Abstract
Each year, > 3 million children die in sub-Saharan Africa before their fifth birthday. Most deaths are preventable or avoidable through interventions delivered in the primary healthcare system. However, evidence regarding the impact of health system characteristics on child survival is sparse. We assembled a retrospective cohort of > 250,000 children in seven countries in sub-Saharan Africa. We described their health service context at the subnational level using standardized surveys and employed parametric survival models to estimate the effect of three major domains of health services—quality, access, and cost—on infant and child survival, after adjusting for child, maternal, and household characteristics. Between 1995 and 2015 we observed 13,629 deaths in infants and 5149 in children. In fully-adjusted models, the largest effect sizes were related to fees for services. Immunization fees were correlated with poor child survival (HR = 1.20, 95% CI 1.12–1.28) while delivery fees were correlated with poor infant survival (HR = 1.11, 95% CI 1.01–1.21). Accessibility of facilities and greater concentrations of private facilities were associated with improved infant and child survival. The proportion of facilities with a doctor was correlated with increased risk of death in children and infants. We quantify the impact of health service environment on survival up to five years of age. Reducing health care costs and improving the accessibility of health facilities should remain a priority for improving infant and child survival. In the absence of these fundamental investments, more specialized interventions may not achieve their desired impact.
Similar content being viewed by others
Introduction
In 2015, the international community embraced the Sustainable Development Goals, which include the ambitious goal of eliminating preventable child deaths by 2030. Annually, more than 50% of childhood deaths occur in sub-Saharan Africa1,2. Thirty-four percent of these deaths occur in the neonatal period3 and of these 70% are preventable through effective prenatal care or safe delivery4,5. After the neonatal period, treatable or preventable infectious diseases such as pneumonia, malaria, and diarrhoea, account for between 64 and 90% of childhood deaths3,6. In short, a large proportion of deaths between birth and the fifth birthday are a result of common causes that are avoidable through affordable and effective interventions. Therefore, child mortality remains unacceptably high where these causes dominate.
Health facilities are the primary distribution channel for many cost-effective interventions such as immunizations, safe delivery and insecticide-treated bednets. Although each individual intervention has great potential to reduce morbidity and mortality, the population-level impact of these life-saving interventions may be limited by the health systems that deliver them4,7. For example, an estimated 15–29% of people in SSA live more than 2 h travel time from the nearest public hospital 8,9 which highlights the limitation of geographic distribution of health services. In an era of renewed emphasis on Universal Health Care (UHC), the importance of measuring health system coverage and quality is being recognized10,11,12. Previous studies in sub-Saharan Africa have assessed quality by benchmarking on guidelines 13,14. However, very few studies have extended these measures to understand their relationship to health outcomes15.
Inadequate health systems may be impeding progress in child survival, but rigorous evaluation of delivery strategies is methodologically challenging7,16,17. Here we adopt the perspective of Watkins18 and focus on the ‘platforms required to deliver essential interventions’ as a critical factor in the success of UHC. Specifically, with respect to the Countdown to 2015 framework19, we focus on three key health system building blocks—infrastructure, workforce, and financing—which, when taken from the point of view of the user, become access, quality and cost. The objective of this study is to better understand the impact of the health system as a delivery platform, independent of specific interventions, on child survival. We focus on subnational measures of health system context motivated by the observation that child mortality varies more within countries than between countries20. We assembled a longitudinal cohort of children born in seven countries over 20 years and estimate the impact of their local health services context on the risk of death in infancy and early childhood. We divide the health context into three dimensions—access, quality and cost—and individually investigate their relationship to survival.
Methods
All data were downloaded from publicly available survey datasets on the Demographic and Health Surveys Program website (https://www.dhsprogram.com/). All survey methods were approved by the ICF Institutional Review Board (IRB) as well as equivalent boards within host countries and all information was gathered in accordance with the guidelines and regulations of these institutions. Further details are available at https://dhsprogram.com/methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm.
Information about health services comes from the Service Provision Assessments (SPA). SPA are carried out in a sample of public and private [both not-for-profit, and for-profit] health facilities and are representative at the sub-national [regional/provincial] level. SPA includes information about infrastructure, facility staffing, staff training, types of services provided, commodities and fees.
We obtained data about births and survival from Demographic and Health Surveys (DHS) conducted in all the countries for which SPA data were available. DHS collect information about household demographics, health metrics, and child survival in a sample of households using a two-stage random sampling strategy. All mothers in sampled households are asked to give complete birth histories which document the date of birth and survival status for every child born to them.
Since SPA and DHS surveys are not carried out concurrently, we linked each birth from the DHS surveys with the health facility data in the SPA surveys. A birth was assigned to the respective SPA data for that country-region if there was an SPA survey available within 5 years of the recorded birth year, or to the nearest SPA if more than one was available. Births not linked to SPA data were excluded, all other births were included. All hospitals, health centers, and clinics from the SPA sample were included; dispensaries and stand-alone VCTs were excluded. A complete list of countries and years for DHS and SPA data is presented in Table S1A and the number of births per region-survey is presented in Table S1B.
Note that we are not linking births to a specific SPA facility, since the DHS and SPA surveys do not provide location data on a more granular level than the country-region. Instead, we are looking at the relationship between region-level mortality and health system characteristics, under the assumption that aa SPA survey conducted within a 5 years of the recorded birth year is representative of the relevant health context in which the child was born.
We defined two outcomes related to child survival—(1) survival past 12 months for every child born alive and (2) survival beyond 59 months for every child who survived to their first birthday. These correspond to standard definitions of infant mortality and child mortality.
We characterized health services based on three ‘domains’—geographic distribution, human resources as a measure of capacity to deliver quality, and out-of-pocket cost. We approximated the geographic distribution of health facilities within a country as the ratio of the proportion of that country’s total number of facilities located within that subnational region to the proportion of that country’s total population within that region. That is, a ratio of how concentrated that country’s health facilities are within each subnational region to how concentrated that country’s population is within that region. This is a measure of the degree to which the distribution of health facilities within a country aligns with the distribution of the population. Ratios > 1 then correspond to regions with greater per-capita concentration of health facilities. In addition, we included as a covariate the proportion of facilities with a region that were privately owned, as a proxy for the accessibility of private healthcare. We examine private health facilities specifically since their distribution is shaped by market forces (demand, ability to pay) rather than government policy.
The capacity to deliver quality services was represented by the proportion of facilities with a physician on staff and the proportion of clinical staff that had received training in the Integrated Management of Childhood Illnesses (IMCI). Healthcare costs to the patient were measured by the proportion of facilities in a region charging fees for three basic types of service—sick child visits, routine immunization, and normal delivery. We used standard sampling weights provided with each SPA dataset to account for survey design when calculating aggregated characteristics within a subnational region21.
The objective of this study was to estimate the relationship between infant and child survival and health systems factors. We identified control variables that may confound this relationship but do not lie on the causal pathway between health service delivery and the outcome of survival. As an example, we do not control for immunization status in our model even though it is related to survival because immunization coverage is likely related to the health services context. Similarly, we do not include measures of availability of specific interventions within each facility. Our goal is to estimate the association between the health services environment and survival rather than the impact of individual interventions. We examined correlations between our explanatory variables and ensured none were highly co-linear.
Separate log-normal accelerated failure time survival models were fit to each mortality outcome, with a normally distributed frailty term to account for the correlation of births with a common mother. The general log-linear representation of this model is given by:
where \({T}_{ij}\) denotes the survival time of child i of mother j, \(\mu \) denotes the intercept, \({\alpha }_{j}\) denotes the frailty term, and \({\sigma \varepsilon }_{ij}\) denotes the residuals, which follow a standard normal distribution and are multiplied by an arbitrary scaling factor \(\sigma .\) The set of control and exposure variables included in the model are given by \({x}_{1}\dots {x}_{p}\) with coefficients \({\beta }_{1}\dots {\beta }_{p}\). We adjusted for individual-level characteristics that have been implicated in child survival: birth order, sex, maternal factors (education, age, marital status), and household wealth. We include an indicator for urban/rural and birth year to control for secular trends in child survival. Exposure variables were mean-centered and scaled by their interquartile range. The complete list of variables in the model is included in Table S3.
For infant mortality, child’s survival time was calculated as the time, in months, from the date of birth to the date of death, the date of the DHS interview, or the date of the child’s first birthday, whichever came first. For child mortality, the same approach was used beginning from the child’s first birthday up through their fifth birthday. Individuals whose interview date came before the relevant birthday were treated as censored. We analyzed survival to the first birthday and fifth birthday separately because we expected factors related to survival to differ between infants and young children. As a sensitivity analysis, we also fit a model for all deaths from date of birth to the child’s fifth birthday to assess the degree to which child mortality results may have been driven by conditioning on having survived to their first birthday. We assume risk of death is uniform within any given month22.
Without loss of generality, we re-parameterized the model such that the resulting coefficients are analogous to standard hazard ratios (i.e. \({\beta }_{i}=-{\gamma }_{i}\), where \(\gamma \) denotes the standard coefficient of the accelerated failure time model). The parameter estimate for a given covariate is then interpreted as the multiplicative degree to which that covariate decreases the expected survival time of a child; so estimates greater than one correspond to a decrease of expected survival time and less than one correspond to an increase of expected survival time. Since this multiplicative factor is proportional to the true log-hazard, we interpret the exponentiated coefficients as approximates to the hazard ratio.
We elected not to use sampling weights. The individual-level sampling weights within DHS survey are normalized to sum to the sample size of that survey; thus, using the given weights would implicitly bias the results towards those surveys with larger sample sizes. Renormalizing the weights across the included surveys would require assumptions about the relationship of the probability of sampling both between and within countries over time. Since we did not feel that any such assumptions could be justified or verified, we took the pragmatic approach of using fixed-effect terms on country and birth year to control for systematic differences between countries and over time.
Finally, we note that we used Tanzania as the reference level for the country fixed effect in our models. We chose Tanzania since the proportion of childhood deaths in the country was approximately equal to the average across countries (see the last two rows of Table S2). This allows for intuitive comparisons of the fixed effect estimates for each country (see Table S3). The interpretation of the covariates of interest (i.e. SPA exposures) is not impacted by the choice of reference level.
All analyses were done in R, version 4.0.2, and models fit using the package ‘survival’, version 3.2–7 23].
Ethics approval and consent to participate
The DHS Program obtained ethical approvals for data collection and we obtained permission from the DHS Program to use these data. Duke Institutional Review Board approved this analysis as exempt from human subjects review.
Results
We assembled a large, multi-national retrospective cohort of 256,031 children from seven African countries between 1995–2016. There were 13,629 deaths among infants before their first birthday and among children 12–59 months, there were an additional 5149 deaths.
Median maternal age at delivery was 26 years and most mothers had not completed primary school (Table 1, 59.1%). A quarter of households were located in urban areas. Mother characteristics differed slightly by country (Table S1)—there were fewer young mothers in Rwanda and more mothers completed secondary school in Namibia and Kenya. In Namibia, far fewer mothers were married and more households were located in urban areas.
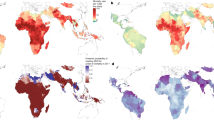
1–3 SPAs were conducted in each of the countries giving 150 region-years of paired SPA and survival information over the study period (Table 2). The ratio of facilities to total population within a region ranged from 0.97 to 1.19 (Fig. 1), and the average across region-years was highest for Senegal and lowest for Kenya. Overall, the proportion of private facilities was low, country-level means ranging from 0.04 in Tanzania to 0.14 in Uganda. Few facilities had doctors; 9 per 100 in Uganda, up to 17 per 100 in Rwanda. Senegal had the highest levels of IMCI training at 20% on average trained per facility. Namibia had the highest proportion of facilities charging fees for sick child visits (97%), while Rwanda had the highest proportion charging fees for delivery (86%). Fees for immunization were least common, although 69% of facilities in Senegal did charge for routine immunization. The fewest facilities charged fees (for any service) in Tanzania and Uganda.
Health system variables by region and year. Maps of region-level means are shown for east Africa to demonstrate variability in space. The box plots show the median and range of each variable by year for all the countries contributing data in that year. Between 7 and 40 (mean = 15) regions are represented in each year of the box plots. Maps were generated in ArcMap 10.7 (Esri Inc., 2019, https://desktop.arcgis.com/en/arcmap/).
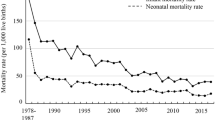
Infant and child survival differed between countries and between regions within countries (Fig. 2). Overall, the risk of childhood death declined over time (Fig. 3). Fully-adjusted models showed country-level deceleration factors ranging from 0.82 in Kenya up to 1.88 in Uganda; this indicates that average child survival time was 18% longer in Kenya and 88% shorter in Uganda relative to the reference country (Tanzania). At the individual-level, increasing maternal education, being married, and increasing household wealth were protective (Supplemental Table 3).
Map of study area with estimated hazard ratio for (A) child and (B) infant mortality per region averaged over the study period relative to the median value. East Africa is enlarged (inset) to better appreciate the inter and intra-country differences in risk of death. Maps were generated in ArcMap 10.7 (Esri Inc., 2019, https://desktop.arcgis.com/en/arcmap/).
Specific aspects of the health services context were related to survival and these patterns were distinct for infant and child mortality (Table 3). In fully-adjusted survival models, higher ratio of health facilities relative to the population was associated with improved child survival (0.97, 95% CI 0.94–0.99), but not infant survival. The proportion of private facilities in a region was associated with improved survival for both children (0.81, 95% CI 0.79–0.84) and infants (0.87, 95% CI 0.85–0.9). However, health workforce indicators were not associated with improved survival. In particular, the proportion of facilities with a doctor was negatively correlated with both child (1.11, 95% CI 1.08–1.14) and infant (1.03, 95% CI 1.01–1.05) survival.
Survival was also related to the cost of care. Moving from the first to the third quartile of prevalence of delivery fees (10–77%) was associated with an 11% (95% CI 1–21%) increase in risk of death in infancy in the fully adjusted model. A similar scaled increase in the proportion of facilities charging immunization fees (from 27.5 to 73.1% of facilities charging fees) was associated with 20% (95% CI 12–28%) increased risk of death among children. Conversely, delivery fees were associated with improved child survival (0.82, 95% CI 0.74–0.91).
Discussion
As the global community solidifies its commitment to UHC, vital initiatives to extend coverage24 will likely be crippled by insufficient health systems and there is an urgent need for evidence to guide investment in health systems themselves25,26. In order to help identify critical shortcomings that may directly impact child survival, we analyzed data from > 250,000 children born over 20 years in seven countries and show that infant and child survival are correlated with specific aspects of health systems context. In our analysis, physical distribution of health services is an important determinant of child survival, a finding which agrees with other studies using similar data sources27 and with results which estimate that, in sub-Saharan Africa, a higher proportion of avertable deaths is associated with poor access than poor quality28. The association between poor access and mortality could reflect limited physical access in terms of distance or travel time or poor distribution of facilities resulting in crowding and unmanageable patient volumes. The positive effect of private facilities on survival, even after adjusting for wealth and urban context, may be attributable to documented higher quality in private facilities in some countries13,29 or potentially a reflection of the private sector responding to a demand for healthcare that the public sector has not met. Although the proportion of facilities that were private was generally low, the effect size was important, further highlighting the value of engaging the private sector in UHC strategies.
The lack of association of child survival with curative service fees coupled with an association with health infrastructure together suggest that expansion of insurance programs may be insufficient to substantially reduce mortality in this vulnerable group. In contrast, the negative association of delivery fees with infant survival points to a key opportunity to reduce neonatal and infant mortality by improving the affordability of safe delivery30. The positive association between delivery fees and child survival may be a survivorship effect whereby higher mortality during infancy in areas where delivery fees are prevalent may lead to lower apparent mortality after one year of age. This interpretation is supported by the lack of a positive association between survival and delivery fees in our sensitivity analysis of survival from birth to the fifth birthday [i.e. the effect is only observed when conditioning on survival to one year]. The negative association between child survival and immunization fees may reflect low uptake of immunization when out-of-pocket payments are required and points to the importance of providing these high-impact, preventive services free of charge. We previously showed that fees for sick child visits reduced child survival in Kenya, but this effect is not seen in the current multi-country analysis31.
Doctors and IMCI-trained staff were not associated with improved survival. A comparison of child mortality in Mozambique also demonstrated a protective effect of higher density of nurses and midwives, but not physicians32. On the surface, the negative association between survival and prevalence of a doctor seems to contradict inter-country comparisons of density of doctors on child mortality33,34. However, when examined more closely, the protective effect of physician density is only observed in high-functioning health systems of low-mortality, high-income countries35. Our finding is consistent with observations by others that the presence of a doctor has no effect on the quality of acute child care, antenatal care, or delivery services in under-resourced settings36. We did not observe a strong correlation between doctors and private facilities or fees which, if present, could confound this result (Table S4), however it is possible that proportion of doctors indicates higher concentrations of larger facilities such as hospitals relative to clinics. Lack of an association between IMCI training and survival agrees with reports that training may have limited impact on quality of care37,38 as well as evaluations of IMCI training itself 37. These results have important implications—first, many life-saving interventions can be effectively deployed by nurses and clinical officers and higher-level formal training is not required to improve child survival. Second, improving the skill level of health facility staff may not have the expected impact without the tools and motivation to put the training into practice.
Results should be interpreted while considering study limitations. Data for this study came from a subset of sub-Saharan African countries, based on the availability of SPA, potentially limiting the generalizability. Health insurance programs may affect the relationship between fees and mortality via prepayment or premiums. Ghana has a comparatively high rate of enrollment in national health insurance and Rwanda has high enrollment in community-based health insurance. Geographic distribution of health facilities relative to population is an imperfect measure of physical access. We may not be able to distinguish between regions of the same population and number of facilities but very different geographic extent which would lead to potentially large unmeasured differences in physical access. Mortality is assessed through birth histories that are subject to recall bias and survivorship bias.
Finally, our exposure variables are aggregated at the sub-national level and we cannot relate each child to their nearest health facility. This restricts us from leveraging more fine-scaled heterogeneities and assigns each birth to the region-level mean, likely biasing effect estimates towards the null. In addition, we did not account for the location of birth at the individual or region level which could be influenced by factors other than health system characteristics, including cultural practices and norms. Despite this imprecision, we are still able to measure substantial correlation with survival outcomes.
Our analysis has several important strengths. First, we move beyond evaluation of quality or readiness and relate health systems characteristics to child survival outcomes. Second, we examine this relationship at the sub-national level over two decades across seven countries, incorporating data from multiple surveys within the same country. This allows us to leverage documented high levels of heterogeneity in child survival between subnational regions20 to quantify the impact of health systems context on survival outcomes. Longitudinal analysis ensures that we capture the effect of change in health systems on mortality, for example the expansion of ARTs and HIV care, investment in infrastructure during the MDG era, the evolution of health insurance, and the abolition of user fees in several countries. These factors enhance the generalizability of our results.
UHC is emerging as a key pillar for achieving Sustainable Development Goal 3 and ending preventable childhood deaths. Ninety-percent of the Disease Control Priorities-3 (DCP3) essential UHC interventions are delivered through primary health care facilities11. As a result, the impact of UHC will depend heavily on the characteristics of the underlying health system and it is important to understand the relationship between health systems factors and health outcomes. Here, we isolate the impact of health systems characteristics and directly measure the impact on population-based survival outcomes. Our findings suggest key areas for further research with respect to realizing the potential of UHC, including (1) the role of public subsidies or health insurance to mitigate the negative impact of user fees for immunization and delivery, (2) investment in physical infrastructure to improve access, (3) engaging the private sector to achieve UHC goals, and (4) closing the human resource gap with basic cadres of health care workers.
References
You, D. et al. Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet (London, England) 386(10010), 2275–2286 (2015).
Burstein, R. et al. Mapping 123 million neonatal, infant and child deaths between 2000 and 2017. Nature 574(7778), 353–358 (2019).
Liu, L. et al. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 388(10063), 3027–3035 (2016).
Bhutta, Z. A. et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost?. Lancet 384(9940), 347–370 (2014).
Darmstadt, G. L. et al. Evidence-based, cost-effective interventions: How many newborn babies can we save?. Lancet (London, England) 365(9463), 977–988 (2005).
Taylor, A. W. et al. Initial findings from a novel population-based child mortality surveillance approach: A descriptive study. Lancet Glob. Health 8(7), e909–e919 (2020).
Bryce, J. et al. Reducing child mortality: Can public health deliver?. Lancet 362(9378), 159–164 (2003).
Falchetta, G., Hammad, A. T. & Shayegh, S. Planning universal accessibility to public health care in sub-Saharan Africa. Proc. Natl. Acad. Sci. 117(50), 31760 (2020).
Ouma, P. O. et al. Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: A geocoded inventory and spatial analysis. Lancet Glob. Health 6(3), e342–e350 (2018).
Scott, K. W. & Jha, A. K. Putting quality on the global health agenda. N Engl J Med. 371(1), 3–5 (2014).
Akachi, Y. & Kruk, M. E. Quality of care: Measuring a neglected driver of improved health. Bull. World Health Organ. 95(6), 465–472 (2017).
Kruk, M. E., Larson, E. & Twum-Danso, N. A. Time for a quality revolution in global health. Lancet Glob. Health 4(9), e594–e596 (2016).
Kruk, M. E., Chukwuma, A., Mbaruku, G. & Leslie, H. H. Variation in quality of primary-care services in Kenya, Malawi, Namibia, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull. World Health Organ. 95(6), 408–418 (2017).
Leslie, H. H., Sun, Z. & Kruk, M. E. Association between infrastructure and observed quality of care in 4 healthcare services: A cross-sectional study of 4,300 facilities in 8 countries. PLoS Med. 14(12), e1002464 (2017).
Leslie, H. H., Fink, G., Nsona, H. & Kruk, M. E. Obstetric facility quality and newborn mortality in Malawi: A cross-sectional study. PLoS Med. 13(10), e1002151 (2016).
Task Force on Health Systems Research. The Millennium Development Goals will not be attained without new research addressing health system constraints to delivering effective interventions. Report of the Task Forice on Health Systems Research (2005).
Victora, C. G., Hanson, K., Bryce, J. & Vaughan, J. P. Achieving universal coverage with health interventions. Lancet (London, England) 364(9444), 1541–1548 (2004).
Watkins, D. A. et al. Alma-Ata at 40 years: Reflections from the Lancet Commission on investing in health. Lancet (London, England) 392(10156), 1434–1460 (2018).
Singh, N. S. et al. Countdown to 2015 country case studies: Systematic tools to address the “black box” of health systems and policy assessment. BMC Public Health 16(2), 790 (2016).
Burke, M., Heft-Neal, S. & Bendavid, E. Sources of variation in under-5 mortality across sub-Saharan Africa: A spatial analysis. Lancet Glob. Health 4(12), e936–e945 (2016).
Korn, E. L. & Graubard, B. I. Analysis of Health Surveys (Wiley, 1999).
Rabinowitz, D., Tsiatis, A. & Aragon, J. Regression with interval-censored data. Biometrika 82(3), 501–513 (1995).
Therneau, T. A Package for Survival Analysis in S. version 2.38 (2015).
Boerma, T., Victora, C. G., Sabin, M. L. & Simpson, P. J. Reaching all women, children, and adolescents with essential health interventions by 2030. BMJ 368, 16986 (2020).
The World Health Report 2013: Research for Universal Health Coverage (World Health Organization, 2013).
Kieny, M. P. et al. Strengthening health systems for universal health coverage and sustainable development. Bull. World Health Organ. 95, 537–539 (2017).
Karra, M., Fink, G. & Canning, D. Facility distance and child mortality: A multi-country study of health facility access, service utilization, and child health outcomes. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyw062 (2016).
Kruk, M. E. et al. Mortality due to low-quality health systems in the universal health coverage era: A systematic analysis of amenable deaths in 137 countries. Lancet (London, England) 392(10160), 2203–2212 (2018).
Berendes, S., Heywood, P., Oliver, S. & Garner, P. Quality of private and public ambulatory health care in low and middle income countries: Systematic review of comparative studies. PLoS Med. 8(4), e1000433 (2011).
McKinnon, B., Harper, S., Kaufman, J. S. & Bergevin, Y. Removing user fees for facility-based delivery services: A difference-in-differences evaluation from ten sub-Saharan African countries. Health Policy Plan. 30(4), 432–441 (2015).
Anthopolos, R., Simmons, R. & O’Meara, W. P. A retrospective cohort study to quantify the contribution of health systems to child survival in Kenya: 1996–2014. Sci. Rep. 7, 44309 (2017).
Fernandes, Q. F. et al. Effects of health-system strengthening on under-5, infant, and neonatal mortality: 11-year provincial-level time-series analyses in Mozambique. Lancet Glob. Health 2(8), e468–e477 (2014).
Anand, S, & Barnighausen, T. Human resources and health outcomes: Cross-country econometric study (1474-547X (Electronic)).
Speybroeck, N., Kinfu, Y., Dal Poz, M. R. & Evans, D. B. Reassessing the Relationship Between Human Resources for Health, Intervention Coverage and Health Outcomes (World Health Organization, 2006).
Cohen, R. L., Murray, J., Jack, S., Arscott-Mills, S. & Verardi, V. Impact of multisectoral health determinants on child mortality 1980–2010: An analysis by country baseline mortality. PLoS ONE 12(12), e0188762 (2017).
Kruk, M. E., Prescott, M. R., de Pinho, H. & Galea, S. Are doctors and nurses associated with coverage of essential health services in developing countries? A cross-sectional study. Hum. Resour. Health 7, 27 (2009).
Gera, T., Shah, D., Garner, P., Richardson, M. & Sachdev, H. S. Integrated management of childhood illness (IMCI) strategy for children under five. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD010123.pub2 (2016).
Leslie, H. H., Gage, A., Nsona, H., Hirschhorn, L. R. & Kruk, M. E. Training and supervision did not meaningfully improve quality of care for pregnant women or sick children in sub-Saharan Africa. Health Affairs (Project Hope) 35(9), 1716–1724 (2016).
Funding
Research reported in this publication was supported in part by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R03HD078600. Biostatistical support for this publication was supported in part by Grant Number UL1TR002553 from the National Center for Advancing Translational Sciences and the National Institutes of Health Roadmap for Medical Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funder had no role in the analysis or decision to publish.
Author information
Authors and Affiliations
Contributions
R.S. contributed to design of the study, carried out the analyses and drafted the manuscript. R.A. developed the statistical approach. W.P.O. conceived the study, led the development and execution of the study and drafted the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Simmons, R.A., Anthopolos, R. & O’Meara, W.P. Effect of health systems context on infant and child mortality in sub-Saharan Africa from 1995 to 2015, a longitudinal cohort analysis. Sci Rep 11, 16263 (2021). https://doi.org/10.1038/s41598-021-95886-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-95886-8
This article is cited by
-
The Impact of Bias on the Pathway to Otolaryngology: Time to Level Up
Current Otorhinolaryngology Reports (2023)
-
The impact of maternal health insurance coverage and adequate healthcare services utilisation on the risk of under-five mortality in Nigeria: a cross-sectional study
Archives of Public Health (2022)
-
Factors associated with healthcare-seeking behavior for symptomatic acute respiratory infection among children in East Africa: a cross-sectional study
BMC Pediatrics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.