb concentration. The DBP patterns were similar to the patterns observed with SBP. DBP increased by 1.1 mm Hg in boys and 0.8 mm Hg in girls with every 1 g/dL increase in Hb concentration. SBP increased by 0.5 mm Hg in boys and 0.3 mm Hg in girls with every 1% increase in Hct. DBP increased by 0.3 mm Hg with every 1% increase in Hct for both sexes.
Discussion
This study showed the prevalence of obesity and HTN and revealed the positive associations between Hb count and hematocrit level, and BP in children and adolescents. To our knowledge, this is the first study that investigated the associations between Hb count and Hct, and systolic and diastolic BP in a large sample of Korean children and adolescents aged 10–18 years. Our study population was representative of Korean children and adolescents because the KNHANES is an official nationwide database that reflects geographic and demographic differences throughout Korea.
Recently, the prevalence of above-healthy BMI has increased rapidly in children and adolescents24. Obesity is a multifactorial disease caused by genetic, biological, environmental, behavioral, and psychological factors25. Childhood obesity leads to adult obesity26,27 and an increased risk for cardiovascular disease and mortality in adulthood28. Moreover, severe obesity in children is positively associated with cardiometabolic risk factors, including low HDL cholesterol, high SBP and DBP, high TG, and high glycated Hb levels29.
The prevalence of above-healthy BMI was reported to be more than 10% in developing countries and even higher (20%) in developed countries30. Reports on the prevalence of childhood obesity in Korea vary, but it has also increased over time. In 2013, the prevalence of overweight BMI in children younger than 20 years old per 100,000 children was 21.2% in boys and 13.2% in girls, and the prevalence of obesity was 4.8% in boys and 3.1% in girls30. In our study considering data from those aged 10–18 years collected between 2007 and 2017, the overall prevalence of overweight BMI was 21% in boys and 17.8% in girls, and the prevalence of obesity was 10.5% in boys and 9.2% in girls. Our study did not analyze the annual prevalence of obesity and overweight BMI, and the difference in prevalence between our study and the previous report was likely caused by the age difference between subjects and the method of analysis.
The prevalence of elevated BP and HTN in children is reported to be around 6% and 3%, respectively9,31. In obese adolescents, the combined prevalence increases to around 30%31. Cho H et al. reported that the prevalence of HTN has increased over time from 6.9% (KNHANES 2007–2009) to 9.0% (KNHANES 2013–2015) in Korean children and adolescents 10–18 years old32. In the previous study, the prevalence of HTN was higher in boys than in girls and increased alongside the degree of obesity. Especially in the obesity group, the prevalence of HTN was higher than the sample average. In our study, the prevalence of HTN was also higher in boys than in girls and increased alongside the severity of obesity. However, our study design and methodology are different than previous studies, and the current study reported the prevalence of HTN to be 19.2% sample-wide (KNHANES 2007–2017) and 30.4% in the obesity group. In our study, we evaluated BP according to reference BP assessments in Korean children, different from the American Academy of Pediatrics (AAP) guidelines. According to the AAP guideline10, HTN criteria in children ≥ 13 years old is ≥ 130/80 mm Hg. However, in the present study, HTN was defined as SBP or DBP in or above the 95th percentile in children ≥ 13 years old or BP ≥ 130/80 mm Hg based on the Korean guidelines33, which are considered to be lower than the AAP guidelines. Therefore, the prevalence of HTN in our study seems to be higher than in previous reports.
The results of our study show that the prevalences of obesity and HTN were higher in boys than girls, and the prevalence of HTN was higher in the obese and overweight groups than in the normal-weight group in both sexes. Hb count and Hct tended to increase with the degree of obesity and BP elevation in both sexes, but there some differences between sexes. In boys and girls, Hb count and Hct higher in the HTN group than in those with normal BP. In boys alone, Hb count and Hct were significantly elevated in the OB group compared to that of the NW and OW groups. On the other hand, in girls, Hb count and Hct were no different according to obesity. As previously mentioned, obesity is a known risk factor of HTN11. In our study, HTN is positively associated with Hb count and Hct. Although there were gender-related differences, obesity might be related to increased Hb count and Hct. Further study should be performed to verify it.
Several studies have investigated the associations between Hb concentration and Hct, and BP; however, most of such investigations are performed in adults20,21,22,23. Previous studies have reported increased Hb concentrations in those with HTN and positive associations between SBP and DBP, and Hb count. The results of our study are in line with such findings20,21,22,23,34,35,36. Atsma et al. reported that Hb level was positively associated with both SBP and DBP in healthy Dutch voluntary blood donors 18–70 years of age21. They found 1.3 mm Hg and 1.8 mm Hg increases in SBP with every 1 mmol/L increase in Hb count for men and women, respectively, and DBP rose 1.4 mm Hg and 1.5 mm Hg with every 1 mmol/L increase in Hb count for men and in women, respectively. Lee et al. reported that SBP in men with Hb concentrations ≥ 13.0 g/dL and in women with Hb concentrations ≥ 11.0 g/dL increased by 2.6 mm Hg for every 1 mmol/L increase in Hb concentration, and DBP increased by 3.2 mm Hg for every 1 mmol/L increase in Hb concentration for both Korean men and women aged ≥ 20 years23. In our study, the regression coefficients were relatively lower than the previous study. SBP increased by 1.3 mm Hg in boys and 0.5 mm Hg in girls with every 1 g/dL increase in Hb level, and DBP increased by 1.1 mm Hg in boys and 0.8 mm Hg in girls with every 1 g/dL increase in Hb level. In our study, subjects were 10–18 years old, younger than in previous studies, and the units for Hb count were g/dL instead of mmol/L, so the regression coefficient seemed to be smaller in comparison. It is estimated that the difference in study design, ethnicity, and characteristics of the study population may have caused the difference in results.
Göbel et al. found significant correlations between mean arterial BP and red blood cell count, Hct, and Hb concentration in healthy subjects. They suggested that Hct plays a role in determining the viscosity of the blood and that it may be involved as a rheological factor controlling BP22. Our study did not collect red blood cell counts but indicated that Hct and Hb level were involved in BP determination, although the mechanisms for BP elevation alongside Hb count and Hct are not entirely known. Previous research has demonstrated Hct levels to be positively associated with HTN incidence37. Furthermore, increased Hct count is associated with increased blood viscosity, and increased viscosity is considered a determinant of vascular resistance, expected to contribute to BP38,39. The fact that polycythemia vera is often associated with cardiovascular disease supported this theory as plausible40. Moreover, Kawamoto reported that Hb count is strongly related to arterial stiffness, which, in turn, increases SBP and DBP41. Therefore, they suggested that slightly low Hb levels were beneficially associated with arterial stiffness in women. In addition, Cabrales et al. reported that Hb is a scavenger of nitric oxide (NO), produced in endothelial cells42. NO acts as a vasodilator and to prevent the development of atherosclerosis and its complications43. Increased levels of free Hb induce vasoconstriction due to NO scavenging and consequently impart BP elevation.
The current study has some limitations. First, since our study is cross-sectional, evaluation of causality was not possible. Second, while the prevalence of HTN was approximated using a population sample, this approximation may be flawed due to the sample’s likely imperfect representation of Korea’s demographics. The BP standard data for Korean children also differs from AAP guidelines. Therefore, the prevalence of HTN in our study may have been overestimated compared to if the AAP guidelines were used. Also, white coat HTN was not excluded in our study. Third, unweighted prevalence using conventional analysis can differ from weighted prevalence using survey analysis, as previous Korean studies have reported weighted prevalence that was not observed in the present study32. Nevertheless, both survey analysis for weighted prevalence and the conventional method for unweighted prevalence showed similar results for overall prevalence of hypertension (19.9% weighted prevalence for hypertension and 19.2% unweighted prevalence for hypertension) (Supplementary Table 1) and similar patterns of changes in prevalence for hypertension according to sex and year (Supplementary Figs. 1) in further analyses. Finally, the cause of the sexual-dependent relationships between Hb count and Hct, and BP were not fully elucidated. Periodic menstrual bleeding in girls might have influenced the difference in results. However, we had no data regarding pubertal status, diagnosis of anemia, or menstrual loss in the present study. Subsequent prospective studies are needed to clarify the mechanisms by which BP increases alongside Hb count and Hct and to determine the cause of the discrepancy between sexes.
In conclusion, Hb count and Hct were positively associated with SBP and DBP in Korean children and adolescents aged 10–18 years. Both Hb count and Hct contribute to BP, and their increase could be a potential risk factor for high BP. In particular, obesity could have a synergistic effect with Hct and Hb count to further elevate BP. It is important to identify and manage the risk factors for cardiovascular disease from childhood and adolescence. Establishing the CVD risk factors and their management would be the cornerstone of long-term healthcare that influences lifelong well-being. Further research is required to identify and verify the factors that increase BP in children of all ages, including newborns and other ethnic groups.
Material and methods
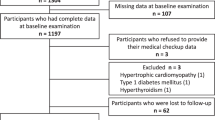
Data from the 2007–2017 KNHANES were analyzed in this study. The survey has been conducted by the Division of Chronic Disease Surveillance in the Korean Centers for Disease Control and Prevention on a 3-year cycle since 1998 to assess the health and nutritional status of the noninstitutionalized civilian population of Korea44. The KNHANES is a cross-sectional and nationally representative survey with a multistage and stratified probability sampling design. Data acquired from the full fourth (2007–2009), fifth (2010–2012), and sixth (2013–2015) cycles and the first year of the seventh cycle (2017) were combined to enhance the statistical power of this analysis.
A total of 89,630 individuals were included. Of these subjects, 7950 participants aged 10–18 years were included in the preliminary analysis. All subjects and their parents were interviewed at home after providing informed consent and underwent various examinations, including blood sampling45. Those with incomplete records regarding physical examination, including anthropometric measurements, BP, and laboratory tests, such as the lipid profile, were excluded. Those who had serum TGs ≥ 400 mg/dL were also excluded (n = 16). The database is available to the public at the KNHANES website (http://knhabes.cdc.go.kr). The study protocols of the 2007–2017 KNHANES survey were approved by the institutional review boards of the Korean Centers for Disease Control and Prevention. Informed consent was provided by all KNHANES subjects. All experiments were performed in accordance with relevant guidelines and regulations.
Anthropometric assessments, including height, weight, WC, SBP, and DBP, were performed by a trained expert. Height was measured to the nearest 0.1 cm using an electronic stadiometer (SECA, Germany). Weight was measured to the nearest 0.1 kg with an electronic scale (G-TECH, Korea). WC was measured to the nearest 0.1 cm using a calibrated measuring tape (SECA). SBP and DBP were measured 3 times to the nearest 1 mm Hg using a standard mercury sphygmomanometer. The SD scores (SDS) for height, weight, WC, and BMI were calculated using age- and sex-specific least mean square (LMS) parameters based on the 2017 growth reference values for Korean children and adolescents developed by the Korean Pediatric Society and the Korea Centers for Disease Control and Prevention46. The subjects were categorized into 3 groups according to BMI: normal weight (NW, BMI < 85th percentile), overweight (OW, BMI between the 85th percentile and the 95th percentile), and obese (OB, BMI ≥ 95th percentile). HTN was defined as sex-, age-, and height-specific SBP or DBP equal to or greater than the 95th percentile based on the Korean reference33, SBP ≥ 130 mmHg, or DBP ≥ 80 mmHg.
Lifestyle-related behaviors, such as alcohol consumption, smoking, household income, and residence, were assessed by means of a questionnaire. Information about alcohol consumption and smoking status (positive vs. negative current statuses) was collected with a self-administered questionnaire from subjects aged 12 years and older45. Physical activity was used to divide subjects into two groups (yes or no), and subjects were included in the ‘yes’ group if they performed intense physical activity ≥ 20 min/day ≥ 3 days/week, performed moderate physical activity ≥ 30 min/day ≥ 5 days/week, or if they walked ≥ 30 min/day ≥ 5 days/week.
Questionnaires on household income and area of residence (urban vs. rural) were administered by trained interviewers. Diagnoses of HTN, diabetes, and dyslipidemia were also included in the questionnaire.
Statistical analyses
R, version 3.5.1 (The R Foundation for Statistical Computing, Austria), was used for statistical analysis. Continuous variables are expressed as mean ± SD. Categorical variables are presented as number and percentage. A two-tailed t-test was performed to identify differences in clinical parameters between boys and girls, whereas categorical variables were compared using the χ2 test. To determine statistical significance, we used analysis of variance (ANOVA) for Hb count and Hct according to BMI groups. The Pearson’s correlation coefficient analysis was performed to evaluate the correlations between Hb count and Hct, and BP. Multiple linear regression was performed to investigate the relationships between Hb count and Hct, and BP. Probability values less than 0.05 were considered statistically significant.
References
Kannel, W. B., Dawber, T. R., Kagan, A., Revotskie, N. & Stokes, J. III. Factors of risk in the development of coronary heart disease–six year follow-up experience. The Framingham study. Ann. Internal Med. 55, 33–50 (1961).
Ezzati, M., Lopez, A. D., Rodgers, A., Vander Hoorn, S. & Murray, C. J. Selected major risk factors and global and regional burden of disease. Lancet (Lond., Engl.). 360(9343), 1347–1360 (2002).
Lawes, C. M., Vander Hoorn, S. & Rodgers, A. Global burden of blood-pressure-related disease, 2001. Lancet (Lond., Engl.). 371(9623), 1513–1518 (2008).
Lauer, R. M. & Clarke, W. R. Childhood risk factors for high adult blood pressure: the Muscatine study. Pediatrics 84(4), 633–641 (1989).
Sun, S. S. et al. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics 119(2), 237–246 (2007).
Chen, X. & Wang, Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 117(25), 3171–3180 (2008).
Falkner, B., Gidding, S. S., Portman, R. & Rosner, B. Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics 122(2), 238–242 (2008).
Riley, M., Hernandez, A. K. & Kuznia, A. L. High blood pressure in children and adolescents. Am. Fam. Physician 98(8), 486–494 (2018).
Hansen, M. L., Gunn, P. W. & Kaelber, D. C. Underdiagnosis of hypertension in children and adolescents. JAMA 298(8), 874–879 (2007).
Flynn, J. T., Kaelber, D. C., Baker-Smith, C. M., Blowey, D., Carroll, A. E. & Daniels, S. R, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140(3).
Falkner, B. et al. The relationship of body mass index and blood pressure in primary care pediatric patients. J. Pediatr. 148(2), 195–200 (2006).
Archbold, K. H., Vasquez, M. M., Goodwin, J. L. & Quan, S. F. Effects of sleep patterns and obesity on increases in blood pressure in a 5-year period: report from the Tucson Children’s assessment of sleep Apnea Study. J. Pediatr. 161(1), 26–30 (2012).
Flynn, J. T. et al. Blood pressure in children with chronic kidney disease: a report from the Chronic kidney disease in children study. Hypertension (Dallas, TX, 1979). 52(4), 631–637 (2008).
Lawlor, D. A. et al. Associations of parental, birth, and early life characteristics with systolic blood pressure at 5 years of age: findings from the Mater-University study of pregnancy and its outcomes. Circulation 110(16), 2417–2423 (2004).
Martin, R. M., Ness, A. R., Gunnell, D., Emmett, P. & Davey, S. G. Does breast-feeding in infancy lower blood pressure in childhood? The Avon Longitudinal Study of Parents and Children (ALSPAC). Circulation 109(10), 1259–1266 (2004).
Brady, T. M., Fivush, B., Parekh, R. S. & Flynn, J. T. Racial differences among children with primary hypertension. Pediatrics 126(5), 931–937 (2010).
Wells, R. Syndromes of hyperviscosity. N. Engl. J. Med. 283(4), 183–186 (1970).
Aleman, M. N. et al. Hemostatic state of children with type 1 diabetes. Ann. Pediatr. Endocrinol. Metab. 26(2), 99–104 (2021).
de Simone, G. et al. Relation of blood viscosity to demographic and physiologic variables and to cardiovascular risk factors in apparently normal adults. Circulation 81(1), 107–117 (1990).
Shimizu, Y. et al. Association between the hemoglobin levels and hypertension in relation to the BMI status in a rural Japanese population: the Nagasaki Islands Study. Internal Med. (Tokyo, Jpn.). 53(5), 435–440 (2014).
Atsma, F. et al. Hemoglobin level is positively associated with blood pressure in a large cohort of healthy individuals. Hypertension (Dallas, TX, 1979). 60(4), 936–941 (2012).
Göbel, B. O. et al. Arterial blood pressure. Correlation with erythrocyte count, hematocrit, and hemoglobin concentration. Am. J. Hypertens. 4(11), 14–19 (1991).
Lee, S. G., Rim, J. H. & Kim, J. H. Association of hemoglobin levels with blood pressure and hypertension in a large population-based study: the Korea National Health and Nutrition Examination Surveys 2008–2011. Clin. Chim. Acta Int. J. Clin. Chem. 438, 12–18 (2015).
Kim, J. & Lee, J. Role of obesity-induced inflammation in the development of insulin resistance and type 2 diabetes: history of the research and remaining questions. Ann. Pediatr. Endocrinol. Metab. 26(1), 1–13 (2021).
Lee, E. Y. & Yoon, K. H. Epidemic obesity in children and adolescents: risk factors and prevention. Front. Med. 12(6), 658–666 (2018).
Ogden, C. L., Carroll, M. D., Kit, B. K. & Flegal, K. M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 311(8), 806–814 (2014).
Venn, A. J. et al. Overweight and obesity from childhood to adulthood: a follow-up of participants in the 1985 Australian Schools Health and Fitness Survey. Med. J. Aust. 186(9), 458–460 (2007).
Twig, G. et al. Body-Mass index in 23 million adolescents and cardiovascular death in adulthood. New Engl. J. Med. 374(25), 2430–2440 (2016).
Skinner, A. C., Perrin, E. M., Moss, L. A. & Skelton, J. A. Cardiometabolic risks and severity of obesity in children and young adults. N. Engl. J. Med. 373(14), 1307–1317 (2015).
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (Lond., Engl.). 384(9945), 766–781 (2014).
McNiece, K. L. et al. Prevalence of hypertension and pre-hypertension among adolescents. J. Pediatrics. 150(6), 640–644 (2007).
Cho, H. & Kim, J. H. Secular trends in hypertension and elevated blood pressure among Korean children and adolescents in the Korea National Health and Nutrition Examination Survey 2007–2015. J. Clin. Hypertens. (Greenwich) 22(4), 590–597 (2020).
Lee, C. G. et al. Normative blood pressure references for Korean children and adolescents. Korean J. Pediatr. 51(1), 33–41 (2008).
Yan, X., Zheng, S., Ji, J., Zuo, J. & Qian, Y. A18078 the hemoglobin was associated with blood pressure in the Chinese community-dwelling cohort. J Hypertens 36, e345 (2018).
Jamshidi-Naeini, Y., Bavil, A. K., Egal, A. & Oldewage-Theron, W. Hemoglobin and ferritin concentrations are positively associated with blood pressure and hypertension risk in older adults: a retrospective cross-sectional study, Sharpeville, South Africa. Asia Pac. J. Clin. Nutr. 28(3), 533–543 (2019).
Chen, X. T. et al. Exploring the relationship of peripheral total bilirubin, red blood cell, and hemoglobin with blood pressure during childhood and adolescence. Jornal de Pediatria. 94(5), 532–538 (2018).
Jae, S. Y. et al. Higher blood hematocrit predicts hypertension in men. J. Hypertens. 32(2), 245–250 (2014).
Taco-Vasquez, E. D. et al. Association between blood viscosity and cardiovascular risk factors in patients with arterial hypertension in a high altitude setting. Cureus. 11(1), e3925 (2019).
Lowe, G. D., Lee, A. J., Rumley, A., Price, J. F. & Fowkes, F. G. Blood viscosity and risk of cardiovascular events: the Edinburgh Artery Study. Br. J. Haematol. 96(1), 168–173 (1997).
Nand, S. & Orfei, E. Pulmonary hypertension in polycythemia vera. Am. J. Hematol. 47(3), 242–244 (1994).
Kawamoto, R. et al. A slightly low hemoglobin level is beneficially associated with arterial stiffness in Japanese community-dwelling women. Clin. Exp. Hypertens. (New York, NY). 34(2), 92–98 (2012).
Cabrales, P., Han, G., Nacharaju, P., Friedman, A. J. & Friedman, J. M. Reversal of hemoglobin-induced vasoconstriction with sustained release of nitric oxide. Am. J. Physiol. Heart Circ. Physiol. 300(1), H49-56 (2011).
Bian, K., Doursout, M. F. & Murad, F. Vascular system: role of nitric oxide in cardiovascular diseases. J. Clin. Hypertens. (Greenwich) 10(4), 304–310 (2008).
Kweon, S. et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 43(1), 69–77 (2014).
Park, H. K. & Shim, Y. S. Distribution of tri-ponderal mass index and its relation to body mass index in children and adolescents aged 10 to 20 Years. J. Clin. Endocrinol. Metab. 105(3), e826–e834 (2020).
Kim, J. H. et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 61(5), 135–149 (2018).
Acknowledgements
This work was supported by the Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Contributions
Dr. H.R.J. drafted the initial manuscript and reviewed and revised the manuscript. Dr. H.S.L. designed the data collection instruments and reviewed and revised the manuscript. Dr. Y.S.S. prepared the original protocol and overall design of the study, collected the data, conducted data management and statistical analyses, and revised the manuscript. Prof. J.S.W. conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jeong, H.R., Shim, Y.S., Lee, H.S. et al. Hemoglobin and hematocrit levels are positively associated with blood pressure in children and adolescents 10 to 18 years old. Sci Rep 11, 19052 (2021). https://doi.org/10.1038/s41598-021-98472-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98472-0
This article is cited by
-
White blood cell and platelet distribution widths are associated with hypertension: data mining approaches
Hypertension Research (2024)
-
The associations between hematological parameters and the incidence of prehypertension and hypertension in children and adolescents: a prospective cohort study
Hypertension Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.