Abstract
The presence or absence of autoantibodies against citrullinated proteins (ACPAs) distinguishes two main groups of rheumatoid arthritis (RA) patients with different etiologies, prognoses, disease severities, and, presumably, disease pathogenesis. The heterogeneous responses of RA patients to various biologics, even among ACPA-positive patients, emphasize the need for further stratification of the patients. We used high-density protein array technology for fingerprinting of ACPA reactivity. Identification of the proteome recognized by ACPAs may be a step to stratify RA patients according to immune reactivity. Pooled plasma samples from 10 anti-CCP-negative and 15 anti-CCP-positive RA patients were assessed for ACPA content using a modified protein microarray containing 1631 different natively folded proteins citrullinated in situ by protein arginine deiminases (PADs) 2 and PAD4. IgG antibodies from anti-CCP-positive RA plasma showed high-intensity binding to 87 proteins citrullinated by PAD2 and 99 proteins citrullinated by PAD4 without binding significantly to the corresponding native proteins. Curiously, the binding of IgG antibodies in anti-CCP-negative plasma was also enhanced by PAD2- and PAD4-mediated citrullination of 29 and 26 proteins, respectively. For only four proteins, significantly more ACPA binding occurred after citrullination with PAD2 compared to citrullination with PAD4, while the opposite was true for one protein. We demonstrate that PAD2 and PAD4 are equally efficient in generating citrullinated autoantigens recognized by ACPAs. Patterns of proteins recognized by ACPAs may serve as a future diagnostic tool for further subtyping of RA patients.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a systemic autoimmune disease characterized by chronic inflammation of the joints and synovial tissue inflammation, leading to pain, swelling, bone erosion, and disability1. Approximately two-thirds of RA patients produce anti-citrullinated protein antibodies (ACPAs)2,3. These autoantibodies may be present years before the onset of clinical symptoms, underlining their possible involvement in the pathogenesis of early RA and may serve as early biomarkers4,5. Anti-CCP-positive and anti-CCP-negative RA can be regarded as two disease entities with different predisposing factors, etiology, disease severity, prognosis, and presumably pathogenesis6,7.
The conversion of peptidyl-arginine into peptidyl-citrulline, commonly known as protein citrullination or arginine deimination, is a posttranslational modification of proteins catalyzed by protein arginine deiminases (PADs). In mammals, five isoforms of PAD differ in tissue distribution and localization within cells: PAD1–4 and PAD68. In particular, PAD2 and PAD4 are relevant to RA due to their expression in macrophages and neutrophils present in the synovial membrane of RA patients9. Their efficiency, relative to each other, in generating citrullinated neoepitopes recognized by ACPAs is not clear10,11,12. Citrullination is central to multiple regulatory cellular functions, such as cell differentiation, apoptosis, gene regulation, and inflammation13. Evidence is accumulating for a central role of citrullination in the pathogenesis of several diseases in addition to RA, including multiple sclerosis, Alzheimer’s disease, and cancers14,15,16.
The clinical presentation of RA varies considerably from patient to patient. In addition, the patients respond differently to various drugs. There is therefore an urgent need for the identification of new diagnostic tools to aid in patient stratification for precision medicine17,18. Characterization of ACPA autoantibody reactivity may provide new insight in this respect19,20,21. We have previously investigated the reactivity of autoantibodies against native proteins in RA patients and healthy subjects, demonstrating insignificant levels of autoantibody reactivity in especially healthy subjects for which intensities were significantly lower than both anti-CCP-positive and anti-CCP-negative RA patient samples against unmodified proteins20. Utilizing the high-throughput capacity of protein microarrays, we performed an exploratory study quantifying the binding of autoantibodies in plasma pools from well-characterized RA patients to more than 1600 different human proteins in citrullinated and non-citrullinated forms.
Results
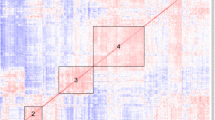
We examined the binding of IgG antibodies in pools of plasma from anti-CCP-positive and anti-CCP-negative RA patients to microarrays containing 1631 human proteins in native form or citrullinated on-slide using PAD2 or PAD4 as catalysts. Figure 1 shows the staining intensity of individual arrays. Data from Fig. 1C,F have previously been published20. The PAD enzyme efficiency was tested on fibrinogen and is shown in Supplementary Dataset 1.
Imaging of autoantibody binding to citrullinated and non-citrullinated protein arrays. Pooled plasma from 15 anti-CCP-positive RA patients or 10 anti-CCP-negative RA patients was diluted 1:200 and added to microarray plates containing 1631 human proteins that had been citrullinated by PAD2 or PAD4 or kept in native form. The binding of IgG antibodies was visualized using Cy3-labelled rabbit anti-human IgG antibodies. (A) Slide with proteins citrullinated by PAD2 and incubated with anti-CCP-positive plasma. (B) Proteins citrullinated by PAD4 incubated with anti-CCP-positive plasma. (C) Native proteins incubated with anti-CCP-positive plasma. (D) Proteins citrullinated by PAD2 incubated with anti-CCP-negative plasma. (E) Proteins citrullinated by PAD4 incubated with anti-CCP negative plasma (F). Native proteins incubated with anti-CCP-negative plasma. (C,F) have previously been published20.
Broad reactivity by low-intensity autoantibodies
We observed low reactivity of IgG antibodies against a large number of citrullinated proteins but not against the corresponding native proteins. After incubation with a pool of anti-CCP-positive plasma, 632 proteins showed more than twofold higher binding of IgG after citrullination with PAD2 than in their native form, and the corresponding number was 629 proteins after citrullination with PAD4, suggesting that these proteins were recognized by ACPAs (Fig. 2, Supplementary Dataset 2).
Quantitative analysis of arrayed proteins recognized by autoantibodies. Bar chart showing the number of proteins recognized by autoantibodies to a higher degree than native proteins. Plasma from anti-CCP-positive or anti-CCP-negative RA patients was incubated with Immunome protein microarray slides containing native proteins or proteins citrullinated by PAD2 or PAD4. The number above the bars indicates the number of proteins recognized by autoantibodies under the given conditions (defined as more than two-fold differences in fluorescence intensity compared to native proteins, an intraprotein CV < 15, and a P value < 0.05). Specific targets for autoantibodies are shown in Supplementary Dataset 2.
Surprisingly, citrullination also enhanced the binding of IgG autoantibodies to a significant number of proteins when the array was incubated with the anti-CCP-negative plasma pool. This was true for 408 proteins after citrullination with PAD2 and 133 proteins after citrullination with PAD4 (Fig. 2, Supplementary Dataset 2).
PAD2 and PAD4 showed strikingly similar efficiency in generating epitopes recognized by ACPAs. Thus, only one protein, minichromosome maintenance complex-binding protein (C10orf119), was targeted to a higher degree (PAD2/PAD4 ratio: 2.7) by antibodies from anti-CCP-positive plasma when citrullinated by PAD2 compared to PAD4, while only four proteins were targeted to a higher degree when citrullinated by PAD4 (PAD4/PAD2 ratio: approximately 2): PC4 and SFRS1-interacting protein (PSIP1), nucleosome assembly protein 1-like 1 (NAP1L1), protein S100-P (S100P), and nucleosome assembly protein 1-like 4 (NAP1L4).
We also found but few differences between IgG antibody binding to PAD2- and PAD4-citrullinated proteins when the protein array was incubated with the anti-CCP negative plasma pool. Three proteins were targeted to a higher degree when citrullinated by PAD2 than by PAD4 (PAD2/PAD4 ratio: approximately 3): caspase recruitment domain-containing protein 9 (CARD9), 3-phosphoinositide-dependent protein kinase 1 (PDPK1), and protein kinase C and casein kinase substrate in neurons protein 3 (PACSIN3). Only one protein was targeted to a lower degree when citrullinated by PAD2: protein CBFA2T3 (ratio PAD2-citrullinated/PAD4-citrullinated: approximately 0.3).
We did not identify native proteins that were targeted by autoantibodies to a higher degree in the native form than in the citrullinated form. We found a total of 844 citrullinated proteins recognized by ACPAs from RA patients. A list of all identified antigens can be found in Supplementary Dataset 2.
Binding pattern of autoantibodies from anti-CCP-positive patients
Many of the proteins identified as targets for ACPAs above showed low-intensity staining for IgG antibodies. Proteins that are autoantigens in vivo can be expected to show staining with high intensity; however, to identify proteins that may be autoantigens in vivo, we limited the analysis to include only proteins with z scores > 2 (Tables 1, 2).
After incubation of the arrayed proteins with the anti-CCP-positive plasma pool, two well-established autoantigens in RA fulfilled this criterion: vimentin and keratin 8. For both proteins, the binding of IgG autoantibodies increased markedly when they were citrullinated by PAD4 compared to native proteins, while the same only applied to keratin 8 after citrullination with PAD2 (Table 1). Irrespective of whether PAD2 or PAD4 was used for citrullination, more antibody binding was observed after incubation with the anti-CCP-positive plasma pool than after incubation with the anti-CCP-negative plasma pool (Table 2).
The proteins that showed the greatest increase in autoantibody capture after citrullination with PAD2 compared to native proteins were interferon-induced 35 kDa protein (IRF5; 29.5-fold increase after citrullination), cas scaffolding protein family member 4 (CASS4; 15.4-fold increase), and endophilin-A2 (SH3GL1; 6.5-fold increase). The proteins with the greatest change in autoantibody capture after citrullination with PAD4 were IRF5 (34.7-fold increase), double-stranded RNA-binding protein Staufen homolog 1 (STAU1; 20.0-fold increase), and melanoma-associated antigen B1 (MAGEB1; 10.1-fold increase).
Binding pattern of autoantibodies from anti-CCP-negative patients
We next examined the binding of autoantibodies contained in the plasma pool from anti-CCP-negative patients to citrullinated and native proteins. Even after exclusion of proteins with z scores < 2, we identified several proteins that showed increased IgG autoantibody binding after citrullination. This applied to 29 proteins after citrullination by PAD2 and 26 proteins after citrullination by PAD4 (Table 1).
Comparison between anti-CCP-positive and anti-CCP-negative plasma
Finally, we examined the binding of IgG autoantibodies to the protein array after incubation with the anti-CCP-positive versus the anti-CCP-negative plasma pool (Table 2). When PAD2 was used for citrullination, 91 proteins showed more than twofold higher binding of autoantibodies when incubated with anti-CCP-positive plasma than with anti-CCP-negative plasma. After citrullination with PAD4, the corresponding number was 98 proteins. The most significant differences were observed for calcium-regulated heat-stable protein 1 (CARHSP1, ratio anti-CCP-positive plasma/anti-CCP-negative: 12.5), macrophage migration inhibitory factor (MIF; ratio 10.9), and keratin type II cytoskeletal 8 (KRT8; ratio 9.9) when PAD2 was used for citrullination. When PAD4 was used for citrullination, the greatest anti-CCP-positive/anti-CCP-negative ratios were observed for calcium-regulated heat-stable protein 1 (CARHSP1, ratio 13.3), acetyl-CoA acetyltransferase (ACAT2, ratio: 12.7), and protein E6 (E6, ratio 12.4).
Discussion
We performed a high-throughput high-density protein microarray analysis on pools of plasma from 15 anti-CCP-positive and 10 anti-CCP-negative RA patients to identify proteins recognized by IgG autoantibodies before and after citrullination. The method proved successful, and we provide here a list of 844 out of 1631 arrayed proteins that were recognized by autoantibodies after citrullination, i.e. recognized by ACPAs. To our knowledge, this is the largest number of proteins identified as potential targets of ACPAs to date. Previous studies have used other types of citrullinated protein arrays to investigate ACPA reactivity but have focused on a single or fewer citrullinated proteins, usually on known RA antigens such as vimentin, fibrinogen, and alpha-enolase or used processed sample material11,22,23,24,25,26,27,28,29. This is the first investigation of autoantibody reactivity against citrullinated proteins on the KREX protein array platform using pure plasma samples from RA patients that we are aware of. Although we demonstrate here that more than 800 proteins can be recognized by ACPAs, they are not necessarily autoantigens in vivo, where several requirements must be met for citrullination to occur: the protein must localize to the same compartment as PAD2 or PAD4 and requirements to pH level, reducing conditions and calcium concentration should be met30,31,32,33. More research is needed to clarify which of the proteins shown to bind ACPAs under the optimal conditions used here in vitro also do so in vivo and elaboratory validation experiments are critical in this regard.
Per se, the high numbers of identified ACPA targets suggest that PAD enzymes are promiscuous in generating citrullinated neoepitopes recognized by ACPAs. On the other hand, approximately half of the proteins in the protein array used here were not recognized by ACPA, suggesting either that those proteins lack surface-exposed arginine residues or that they lack citrullination motifs for PADs.
Many of the abovementioned proteins that bound IgG autoantibodies showed low staining intensity. ACPAs appear to consist of a pool of either specific or cross-reactive antibodies, and it can be speculated that the low staining intensity is a result of cross-reactive antibodies34. The literature on monoclonal ACPAs shows extensive cross-reactivity, especially if glycine is present in the + 1 position of citrulline35,36. This fact may be important to consider in any multiplex ACPA assay using on-array citrullination so that there is complete control of which epitopes are citrullinated and which are not. Proteins that are potential autoantigens in vivo are likely to have relatively high affinity and/or concentrations, so in an effort to narrow down the list to potential genuine autoantigens, we implemented an additional filtration using z score (cut-off > 2) that excluded low-intensity antigens. Approximately 100 proteins in anti-CCP-positive plasma were identified. Among them was vimentin, a well-known autoantigen in RA. Other proteins showed strong increases in IgG binding intensity after citrullination, e.g., IRF5, CASS4, SH3GL1, and STAU1. Further studies are needed to determine whether the citrullinated forms of these proteins contain T-cell epitopes in addition to being targeted by ACPAs.
Interestingly, we also identified a rather large number of proteins recognized by autoantibodies from anti-CCP-negative individuals. This has been shown several times before and may demonstrate a subgroup of RA patients not identified using traditional serological testing37,38,39. Furthermore, this supports the conclusion of Wagner and colleagues that the commonly used commercial anti-CCP assays fail to identify some ACPA-positive RA patients (at least 10% in the authors setup)40. ACPA-positive and ACPA-negative RA have quite different pathogenesis6,7, and when future treatment targeting ACPA-positive RA specifically (e.g., PAD inhibitors) becomes available, protein arrays such as the one employed here may discriminate ACPA-positive and ACPA-negative RA better than the anti-CCP test. Another explanation why we identify several proteins recognized by autoantibodies from anti-CCP negative patients may be due to the implication of citrullination and not the citrullinated epitope. As already mentioned, the citrullination process results in conformational changes of the proteins which may lead to recognition of unmodified proteins from the anti-CCP negative patient pool and not necessarily recognition of the citrullinated epitope.
The relative efficiency of PAD2 and PAD4 in generating epitopes recognized by ACPAs has been a matter of some controversy. One study showed that at high antibody titers (1:250 and 1:1000) but not low titers (1:40 and 1:100), ACPAs preferentially bind to fibrinogen citrullinated by PAD4, while we have previously reported that PAD2 and PAD4 are equally efficient in generating epitopes for the binding of ACPAs to fibrinogen and alpha-enolase10,11. In a similar setup, we previously showed that PAD4 was the dominant isoform in generating ACPA-binding sites in histone H311. At the serum dilution used in the present study (1:200), the staining IgG ACPAs was equally intense when proteins were citrullinated by PAD2 and PAD4, except for only four proteins out of 1631 proteins.
The protein array methodology to investigate posttranslationally modified epitopes may not only be relevant for RA but may also be used in diseases where autoantibodies against other modified proteins have been shown, such as oxidized proteins in type 1 diabetes or autoantigens phosphorylated during stress-induced apoptosis in systemic lupus erythematosus5,41,42. Furthermore, it may be relevant to investigate at risk individuals to compare citrullination profiles or investigate other PAD enzymes such as the P. gingivalis PAD enzyme, which has been proposed to trigger RA even though conflicting studies exist43,44.
A limitation to the current study is that the Immunome protein arrays were not specifically enriched for antigens of particular relevance for RA, i.e. proteins that are present in joints or proteins that have previously been identified as autoantigens in RA, although numerous prominent ribonuclear proteins and other well-known autoantigens are present on the arrays. The development of focused arrays containing such proteins would be a natural next step. Another limitation is the use of plasma pools rather than individual plasma samples. Using individual samples, we could compare specific clinical phenotypes to autoantibody patterns or demonstrate the potential of subdifferentiation of patients based on their autoantibody profile45,46,47,48. This first study of its kind was merely a proof-of-concept study; it proves that further development of the technique is warranted.
Conclusion
We present a list of 844 citrullinated proteins recognized by ACPAs from RA patients. We demonstrate that PAD2 and PAD4 are equally efficient at generating binding sites for ACPAs. We present a list of approximately 100 potential autoantigens in RA, and we suggest that the pattern of autoantibody recognition may form a basis for subgrouping of anti-CCP-positive RA patients and anti-CCP-negative patients that rightfully should be considered ACPA-positive. The next steps in the development of the technique should be the production of arrays with RA-associated antigens and comparison of ACPA reactivity patterns with clinical phenotypes.
Materials and methods
Collection of patient plasma
Plasma samples were obtained from 10 anti-CCP-negative RA patients and 15 anti-CCP-positive RA patients. Patient data can be seen in Table 3. Plasma from anti-CCP-negative and anti-CCP-positive RA patients was pooled separately before protein array analysis. Individual patient response data have previously been published, and we have previously used the same patient cohorts in another study to investigate autoantibody reactivity against native autoantigens11,20. RA patients fulfilled the American College of Rheumatology and European League Against Rheumatism criteria for the diagnosis of RA49. Plasma was isolated from peripheral venous blood and drawn into BD Vacutainers containing EDTA (BD, Plymouth, UK). The use of patient samples was approved by the local ethics committee of the Institute of Rheumatology in Prague, Czech Republic, and written informed consent was obtained from all patients before initiation of the study (June 26, 2012, No. 3294/2012). All methods were performed according to relevant guidelines and regulations and in accordance with the Declaration of Helsinki.
Sample preparation for protein array analysis
The Immunome (v1) protein microarray (Sengenics, Singapore) consists of 1631 proteins, in addition to several control proteins, spotted in quadruplicates, allowing assessment of spot-to-spot variation and across-slide variation in background intensity (Fig. 3A). The microarray consists of a variety of different proteins representing different categories, such as cancer-associated antigens, transcription factors, kinases, and other proteins involved in inflammation and cell signaling (Fig. 3B).
Immunome slide design and protein categories on the protein microarray. (A) The Immunome protein microarray consists of four identical subarrays, each containing 1631 different proteins in addition to 11 control proteins (BCCP, BSA, Cy3BSA, IgA, IgG, IgM, and four different control probes for the BCCP tag acting as negative controls). The control proteins are located between the subarrays. (B) The proteins spotted on the microarray represent different protein groups, such as cancer-associated antigens, transcription factors, kinases, and signaling proteins. The number of proteins in each category is shown. BCCP biotin carboxyl carrier protein, BSA bovine serum albumin.
Each protein in the array is coupled to a biotin carboxyl carrier protein tag, which ensures correct three-dimensional folding during expression. Four slides were carefully transferred to different quadriperm chambers (Greiner BioOne, Kremsmünster, Austria) containing different citrulline reaction buffers consisting of 1.2 µg/mL recombinant human PAD2 or PAD4 (Cayman Chemicals, Ann Arbor, MI, USA); 1 mM 1,4-dithiothreitol (DTT), 10 mM CaCl, and 100 mM Tris–HCl and incubated at 37 °C for 3 h while shaking under horizontal rotation at 50 rpm (IKA, Germany, Königswinter). The slides were washed two times using cold serum albumin buffer (SAB) containing 0.1% Triton X-100 and 0.1% bovine serum albumin (BSA) in phosphate-buffered saline (PBS) and placed in a new quadriperm chamber. Additionally, two slides following the same procedure, but without the addition of PAD enzymes, were used.
Four milliliters of diluted pooled plasma (1:200) from anti-CCP-positive or anti-CCP-negative RA patients was added to the new chambers and incubated at 20 °C for 2 h at 50 rpm. The slides were washed using SAB buffer and added to a new quadriperm chamber. The binding of IgG antibodies was detected using Cy3-conjugated (GE Healthcare, Chicago, Ill, USA) polyclonal rabbit anti-human IgG (Dako, Santa Clara, CA, USA) diluted 1:1000 (v/v) in SAB buffer. The slides were covered in tinfoil and incubated at 20 °C for 2 h at 50 rpm. Finally, the slides were washed twice in SAB buffer and three times in ultrapure water followed by centrifugation at 240g for 5 min to dry the slides. Slides were stored at room temperature and scanned within 24 h.
Protein array imaging
The intensity of the individual spots was measured using a microarray laser scanner (Innoscan 710AL, Innopsys, Carbonne, France) using Mapix software (Ver. 8.2.2, Innopsys). The scan settings were as follows: 532 nm laser with low laser power (5 V), PMT gain at 60%, 5 µm resolution, and a scan speed of 35 px/s. Spotxel (SICASYS ver. 1.7.6) was used to automatically annotate each protein on the slide. Semiautomatic array alignment was used to specify the location of each spot. The median pixel intensity for each spot was used to eliminate the effect of outliers. Background intensity levels were extracted from the intensity of the adjacent spot. The data were exported as CSV files, and further data analysis was performed in R (Ver. 1.1.456, R Core Team).
Protein array quantitation data analysis
Raw intensities were normalized using a combination of quantile and intensity-based normalization50. Based on the normalized intensity levels, a z score, percent coefficient of variation (CV%), and Chebyshev inequality precision (CI-P) were calculated for each protein. An intraprotein CV% cutoff of < 15 was applied to ensure high reproducibility between the same protein spots (n = 4) on each microarray and to demonstrate an equal degree of citrullination. A CI-P cutoff of < 0.05 was applied to ensure that the identified intensities did not belong to the negative control distribution. We applied a z score with a cutoff of > 2 to discard low RFU intensities. Two-sample t tests with Benjamini–Hochberg FDR were performed to identify any statistically significant changes between the positive spots and the corresponding spots on the other slides. Finally, ratios for the statistically significantly changed expressions were calculated, and fold differences below 2 were discarded.
Mass spectrometry sample preparation
Fibrinogen (Cayman Chemical) was incubated for 3 h at 37 °C in citrulline reaction buffer containing 1.2 µg/mL PAD2 or PAD4 (Cayman Chemicals), 1 mM DTT, 10 mM CaCl, and 100 mM Tris–HCl to citrullinate fibrinogen. Digestion of fibrinogen (Cayman Chemical) was performed using filter-aided sample preparation51. Briefly, samples were transferred to Amicon Ultra 0.5 Centrifugal filters 10 kDa (Merck Millipore, MA, USA) containing 0.5% SDC in 50 mM triethylammonium bicarbonate (TEAB) buffer were centrifuged at 14,000g for 15 min. Next, the samples were reduced and alkylated by incubating in 10 mM tris(2-carboxyethyl)phosphine hydrochloride and 50 mM chloroacetamide for 30 min at 37 °C. Samples were washed in 0.5% sodium deoxycholate in 50 mM TEAB, and each wash was followed by centrifugation at 14,000g for 15 min at 20 °C. Next, samples were digested using 1 µg trypsin/100 µg sample protein in 0.5% SDC in TEAB and incubated overnight at 37 °C. Peptides were eluted by centrifugation at 14,000g for 15 min followed by the addition of 200 µl TEAB buffer and another centrifugation step. Next, the peptides were isolated by phase separation using ethyl acetate and acidified by trifluoroacetic acid. Phase separation was repeated two times, and the aqueous phase containing the peptides was recovered. All samples were dried down and stored at − 20 °C until the time of analysis.
Ultra-performance liquid chromatography tandem mass spectrometry
Fibrinogen samples were rehydrated in 2% acetonitrile and 0.1% formic acid. Protein concentration was measured using a DeNovix spectrophotometer DS-11 FX+ (DeNovix, Wilmington, Del, USA), and 0.4 µg was loaded per sample. Peptides were separated by reverse-phase liquid chromatography on a UPLC system (Dionex RSLX, Thermo Scientific), ionized by a nanoelectrospray ion source (CaptiveSpray, Bruker Daltonics), and analyzed using a timsTOF PRO mass spectrometer (Bruker Daltonics, Bremen, Germany). Samples were injected directly onto a C18 reversed-phase column (IonOpticks, 25 cm × 75 µm ID, 1.6 µm C18) kept at 40 °C. The peptides were eluted with a constant flow rate of 400 nL/min using solvent A (0.1% formic acid in water) and solvent B (acetonitrile with 0.1% formic acid) with a total runtime of 60 min. The gradient was as follows: 0–16 min at 2% B, 16–45 min at 5% B, 45–48 at 35% B, 48–52 min at 95% B, 52–60 min at 2% B. Raw files were loaded into PEAKS (Bioinformatics Solution Inc, v. 10.5) and followed the standard analysis pipeline with the addition of citrulline as a variable modification.
Ethics approval and consent to participate
The use of patient samples was approved by the local ethics committee of the Institute of Rheumatology in Prague, Czech Republic, and written informed consent was obtained from all patients before initiation of the study (June 26, 2012, No. 3294/2012).
Data availability
The microarray raw data are available from the corresponding author on reasonable request. The mass spectrometry proteomics data generated during the current study are available from the ProteomeXchange Consortium via the partner repository with the dataset identifier PXD02495552.
Abbreviations
- RA:
-
Rheumatoid arthritis
- ACPA:
-
Anti-citrullinated protein antibody
- PAD:
-
Protein arginine deiminase
- anti-CCP:
-
Anti-cyclic citrullinated peptide
- CV%:
-
Percent coefficient of variation
- CI-P:
-
Chebyshev inequality precision
- BCCP:
-
Biotin carboxyl carrier protein
References
Arend, W. P. & Firestein, G. S. Pre-rheumatoid arthritis: Predisposition and transition to clinical synovitis. Nat. Rev. Rheumatol. 8(10), 573–586 (2012).
Schellekens, G. A., de Jong, B. A., van den Hoogen, F. H., van de Putte, L. B. & van Venrooij, W. J. Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J. Clin. Investig. 101(1), 273–281 (1998).
Schellekens, G. A. et al. The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum. 43(1), 155–163 (2000).
Nielen, M. M. J. et al. Specific autoantibodies precede the symptoms of rheumatoid arthritis: A study of serial measurements in blood donors. Arthritis Rheum. 50(2), 380–386. https://doi.org/10.1002/art.20018 (2004).
Tracy, A., Buckley, C. D. & Raza, K. Pre-symptomatic autoimmunity in rheumatoid arthritis: When does the disease start?. Semin. Immunopathol. 39(4), 423–435. https://doi.org/10.1007/s00281-017-0620-6 (2017).
Seegobin, S. D. et al. ACPA-positive and ACPA-negative rheumatoid arthritis differ in their requirements for combination DMARDs and corticosteroids: Secondary analysis of a randomized controlled trial. Arthritis Res. Ther. 16(1):R13. http://arthritis-research.com/content/16/1/R13 (2014).
van der Helm-van Mil, A. H. M., Verpoort, K. N., Breedveld, F. C., Toes, R. E. M. & Huizinga, T. W. J. Antibodies to citrullinated proteins and differences in clinical progression of rheumatoid arthritis. Arthritis Res. Ther. 7(5), R949–R958. https://doi.org/10.1186/ar1767 (2005).
Vossenaar, E. R., Zendman, A. J. W., van Venrooij, W. J. & Pruijn, G. J. M. PAD, a growing family of citrullinating enzymes: Genes, features and involvement in disease. BioEssays 25(11), 1106–1118 (2003).
Foulquier, C. et al. Peptidyl arginine deiminase type 2 (PAD-2) and PAD-4 but not PAD-1, PAD-3, and PAD-6 are expressed in rheumatoid arthritis synovium in close association with tissue inflammation. Arthritis Rheum. 56(11), 3541–3553 (2007).
Blachère, N. E. et al. High-titer rheumatoid arthritis antibodies preferentially bind fibrinogen citrullinated by peptidylarginine deiminase 4. Arthritis Rheumatol. 69(5), 986–995. https://doi.org/10.1002/art.40035 (2017).
Damgaard, D. et al. Relative efficiencies of peptidylarginine deiminase 2 and 4 in generating target sites for anti-citrullinated protein antibodies in fibrinogen, alpha-enolase and histone H3. Pizzo S V, editor. PLoS One 13(8), 0203214. https://doi.org/10.1371/journal.pone.0203214 (2018).
van Beers, J. J. et al. Mapping of citrullinated fibrinogen B-cell epitopes in rheumatoid arthritis by imaging surface plasmon resonance. Arthritis Res. Ther. 12(6), R219. https://doi.org/10.1186/ar3205 (2010).
Willis, V. C. et al. Protein arginine deiminase 4 inhibition is sufficient for the amelioration of collagen-induced arthritis. Clin. Exp. Immunol. 188(2), 263–274 (2017).
Moscarello, M. A. et al. Inhibition of peptidyl-arginine deiminases reverses protein-hypercitrullination and disease in mouse models of multiple sclerosis. Dis. Model Mech. 6(2), 467–478. https://doi.org/10.1242/dmm.010520 (2013).
Mohanan, S. et al. Potential role of peptidylarginine deiminase enzymes and protein citrullination in cancer pathogenesis. Biochem. Res. Int. 2012, 895343 (2012).
Ishigami, A. et al. Abnormal accumulation of citrullinated proteins catalyzed by peptidylarginine deiminase in hippocampal extracts from patients with Alzheimer’s disease. J. Neurosci. Res. 80(1), 120–128 (2005).
Aggarwal, A. Role of autoantibody testing. Best Pract. Res. Clin. Rheumatol. 28(6), 907–920. https://doi.org/10.1016/j.berh.2015.04.010 (2014).
Takeuchi, T. Biomarkers as a treatment guide in rheumatoid arthritis. Clin. Immunol. 186, 59–62 (2018).
Soe, H. J. et al. Identifying protein biomarkers in predicting disease severity of dengue virus infection using immune-related protein microarray. Medicine (Baltimore) 97(5), 6–12 (2018).
Poulsen, T. B. G. et al. Identification of novel native autoantigens in rheumatoid arthritis. Biomedicines 8(6):141. https://doi.org/10.3390/biomedicines8060141 (2020).
Poulsen, T. B. G. et al. Protein array-based companion diagnostics in precision medicine. Expert Rev. Mol. Diagn. 20(12), 1183–1198. https://doi.org/10.1080/14737159.2020.1857734 (2020).
Konig, M. F., Giles, J. T., Nigrovic, P. A. & Andrade, F. Antibodies to native and citrullinated RA33 (hnRNP A2/B1) challenge citrullination as the inciting principle underlying loss of tolerance in rheumatoid arthritis. Ann. Rheum. Dis. 75(11), 2022–2028. https://doi.org/10.1136/annrheumdis-2015-208529 (2016).
Wang, X., Chen, P., Cui, J., Yang, C. & Du, H. Biochemical and biophysical research communications keratin 8 is a novel autoantigen of rheumatoid arthritis. Biochem. Biophys. Res. Commun. 465(4), 665–669. https://doi.org/10.1016/j.bbrc.2015.07.161 (2015).
Snir, O. et al. Multiple antibody reactivities to citrullinated antigens in sera from patients with rheumatoid arthritis: Association with HLA-DRB1 alleles. Ann. Rheum. Dis. 68(5), 736–743. https://doi.org/10.1136/ard.2008.091355 (2009).
Schwenzer, A. et al. Identification of an immunodominant peptide from citrullinated tenascin-C as a major target for autoantibodies in rheumatoid arthritis. Ann. Rheum. Dis. 75(10), 1876–1883. https://doi.org/10.1136/annrheumdis-2015-208495 (2016).
Van Steendam, K., Tilleman, K. & Deforce, D. The relevance of citrullinated vimentin in the production of antibodies against citrullinated proteins and the pathogenesis of rheumatoid arthritis. Rheumatology 50(5), 830–837. https://doi.org/10.1093/rheumatology/keq419 (2011).
Kurowska, W., Kuca-Warnawin, E. H., Radzikowska, A. & Maśliński, W. The role of anti-citrullinated protein antibodies (ACPA) in the pathogenesis of rheumatoid arthritis. Cent. J. Immunol. 42(4), 390–398 (2017).
Karthikeyan, K. et al. A contra capture protein array platform for studying post-translationally modified (PTM) Auto-antigenomes. Mol. Cell Proteom. 15(7), 2324–2337 (2016).
Sahlström, P. et al. Different hierarchies of anti-modified protein autoantibody reactivities in rheumatoid arthritis. Arthritis Rheumatol. 72(10), 1643–1657. https://doi.org/10.1002/art.41385 (2020).
Damgaard, D., Bjørn, M. E., Jensen, P. Ø. & Nielsen, C. H. Reactive oxygen species inhibit catalytic activity of peptidylarginine deiminase. J. Enzyme Inhib. Med. Chem. 32(1), 1203–1208. https://doi.org/10.1080/14756366.2017.1368505 (2017).
Nakayama-Hamada, M. et al. Comparison of enzymatic properties between hPADI2 and hPADI4. Biochem. Biophys. Res. Commun. 327(1), 192–200 (2005).
Vossenaar, E. R. et al. Expression and activity of citrullinating peptidylarginine deiminase enzymes in monocytes and macrophages. Ann. Rheum. Dis. 63(4), 373–381 (2004).
Damgaard, D., Senolt, L., Nielsen, M. F., Pruijn, G. J. & Nielsen, C. H. Demonstration of extracellular peptidylarginine deiminase (PAD) activity in synovial fluid of patients with rheumatoid arthritis using a novel assay for citrullination of fibrinogen. Arthritis Res. Ther. 16(6), 498. https://doi.org/10.1186/s13075-014-0498-9 (2014).
Ioan-Facsinay, A. et al. Anti-CCP antibodies are a collection of ACPA that are cross-reactive to multiple citrullinated antigens. Ann. Rheum. Dis. 69(Suppl 2), A8–A8. https://doi.org/10.1136/ard.2010.129577s (2010).
Ge, C. et al. Structural basis of cross-reactivity of anti-citrullinated protein antibodies. Arthritis Rheumatol. 71(2), 210–221. https://doi.org/10.1002/art.40698 (2019).
Trier, N. H., Leth, M. L., Hansen, P. R. & Houen, G. Cross-reactivity of a human IgG 1 anticitrullinated fibrinogen monoclonal antibody to a citrullinated profilaggrin peptide. Protein Sci. 21(12), 1929–1941. https://doi.org/10.1002/pro.2178 (2012).
Reed, E. et al. Presence of autoantibodies in “seronegative” rheumatoid arthritis associates with classical risk factors and high disease activity. Arthritis Res. Ther. 22(1), 170. https://doi.org/10.1186/s13075-020-02191-2 (2020).
Somers, K. et al. Novel autoantibody markers for early and seronegative rheumatoid arthritis. J. Autoimmun. 36(1), 33–46 (2011).
De Winter, L. M. et al. Autoantibodies to two novel peptides in seronegative and early rheumatoid arthritis. Rheumatology 55(8), 1431–1436. https://doi.org/10.1093/rheumatology/kew198 (2016).
Wagner, C. A. et al. Identification of anticitrullinated protein antibody reactivities in a subset of anti-CCP-negative rheumatoid arthritis: Association with cigarette smoking and HLA-DRB1 ‘shared epitope’ alleles. Ann. Rheum. Dis. 74(3), 579–586. https://doi.org/10.1136/annrheumdis-2013-203915 (2013).
Strollo, R. et al. Antibodies to post-translationally modified insulin as a novel biomarker for prediction of type 1 diabetes in children. Diabetologia 60(8), 1467–1474. https://doi.org/10.1007/s00125-017-4296-1 (2017).
Utz, P. J., Hottelet, M., Schur, P. H. & Anderson, P. Proteins phosphorylated during stress-induced apoptosis are common targets for autoantibody production in patients with systemic lupus erythematosus. J. Exp. Med 185(5):843–54. https://doi.org/10.1084/jem.185.5.843 (1997).
Wegner, N. et al. Peptidylarginine deiminase from Porphyromonas gingivalis citrullinates human fibrinogen and α-enolase: Implications for autoimmunity in rheumatoid arthritis. Arthritis Rheum. 62(9), 2662–2672. https://doi.org/10.1002/art.27552 (2010).
Konig, M. F., Paracha, A. S., Moni, M., Bingham, C. O. & Andrade, F. Defining the role of Porphyromonas gingivalis peptidylarginine deiminase (PPAD) in rheumatoid arthritis through the study of PPAD biology. Ann. Rheum. Dis. 74(11), 2054–2061. https://doi.org/10.1136/annrheumdis-2014-205385 (2015).
de Moel, E. C. et al. Baseline autoantibody profile in rheumatoid arthritis is associated with early treatment response but not long-term outcomes. Arthritis Res. Ther. 20(1), 33. https://doi.org/10.1186/s13075-018-1520-4 (2018).
Lal, P. et al. Inflammation and autoantibody markers identify rheumatoid arthritis patients with enhanced clinical benefit following rituximab treatment. Arthritis Rheum. 63(12), 3681–3691. https://doi.org/10.1002/art.30596 (2011).
Hamaguchi, Y. Autoantibody profiles in systemic sclerosis: Predictive value for clinical evaluation and prognosis. J. Dermatol. 37(1), 42–53. https://doi.org/10.1111/j.1346-8138.2009.00762.x (2010).
Liang, Z. et al. Identification of clinically relevant subgroups of COPD based on airway and circulating autoantibody profiles. Mol. Med. Rep. https://doi.org/10.3892/mmr.2019.10498 (2019).
Aletaha, D. et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 62(9), 2569–2581. https://doi.org/10.1002/art.27584 (2010).
Duarte, J., Serufuri, J., Mulder, N. & Blackburn, J. Bioinformatics of Human Proteomics, Vol 3 39–74 (Springer, 2013). https://doi.org/10.1007/978-94-007-5811-7.
Bennike, T. B. et al. Neutrophil extracellular traps in ulcerative colitis. Inflamm. Bowel Dis 21(9):2052–67. https://doi.org/10.1097/MIB.0000000000000460. (2015).
Perez-Riverol, Y. et al. The PRIDE database and related tools and resources in 2019: Improving support for quantification data. Nucleic Acids Res. 47(D1), D442–D450 (2019).
Acknowledgements
Department of Immunology at Rigshospitalet, Denmark is acknowledged for providing the biological samples. TP is co-financed by a Grant from the Sino-Danish Center and Aalborg University. LS is supported by research project No. 023728 of the Ministry of Health of the Czech Republic for the conceptual development of a research organization. JMB thanks the National Research Foundation for a Research Chair Grant. Figure 3 was reproduced from a figure provided by Sengenics.
Funding
The study is part of the PROCIT study financed by the Danish Council for Independent Research (DFF-7016-00233). Moreover, the Danish National Mass Spectrometry Platform for Functional Proteomics (PRO-MS; Grant no. 5072-00007B), the Obelske family foundation, the Svend Andersen Foundation, and the SparNord foundation are acknowledged for grants to the analytical platform, enabling parts of this study.
Author information
Authors and Affiliations
Contributions
T.P., A.S., C.N., and D.D. conceptualized the overall study. D.D. and L.S. collected samples for the study. T.P. wrote the draft version of the paper and revised it according to the coauthors' comments (C.N., A.S., D.D., and J.B.). T.P. performed the sample preparation and data analysis. M.J. contributed to the methodology. A.S. and C.N. supervised the study. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
JMB is the Chief Scientific Officer of Sengenics Corporation who commercializes the Immunome arrays used in this study. TP, DD, MJ, CN, AS, and LS declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Poulsen, T.B.G., Damgaard, D., Jørgensen, M.M. et al. Identification of potential autoantigens in anti-CCP-positive and anti-CCP-negative rheumatoid arthritis using citrulline-specific protein arrays. Sci Rep 11, 17300 (2021). https://doi.org/10.1038/s41598-021-96675-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96675-z
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.