Abstract
In the years 2006–2011, 617 Proteus spp. strains isolated mostly from urine and wounds or other clinical sources were collected in Łódź, Poland, to determine the offensive O serotypes frequently occurring among patients. P. mirabilis exhibited the most intensive swarming growth and was dominating species (86.9%), followed by P. genomospecies, P. vulgaris, and P. penneri. Ninety four per cent strains were recognized as S (smooth) forms. Serological studies (involving ELISA—enzyme-linked immunosorbent assay and Western blotting using native and adsorbed rabbit antisera) enabled classification of 80% S isolates into respective Proteus O serogroups among the 83 ones, described so far. The remaining strains seemed to be serologically unique. Despite the observed big serological variety of Proteus spp. isolates, we found the O78 serogroup recently described in Poland as dominating and identified other widespread serotypes: O3, O6, O10, O11, O27, O28, and O30 reported earlier as predominating also in other countries; O77 and O79 detected lately in Poland; O16, O18, O20, and O50. No unique structural feature of the prevalent O serotypes has been indicated. However, the prevalence of some O serogroups indicates that particular serotypes may be in some ways beneficial to the strains producing these kinds of O antigen.
Similar content being viewed by others

Introduction
Proteus spp. bacteria are peritrichously flagellated members of Morganellaceae family distinguished from the other representatives of the order Enterobacterales by intensive and spectacular swarming growth on solid media as a result of the multicellular differentiation phenomenon1,2. These bacilli are detected in natural environments (water or soil) and in many species of wild and domestic animals. They have also been found to be a component of natural faecal microbiota in a part of human population. On the other hand, Proteus spp. are opportunistic pathogens, which may affect mainly immunocompromised individuals and cause infections of the urinary tract and wounds, bacteraemia, abscesses in many organs or other infections3. Among the pathogenic species, P. mirabilis is most common followed by less frequently isolated P. vulgaris, P. penneri, P. hauseri, and three genomospecies without names (P. genomospecies 4, 5, and 6). Lack of biochemical reactions which would reliably distinguish between different P. genomospecies resulted in limited knowledge on their characteristics and isolation frequency4,5, when compared to well-described P. mirabilis. Urinary tract infections (UTIs) of P. mirabilis aetiology are frequently catheter-associated—CAUTIs, recurrent and dangerous due to the frequent and severe complications like pyelonephritis and urolithiasis2.
Among numerous virulence factors of Proteus bacteria, the lipopolysaccharide (LPS) should be emphasized as an endotoxin and an important antigen determining the serological specificity of Proteus spp. strains. The LPS core region in the genus Proteus is structurally and serologically diverse, which has led to the formation of the R (rough) typing Proteus scheme containing 11 R serotypes6. However, mainly the highly immunogenic O-polysaccharide region determines the serological specificity of LPS S (smooth) forms, which has become a basis for the classification of Proteus strains into 83 O serogroups7,8. The first O type scheme for P. mirabilis and P. vulgaris strains including 49 O serogroups was founded by Kauffmann9. Later, Larsson10 indicated O3, O6, O10, O11, O13, O23, O24, O26, O27, O28, O29, and O30 as the most prevalent serogroups in many countries. The Kauffmann’s scheme was further extended with other O serogroups containing all Proteus species7 but only a few P. penneri and P. mirabilis strains come from Poland11,12. Gathering a new wide collection of more than 600 Proteus spp. clinical isolates from the Łódź region (central Poland) enabled us to study their serological differentiation. Up to date, serologically unique strains from the collection have formed six new serogroups O77-O8213,14,15,16,17,18 and two new subgroups in O8 and O11 serogroups19,20. In this work the serological variety of the whole collection of Proteus spp. strains is shown focusing on Proteus O serogroups most widespread in central Poland (Łódź region).
Methods
Bacterial strains, physiological tests, LPSs
Six hundred and seventeen Proteus spp. strains (including the 24 strains reported earlier13,14,15,16,17,18,19,20) were isolated from different clinical sources (Fig. 1) in the Łódź city, central Poland, in that number 606 ones from infected individuals. The bacteria were also detected in faeces from eleven carriers out of 189 individuals with no problems in the digestive tract. The strains were kindly gifted in 2006–2011 by the four biggest medical laboratories in Łódź (Poland): laboratories in Barlicki Hospital and in Biegański Hospital, as well as „Synevo” laboratory and „Diagnostyka” laboratory. The strains were isolated both in hospitals and from non-hospitalized patients, coming from Łódź city and Łódź region. We identified all the isolates’ species by the cultivation on the media proposed by Senior21, modified as described13 and used for testing ornithine decarboxylation, phenylalanine deaminase and urease production, mannose fermentation and indole formation. Additional tests (for L-rhamnose fermentation, lipase production, Jordan’s tartrate and DNase) were applied for the strains recognized as P. genomospecies, as described4,15 (Table 1). All strains were retained in stocks (Luria Broth (LB) cultures with 25% glycerol) at − 80 °C.
S-R tests included both the thermal stability in the boiled broth medium test and the pseudoagglutination test22. Additionally, the swarming growth ability on Luria Broth medium with 1.5% agar was studied, according to Wilkerson and Niederhoffer23. In these tests, P. penneri 13 rough strain coming from the collection of the Laboratory of General Microbiology, University of Łódź, was applied as a control.
Thermal stability of broth cultures: 18-h bacterial cultures in LB liquid medium were heated (2.5 h at 100 °C). Bacterial R forms precipitated from the broth and formed a sediment (the broth above it was clear), which differentiated them from S forms (not precipitating, stable suspended in the whole broth volume). In contrast, SR phenotypes formed a small amount of sediment but the broth above it remained cloudy.
Pseudoagglutination assay: the bacterial cells from 18-h nutrient broth agar slant cultures were suspended in a drop of 0.85% NaCl in a microscopic slide. Self-agglutination was seen for R forms of bacteria while S forms did not agglutinate.
Swarming growth ability: plates with the LB medium supplemented with agar (1.5%) were dried to remove drops of water from their surface. LB liquid culture of each strain was spot inoculated (10 μl) in the center of an LB plate and incubated for 24 h at 37 °C. Over this period concentric swarm zones were counted and a radius of the total swarming growth area was measured.
Biomasses of the studied strains were obtained by 18-h cultivation on a nutrient broth medium supplemented with 0.2% glucose, with aeration, at 37 °C. The strains were killed by 1% phenol, centrifuged, washed with distilled water and stored in + 4 °C (wet biomass) or lyophilized (dry biomass).
LPSs were extracted from strains’ dry biomass in 45% phenol for 5 min at 65 °C using the classic phenol-water method, published by Westphal and Jann24. After centrifugation (4845×g) the water phase containing LPS with long OPS chains was collected and the extraction was repeated. The water phases were combined, dialyzed from phenol for 48 h and centrifuged (4845×g) to remove the cell debris. The LPS solution was adjusted to 2% CH3COONa and a crude LPS was precipitated by the addition of 2 v of 96% ethanol. The LPS precipitate was dissolved in distilled water, dialyzed from the salt and ethanol remains (24 h, 4 °C) and lyophilized.
LPSs and biomasses used as the antigens in SDS-PAGE were suspended in loading buffer, boiled for 10 min. and then treated with proteinase K (10 mg/ml) for 1 h at 60 °C15.
Serological investigation
We applied ELISA (enzyme-linked immunosorbent assay) and Western-blotting methods using bacterial biomasses and LPS preparations (extracted from selected studied strains or coming from our collection) as a source of O antigens as well as polyclonal rabbit sera specific to all the O serotypes reported in the genus Proteus (from our collection), as described earlier15,25.
Additionally, to confirm the classification of studied strains to 14 most numerous serogroups, we used the respective 14 antisera adsorbed by wet bacterial mass of cross-reacting strains, previously washed in PBS. The biomass was suspended in a serum diluted (1:50) in PBS in a proportion of 1:10 and incubated for 30 min. on ice. The cells were removed from the serum by centrifugation and the process was repeated twice13. Then, in ELISA, a lack of the reaction of the adsorbed antiserum with the homologous LPS confirmed the identity of the cross-reacting O antigen with the reference LPS due to removal of all the specific antibodies during adsorption. The stronger reaction observed in ELISA or Western blotting after adsorption, the lower similarity was proved.
In ELISA, LPSs (50 ng per well) or the bacterial biomasses (5 µg per well) were applied for coating the F96 Maxisorp Nunc-Immuno plates (12 h, + 4 °C). After washing the plates twice with distilled water to remove the residual antigens, the uncoated sites in the wells were blocked with casein buffer (2.5% casein, 240 mM of NaOH, 1.5 mM of KH2PO4, 8 mM of Na2HPO4, pH 7.2) for 1 h at 37 °C, to avoid subsequent unspecific adsorption of antibodies. The plates were doubly washed with phosphate buffer saline (PBS, 136.8 mM of NaCl, 2.7 mM of KCl, 8 mM of Na2HPO4, pH 7.2) and incubated with the appropriate polyclonal rabbit antiserum (twofold serially diluted in 50 µl of casein buffer) for 1 h at 37 °C. After triple washing the plates with PBS (to remove the unbound immunoglobulins), the rabbit-IgG specific goat antibodies labelled with horseradish peroxidase (Jackson ImmunoResearch) diluted 1:5.000 in casein buffer were added (50 µl/well) and the plates were incubated as described above. Triple washing with PBS and a single one with substrate buffer (0,1 M of C6H5Na3O7, pH 4.5) were applied and the solution of 2,2’-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) diammonium salt (ABTS) in substrate buffer with the addition of 3% H2O2 (1:25) was used (50 µl/well) as a substrate for peroxidase. After 30 min. of incubation at 37 °C, the colour reaction was stopped by the use of oxalic acid (222 mM). Antibody titers were determined, in relation to a blind sample (ABTS solution), by measuring the absorbance (A405) using Multiskan Go microplate reader (Thermo Scientific). Absorbance ≥ 0.2 was considered as indicating a positive reaction.
In Western blotting, bacterial biomass or LPS in the loading buffer (5–8 µg per lane of polyacrylamide 3% stacking gel) were separated during sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS PAGE) on 200 V. Then, the samples were transferred to nitrocellulose (Whatman Schleicher & Schuel) in transfer buffer (25 mM Tris/HCl, 192 mM of glycine, 20% methanol) on 100 V for 1 h. The membrane was fixed for 5 min. with the solution of 10% isopropanol and 10% acetic acid in water and blocked with 10% skimmed milk in dot-blot buffer (50 mM of Tris/HCl pH 7,4, 200 mM of NaCl) for 1 h. Then, the nitrocellulose was incubated with appropriate rabbit antiserum diluted 1:500 in dot-blot-10% skimmed milk buffer (2 h) and, after washing with the dot-blot buffer, with the rabbit-IgG specific goat antibodies conjugated with alkaline phosphatase (Jackson ImmunoResearch) diluted 1:5000 in the dot-blot-10% skimmed milk buffer (2 h). AP Conjugate Substrate Kit (Bio-Rad) was applied as a substrate of alkaline phosphatase to obtain a colour reaction, which was stopped by washing the membrane in distilled water. Western blotting reactions were scanned by means of Canon Toolbox 4.9.
Results
Physiological features
Among the 617 studied strains, urine isolates and wound isolates (including bacteria from pus, bedsores, fistulas, skin and wound swabs, and abscesses) were dominating. Other frequent sources of isolation were connected with the respiratory tract (bronchoaspirates, sputum, and the pharyngonasal cavity), vagina, and faeces, while strains from other sources were isolated rarely (Fig. 1). It was also shown that the eleven Proteus spp. strains (nine P. mirabilis, one P. vulgaris, and one P. genomospecies 5/6 including four strains reported earlier13,14,20) were inhabiting the intestines of 5.8% from 189 individuals (carriers).
The strains species were identified on the basis of the metabolic features of the isolates (Table 1). P. mirabilis species was definitely predominant, while the contribution of the other detected Proteus species was much lower (Table 1). Totally, 41 isolates (6.6%) were found to belong to P. genomospecies 4 or 5/6, the two last are still impossible to distinguish on the grounds of their metabolic properties4,5, while no isolate was classified to P. hauseri species. Thus, it can be assumed that P. genomospecies are isolated from clinical sources with a frequency comparable to that observed for P. vulgaris and all the isolates belonging to the so called P. vulgaris group together account for 11.7% of the whole collection, where P. genomospecies 4 is the rarest. Contrary to P. mirabilis and P. penneri (Fig. 1a,b), among P. vulgaris and P. genomospecies the isolates from wounds were found to dominate, while the isolates from urine were less common (Fig. 1c,d).
To select the isolates which can be typed to O serogroups (S forms), we conducted S-R tests. Thirty seven studied strains (6% of the collection) which were totally or partly non-thermal stable and agglutinated in 0.85% NaCl were recovered as R or S/R forms possessing LPS deficient in O polysaccharide or LPS with only one O-repeating unit, respectively. R forms constituted only 4.9% of P. mirabilis strains (26 out of all collected P. mirabilis isolates), while in P. vulgaris it was 9.7% (three out of 31 P. vulgaris isolates), in P. genomospecies 4 and 5/6—14.6% (six out of 41 isolates), and in P. penneri—22.2% (two out of nine isolates). As the shortened LPS without O-polysaccharide part does not guarantee a proper and stable truncation of the flagella, the swarming growth of R forms is usually decreased or stopped. As expected, the majority of R strains were not able to swarm on the surface of solid Luria Broth medium. However, among the smooth strains, the non-swarming ones were also detected. Most of P. mirabilis isolates (more than 90%) were found to be able to swarm and 70% exhibited intensive swarming growth (on the distance > 30 mm within 24 h). In the case of P. penneri, non-swarming strains constituted 22% (R forms only) while the other isolates were able to swarm effectively. The weakest swarming growth ability was observed among P. vulgaris and P. genomospecies isolates as 50% of strains have not showed this ability or could swarm very weakly (< 10 mm within 24 h).
Serological features
A total of the 580 S strains (possessing an O antigen in the LPS molecules) were serologically investigated to classify them into proper O serogroups in the genus Proteus. The results for 24 of these strains classified to O2, O8, O11, O77—O82 serogroups, respectively, had been reported previously13,14,15,16,17,18,19,20 .
Biomasses of the S strains were studied in ELISA with rabbit polyclonal antisera specific to all the Proteus O serogroups described so far. Strong cross reactions comparable to the ones in the homologous systems (mostly to the titre 1:128000 or more) were the first indication on the serological type of the studied strains. But the obtained results were not always so clear.
Several biomasses were not recognized by any antisera (the O antigens present on the cells were possible to be masked by other cell wall components) and some cross reacted with more than one antiserum achieving various titres (other surface antigens may have also been recognized by the antibodies present in the used rabbit antisera). In these cases, LPS preparations were extracted from the biomasses by the phenol-water procedure24. Purified LPS antigens coated on the ELISA plates might be better exposed and better accessible to specific antibodies. Indeed, in consequence the O serotype of several such strains was identified.
These results allowed recognizing the similarity of most of the isolates (447/556 S forms studied in this work) to particular O serotypes among 83 Proteus O serogroups recognized so far, while the remaining strains seemed to be serologically unique and were considered to represent new O serogroups in the genus Proteus. One hundred and fifty six isolates had been preliminarily classified into 47 O serogroups (data not shown) formed by fewer than 10 studied strains. More than a half (291) of the studied here 556 S Proteus spp. clinical strains were initially considered as belonging to 14 predominating O serogroups consisting of 10 or more strains: O3, O6, O10, O11, O16, O18, O20, O27, O28, O30, O50, O60, O77, and O78.
To confirm that consideration, the sera specific to the 14 most prevalent O serotypes were adsorbed by the cross-reacting biomasses and their reactions with the homologous LPSs were analyzed in ELISA. In most cases, the reactions of the antisera in the homologous systems were totally abolished due to the removal of all LPS-specific antibodies by the cross-reacting biomasses, indicating their antigenic identity and confirming the initial serological classification (Table 2). However, in some cases the adsorption was not complete and some remaining fractions of antibodies still reacted with homologous LPSs, although the reactions were obviously weaker than the ones of the native antisera (Table 2). In these 34 cases, some differences in the strains serospecificity were responsible for not full adsorption of the antisera. The antibodies which could not be removed from the adsorbed antisera should be specific to some epitopes, which are present in the reference homologous LPSs (core region or O antigen) but absent in the cross-reacting studied strains. Thus, such reactions indicated more or less antigenic similarity but not the identity of the studied strains and the reference LPSs.
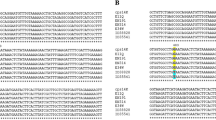
The nature of the cross reactions, observed in ELISA, was visualized in the Western-blotting method using LPS preparations obtained by proteinase-K treated biomasses as antigens (Figs. 2, 3, 4). The reactions are similar and comparable to the ones observed for the LPS preparations obtained using phenol-water extraction, which is demonstrated on the example of strains classified to O77 serogroup (Fig. 2a,b). By the degradation of proteins, we could remove possible non-specific cross reactions caused by protein antigens rather than by O antigens26. Indeed, the initially observed in ELISA reactions of several biomasses not fully adsorbing the respective antisera, could have been caused by protein antigens, as they were not confirmed in Western blots. That was the case of four strains (Fig. 3b, paths 2–5) preliminarily classified into O10 serogroup, two strains (Fig. 3c, paths 8, 9) classified into O28 serogroup, and one strain (Fig. 3d, path 8) classified into O50 serogroup, which displayed completely no reaction after proteinase-K treatment in Western blots.
The Western-blotting technique also allowed localizing LPS epitopes responsible for the strong cross reactions initially observed in ELISA. The epitopes may have been present in the O-specific part and/or in the core region of the LPSs exposed on the biomasses of the studied strains. Indeed, among the strains preliminarily classified into O10 serogroup on the basis of strong reactions of their biomasses in ELISA, one isolate showed in Western blot reactions only in the fast-migrating fractions corresponding to the lipid A-core region, while there were no reactions observed for the slowly migrating LPS bands additionally possessing O-polysaccharide chains (Fig. 3b, path 8). Similar results were obtained in the case of as many as four strains (Fig. 3a, paths 2, 6, 7, and 9) initially classified into O3 serogroup. The O3 and O10 antisera are visibly rich in antibodies recognizing core-localized common epitopes and responsible for strong cross reactions observed both in ELISA and in Western blots. Obviously, these five strains cannot be included in O3 or O10 serogroups, although they may form R serogroups.
Noteworthy, the 15 strains initially classified into the most numerous O78, O16, and O11 serogroups but not fully adsorbing the respective O78, O16, or O11 antisera (Table 2) displayed in Western blots visible strong reactions of the slowly-migrating LPS molecules possessing O polysaccharides (O-PS), which is showed on the example of the strains (2–7) classified to O78 serogroup (Fig. 4a, paths 2–7). The use of the O78, O16, or O11 antisera adsorbed by the respective biomasses in the Western-blotting technique proved that the observed serological differences refer mainly to the O-specific parts of these strains’ LPS. As the antisera contain small amounts of anti-core antibodies, the possible differences in core antigens were hard to be detected. The adsorbed O78, O16, and O11 antisera did not react with the respective adsorbing biomasses, which confirmed the properly conducted adsorption processes (control), but still in these three antisera there were remaining some fractions of antibodies recognizing the epitopes located in the homologous O antigens (slowly-migrating LPS bands) but absent in the studied strains. The Western-blotting results for these 15 strains were similar and they are shown on the example of O78 antiserum adsorbed with strain 2 (Fig. 4b). Thus, the 15 strains were recognized as representing different subgroups within O78, O16, or O11 serogroups, respectively.
Discussion
In the years 2006–2011 a total of 617 Proteus spp. strains were collected in Łódź, Poland (Fig. 1) including the 24 clinical strains reported earlier13,14,15,16,17,18,19,20. What is worth noticing, no strains were collected from blood, although Proteus spp. bacteria may also cause severe bacteremia and sepsis2,27. Urine and wound isolates were prevailing (Fig. 1). Frequent isolation of P. mirabilis (Table 1) is not surprising, as the species is regarded as the most virulent and widespread species in the genus Proteus, especially in patients suffering from nosocomial urinary tract and wound infections and it is still the most frequently isolated species among Proteus spp.2. P. genomospecies 4, 5, 6, or P. hauseri are not usually distinguished from P. vulgaris in the routine laboratory work and so there are very few reports available on their occurrence in patients. Similarly to our results, O’Hara et al.4 and Janda et al.5 studying several P. hauseri, P. genomospecies 4, 5, and 6 strains, mostly from human sources, found P. genomospecies 5 and 6 to be the most numerous. Our results confirm the low frequency of P. penneri isolation from clinical sources28,29. Recently, Dai et al.30 have proposed a new molecular MLSA (multilocus sequence analysis) technique for identification of Proteus species, suggesting a reclassification of P. cibarius and P. genomospecies 5 into the formerly described species P. terrae isolated from soil. Among 210 isolates from clinical specimens and food in China, the authors found P. terrae as being the second most abundant species after P. mirabilis, when P. vulgaris and P. penneri as the third and fourth ones, respectively.
R forms which are regarded as less virulent, we found among the isolates belonging to all the identified Proteus species. However, in the most pathogenic P. mirabilis species, the smallest number of R forms was detected and the best swarming ability was noticed which is considered to be an important virulence factor. P. genomospecies and P. vulgaris isolates demonstrated weaker swarming growth in comparison to P. penneri strains, similarly to the results achieved by Kwil et al.31.
Serotyping is an important way of typing and classification of bacteria, especially in diagnostics and epidemiology of some pathogenic genera like Salmonella. In the case of this genus, besides the classical phenotypic methods new precise molecular tools are recommended, such as whole genome sequencing (WGS)-based serotype prediction and microarray-based method32. WGS was also applied in studies of a P. mirabilis strain virulence33. Many O-antigen gene clusters were analyzed and O serotype-specific suspension array for detecting selected Proteus serotypes has been proposed34. However, the prevalence and significance of particular serogroups in patients have still not been obvious.
Serological studies of Polish strains confirmed that the studied strains possess various core types which is typical in the genus Proteus. Frequently, strains forming a common R serogroup do not belong to a common O serogroup and the strains classified into one O serogroup may differ in their core-region serospecificity6,11. Our studies showed a big serological diversity among Proteus spp. strains isolated recently from patients in central Poland. However, half of the isolates (299) including 18 strains reported before13,14,15,19 belong to 15 most numerous O serogroups, comprising ten or more studied strains (Fig. 5). O78 serogroup is the biggest one, formed by 61 studied strains (10.5% of 580 collected S strains). This serogroup together with O77 and O79 serogroups were described as new ones not long ago by Drzewiecka et al.13,14 and Arbatsky et al.15 and they currently include only the isolates from Poland. O50 serogroup, in turn, was reported in 200335 and has so far been represented by P. mirabilis strain TG 332 described earlier as being serologically unique36. O60 serogroup was also formed in 200337 for a non-clinical P. myxofaciens isolate from a gypsy larva. Lately, the species has been proposed to be excluded from the genus Proteus38. However, our results clearly indicate that O60 serotype exists among P. mirabilis and P. genomospecies clinical strains. The other 10 most prevalent serogroups have been included in the first classic serological scheme proposed for P. mirabilis and P. vulgaris bacteria9. What is interesting, the majority of these predominant serogroups had been previously reported as frequently found among hundreds of clinical P. mirabilis and P. vulgaris isolates from urine, faeces, blood, or unknown sources. Summarizing these data, Larsson10 indicated O3 serogroup as dominating in all reports and O10, O13, O26, O28, and O30 serogroups as the most prevalent ones. O6, O11, O23, O24, O27, and O29 serogroups were also widely distributed. Analyzing the serological properties of 99 Swedish and 24 Polish P. mirabilis strains from urinary tract infections, Kaca et al.12 also found O10 and O30 to be the most numerous serogroups. However, the authors applied only 20 Proteus O-specific sera in their studies so the attachment of the strains to the other prevalent serogroups (e.g. O6, O26, O28, or O29) was not analyzed. In our studies, some of the prevalent serogroups turned out to be multi-species (Table 3), including not only the ubiquitous P. mirabilis but also the other species. Three P. penneri isolates were classified into O10 serogroup (so far found mostly in O17, O61, O64, and O65 serogroups11,39 including also P. mirabilis and/or P. vulgaris strains7), several P. genomospecies strains were classified into O11, O60, O78, and O79 serogroups and two P. vulgaris isolates into O27 and O78 serogroups. In all the prevalent serogroups, the isolates from urine and/or wounds were most numerous and we could not see any relations between serotypes and sources of isolation.
O78, O16, and O11 serogroups seem to be heterogenous. Further chemical analysis may show the differences in the structures of O antigens, responsible for their slight serological variety observed within these serogroups and will allow the formation of new subserogroups or new cross-reacting O serogroups.
It can be seen that for many years, Proteus spp. strains belonging to O3, O6, O10, O11, O27, O28, and O30 serogroups have been most frequently isolated in many different countries. What is worth noticing, the Proteus O60 antigen structure resembles that of the Proteus O30 antigen7 so before the O60 serogroup was created in 200337, O60 isolates could be classified to O30 serogroup due to their mutual similarity and strong cross reactivity revealed in our work (data not shown). It should be noted that at present, O78 serogroup obviously seems to be the most prevalent among Polish patients from the Łódź region accounting for 10.5% of all S isolates, although its predominance is not big. The prevalence of the serotypes dominating over others may be connected with some features of their O antigens. However, it is difficult to indicate common structural O-PS features (Table 3) distinguishing the biggest serogroups from the smaller ones, e.g. the compounds present exclusively in the frequent O antigens and, simultaneously, absent in the rarely found O serotypes7. Among the 15 most numerous serotypes, both branched and linear O-PS repeating units can be found, which are built of three-to-five sugars, including glucose, galactose, and their derivatives frequently occurring in Proteus O-PSs. For example, the repeating unit of the most ubiquitous O78 antigen is composed of five different sugars and sugar derivatives. Three of them constitute the main chain and two form side branches. This antigen is not characterized by any unusual or unique structural feature. It shares disaccharide fragments with several Proteus O antigens, but no cross reactions have been noticed14. It is possible that the most prevalent Proteus O serotypes may be especially connected with some virulence factors, like it is observed e.g. in Vibrio cholerae O140 or with drug resistance, which is the case of P. mirabilis O78 (unpublished data).
Conclusion
In general, clinical Proteus spp. isolates from central Poland are characterized by high serological diversity and include the representatives of almost all described O serogroups. These results may suggest that either Proteus spp. strains do not intensively transmit from one patient to another or they are able to rapidly change their antigenic specificity by avoiding the immune response from host organisms, increasing their own virulence and adapting to environmental conditions. Such examples of antigenic variation are known in other Gram-negative genera and may be caused either by mutations in O antigen genes or by inter/intra-species lateral transfer of O antigen genes by homologous recombination, IS elements, plasmids, or bacteriophages41.
The genus Proteus is currently divided into 83 O serogroups8 and their number continually grows exceeding numbers of serogroups in many other Gram-negative bacteria like the genera: Shigella or Salmonella (each 46 O serogroups), Yersinia (~ 35 O serogroups), Citrobacter (43 O serogroups), Pseudomonas (~ 30 O serogroups), and others, except for Escherichia coli (~ 180 O serogroups) and Vibrio cholerae (~ 200 O serogroups)41,42. Despite the high serological diversity among Proteus bacilli, the results of the presented research confirm the persisting for many years predominance of some serogroups reported earlier10 and reveal new prevalent O serotypes (especially O78). The presence of the representatives of different Proteus species among these serogroups suggests that the bacteria acquire these special O phenotypes as a result of adaptation in convergence processes. Thus, these O antigens may be in some ways attractive and beneficial to the expressing bacteria. It will be reasonable to investigate a clonal homology of one-species isolates belonging to the respective predominating O serogroups. Their diversity would confirm the special role of a particular O-antigen type in their survival and virulence.
The appointment of the most virulent O serotypes among the Proteus spp. bacilli would allow developing methods, which might enable rapid detection and eradication of such strains and the prophylaxis of recurrent complicated UTIs and CAUTIs.
Data availability
The data and materials are available from the corresponding author on reasonable request.
References
Adeolu, M., Alnajar, S., Naushad, S. & Gupta, R. S. Genome-based phylogeny and taxonomy of the ‘Enterobacteriales’: Proposal for Enterobacterales ord. nov. divided into the families Enterobacteriaceae, Erwiniaceae fam. nov., Pectobacteriaceae fam. nov., Yersiniaceae fam. nov., Hafniaceae fam. nov., Morganellaceae fam. nov., and Budviciaceae fam. nov. Int. J. Syst. Evol. Microbiol. 66, 5575–5599 (2016).
Armbruster, C. E., Mobley, H. L. T. & Pearson, M. M. Pathogenesis of Proteus mirabilis infection. EcoSal Plus 8, 1–123 (2018).
Drzewiecka, D. Significance and roles of Proteus bacteria in natural environments. Microb. Ecol. 72, 741–758 (2016).
O’Hara, C. M. et al. Classification of Proteus vulgaris biogroup 3 with recognition of Proteus hauseri sp. nov., nom. rev. and unnamed Proteus genomospecies 4, 5 and 6. Int. J. Syst. Evol. Microbiol. 50, 1869–1875 (2000).
Janda, J. M., Abbot, S. L., Khashe, S. & Probert, W. Biochemical identification and characterization of DNA groups within the Proteus vulgaris complex. J. Clin. Microbiol. 39(4), 1231–1234 (2001).
Palusiak, A. Classification of Proteus penneri lipopolysaccharides into core region serotypes. Med. Microbiol. Immunol. 205, 615–624 (2016).
Knirel, Y. A. et al. Structure and serology of O-antigens as the basis for classification of Proteus strains. Innate Immunol. 17, 70–96 (2011).
Siwińska, M. et al. The unique structure of bacterial polysaccharides - immunochemical studies on the O antigen of Proteus penneri 4034–85 clinical strain classified into a new O83 Proteus serogroup. Int. J. Biol. Macromol. 163, 1168–1174 (2020).
Kauffmann, F. Proteus. In The Bacteriology of Enterobacteriaceae (ed. Kauffmann, F.) 333–360 (Munksgaard, Copenhagen, 1966).
Larsson, P. Serology of Proteus mirabilis and Proteus vulgaris. Methods Microbiol. 14, 187–214 (1984).
Drzewiecka, D., Zych, K. & Sidorczyk, Z. Characterization and serological classification of a collection of Proteus penneri clinical strains. Arch. Immunol. Ther. Exp. 52, 121–128 (2004).
Kaca, W. et al. Serotyping of Proteus mirabilis clinical strains based on lipopolysaccharide O polysaccharide and core oligosaccharide structures. Biochem. Mosc. 76(7), 851–861 (2011).
Drzewiecka, D. et al. Structure and serological properties of the O-antigen of two clinical Proteus mirabilis strains classified into a new Proteus O77 serogroup. FEMS Immunol. Med. Microbiol. 54, 185–194 (2008).
Drzewiecka, D. et al. Structural and serological studies of the O-polysaccharide of strains from a newly created Proteus O78 serogroup prevalent in Polish patients. FEMS Immunol. Med. Microbiol. 58, 269–276 (2010).
Arbatsky, N. P. et al. Structure of a Kdo-containing O polysaccharide representing Proteus O79, a newly described serogroup for some clinical Proteus genomospecies isolates from Poland. Carbohydr. Res. 379, 100–105 (2013).
Siwińska, M. et al. Classification of a Proteus penneri clinical isolate with a unique O-antigen structure to a new Proteus serogroup, O80. Carbohydr. Res. 407, 131–136 (2015).
Zabłotni, A., Arbatsky, N. P., Drzewiecka, D., Shashkov, A. S. & Knirel, Y. A. Chemical characterization and serological properties of a unique O-polysaccharide of the Proteus mirabilis Sm 99 clinical strain - identification of a new, O81, serotype. Int. J. Biol. Macromol. 118, 1131–1135 (2018).
Siwińska, M. et al. Structural and serological characterization of the O82 antigen of a Proteus mirabilis strain isolated from a patient in Poland. Carbohydr. Res. 486, 107831 (2019).
Drzewiecka, D., Arbatsky, N. P., Kondakova, A. N., Shashkov, A. S. & Knirel, Y. A. Structures and serospecificity of threonine-containing O polysaccharides of two clinical isolates belonging to the genus Proteus and their classification into O11 subserogroups. J. Med. Microbiol. 65(11), 1260–1266 (2016).
Drzewiecka, D., Shashkov, A. S., Arbatsky, N. P. & Knirel, Y. A. Immunochemical characterization of the O antigens of two Proteus strains, O8-related antigen of Proteus mirabilis 12 B-r and O2-related antigen of Proteus genomospecies 5/6 12 B-k, infecting a hospitalized patient in Poland. Microbiology 162, 789–797 (2016).
Senior, B. W. Media and tests to simplify the recognition and identification of members of the Proteeae. J. Med. Microbiol. 46, 39–44 (1997).
Lüderitz, O., Westphal, O., Staub, A. M. & Nikaido, H. Isolation and chemical and immunological characterization of bacterial lipopolysaccharides. In Bacterial Endotoxins. A Comprehensive Treatise (eds Weinbaum, G. et al.) 145–233 (Academic Press, INC, Cambridge, 1971).
Wilkerson, M. L. & Niederhoffer, E. C. Swarming characteristics of Proteus mirabilis under anaerobic and aerobic conditions. Anaerobe 1, 345–350 (1995).
Westphal, O. & Jann, K. Bacterial lipopolysaccharides. Extraction with phenol-water and further applications of the procedure. Methods Carbohydr. Chem. 5, 83–89 (1965).
Sidorczyk, Z. et al. Structure of the O-polysaccharide and classification of Proteus mirabilis G1 in Proteus serogroup O3. Eur. J. Biochem. 269, 1406–1412 (2002).
Palusiak, A. The antigens contributing to the serological cross-reactions of Proteus antisera with Klebsiella representatives. Mol. Immunol. 64, 228–234 (2015).
Kim, B.-N. et al. Bacteraemia due to tribe Proteeae: A review of 132 cases during a decade (1991–2000). Scand. J. Infect. Dis. 35, 98–103 (2003).
Drzewiecka, D. & Sidorczyk, Z. Characterization of Proteus penneri species—human opportunistic pathogens. Post. Mikrobiol. 44, 113–126 (2005) (in Polish).
Palusiak, A. Immunochemical properties of Proteus penneri lipopolysaccharides—one of the major Proteus sp. virulence factors. Carbohydr. Res. 380, 16–22 (2013).
Dai, H. et al. Multilocus sequence analysis for the taxonomic updating and identification of the genus Proteus and reclassification of Proteus genospecies 5 O’Hara et al. 2000, Proteus cibarius Hyun et al. 2016 as later heterotypic synonyms of Proteus terrae Behrendt et al. 2015. BMC Microbiol. 20, 152 (2020).
Kwil, I., Kaźmierczak, D. & Różalski, A. Swarming growth and resistance of Proteus penneri and Proteus vulgaris strains to normal human serum. Adv. Clin. Exp. Med. 22(2), 165–175 (2013).
Diep, B. et al. Salmonella serotyping; comparison of the traditional method to a microarray-based method and an in silico platform using whole genome sequencing data. Front. Microbiol. 10, 2554 (2019).
Shelenkov, A. et al. Multidrug-resistant Proteus mirabilis strain with cointegrate plasmid. Microorganisms 8, 1775 (2020).
Yu, X. et al. Genetic diversity of the O antigens of Proteus species and the development of a suspension array for molecular serotyping. PloS ONE 12(8), e0183267 (2017).
Kołodziejska, K. et al. Structure of the O-polysaccharide of a serologically separate strain of Proteus mirabilis, TG 332, from a new proposed Proteus serogroup O50. Carbohydr. Res. 338(20), 2105–2109 (2003).
Penner, J. L. & Hennessy, J. N. Separate O-grouping schemes for serotyping clinical isolates of Proteus mirabilis and Proteus vulgaris. J. Clin. Microbiol. 12, 304–309 (1980).
Sidorczyk, Z. et al. Structure of the O-polysaccharide from Proteus myxofaciens. Classification of the bacterium into new Proteus O serogroup. Eur. J. Biochem. 270, 3182–3188 (2003).
Giammanco, G. M. et al. Phylogenetic analysis of the genera Proteus, Morganella, and Providencia by comparison of rpoB gene sequence of type and clinical strains suggests the reclassification of Proteus myxofaciens in a new genus, Cosenzaea gen. nov., as Cosenzaea myxofaciens comb. nov. Int. J. Syst. Evol. Microbiol. 61, 1638–1644 (2011).
Sidorczyk, Z. et al. Structural and serological characterization of the lipopolysaccharide from Proteus penneri 20 and classification of the cross-reacting Proteus penneri strains 10, 16, 18, 20, 32 and 45 in Proteus serogroup O17. Arch. Immunol. Ther. Exp. 50, 345–350 (2002).
Tulatorn, S., Preeprem, S., Vuddhakul, V. & Mittraparp-arthorn, P. Comparison of virulence gene profiles and genomic fingerprints of Vibrio cholerae O1 and non-O1/non-O139 isolates from diarrheal patients in southern Thailand. Trop. Med. Health 46, 31 (2018).
Wang, L., Wang, Q. & Reeves, P. R. The variation of O-antigens in gram-negative bacteria. In Endotoxins: Structure, Function and Recognition (eds Wang, X. & Quinn, P. J.) 123–152 (Springer, Dordrecht, 2010).
Knirel, Y. A. Structure of O-antigens. In Bacterial lipopolysaccharides. Structure, Chemical Synthesis, Biogenesis and Interaction with Host Cells (eds Knirel, Y. A. & Valvano, M. A.) 41–116 (Springer, Wien, 2011).
Acknowledgements
This work was financially supported by grant no. N N401 020135 from the Ministry of Science and Higher Education (Poland). We thank medical laboratories in Łódź (Poland): in Barlicki Hospital, in Biegański Hospital, “Synevo”, “Diagnostyka” for kindly providing the studied Proteus spp. strains.
Author information
Authors and Affiliations
Contributions
D.D. led the project and acquired the funding. All the authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by all the authors. The first draft of the manuscript was written by D.D., detailed description of methods by A.P., and all the authors commented on the previous versions of the manuscript, read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Drzewiecka, D., Palusiak, A., Siwińska, M. et al. The prevailing O serogroups among the serologically differentiated clinical Proteus spp. strains in central Poland. Sci Rep 11, 18982 (2021). https://doi.org/10.1038/s41598-021-98228-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98228-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.