Abstract
To define an algorithm for differential diagnostics of parotid malignancies and Warthin tumors (WTs) based on dynamic contrast enhanced MRI (DCE-MRI). 55 patients with parotid tumors treated surgically were analyzed. Of which, 19 had parotid malignancy and 36 had WTs confirmed with postoperative histopathological examination. Accuracy of DCE-MRI parameters (Tpeak and WR) was compared with the histopathological diagnosis. ROC analysis was performed to determine sensitivity and specificity of DCE-MRI with various Tpeak and WR cut-off values. WT showed significantly lower median Tpeak and higher median WR than malignant lesions. The cut-off values for Tpeak and WR providing maximum sensitivity (84.2%) and specificity (86.1%) for malignant tumors were Tpeak > 60 s and WR ≤ 30%. Different diagnostic algorithm, i.e., lower cut-off value for Tpeak (Tpeak = 60 s), increases sensitivity of DCE-MRI in differentiating parotid malignancies from WTs. However, WR > 30% seems to be a key diagnostic criterion for benign lesions. Precise and reliable preoperative diagnostics of parotid tumors aids in careful surgical planning, thereby assisting in achieving sufficient surgical resection margins and facial nerve preservation.
Similar content being viewed by others
Introduction
Parotid tumors represent approximately 5% of all head and neck neoplasms1,2. Warthin tumors (WTs), also referred to as papillary cystadenoma lymphomatosum, is the second most common benign tumor of the parotid found in 14–30% of the patients. It usually occurs in the 6th–7th decade of life with a greater incidence in smokers than non-smokers3,4,5,6. As benign slowly growing lesions that rarely recur or undergo malignant transformation, WTs are often treated less radically with local excision or even expectant management6,7,8,9. However, such therapeutic decisions can only be made when malignancy is unequivocally excluded.
Fine needle biopsy remains a standard in preoperative evaluation of parotid tumors10. However, this method has limited application in the case of small and/or deeply located lesions11,12,13, and if performed incorrectly may result in systemic spread of cancer cells14 as well as other complications3. Moreover, fine needle biopsy has been shown to be less accurate in distinguishing WTs from parotid malignancies7. In an era of minimizing the invasiveness of surgical treatment, alternative methods are being sought to accurately differentiate between benign and malignant lesions, while also reducing patient suffering and therapeutic costs. Since previous attempts to utilize conventional MRI to distinguish WTs from parotid malignancies have proven unsuccessful15, great hopes are being pinned on the application of novel dynamic imaging techniques. The results from previous research imply that dynamic contrast enhanced MRI (DCE-MRI) can be applied to differentiate parotid tumors. This is primarily based on the finding that time-signal intensity curves (TICs) for malignant tumors and the two commonest benign lesions, pleomorphic adenomas (PAs) and WTs, differ markedly, especially in terms of the time to peak enhancement (Tpeak) and washout rate values (WR). According to literature, PAs show a gradual enhancement (high Tpeak) followed by a slow contrast washout (low WR)14,16,17,18. In contrast, WTs and malignant lesions are characterized by an early enhancement (low Tpeak) followed by a rapid17,19,20 or gradual washout, respectively21,22, which results in high or low WR. However, majority of these studies were limited due to inclusion of relatively small cohorts, providing inconclusive results, especially with regards to Tpeak cut-off values for achieving optimal accuracy in distinguishing WTs from parotid malignancies.
We verified the accuracy of the existing radiological criteria for differentiating between WTs and parotid malignancies, using our relatively large database of patients subjected to preoperative DCE-MRI and treated surgically for parotid tumors. The aim of this study was to define an optimal algorithm for the differential diagnostics of these two groups of lesions on the basis of DCE-MRI.
Material and methods
This study included 100 consecutive patients with parotid tumors, treated surgically at the Department of Otolaryngology, Medical University of Gdansk, between 2013 and 2014. 41 men and 59 women aged between 18 and 88 years (mean age 56.1 ± 15.8 years) were included in the analysis. The protocol of the study was approved by the Local Bioethics Committee at the Medical University of Gdansk, and all patients gave their written informed consent to participate in the project. Authors confirm that all research was performed in accordance with relevant guidelines/regulations. Research was performed in accordance with the Declaration of Helsinki.
Prior to the surgery, all patients underwent fine needle biopsy of the parotid tumor. Both biopsy and surgical specimens were subjected to routine cytological and histological examination at the Department of Pathomorphology, Medical University of Gdansk. Moreover, all patients routinely underwent preoperative multiparametric MRI.
Image acquisition and processing
All MRI examinations were performed using a 1.5 T scanner (Magnetom Aera, Siemens, Erlangen, Germany) using a head coil. Table 1 displays the applied MRI examination protocol. To obtain contrast-enhanced sequences, gadolinium-based contrast agent, gadobutrol, (Gadovist, Bayer Schering Pharma, Berlin, Germany) was utilized at standard dose of 0.1 mmol/body weight (0.1 ml/body weight) at a rate of 2–3 ml/s, followed by a 20-ml saline flush. No adverse reactions occurred following contrast administration.
Diffusion restriction was evaluated qualitatively based on increasing signal intensity with growing b factor in DWI sequence, along with low apparent diffusion coefficient (ADC) values. ADC values were measured using ADC maps, which were generated automatically with commercially available Siemens software (SyngoVia) by manually placing the region of interest (ROI) over the tumor area.
Dynamic contrast enhanced sequences were obtained with 36 repetitions over 226 s. DCE-MRI analysis was based on time-signal intensity curves (TIC) obtained with the above mentioned software (Siemens SyngoVia, MeanCurve tool) by placing ROI over the lesion. In the case of heterogeneous lesions, ROI was carefully placed to exclude cystic/necrotic/calcified areas and blood vessels. The mean size of ROI was approximately 3–4 mm. The MeanCurve tool provided graphical as well as numerical representation of the enhancement pattern, which enabled further mathematical calculations of Tpeak and WR.
Image analysis
All radiological images and obtained data were evaluated by two independent radiologists with prior experience in Head and Neck Radiology. The radiologists were blinded to the clinical history of the patient, and results of fine needle biopsy and histopathological analysis. The number and topography of the lesions as well as their morphology, including tumor size, signal intensity on T2-, T1-weighted and T1-weighted images with fat saturation and homogeneity were assessed. Additionally, ADC values for the tumor and normal parotid were measured and enhancement pattern assessed with calculation of TICs in order to establish a radiological diagnosis. The obtained TICs were classified according to criteria utilized by Yabuuchi et al.23, on the basis of Tpeak and WR: A) gradual enhancement (Tpeak > 120 s, WR < 10%, typical for 75% of PA and other adenomas), B) early enhancement and high washout (Tpeak < 120 s, WR > 30%, typical for WTs), C) early enhancement and low washout (Tpeak < 120 s, WR < 30%, characteristic for malignant tumors), and D) no enhancement (flat curve, specific for cystic lesions). Presence of lymphadenopathy and signs of perineural spread was also reported.
Statistical analysis
Normal distribution of continuous variables was verified using the Kolmogorov–Smirnov test. Depending on the type of distribution, statistical characteristics of continuous variables were presented either as arithmetic means and standard deviations (SD) or medians and ranges. Statistical characteristics of discrete variables were presented as distributions of numbers and percentages. Significance of intergroup differences in the characteristics of continuous variables was verified using the Student’s t-test or Mann–Whitney U test, while Pearson’s chi-squared test or Fisher’s exact test were used for intergroup comparisons of discrete variables. Accuracy of DCE-MRI parameters (Tpeak and WR) in differential diagnostics of WTs and malignant lesions was determined in relation to the gold standard, i.e., histological diagnosis. ROC analysis was conducted to determine sensitivity and specificity of DCE-MRI with various cut-off values for Tpeak and WR, as well as the area under ROC curve (AUC) and its 95% confidence interval (95% CI). The accuracy of DCE-MRI with various combinations of cut-off values for Tpeak and WR was determined on the basis of expected values from bivariate logistic regression analysis. All calculations were carried out using Statistica 10 package (StatSoft, USA), with the threshold of statistical significance set at p ≤ 0.05.
Ethical approval
All procedures performed in this studu involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The protocol of the study was approved by the Local Bioethics Committee at the Medical University of Gdansk (NKBBN/591/2013).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Results
One hundred patients with parotid tumors, operated between 2013 and 2014, were included in this study. Of these, 19 individuals had postoperative histopathological examination confirmed presence of malignant lesion (Table 2) while 36 were diagnosed with WTs. This subset of patients comprised of 31 men and 24 women aged between 25 and 88 years (mean age 62.2 ± 13.5). The lesions eventually identified as WTs were characterized by significantly lower median Tpeak (40.25 s [range 31.90–209.58 s] vs 181.48 s [39.61–255.32 s], p < 0.001) and significantly higher median washout rate (30.17% [1.85–41.29%] vs 2.91% [0–35.7%], p < 0.001) than malignant lesions.
During the first stage of the analysis, the accuracy of Tpeak = 60 s and Tpeak = 120 s for differentiating WTs from parotid malignancies was compared. These cut-off values for Tpeak were previously used by Takashima et al.24 (Tpeak = 60 s), Yabuuchi et al.23 and Hisatomi et al.14 (Tpeak = 120 s). Using cut-off values of Tpeak = 60 s and Tpeak = 120 s, we correctly identified 16/19 and 11/19 malignant tumors, respectively, and 31/36 and 34/36 WTs, respectively. Upon analyzing the distributions of malignant lesions and WTs within subgroups identified based on these cut-off values, we found that both criteria were able to accurately distinguish between these histological types (p < 0.001) (Table 3). ROC analysis showed that DCE-MRI with cut-off value Tpeak = 60 s provided 84.2% sensitivity and 86.1% specificity for identification of malignant tumors (AUC = 0.852, 95% CI 0.736–0.968). While the sensitivity and specificity with cut-off value Tpeak = 120 s were 57.9% and 94.4%, respectively (AUC = 0.762, 95% CI 0.613–0.910) (Fig. 1).
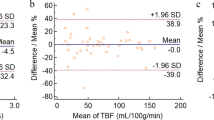
Subsequently, the accuracy of WR = 30% and WR = 40% for differentiating between malignant lesions and WTs was also analyzed. These cut-off values were previously used by Yabuuchi et al.23 (WR = 30%) and Hisatomi et al.14 (WR = 40%). WR = 30% was found to be a significant predictor of tumor type, enabling us to correctly identify 18/19 malignant lesions and 20/36 WTs (p < 0.001). ROC analysis revealed that DCE-MRI with this cut-off value provided 94.7% sensitivity and 55.6% specificity for identification of malignant tumors (AUC = 0.751, 95% CI 0.623–0.880) (Fig. 1). While cut-off of WR = 40% did not assist in discriminating between WTs and malignant lesions (p = 0.286) (Table 3).
During the next stage, the accuracy of TICs defined on the basis of the abovementioned cut-off values for Tpeak and WR were analyzed. We defined TICs based on two sets of cut-off values: Tpeak = 120 s/WR = 30% as previously used by Yabuuchi et al.23, and our original set Tpeak = 60 s/WR = 30%. We did not analyze the sets with cut-off value WR = 40% since it did not significantly discriminate between WTs and malignant lesions. The distributions of TICs obtained on the basis of these two sets are presented in Table 3. The AUC for DCE-MRI with these cut-off values were 0.873 (95% CI 0.771–0.975) for Tpeak = 60 s/WR = 30% and 0.854 (95% CI 0.748–0.960) for Tpeak = 120 s/WR = 30% (Fig. 1). The sensitivity and specificity were 84.2% and 86.1% for Tpeak = 60 s/WR = 30%, and 57.9% and 94.4% for Tpeak = 120 s/WR = 30%, respectively.
Lastly, ROC analysis was conducted to identify cut-off values for Tpeak and WR providing maximum sensitivity and specificity for identifying malignant tumors in our series. While the cut-off value for Tpeak was the same as in previous studies dealing with the issue at hand (Tpeak = 60 s), the cut-off value for WR was markedly lower (WR = 13%). Using this cut-off value, we were able to identify correctly 16/19 malignant lesions and 31/36 WTs (p < 0.001) (Table 3). ROC analysis showed that DCE-MRI with this cut-off value provided 84.2% sensitivity and 86.1% specificity in identification of parotid malignancies in our series (AUC = 0.852, 95% CI 0.736–0.968) (Fig. 1).
During the last stage, we verified the accuracy of TICs defined with the cut-off values Tpeak = 60 s and WR = 13% (Table 4). The AUC with these cut-off values was 0.880 (95% CI 0.776–0.984) (Fig. 1), and the sensitivity and specificity were 78.9% and 88.9%, respectively.
Discussion
Majority of the studies on the application of DCE-MRI in the differential diagnostics of parotid tumors are based on two parameters, Tpeak and WR. As mentioned previously, these two parameters are sufficient for determining the type of TIC for a given lesion. Elmokadem et al. evaluated the value of multiparametric MRI for parotid tumor diagnostics. The study proved that the TIC type based on DCE-MRI significantly differentiates between benign and malignant lesions (p < 0.001) and has diagnostic accuracy of 96.55%. Additionally, no statistically significant difference was found between the ADC values of benign and malignant lesions25. Through our study, we aimed at determining whether the subset of “low” Tpeak values traditionally assigned to both WTs and parotid malignancies17,19,20,21,22, includes some values which are specific solely for one of these groups. Our analysis demonstrates that the cut-off value for Tpeak which most accurately differentiates between WTs and parotid malignancies was Tpeak = 60 s. Using Tpeak > 60 s as the only diagnostic criterion, we correctly identified 16/19 (84.2%) malignant tumors, while achieving false-positive results in 5/21 (23.8%). To the best of our knowledge, the role of Tpeak as the only parameter of DCE-MRI for distinguishing between these tumors was studied in only a few studies25,26,27. Moreover, only Takashima et al. analyzed the accuracy of Tpeak cut-off value at 60 s24. Using this cut-off value, they correctly identified 6/11 (54.5%) malignant parotid tumors, with the false-positive rate of 2/8 (25.0%).
However, differential diagnostics of parotid tumors is typically based on simultaneous analysis of two DCE-MRI parameters Tpeak and WR28. Therefore, our study additionally aimed at identifying a cut-off value for WR, which if analyzed in combination with Tpeak = 60 s, would provide the highest accuracy for differentiating WTs and parotid malignancies based on radiological imaging. In previous studies on this topic, a lesion was considered malignant whenever its Tpeak was > 120 s and its WR > 30% or > 40%. The principal limitation of these studies stemmed from the fact that they included PAs in addition to WTs and malignant lesions. Due to their specific microscopic structure, the TICs of PAs have markedly different characteristics. Our study, limited solely to WTs and malignant lesions, showed that the sensitivity of DCE-MRI for radiologically differentiating these lesions can be improved by 26% by using cut-off values Tpeak = 60 s and WR = 30%. Importantly, ROC analysis revealed that the cut-off value for WR, which most accurately distinguishes WTs from malignant lesions was 13%. However, further analysis showed that an increase in AUC resulted due to a slight improvement in the specificity of DCE-MRI, but at the expense of its sensitivity (Fig. 2). Consequently, we did not find sufficient evidence to decrease the cut-off value for WR below 30%, especially since false-negative diagnosis of a malignant lesion as a WTs has considerably more devastating consequences than too extensive surgery inadvertently performed in the patient with false-positive diagnosis of a malignancy.
Besides showcasing a potential way to improve DCE-MRI accuracy for parotid tumor diagnostics, our study also revealed some drawbacks of this modality. To this date, majority of lesions with Tpeak > 120 s were considered PAs14,23. However, our study showed that this cut-off value was also exceeded in as many as 11/19 (57.9%) parotid malignancy cases. This observation is consistent with the results of a small study conducted by Tsushima et al.29. Among nine parotid malignancies examined by DCE-MRI, the authors identified two adenoid cystic carcinomas whose TICs closely resembled those traditionally assigned to PAs (Tpeak > 240 s). In our subset of 19 parotid malignancies, there were also two adenoid cystic carcinomas, one of which had Tpeak value of 235 s. Altogether, these findings imply that characteristics of parotid tumors determined on DCE-MRI are likely modulated by their histological type and perhaps also clinical stage. Previous studies have showed that Tpeak is inversely correlated with microvessel density in the examined tissue, and that WR increases proportionally to the connective tissue content30. Patella et al. investigated heterogeneity of intravoxel incoherent motion (IVIM) and DCE-MRI biomarkers in differentiating WTs and PAs. They found statistically significant differences for all histogram parameters and suggested that this was a result of wider capillary network in WTs than in PAs31. Based on this data, it can be hypothesized that some rapidly growing malignant tumors can present with extremely high Tpeak and low WR, and as such may be misdiagnosed as PAs. Since only 1/19 parotid malignancy case in our series showed WR > 30%, this cut-off value seems to be a key diagnostic criterion for benign lesions. In the case of remaining tumors, the final decision on the type and extent of their resection should be established on the basis of cytological examination.
Conclusions
The use of a different diagnostic algorithm than in the case of PAs, i.e., lower cut-off value for Tpeak (= 60 s), appears to markedly increase the sensitivity of DCE-MRI in differentiating parotid malignancies and WTs. However, it is the WR value of > 30% which seems to be a key diagnostic criterion for benign lesions, as some parotid malignancies subjected to dynamic MRI may show features traditionally associated with PAs (Tpeak > 120 s).
References
Przewozny, T. & Stankiewicz, C. Neoplasms of the parotid gland in northern Poland, 1991–2000: an epidemiologic study. Eur. Arch. Otorhinolaryngol. 261, 369–375 (2004).
Spiro, R. H. Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg. 8, 177–184 (1986).
Batsakis, J. G. & el-Naggar, A. K. Warthin’s tumor. Ann. Otol. Rhinol. Laryngol. 99, 588–591 (1990).
Eveson, J. W. & Cawson, R. A. Warthin’s tumor (cystadenolymphoma) of salivary glands. A clinicopathologic investigation of 278 cases. Oral Surg. Oral Med. Oral. Pathol. 61, 256–262 (1986).
Kotwall, C. A. Smoking as an etiologic factor in the development of Warthin’s tumor of the parotid gland. Am. J. Surg. 164, 646–647 (1992).
Yoo, G. H., Eisele, D. W., Askin, F. B., Driben, J. S. & Johns, M. E. Warthin’s tumor: a 40-year experience at The Johns Hopkins Hospital. Laryngoscope 104, 799–803 (1994).
Parwani, A. V. & Ali, S. Z. Diagnostic accuracy and pitfalls in fine-needle aspiration interpretation of Warthin tumor. Cancer 99, 166–171 (2003).
Batsakis, J. G. Carcinoma ex papillary cystadenoma lymphomatosum. Malignant Warthin’s tumor. Ann. Otol Rhinol. Laryngol. 96, 234–235 (1987).
Heller, K. S. & Attie, J. N. Treatment of Warthin’s tumor by enucleation. Am. J. Surg. 156, 294–296 (1988).
Stewart, C. J., MacKenzie, K., McGarry, G. W. & Mowat, A. Fine-needle aspiration cytology of salivary gland: a review of 341 cases. Diagn. Cytopathol. 22, 139–146 (2000).
Flezar, M. & Pogacnik, A. Warthin’s tumour: unusual vs. common morphological findings in fine needle aspiration biopsies. Cytopathology 13, 232–241 (2002).
Que Hee, C. G. & Perry, C. F. Fine-needle aspiration cytology of parotid tumours: is it useful?. ANZ J. Surg. 71, 345–348 (2001).
Zbaren, P., Schar, C., Hotz, M. A. & Loosli, H. Value of fine-needle aspiration cytology of parotid gland masses. Laryngoscope 111, 1989–1992 (2001).
Hisatomi, M. et al. Diagnostic value of dynamic contrast-enhanced MRI in the salivary gland tumors. Oral Oncol. 43, 940–947 (2007).
Minami, M. et al. Warthin tumor of the parotid gland: MR-pathologic correlation. AJNR Am. J. Neuroradiol. 14, 209–214 (1993).
Hisatomi, M. et al. Assessment of pleomorphic adenomas using MRI and dynamic contrast enhanced MRI. Oral Oncol. 39, 574–579 (2003).
Joe, V. Q. & Westesson, P. L. Tumors of the parotid gland: MR imaging characteristics of various histologic types. AJR Am. J. Roentgenol. 163, 433–438 (1994).
Traxler, M., Hajek, P., Solar, P. & Ulm, C. Magnetic resonance in lesions of the parotid gland. Int. J. Oral Maxillofac. Surg. 20, 170–174 (1991).
Hisatomi, M. et al. Assessment of dynamic MRI of Warthin’s tumors arising as multiple lesions in the parotid glands. Oral Oncol. 38, 369–372 (2002).
Ikarashi, F., Nakano, Y., Nonomura, N. & Kawana, M. Radiological findings of adenolymphoma (Warthin’s tumor). Auris Nasus Larynx 24, 405–409 (1997).
Asaumi, J. et al. Assessment of carcinoma in the sublingual region based on magnetic resonance imaging. Oncol. Rep. 9, 1283–1287 (2002).
Park, J. et al. Salivary gland masses: dynamic MR imaging and pathologic correlation. Nippon Igaku Hoshasen Gakkai Zasshi 57, 581–585 (1997).
Yabuuchi, H. et al. Salivary gland tumors: diagnostic value of gadolinium-enhanced dynamic MR imaging with histopathologic correlation. Radiology 226, 345–354 (2003).
Takashima, S., Noguchi, Y., Okumura, T., Aruga, H. & Kobayashi, T. Dynamic MR imaging in the head and neck. Radiology 189, 813–821 (1993).
Elmokadem, A. H. et al. Diagnostic accuracy of multiparametric magnetic resonance imaging for differentiation between parotid neoplasms. Can. Assoc. Radiol. J. 70(3), 264–272 (2019).
Yabuuchi, H. et al. Characterization of parotid gland tumors: added value of permeability MR imaging to DWI and DCE-MRI. Eur. Radiol. 30, 6402–6412 (2020).
Coudert, H., Mirafzal, S., Dissard, A., Boyer, L. & Montoriol, P.-F. Multiparametric magnetic resonance imaging of parotid tumors: A systematic review. Diagn. Interv. Imaging 102(3), 121–130 (2021).
Xu, Z., Zheng, S., Pan, A., Cheng, X. & Gao, M. A multiparametric analysis based on DCE-MRI to improve the accuracy of parotid tumor discrimination. Eur. J. Nucl. Med. Mol. Imaging 46, 2228–2234 (2019).
Tsushima, Y., Matsumoto, M., Endo, K., Aihara, T. & Nakajima, T. Characteristic bright signal of parotid pleomorphic adenomas on T2-weighted MR images with pathological correlation. Clin. Radiol. 49, 485–489 (1994).
Murakami, T. et al. Contrast-enhanced MR imaging of intrahepatic cholangiocarcinoma: pathologic correlation study. J. Magn. Reson. Imaging 5, 165–170 (1995).
Patella, F. et al. Quantification of heterogeneity to classify benign parotid tumors: a feasibility study on most frequent histotypes. Future Oncol. 16(12), 763–778 (2020).
Funding
No founding for this work was received.
Author information
Authors and Affiliations
Contributions
B.M., E.S.: concept and design of the study, data analysis, data interpretation, drafting the manuscript for intellectual content, revision the manuscript. K.M., A.S., D.S: major role in data acquisition, interpretation of the data. E.G., J.P.: acquisition of data, interpretation of the data, drafting the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mikaszewski, B., Markiet, K., Smugała, A. et al. Value of dynamic contrast enhanced MRI in differential diagnostics of Warthin tumors and parotid malignancies. Sci Rep 11, 16282 (2021). https://doi.org/10.1038/s41598-021-95820-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-95820-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.