Abstract
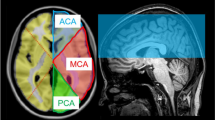
Adaptive recovery of cerebral perfusion after pediatric arterial ischemic stroke (AIS) is sought to be crucial for sustainable rehabilitation of cognitive functions. We therefore examined cerebral blood flow (CBF) in the chronic stage after stroke and its association with cognitive outcome in patients after pediatric AIS. This cross-sectional study investigated CBF and cognitive functions in 14 patients (age 13.5 ± 4.4 years) after pediatric AIS in the middle cerebral artery (time since AIS was at least 2 years prior to assessment) when compared with 36 healthy controls (aged 13.8 ± 4.3 years). Cognitive functions were assessed with neuropsychological tests, CBF was measured with arterial spin labeled imaging in the anterior, middle, and posterior cerebral artery (ACA, MCA, PCA). Patients had significantly lower IQ scores and poorer cognitive functions compared to healthy controls (p < 0.026) but mean performance was within the normal range in all cognitive domains. Arterial spin labeled imaging revealed significantly lower CBF in the ipsilesional MCA and PCA in patients compared to healthy controls. Further, we found significantly higher interhemispheric perfusion imbalance in the MCA in patients compared to controls. Higher interhemispheric perfusion imbalance in the MCA was significantly associated with lower working memory performance. Our findings revealed that even years after a pediatric stroke in the MCA, reduced ipsilesional cerebral blood flow occurs in the MCA and PCA and that interhemispheric imbalance is associated with cognitive performance. Thus, our data suggest that cerebral hypoperfusion might underlie some of the variability observed in long-term outcome after pediatric stroke.
Similar content being viewed by others
Introduction
Arterial ischemic stroke (AIS) in children is a rare but devastating condition. The incidence of childhood stroke ranges from 1.3–13 per 100,000 children per year1, and boys are twice as likely to be affected as girls2. The etiology, presentation, and prognosis of stroke in children differ from those in adults3 and, although specific risk factors have been identified, the etiology of pediatric stroke often remains unclear4. Survivors of childhood stroke suffer from motor5 and cognitive restrictions6,7,8,9. While general intelligence is often within the average range7,9,10,11, deficits in specific cognitive subdomains can lead to learning difficulties and behavioral abnormalities12.
The severity of cognitive deficits are thought to vary according to lesion-related characteristics, such as size and location, as well as alterations in functional networks and cerebral blood flow. Therefore, it is important to study cerebral, post-ischemic changes in detail. A modern approach to investigate cerebral blood flow is by means of arterial spin labeling (ASL). This is a non-invasive, non-ionizing magnetic resonance imaging (MRI) technique using arterial blood as an endogenous tracer. ASL provides a safe, economical, and quantifiable measure of cerebral blood flow reflecting the level of glucose metabolism associated with neuronal activity13. AIS is associated with an acute local reduction of cerebral blood flow14. In adults under normal conditions, a cerebral blood flow of 50–80 ml/100 g/min ensures a sufficient energy supply to the brain15, however, a short-term reduction to < 20 ml/100 g/min leads to reversible nerve cell damage and a reduction to < 15 ml/100 g/min leads to necrosis of the brain parenchyma within a few minutes16. As cerebral blood flow mirrors the brain’s metabolic demands and neuronal activity, its measurement provides important information on brain activity and functional recovery17.
Both, hyper- and hypoperfusion of cerebral blood flow have been found after AIS in the acute and sub-acute phase17,18,19,20. Large lesions and more severe intracranial arteriopathy have been associated with hypoperfusion, whereas smaller lesions have been associated with reperfusion or hyperperfusion17,18. Hyperperfusion is thought to be due to neuronal hyperexcitability following the insult or due to stroke-associated seizures. Hypoperfusion has previously been suggested to resolve over time in accordance with early behavioral recovery patterns21,22,23. However, case studies of patients in the chronic phase after stroke report hypoperfusion in the lesioned hemisphere22,24,25 and relate it to functional deficits, i.e. language problems22, reading deficits24,26, and phonological competence26.
In the chronic stage after stroke, reductions of ipsilesional cerebral blood flow was correlated with infarct size in patients after left-hemisphere stroke, indicating sustained hypoperfusion in the affected hemisphere20. Compared to acute stroke27, the understanding of cerebral perfusion in the chronic stage after stroke is far less clear20,24,25,28 and was barely described in children and adolescence so far17,20,25.
Besides measuring cerebral blood flow after AIS, it is crucial to study the interhemispheric imbalance between ipsilesional and contralesional perfusion. A longitudinal study with adults in the subacute phase after AIS showed that sustained hemispheric perfusion imbalance is associated with poor motor function, suggesting that the interhemispheric balance may be critical for motor recovery after AIS29. In line with this finding, we observed in a previous study that patients with hemiparesis after pediatric AIS present with sustained interhemispheric perfusion imbalance, which was related to poorer manual ability30. So far, however, the relationship between cerebral blood flow and cognitive outcome has rarely been studied.
Depending on the region of interest, positive as well as negative correlations occurred between cerebral blood flow and cognitive functions such as i.e. intelligence quotient (IQ) in 39 healthy children aged 7–17 years31. A longitudinal study in a healthy cohort of older adults showed that cerebral blood flow can predict both, general cognitive ability as well as specific cognitive functions, with higher blood flow enabling better cognitive functions32.
There is no clear relationship between cerebral blood flow and cognitive functions in patients33. A study using SPECT in 21 pediatric patients with moyamoya disease (aged 5–14 years) showed a significant positive association between regional cerebral blood flow and intelligence, perceptual reasoning and processing speed34. Contrary, a negative correlation between cerebral blood flow (measured with ASL) and IQ has been found in 24 children with sickle cell anemia (aged 6–12 years33). In line with the negative correlation between cerebral blood flow and cognition are the results of a study on 26 children with hypoxic-ischemic encephalopathy. Neonatal cerebral blood flow assessed using PET correlated negatively with IQ measured in childhood35.
Results of the different clinical studies may not be comparable due to differences in perfusion assessments, cognitive assessment, age at assessment and underlying disease. Cerebral blood flow in the chronic phase after pediatric AIS has never been investigated so far and the relationship between interhemispheric perfusion balance and cognitive outcome has not yet been studied, neither in healthy subjects nor in patients following AIS.
Therefore, the aim of the present study was to investigate cerebral perfusion in patients in the chronic stage after pediatric arterial ischemic stroke in the MCA compared to healthy controls. Further, we aimed to investigate the relationship between interhemispheric perfusion balance and long-term cognitive outcome in children after AIS. In accordance with the existing literature, we hypothesized that (1) children after AIS in the MCA have lower cerebral blood flow in the ipsilesional hemisphere compared to healthy controls even years after stroke and (2) sustained interhemispheric cerebral blood flow imbalance is associated with lower cognitive outcome such as previously described for motor outcome29,30. Disentangling the relationship between cerebral blood flow and cognitive functions after AIS will indicate whether cerebral blood flow can be used as a proxy for rehabilitation capacity.
Methods
We report on data from the HERO Study36 examining functional reorganization after childhood stroke with a cross-sectional as well as a longitudinal approach. The HERO Study was approved by the local ethics committee of the Canton of Berne (KEK 212/13) and the ethics committee of the Children’s University Hospital and was performed in accordance with the declaration of Helsinki. All participants, or their parent or legal guardian if they were younger than 18 years, gave written informed consent prior to enrollment. Participants were compensated for their participation (with a movie voucher or book voucher).
Participants
Patients were identified by the Swiss Neuropediatric Stroke Registry (SNPSR)—a multicenter, prospective, and population-based registry that includes children diagnosed with AIS under the age of 16 years5. Patients were included if AIS had occurred at least 2 years prior to the assessment. Exclusion criteria were active epilepsy, iron implants, claustrophobia and behavioral problems that make an MRI scan impossible.
Of the twenty nine patients recruited for the HERO Study, 14 had an arterial ischemic stroke in the MCA territory after exclusion of patients due to developmental delay or behavioral problems that interfered with compliance (n = 2), bilateral lesions (n = 4), retainer artifacts (n = 1), error in T1-weighted anatomical image or ASL sequences (n = 2) or neonatal stroke (n = 3). Healthy controls met the following inclusion criteria: absence of neurological disease or psychiatric disorders, no deficit in general intellectual functioning as measured with IQ (IQ > 85), and no contraindications for MRI (metal braces, metallic implants). Of the forty four healthy controls eight had to be excluded because of incorrect relaxation time in ASL sequence (n = 2), retainer artifacts (n = 2), missing age norms for the youngest children (< 7 years, n = 4). Detailed clinical characteristics of the study participants are provided in Supplementary Table S1.
Cognitive outcome
All tests were conducted by a trained neuropsychologist. To obtain a reliable and valid assessment of different cognitive domains, an extended and standardized test battery was adopted. Details on the tests have been previously published (HERO Study36). Raw scores for all tests were transformed into age-dependent standard scores (M = 100, SD = 15) according to the relevant test manual. Test scores measuring the same cognitive domain were z-transformed and the means from the tasks were calculated to obtain the domain-specific index. IQ was measured using the Test of Nonverbal Intelligence (TONI-4)37, which is a language-free test assessing fluid intelligence in children and adults.
Executive functions
Verbal working memory was assessed using the subtests Letter-Number-Sequencing of the Wechsler Intelligence Scale for Children (WISC-IV)38 or the Wechsler Intelligence Scale for Adults (WAIS-IV)39 depending on the age of the participant. Visuo-spatial working memory was assessed using the spatial positioning subtest of the Learning and Memory Test (basic-MLT). Inhibition was measured using the Go/NoGo task of the Test of Attentional Performance (TAP)40 and the Color Word Interference Test (CWI) 3rd condition of the Delis-Kaplan Executive Function System™ (D-KEFS™41. For the assessment of shifting, the Trail-Making-Test and the 4th condition and the CWI of the D-KEFS™41 were used.
Processing speed
Processing speed was measured with the subtests Symbol Search and Digit Symbol-Coding of the WISC-IV38 or the WAIS-IV39 depending on the age of the participant.
Attention
Selective attention was evaluated with the cancellation task of the WISC-IV38 or the WAIS-IV39. The Divided Attention task of the TAP40 was also used.
Memory
Verbal learning was assessed with a standardized multitrial learning task consisting of five repeated auditory presentations of a 15-word list that had to be recalled by the participant immediately after each presentation (VLMT)42. Visual learning was measured with the Rey Visual Design Learning Test (RVDLT). This test consists of 15 cards displaying simple geometric forms that are presented to the child one by one, with an interval of 2 s per card. After all test items have been shown, the child is asked to draw as many of the items as she or he can recall. This procedure is repeated another four times (learning and recall phase).
Visuo-spatial abilities
Visuo-spatial abilities were measured with the Beery-Buktenica Developmental Test of Visual-Motor Integration (VMI), which is a standardized copy forms-type test used to assess visual-motor integration. The three subtests: (visual-motor integration subtest, test of visual perception, and test of motor coordination were individually administered in that order to each participant as described in the VMI Administration, Scoring, and Teaching Manual (4th edition). Each perceptual test was scored according to the published instructions43.
Overall cognitive outcome
The overall cognitive outcome score was calculated as the mean of all domain-specific index scores. All cognitive domain scores were z-transformed and summarized.
Neuroimaging
Structural imaging
High-resolution anatomical T1-weighted images were acquired on a 3 T Magnetom Verio Siemens scanner (Siemens, Erlangen, Germany) using a magnetization-prepared rapid acquisition gradient-echo (MP-RAGE) sequence (repetition time = 2530 ms; echo time = 2.92 ms; inversion time = 1100 ms; 160 sagittal slices; flip angle = 9°; field of view = 256 mm × 256 mm; matrix dimension = 256 × 256; isotropic voxel resolution = 1 mm3). The scan duration was 5 min 05 s.
Lesion-related characteristics were determined by a board-certified neuroradiologist. Ischemic lesions were manually traced to calculate the volume of affected brain tissue. Lesion size was defined as the affected brain tissue in relation to the total brain volume (ratio). Total intracranial volume (gray matter (GM), white matter and cerebrospinal fluid (CSF)) was calculated using the MATLAB-based toolbox SPM (SPM12, Wellcome Department of Imaging Neuroscience, London, England). Lesion laterality was classified depending on the affected hemisphere (i.e. left, right, or bilateral) and lesion location was divided into three categories (cortical, subcortical, combined cortical and subcortical, according to Everts et al. 2008). All lesions were flipped to the left hemisphere, so that the left hemisphere was always the ipsilesional hemisphere. Hence, in controls, the left hemisphere was compared to the ipsilesional hemisphere in patients.
Arterial spin labeling
To assess cerebral blood flow, we adopted a pseudo-continuous arterial spin labeling (pCASL) sequence44,45. Specifically, an alternating sequence of label and control images was acquired and labeling was performed at 80 mm below the isocenter of the imaging region. A post-labeling delay (PLD) of 1.25 s was set with a label time of 1.6 s. A total of 16 slices with a slice thickness of 6 mm were recorded sequentially from inferior to superior. Each pCASL measurement was repeated 120 times. Images were acquired using the following parameters: TE = 12 ms; TR = 3400 ms; field of view, 230 mm2; matrix size, 64 × 64; flip angle 90°; voxel size, 3.6 × 3.6 × 6.0 mm. Additionally, one M0 image for tissue at equilibrium magnetization was recorded with TR = 8000 ms and PLD = 5000 ms. All other parameters were unchanged. The duration of the ASL scan was 6 min 58 s.
SPM12 and MATLAB (MathWorks Inc.; version R2017a) was used for all processing steps. ASL time series were realigned to correct for motion artifacts and anatomical T1 images were segmented into GM, white matter, and CSF. The estimation of cerebral blood flow can be performed with the ASL technique. In fact, a calibrated cerebral blood flow measure can be obtained using a one-compartment model46,47 solving the following equation:
The variables are as follows: post-labeling delay (ω) (PLD), labeling duration (τ), blood/tissue water partition coefficient λ = 0.9 g/mL, and labeling efficiency α = 0.8521. In the human brain, and for 3.0 T, a decay time for labeled blood T1b = 1650 ms is assumed. Moreover, M0 are the equilibrium brain tissue magnetization images13,46,48 and were acquired in separate runs. ΔΜ represents the time series obtained by subtraction of control and label images. The ASL images used for cerebral blood flow quantification were all recorded and processed according the “ASL white paper”49. All MRI modalities were processed so that a normalized standard space (Montreal Neurological Institute coordinate system, MNI) was available to ensure the extraction of cerebral blood flow values for homologous brain regions. Each cerebral blood flow map was then masked with the segmented GM anatomical images. We used a threshold of 0.7 for the creation of each GM mask, which was then applied to each cerebral blood flow map.
To ensure that cerebral blood flow was only measured in anatomically intact tissue, we superimposed the lesion masks generated from the T1-weighted anatomical images on the cerebral blood flow map. The resulting mean cerebral blood flow maps were then co-registered to the anatomical scans, normalized to the MNI and spatially smoothed with a Gaussian kernel (8 mm, full-width at half-maximum). Cerebral blood flow was measured throughout the brain and separately in each of the hemispheres in the territories of the anterior (ACA), middle (MCA) and posterior cerebral artery (PCA).
Cerebral blood flow balance was assessed by calculating cerebral blood flow difference scores between the ipsilesional and contralesional cerebral blood flow of the ACA, MCA and PCA.
To control for subject motion, deviations from the initial position were assessed during the ASL scan. Deviations were measured along the x-, y- and z-axes in mm (x, y, z) and in radians (α, β, γ).
Statistical analysis
All analyses were performed using the statistical software package R 3.6.0 (Core Team, 2019). Variables were tested for normality with the Shapiro–Wilk test. Mean values between two groups were compared using one-sided (for cognition) or two-sided (for cerebral blood flow) independent samples t tests (normally distributed variables) or Mann–Whitney U tests. For correlation analyses, Pearson (normally distributed variables) or Spearman correlations (non-normally distributed variables) were applied. To investigate the relationship between cerebral blood flow and cognition, we applied partial correlations (Spearman), with lesion size as covariates. To account for the effects of multiple hypothesis testing (type I error), false discovery rate (FDR) correction was employed for all analysis. Results of P < 0.05 FDR-corrected were considered significant.
Results
Demographics
Patients and healthy controls were comparable in terms of sex (χ2 = 0.828, p = 0.363) and age at examination (t = 2.226, p = 0.822). Mean age at stroke was 6.2 years (SD = 3.8, range = 1.17–14.33), mean time since stroke was 7.2 years (SD = 3.9, range = 2.1–15.5). Mean lesion size corrected for intracranial volume was 1.8 mm3 (SD = 3.1, range = 0.003–11.7 mm3). Of the AIS group, 78.6% (n = 11) had a lesion in the left and 21.4% (n = 3) in the right hemisphere. A subcortical lesion was seen in 71.4% (n = 10) of the patients and 28.6% (n = 4) had a combined lesion (subcortical and cortical). No patient had an exclusively cortical lesion. Detailed clinical characteristics of the study participants are provided in Supplementary Table S1.
Cognitive outcome
Patients mean cognitive performance was within the normal range in all cognitive domains. However, when compared to healthy controls, patients had significantly reduced overall cognitive functions (U(2) = 76.0, p = 0.001). In particular, IQ (U(2) = 115, p = 0.003), memory (verbal and visual learning) (U(2) = 112.0, p = 0.003), working memory (U(2) = 118, p = 0.005), cognitive flexibility (U(2) = 159.5, p = 0.026), attention (U(2) = 151.5, p = 0.019), processing speed (U(2) = 133.5, p = 0.007), and visuo-spatial abilities (U(2) = 134, p = 0.007) differed significantly between the AIS group and healthy controls (Table 1). There was no significant between group difference for inhibition, even though the AIS group displayed worse mean performance in this domain than controls. On a descriptive level, patients with combined lesions (n = 4) showed worse median cognitive performance across all cognitive domains when compared to patients with subcortical lesions only (n = 10, see Fig. S1).
Lesion size correlated negatively with cognitive variables (Table 2), indicating that patients with larger stroke volume performed worse in almost all cognitive domains (r = − 0.470 to r = − 0.756). No significant association was found between cognitive variables and time since stroke and age at stroke (p > 0.05).
Cerebral blood flow
To ensure that differences in cerebral blood flow were not related to motion during MR scanning, motion parameters were compared between patients and healthy controls. No significant differences were found between patients and controls. Detailed results with z and p values are provided in Supplementary Table S2.
In all vessel territories median cerebral blood flow of patients was lower than in controls (Table 3) with significant cerebral blood flow differences ocurring in the ipsilesional MCA and PCA (MCA U(2) = 121, p = 0.004; PCA (U(2) = 147, p = 0.011). Descriptively, median cerebral blood flow was slightly lower in patients with subcortical lesions (n = 10) when compared to patients with combined lesions (n = 4) in all vessel territories (see Fig. S2).
As hypothesized, cerebral blood flow imbalance in the MCA (calculated as difference score between the ipsilesional and contralesional cerebral blood flow) was significantly higher in patients than controls (Table 3; Fig. 1). Whereas median cerebral blood flow imbalance was higher in patients across all vessel territories, there were no significant group differences for cerebral blood flow imbalance in the ACA and PCA.
Association between cerebral blood flow imbalance, lesion size and cognitive outcome
First, we analyzed the association between cerebral blood flow imbalance and lesion related variables and cognitive outcome (Table 4). Analyses revealed no significant associations between cerebral blood flow imbalance and age at stroke nor with time since stroke (p < 0.05). However, lesion size correlated positively with cerebral blood flow imbalance in the MCA (r = 0.695, p = 0.036). Patients with combined lesions (larger lesions, n = 4) showed higher median cerebral blood flow imbalance than patients with subcortical lesions (smaller lesions, n = 10) when looking at the data descriptively (see Fig. S3).
In patients, partial correlations (with lesion size as covariate) revealed significant negative relationships between interhemispheric cerebral blood flow imbalance in the MCA and working memory (r = − 0.787, p = 0.005).
Discussion
This cross-sectional study adopted arterial spin labeled perfusion imaging to investigate cerebral blood flow after pediatric AIS in the MCA and its relation to long-term cognitive outcome in the chronic phase years after stroke. The performance of patients was significantly worse than that of controls in several cognitive domains providing further support for cognitive deficits after pediatric AIS such as presented in previous studies8,10,12. We found significantly lower cerebral blood flow in the ipsilesional MCA and PCA in patients than in controls. Imbalance of cerebral blood flow in the MCA did significantly differ between groups. According to our second hypothesis, we found that sustained hemispheric imbalance of cerebral blood flow was negatively associated with working memory.
Our finding of reduced mean ipsilesional cerebral blood flow after pediatric AIS across all vessel territories (reaching significance for the MCA and PCA) is in line with findings from studies of adult patients with chronic stroke20 or in the subacute phase after stroke29, indicating sustained hypoperfusion in the affected hemisphere20. The reduction of cerebral blood flow in ipsi- and to some degree also in contralesional vessel territories, even several years post-stroke, suggests that cerebral blood flow perfusion has not fully recovered. This finding is in line with studies showing that adult patients after stroke show decreased cerebral blood flow due to impaired autoregulation in the long term49,50,52. Our data follows up on a case study24 suggesting that even in structurally intact brain areas, cerebral perfusion is altered in the long-term. A stroke causes hypoperfusion to the stroke core where neurons are likely to die53. Hypoperfusion additionally occurs in peri-infarct tissue where neurons may remain alive if blood flow is restored within two days after stroke54. However, hypoperfusion in the peri-infarct area can remain for weeks after stroke22. In line with the results of the present study, the effects of stroke can also affect remote functional networks26, likely due to diaschisis (electrical, metabolic, or blood flow dysfunction in functionally connected areas remote from the lesion55) or due to other signals leading to a widespread disconnection of brain networks54. In adult patients after stroke, hypoperfusion of anatomically intact areas can be seen up to a year after stroke56. Hence, functional brain recovery is suggested to crucially depend on what happens in the peri-infarct areas and in larger functional neural network57.
Our results are supposedly contrasting previous findings on the association between cerebral blood flow and lesion size17. On a descriptive level, our data shows higher cerebral blood flow in patients with combined lesions (larger lesions n = 4, mean age at assessment 15.3 years) than patients with subcortical lesions only (smaller lesions, n = 10, mean age at assessment 12.7 years). In a previous study, hyperperfusion occurred more likely in children with smaller stroke volume whereas hypoperfusion related to larger lesions in the acute and subacute phase after stroke17. This opposing finding is likely explained by differences in respect to the age at assessment (17: 9.2 years) and the time-point of the follow-up assessment (17: average of 6 months after stroke; our patients: average of 8.4 years for patients with combined lesions and 6.7 years after stroke for patients with subcortical lesions; see Table S1). Cerebral blood flow characteristics are known to change with age31 and during recovery22,56 which hinders a comparison of studies with different patient characteristics.
Further, the literature shows that cerebral blood flow imbalance is more accentuated in children with severe arteriopathy when compared to mild arteriopathy18, a finding which is consistent with the results of the present study, where larger lesions related to higher imbalance. In adults with arterial disease, the extent of white matter lesion modified the association between cerebral blood flow and executive functions; the association between lower cerebral blood flow and worse executive functions became stronger with increasing volumes of white matter lesion50. Consequently, patients with large lesions may suffer from a “double-hazard” phenomenon: larger lesions correlated with lower cerebral blood flow in the affected hemisphere and both aspects are likely affecting cognitive outcome negatively.
Decreased cerebral blood flow is thought to be associated with reduced functional and structural reorganization capacities, which in turn might lead to slower cognitive recovery. During childhood, brain development undergoes shifts in functional connectivity58,59, hemodynamic properties60, cortical surface expansion61, increases in white matter volume62 and decrease in synapse density due to pruning63. Cerebral blood flow plays an important role during these changes, as it supplies blood and nutrients to the brain, supports ongoing development and likely reflects decreased synaptic density63,64.
Cerebral blood flow imbalance (calculated as difference score between the ipsilesional and contralesional cerebral blood flow) differed significantly in the MCA between healthy controls and the AIS group. Cerebral blood flow imbalance of the MCA was negatively associated with working memory performance in children after pediatric AIS. Working memory is a crucial functional domain that underlies many higher-order cognitive functions such as reading, arithmetics and self-regulation processes65. Mean working memory performance was 0.55 standard deviations below the mean in the present patient sample and presents the most pronounced deficit among the cognitive functions measured. However, cognitive flexibility was also negatively related to cerebral blood flow imbalance of the MCA with weak to moderate effect sizes. Our findings suggest that a certain hemispheric imbalance seems to promote the persistence of cognitive deficits. Wiest et al.29 examined cerebral blood flow imbalance in adults in the subacute phase of AIS and reported similar results, showing that incomplete motor recovery was associated with a greater interhemispheric imbalance. After stroke, alterations in neurovascular function, such as cerebrovascular reactivity (CVR), might help to explain the present results. The co-occurrence of hypoperfusion and reduced CVR has been reported previously66 and reduced CVR has been reported in lesioned brain areas in both acute and chronic recovery66,67. Additionally, cerebral blood flow mirrors metabolic demand and neuronal activity. Thus, decreased ipsilesional cerebral blood flow may reflect decreased neuronal activity due to reductions in the neurons’ metabolic needs and network connectivity after the loss of cells within the lesioned brain area20. This would be in line with the negative correlation between cerebral blood flow and cognitive functions described previously33. Whether the relationship between cerebral blood flow imbalance and cognitive outcome is of causal nature remains to be determined in future studies using methods that have the power to unravel causality.
Overall, our data support the idea that cerebral hypoperfusion might underlie some of the variability observed in long-term outcome after stroke. The present findings offer insights into the state of cerebral perfusion years after stroke and highlight the role of interhemispheric perfusion balance in the MCA for working memory performance. Our results provide further support that the assessment of cerebral blood flow perfusion with ASL presents a possible index for evaluating the effectiveness of rehabilitation at the perfusion level.
Strengths and limitations
This study had some notable strengths. First, ASL is gaining attention as a non-invasive alternative to invasive perfusion imaging after stoke and can be performed in 2–5 min. Second, an extended test battery was adopted to investigate several cognitive domains with different tasks to enable the assessment of domain-specific outcome, as well as an overall cognitive outcome score. Third, our study included a homogeneous sample of patients after pediatric AIS in the MCA and excluded children following neonatal arterial ischemic stroke, periventricular venous infarction or stroke to other vessel territories. This helps in disentangling the effects of pathophysiological mechanisms and lesion-related characteristics on cerebral perfusion alterations and on cognitive outcome.
Nevertheless, our study has some limitations. First, our results are based on a small and clinically heterogeneous sample. However, there is the chance of recruitment bias towards a rather homogeneous and well-functioning patient group, as patients with behavior problems or severe handicaps were unable to follow the study regime and hence were excluded. The study sample included children across a wide age range at time of assessment and hence at different neurodevelopmental stages. The rarity of childhood stroke (1–2 cases per center per year in Switzerland based on estimates from the SNPSR from 2000 to 2019) makes recruitment a challenge. Nonetheless, further research is needed to replicate our findings in a larger cohort and confirm that cerebral blood flow alterations are related to cognitive functions throughout post-stroke recovery. Secondly, AIS in childhood is based on multifactorial causes, which themselves can be associated with perfusion characteristics and cognitive outcome68.
Conclusion
Our findings revealed that ipsilesional cerebral blood flow is reduced across all vessel territories even years after pediatric stroke. Hemispheric imbalance of the cerebral blood flow is negatively associated with cognitive outcome. This finding has important clinical and theoretical implications and may need to be taken into account when examining the relationship between brain lesion and cognition in the future. First, measurements of cerebral perfusion imbalance in the acute phase after stroke might be useful in predicting future cognitive impairment. Second, changes in cerebral blood flow imbalance may be used to track the process of recovery longitudinally, in particular as a marker of neuronal recovery. Identification of optimal treatment strategies to support recovery is still limited by the wide variance in outcomes of patients after AIS. Thus, identifying biomarkers that distinguish patient subgroups will help to identify factors that are important for successful recovery after pediatric AIS. The results of this study raise new questions for future research including whether rehabilitation efforts can increase interhemispheric perfusion recovery. In the future, a multimodal imaging approach will be needed to find out how functional networks measured with functional MRI or resting-state fMRI are related to cerebral blood flow.
References
Mallick, A. A. & O’Callaghan, F. J. The epidemiology of childhood stroke. Eur. J. Paediatr. Neurol. 14, 197–205 (2010).
deVeber, G. Stroke and the child’s brain: An overview of epidemiology, syndromes and risk factors. Curr. Opin. Neurol. 15, 133–138 (2002).
Goeggel Simonetti, B. et al. Long-term outcome after arterial ischemic stroke in children and young adults. Neurology 84, 1941–1947 (2015).
Sutherly, L. J. & Malloy, R. Risk factors of pediatric stroke. J. Neurosci. Nurs. 52, 58–60 (2020).
Steinlin, M. et al. The first three years of the Swiss Neuropaediatric Stroke Registry (SNPSR): A population-based study of incidence, symptoms and risk factors. Neuropediatrics 36, 90–97 (2005).
Greenham, M., Gordon, A., Anderson, V. & Mackay, M. T. Outcome in childhood stroke. Stroke 47, 1159–1164 (2016).
Pavlovic, J. et al. Neuropsychological problems after paediatric stroke: Two year follow-up of Swiss children. Neuropediatrics 37, 13–19 (2006).
O’Keeffe, F. et al. Neuropsychological and neurobehavioral outcome following childhood arterial ischemic stroke: Attention deficits, emotional dysregulation, and executive dysfunction. Child Neuropsychol. 20, 557–582 (2014).
Everts, R. et al. Cognitive functioning, behavior, and quality of life after stroke in childhood. Child Neuropsychol. 14, 323–338 (2008).
Studer, M. et al. Factors affecting cognitive outcome in early pediatric stroke. Neurology 82, 784–792 (2014).
Westmacott, R., Askalan, R., MacGregor, D., Anderson, P. & Deveber, G. Cognitive outcome following unilateral arterial ischaemic stroke in childhood: Effects of age at stroke and lesion location. Dev. Med. Child Neurol. 52, 386–393 (2010).
Long, B. et al. Executive function following child stroke: The impact of lesion location. J. Child Neurol. 26, 279–287 (2011).
Jann, K., Kottlow, M., Dierks, T., Boesch, C. & Koenig, T. Topographic electrophysiological signatures of FMRI Resting State Networks. PLoS One 5, e12945 (2010).
Heiss, W. D., Sobesky, J. & Hesselmann, V. Identifying thresholds for penumbra and irreversible tissue damage. Stroke 35, 2671–2674 (2004).
Moustafa, R. R. & Baron, J. C. Pathophysiology of ischaemic stroke: Insights from imaging, and implications for therapy and drug discovery. Br. J. Pharmacol. 153(Suppl 1), S44–S54 (2008).
Andersen, K. K., Olsen, T. S., Dehlendorff, C. & Kammersgaard, L. P. Hemorrhagic and ischemic strokes compared: Stroke severity, mortality, and risk factors. Stroke 40, 2068–2072 (2009).
Chen, J. et al. Arterial spin labeling perfusion MRI in pediatric arterial ischemic stroke: Initial experiences. J. Magn. Reson. Imaging 29, 282–290 (2009).
Bulder, M. M. et al. Arterial spin labeling perfusion MRI in children and young adults with previous ischemic stroke and unilateral intracranial arteriopathy. Cerebrovasc. Dis. 37, 14–21 (2014).
Wang, C. et al. Cerebral blood flow features in chronic subcortical stroke: Lesion location-dependent study. Brain Res. 1706, 177–183 (2019).
Richardson, J. D. et al. Cerebral perfusion in chronic stroke: Implications for lesion-symptom mapping and functional MRI. Behav. Neurol. 24, 117–122 (2011).
Beaulieu, C. et al. Longitudinal magnetic resonance imaging study of perfusion and diffusion in stroke: Evolution of lesion volume and correlation with clinical outcome. Ann. Neurol. 46, 568–578 (1999).
Hillis, A. E. Magnetic resonance perfusion imaging in the study of language. Brain Lang. 102, 165–175 (2007).
Rodriguez, G. et al. Regional cerebral blood flow in chronic stroke patients. Stroke 24, 94–99 (1993).
Love, T., Swinney, D., Wong, E. & Buxton, R. Perfusion imaging and stroke: A more sensitive measure of the brain bases of cognitive deficits. Aphasiology 16, 873–883 (2002).
Fridriksson, J., Rorden, C., Morgan, P. S., Morrow, K. L. & Baylis, G. C. Measuring the hemodynamic response in chronic hypoperfusion. Neurocase 12, 146–150 (2006).
Boukrina, O., Barrett, A. M. & Graves, W. W. Cerebral perfusion of the left reading network predicts recovery of reading in subacute to chronic stroke. Hum. Brain Mapp. 40, 5301–5314 (2019).
Chalela, J. A. et al. Magnetic resonance perfusion imaging in acute ischemic stroke using continuous arterial spin labeling. Stroke 31, 680–687 (2000).
Bonakdarpour, B., Parrish, T. B. & Thompson, C. K. Hemodynamic response function in patients with stroke-induced aphasia: Implications for fMRI data analysis. Neuroimage 36, 322–331 (2007).
Wiest, R. et al. Interhemispheric cerebral blood flow balance during recovery of motor hand function after ischemic stroke—A longitudinal MRI study using arterial spin labeling perfusion. PLoS One 9, e106327 (2014).
Leistner, R. et al. Cerebral blood flow imbalance is associated with motor outcome after pediatric arterial ischemic stroke. PLoS One 14, e0223584 (2019).
Kilroy, E. et al. Relationships between cerebral blood flow and IQ in typically developing children and adolescents. J. Cogn. Sci. (Seoul) 12, 151–170 (2011).
De Vis, J. B. et al. Arterial-spin-labeling (ASL) perfusion MRI predicts cognitive function in elderly individuals: A 4-year longitudinal study. J. Magn. Reson. Imaging 48, 449–458 (2018).
Strouse, J. J. et al. Inverse correlation between cerebral blood flow measured by continuous arterial spin-labeling (CASL) MRI and neurocognitive function in children with sickle cell anemia (SCA). Blood 108, 379–381 (2006).
Kazumata, K. et al. Association of cognitive function with cerebral blood flow in children with moyamoya disease. J. Neurosurg. Pediatr. https://doi.org/10.3171/2019.7.PEDS19312 (2019).
Rosenbaum, J. L., Almli, C. R., Yundt, K. D., Altman, D. I. & Powers, W. J. Higher neonatal cerebral blood flow correlates with worse childhood neurologic outcome. Neurology, 49, 1035–1041 (1997).
Kornfeld, S. et al. Cortical reorganisation of cerebral networks after childhood stroke: Impact on outcome. BMC Neurol. 15, 90 (2015).
Brown, L., Sherbenov, R. J. & Johnsen, S. K. Test of Nonverbal Intelligence (TONI-4) 4th edn. (PRO-ED, 2010).
Petermann, F. & Petermann, U. Hamburg-Wechsler-Intelligenztest für Kinder—IV (HAWIK-IV) (Hans Huber, 2012).
Petermann, F. Wechsler Adult Intelligence Scale 4th edn. (Pearson, 2012).
Zimmermann, P. & Fimm, B. Testbatterie zur Aufmerksamkeitsprüfung: TAP (Version 2.1) (Psytest, 2008).
Delis, D. C., Kramer, J. H., Kaplan, E. & Holdnack, J. Reliability and validity of the Delis-Kaplan Executive Function System: An update. J. Int. Neuropsychol. Soc. 10, 301–303 (2004).
Helmstaedter, C. A., Lendt, M. & Lux, S. Verbaler Lern- und Merkfähigkeitstest: VLMT (Beltz Test, 2001).
Beery, K. E. & Beery, N. A. The Beery-Buktenica Developmental Test of Visual-Motor Integration: Administration, scoring, and teaching manual 5th edn. (NCS Pearson, 2004).
Wu, K. et al. Topological organization of functional brain networks in healthy children: Differences in relation to age, sex, and intelligence. PLoS One 8, e55347 (2013).
Dai, W., Garcia, D., de Bazelaire, C. & Alsop, D. C. Continuous flow-driven inversion for arterial spin labeling using pulsed radio frequency and gradient fields. Magn. Reson. Med. 60, 1488–1497 (2008).
Wang, J. et al. Pediatric perfusion imaging using pulsed arterial spin labeling. J. Magn. Reson. Imaging 18, 404–413 (2003).
Buxton, R. B. Quantifying CBF with arterial spin labeling. J. Magn. Reson. Imaging 22, 723–726 (2005).
Federspiel, A., Muller, T. J., Horn, H., Kiefer, C. & Strik, W. K. Comparison of spatial and temporal pattern for fMRI obtained with BOLD and arterial spin labeling. J. Neural Transm. (Vienna) 113, 1403–1415 (2006).
Alsop, D. C. et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn. Reson. Med. 73, 102–116 (2015).
Appelman, A. P., van der Graaf, Y., Vincken, K. L., Mali, W. P. & Geerlings, M. I. Combined effect of cerebral hypoperfusion and white matter lesions on executive functioning—The SMART-MR study. Dement. Geriatr. Cogn. Disord. 29, 240–247 (2010).
Yao, H. & Fujishima, M. Cerebral blood flow and metabolism in silent brain infarction and related cerebrovascular disorders. Ann. Med. 33, 98–102 (2001).
Logothetis, N. K., Pauls, J., Augath, M., Trinath, T. & Oeltermann, A. Neurophysiological investigation of the basis of the fMRI signal. Nature 412, 150–157 (2001).
Baron, J. C. & Marchal, G. Ischemic core and penumbra in human stroke. Stroke 30, 1150–1153 (1999).
Carmichael, S. T. The 3 Rs of stroke biology: Radial, relayed, and regenerative. Neurotherapeutics 13, 348–359 (2016).
Crinion, J., Holland, A. L., Copland, D. A., Thompson, C. K. & Hillis, A. E. Neuroimaging in aphasia treatment research: Quantifying brain lesions after stroke. Neuroimage 73, 208–214 (2013).
Brumm, K. P. et al. An arterial spin labeling investigation of cerebral blood flow deficits in chronic stroke survivors. Neuroimage 51, 995–1005 (2010).
Ohab, J. J. & Carmichael, S. T. Poststroke neurogenesis: Emerging principles of migration and localization of immature neurons. Neuroscientist 14, 369–380 (2008).
Long, B. et al. Executive function following child stroke: The impact of lesion size. Dev. Neuropsychol. 36, 971–987 (2011).
Steiner, L. et al. Functional topography of the thalamo-cortical system during development and its relation to cognition. Neuroimage 223, 117361 (2020).
Everts, R. et al. Strengthening of laterality of verbal and visuospatial functions during childhood and adolescence. Hum. Brain Mapp. 30, 473–483 (2009).
Remer, J. et al. Quantifying cortical development in typically developing toddlers and young children, 1–6 years of age. Neuroimage 153, 246–261 (2017).
Deoni, S. C., Dean, D. C. 3rd., O’Muircheartaigh, J., Dirks, H. & Jerskey, B. A. Investigating white matter development in infancy and early childhood using myelin water faction and relaxation time mapping. Neuroimage 63, 1038–1053 (2012).
Toga, A. W., Thompson, P. M. & Sowell, E. R. Mapping brain maturation. Trends Neurosci. 29, 148–159 (2006).
Kandel, E. R., Schwartz, J. H. & Jessell, T. M. Principles of Neural Science 4th edn, 1227–1246 (McGraw-Hill, 2000).
Nouwens, S., Groen, M. A., Kleemans, T. & Verhoeven, L. How executive functions contribute to reading comprehension. Br. J. Educ. Psychol. 91, 169–192 (2020).
Bokkers, R. P. et al. Symptomatic carotid artery stenosis: Impairment of cerebral autoregulation measured at the brain tissue level with arterial spin-labeling MR imaging. Radiology 256, 201–208 (2010).
Krainik, A., Hund-Georgiadis, M., Zysset, S. & von Cramon, D. Y. Regional impairment of cerebrovascular reactivity and BOLD signal in adults after stroke. Stroke 36, 1146–1152 (2005).
Curry, C. J. et al. Risk factors for perinatal arterial stroke: A study of 60 mother-child pairs. Pediatr. Neurol. 37, 99–107 (2007).
Acknowledgements
This study was supported by the Swiss National Science Foundation (Grant 32003B_146894) and the Anna Müller Grocholski Foundation (Switzerland). The authors thank all the children who participated in the study as well as their parents. Furthermore, a big thank you goes to all co-workers at the Swiss Neuropaediatric Stroke Registry: Andrea Capone Mori (Aarau), Alexandre Datta (Basel), Joël Fluss (Geneva), Annette Hackenberg (Zürich), Elmar Keller (Chur), Oliver Maier (St. Gallen), Jean-Pierre Marcoz (Sion), Claudia Poloni (Lausanne), Gian Paolo Ramelli (Bellinzona), Maria Regenyi (Berne), Regula Schmid (Winterthur), and Thomas Schmitt-Mechelke (Lucerne). We would also like to thank Salome Kornfeld, Sandeep Kamal and Juan Delgado-Rodriguez for their numerous hours of help with clinical data acquisition. In addition, we thank Susan Kaplan for editing the manuscript.
Author information
Authors and Affiliations
Contributions
L.S. and R.E. wrote the manuscript. M.S., S.G. and R.E. obtained funding and designed the study. N.S. and R.W. were responsible for the acquisition and interpretation of neuroimaging data, J.J. assisted in the set up of the manuscript. All authors reviewed and revised the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Steiner, L., Federspiel, A., Jaros, J. et al. Cerebral blood flow and cognitive outcome after pediatric stroke in the middle cerebral artery. Sci Rep 11, 19421 (2021). https://doi.org/10.1038/s41598-021-98309-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98309-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.