Abstract
Most published newborn growth references are based on conventional monitoring data that usually included both low- and high-risk pregnancies. We sought to develop a set of neonatal growth standards constructed from only a large sample of low-risk pregnancies. A total of 24,375 naturally conceived singleton live births with gestational ages of 24–42 weeks were collected in 69 hospitals in thirteen Chinese cities between 2015 and 2018. Unhealthy infants or those with high-risk mother were excluded. Smoothed percentile curves of six anthropometric indicators were established using the Generalized Additive Model for Location, Scale and Shape. The 3rd, 10th, 25th, 50th, 75th, 90th, and 97th percentile references for birth weight, length, head circumference, weight/length, body mass index, and ponderal index were calculated for neonates with gestational ages of 24–42 weeks. This set of neonatal growth standards with six anthropometric indicators can provide more tools for growth and nutrition assessment and body proportionality in neonatal clinical practice. These standards might also help to show the differences between growth curves based on low-risk and mixed low- and high-risk pregnancies.
Similar content being viewed by others
Introduction
Intrauterine growth is associated with infant survival, future growth and development, and health conditions. An appropriate growth standard or reference is an essential tool for neonatal growth assessment at birth. Therefore, some countries have established newborn growth standards based on low-risk pregnancies with a normal outcome1,2 or newborn growth references based on mixed low- and high-risk pregnancies3,4,5,6. Whether sample population are drawn from low-risk pregnancies or mixed low- and high-risk pregnancies is the key to distinguish growth standards and growth references7,8. The sample populations for growth standards are selected based on relatively healthy and adequately nourished pregnant women and represent relative healthy patterns of growth of neonates that can answer how infants ought to grow rather than how they do grow9. Considering the difference of the reference samples, a standard may have more clinical utility than a population reference8.
The growth reference for Chinese newborns constructed in 198810 is ill-suited for assessing the growth and development of today’s Chinese newborns due to several limitations. Recent monitoring data has shown that the growth level of newborns is substantially higher compared to the 1988 reference11,12,13. Further, the 1988 reference only covers newborns with a gestational age (GA) of greater than 28 weeks, which does not meet the current need of assessing infants with a GA of less than 28 weeks as more extremely preterm babies are being born. To overcome these limitations, we aimed to develop a set of growth standards for neonates with GA of 24–42 weeks based on a large sample of low-risk pregnancies. Three commonly used indicators—birth weight, length, and head circumference—that allowed better definition of small for GA (SGA) and large for GA (LGA) were employed. In addition, three anthropometric ratios—weight/length, body mass index (BMI), and ponderal index (PI)—that allowed for better assessment of symmetric vs asymmetric abnormalities in growth were utilized. We also examined the differences among our standards, the INTERGROWTH-21st standards1,14,15 and the new US curves4,16.
Materials and methods
Subject
From June 2015 to November 2018, a cross-sectional survey of newborn babies with a GA of 24–42 weeks in 13 cities in China was carried out. Of these 13 cities, nine, including Beijing, Harbin, Xi’an, Shanghai, Nanjing, Wuhan, Guangzhou, Fuzhou, and Kunming, were selected to investigate newborn babies with GA of 24–42 weeks. These nine cities were also the sample cities on the National Survey on the Physical Growth and Development of Children in China, which was a representative national survey of the country17. Considering the low numbers of extremely and early preterm babies, four cities in the surrounding regions of the nine cities including Tianjin, Shenyang, Changsha, and Shenzhen were added to supplement the sample sizes of preterm babies with GA of 32 weeks and below.
Single naturally conceived live births with a GA of 24–42 weeks were included. Infants who were not healthy or whose mothers were at high health risk were excluded according to the following exclusion criteria: ① unclear GA; ② severe congenital malformation at birth or known chromosomal abnormality; ③ edema or hematoma during physical measurement; ④ parents of non-Chinese origin; ⑤ mothers were not permanent residents in surveyed cities and lived in surveyed cities for < 2 years; ⑥ maternal height < 145 cm; ⑦maternal age < 18 years or > 40 years; ⑧ mothers who were smoking, alcoholic or drug dependent over the three months before or during pregnancy; ⑨ mothers who had continuously taken adrenal cortex hormones or other immunosuppressive agents for > 1 month during pregnancy; ⑩ mothers of full-term babies with any of the following conditions during pregnancy: severe anemia (Hb ≦ 60 g/L), gestational diabetes, preeclampsia, eclampsia, hyperthyroidism or hypothyroidism, heart and kidneys dysfunction, chronic hypertension; ⑪ mothers of preterm babies with any of the following conditions during pregnancy: severe anemia (Hb ≦ 60 g/L), gestational diabetes that cannot be effectively controlled by diet and exercise intervention, severe preeclampsia, eclampsia, hyperthyroidism or hypothyroidism that cannot be effectively controlled by drug therapy, severe heart and kidneys dysfunction.
GA was jointly determined based on the mother’s last menstrual period (LMP) and the results of ultrasound examination in the first three months of pregnancy. GA based on LMP was used when the GA difference between the two methods was ≦ 1 week, and GA based on ultrasound examination was used when the GA difference was > 1 week. GA groups were divided by week, such as 24+0 to 24+6 weeks for the 24 week GA group.
Sample size was estimated according to both statistical accuracy requirements for establishing percentile curves and observed numbers of newborns at each GA. For full-term babies with GA of 37–41 weeks, the sample size for each GA group was about 100 per sex and city; for preterm babies with GA of 29–36 weeks, the sample size for each GA group was about 50. Full-term babies with GA of 37–41 weeks were sampled by cluster sampling. Samples were evenly distributed by season, and babies randomly selected from each season. All eligible full-term babies with GA ≧ 42 weeks or preterm babies with GA ≦ 28 weeks within selected hospitals were included in this study. The study was reviewed and approved by the Ethics Committees of the Capital Institute of Pediatrics (No.SHERLL-2015009). Written informed consent at the top of questionnaires was obtained from all respondents (i.e., parents of the newborns). All methods were performed in accordance with the relevant guidelines and regulations.
Measurement
Birth weight was measured within 12 h of birth with an electronic scale (maximum range 20 kg, accurate to 10 g). Birth recumbent length was measured within 24 h with infantometer (maximum range 65 cm, accurate to 0.1 cm) for term babies and preterm babies of large GA and new patent infantometer (Patent No. zl201520996396.X) (maximum range 45 cm, accurate to 0.1 cm) for preterm babies of small GA. Birth head circumference was measured within 24 h with a flexible non-stretchable plastic tape (0.7 cm wide, maximum range 100 cm, accurate to 0.1 cm). Birth weight, length, and head circumference were measured twice and recorded twice in a standardized measurement procedure18. Each measurement was collected independently by two trained doctors or nurses. If the difference between the two measurements exceeded the maximum allowable difference (weight 10 g, length 0.5 cm, head circumference 0.5 cm), a third measurement was taken, and then those two measurements not exceeding the allowable difference were recorded.
Quality control
Uniform measuring tools were equipped for all sites, including infantometer and new patent infantometer for length measurement, non-stretchable plastic tape for head circumference measurement, standard weights (accuracy 10 g, 50 g, 100 g, 500 g) for calibration of electronic scale, and standard steel tape (accuracy 1 mm) for calibration of infantometer and plastic tape. The electronic scales in each site were used for investigation after evaluation and calibration of standard weights with a maximum allowable difference of 10 g. Calibration was taken every week with maximum allowable differences of weight 10 g, length 0.5 cm, and head circumference 0.5 cm. Questionnaires were completed by pairs of trained doctors or nurses, with one recording the answers and the other reviewing. The completed questionnaires in each city were sent to the Beijing Steering Committee for final check and data entry. EpiData 3.0 software was used for double entry and logic check of the questionnaires.
Statistical analysis
The mean of two measurements for birth weight, length and head circumference was used for data analysis and calculation of anthropometric ratio. Weight/length, BMI, and PI were calculated according to the following formula: [weight (kg)/length (m)], [weight (kg)/length (m)2], and [weight (kg)/length (m)3], respectively. During data cleaning, we excluded 2 missing weight values, 8 missing length values, and 16 missing head circumference values. Few measures not within ± 5 standard deviation (SD) of the mean of overall sex- and GA-specific values was also excluded (12 for weight, 17 for length, 10 for head circumference, 29 for weight/length, 49 for BMI, and 208 for PI). The final sample sizes contributing to the establishment of the growth curves for each indicator are listed below: weight (13,192 males and 11,169 females), length (13,183 and 11,167), head circumference (13,181 and 11,168), weight/length (13,176 and 11,159), BMI (13,162 and 11,153), and PI (13,075 and 11,081). During the establishment of the growth curves, normality test, and skewness and kurtosis analysis were assessed for each indicator. Data analyses used SAS v9.4 (SAS Institute Inc).
The Generalized Additive Model for Location, Scale and Shape (GAMLSS) which is a general framework for fitting regression models where the distribution of the response variable allows for highly skewed and kurtotic continuous distribution19, was employed to establish smoothed percentile growth curves of male and female newborn babies with GA of 24–42 weeks. Curve fitting was performed using the GAMLSS 4.3–1 library running under R 3.1.2. Goodness of fit of the GAMLSS models was assessed by the Schwarz Bayesian Information Criterion that is justified as a general criterion for model selection and by Q-Q plots that assesses the age-conditional normality of the transformed data20,21. After comparative testing of alternative methods (ie, distribution transformation and smoothing function) used to generate the growth curves, birth weight, weight/length, BMI, and PI percentile curves were established using the GAMLSS with Box-Cox t (BCT) distribution with cubic splines, and birth length and head circumference using the GAMLSS with Box-Cox power exponential (BCPE) distribution with cubic spline. All these GAMLSS models did not need to be weighted because the difference of each indicator between non-weighting and equal proportional weighting were negligibly small16. The differences between fitted percentiles and empirical values at each week were examined for all the six anthropometric indicators.
Results
Basic characteristics of the reference sample
A total of 24,375 singleton live births with GA of 24–42 weeks were collected in 69 hospitals in 13 Chinese cities, including 12,264 preterm babies (7,042 males and 5,222 females) and 12,111 full-term babies (6,155 males and 5,956 females). Table 1 presents sample sizes and means (SD) of birth weight, length, and head circumference by sex and GA. Table 2 presents sample sizes of the 13 cities by city and GA. 61.4% of newborn babies were delivered vaginally and 38.6% by cesarean section. The proportion for first births was 65.9% and for second and higher 34.1%. Mothers with high school and college degrees accounted for 84.8% of the sample population, and childbearing age was 31.5 (± 5.0) years. Average maternal height was 161.0 (± 5.0) cm, pre-pregnancy BMI was 21.0 (± 3.0) kg/m2, and weight gain during pregnancy was 13.8 (± 5.0) kg.
Percentile reference values of six anthropometric indicators
Tables 3, 4, 5, 6, 7 and 8 present the 3rd, 10th, 25th, 50th, 75th, 90th, and 97th percentile reference values of weight for GA, length for GA, head circumference for GA, weight/length for GA, BMI for GA, and PI for GA for male and female newborns with GA of 24–42 weeks. All the six anthropometric indicators increased rapidly with GA, but growth velocity decreased slightly after 37 weeks.
Comparison of fitted centile curves and observed empirical values
Figure 1A to F demonstrates the comparison of smoothed fitted centiles and observed empirical values of birth weight, length, head circumference, weight/length, BMI, and PI by sex and GA, showing almost identical values with very few exceptions at the lower end of GA distribution where only a small number of individual measures could be obtained, i.e., at 24–26 weeks of gestation.
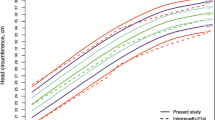
Comparison of the China standards with the INTERGROWTH-21st standards
Overall, the percentile curves of birth weight, length, head circumference, and weight/length in China presented similar growth trajectories with the INTERGROWTH-21st standards, but also expressed distinct differences for length at 37–42 weeks and weight/length at 24–32 weeks (Fig. 2A to D).
Comparison of the China standards with the new US curves
There are small differences for the percentile curves of birth weight, length, and head circumference at 24–36 weeks between China and US curves, but considerable differences at 37–41 weeks, especially at the upper centiles (e.g., 90th); and there is a large disparity for birth BMI from 24 to 41 weeks (Fig. 3A to D).
Discussion
The reference sample of our standards derive from a population-based survey of newborns from economically developed urban areas with strict criteria for inclusion, such as single live birth, naturally conception, and health condition of both the mother and the newborn. The shapes of growth curves based on low-risk pregnancies with a normal outcome may differ from those of growth curves generated from more conventional data sets that include both low- and high-risk pregnancies. These differences mainly reflect the variations in the distance between the lowermost and uppermost centiles (e.g., 3rd and 97th). For example, the distance in our weight curves from low-risk individuals was shorter compared to other weight curves from Chinese routine monitoring data that included both low- and high-risk individuals11,12. Similar to our observations, new and improved Dutch birth weight percentile curves based on data from low-risk pregnancies displayed lower range/variation, which proved to be more effective in identifying clinically important risk SGA infants2,22.
The health of the mother and the newborn is the foundation of sustainable development for individuals, families, and societies as it is closely linked with health throughout life23. Assessment of growth and nutrition of the neonates is essential for a positive outcome in later life. However, no single anthropometric measure fully reflects growth, development and health of newborn babies, so we established percentile curves of multiple anthropometric measures, with each measure revealing distinct relationships with specific health risks or diseases. Birth weight is typically used to define the classification of newborn size as small, appropriate, or large for a specified GA at birth24. Birth length is helpful in evaluating whether postnatal catch-up growth is appropriate25,26. Birth head circumference reflects intrauterine brain development and predicts the prognosis of nervous system development27. A consensus was reached on the definition of growth restriction as birth weight < 3rd percentile or at least 3 out of 5 of the following: birth weight < 10th percentile, length < 10th percentile, head circumference < 10th percentile, prenatal diagnosis of fetal growth restriction, and maternal pregnancy complications28. Traditional classification based on birth weight centiles for GA does not reflect body fat in both term and preterm newborns29, while weight/length greatly aids in predicting newborn fat mass and fat-free mass as well as body proportionality15,30. BMI is useful for measuring body proportionality for newborn infants30,31,32. PI is a customary measure to evaluate whether abnormalities in growth in preterm infants are symmetric or asymmetric33,34,35. In sum, our established reference values of six indicators can provide more tools for growth and nutrition assessment (e.g., frequently using weight, length and head circumference) and nutrition assessment/body proportionality (e.g., frequently using weight/length, BMI and PI) in neonatal clinical practice.
Our study has several strengths. First, our standards were based on low-risk pregnancies with a normal outcome. Second, besides the commonly used weight, length, and head circumference, we also established percentile curves of weight/length, BMI, and PI that help assess whether abnormal babies in growth are symmetric or asymmetric. Under strict exclusion criteria, we included a relatively large sample size of preterm infants that guaranteed more reliable percentile curves; however, the screening efficacy of this set of new standards for SGA or LGA and body proportionality still needs to be further validated and evaluated.
Based on a contemporary, large-scaled, population-based cross-sectional nationally representative sample from low-risk pregnancies with a normal outcome that represents optimal intrauterine growth, we developed a set of neonatal growth standards for 24–42 weeks of gestation, including reference values of six anthropometric indicators that can provide more tools for growth and nutrition assessment and body proportionality in neonatal clinical practice. In addition, our study aids in better understanding the differences in the shapes of growth curves between based on data from low-risk pregnancies only or from mixed low- and high-risk pregnancies.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to the confidential policy of our institute and hospital but are available from the corresponding author on reasonable request.
References
Villar, J. et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 384(9946), 857–868 (2014).
Hoftiezer, L. et al. From population reference to national standard: New and improved birthweight charts. Am. J. Obstet. Gynecol. 220(4), 383.e1–17 (2019).
Cole, T. J., Williams, A. F., Wright, C. M. & RCPCH Growth Chart Expert Group. Revised birth centiles for weight, length and head circumference in the UK-WHO growth charts. Ann. Hum. Biol. 38(1), 7–11 (2011).
Olsen, I. E., Groveman, S. A., Lawson, M. L., Clark, R. H. & Zemel, B. S. New intrauterine growth curves based on United States data. Pediatrics 125(2), e214–e224 (2010).
Bertino, E. et al. Neonatal anthropometric charts: The Italian neonatal study compared with other European studies. J. Pediatr. Gastroenterol. Nutr. 51(3), 353–361 (2010).
Fenton, T. R. & Kim, J. H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 13, 59 (2013).
Kiserud, T. et al. The World Health Organization fetal growth charts: Concept, findings, interpretation, and application. Am. J. Obstet. Gynecol. 218(2S), S619–S629 (2018).
Zhang, J., Merialdi, M., Platt, L. D. & Kramer, M. S. Defining normal and abnormal fetal growth: Promises and challenges. Am. J. Obstet. Gynecol. 202(6), 522–528 (2010).
Cole, T. J. The development of growth references and growth charts. Ann. Hum. Biol. 39(5), 382–394 (2012).
Zhang, B., Feng, Z. & Zhang, L. An investigation on the physical development of neonates of various gestational age in 15 cities of China. Chin. J. Pediatr. 26(4), 206–208 (1988) ((in Chinese)).
Zhu, L. et al. Chinese neonatal birth weight curve for different gestational age. Chin. J. Pediatr. 53(2), 97–103 (2015) ((in Chinese)).
Dai, L. et al. Birth weight reference percentiles for Chinese. PLoS ONE 9(8), e104779 (2014).
Yao, F., Miao, H., Li, B., Wu, Y. & Zhao, Q. New birthweight percentiles by sex and gestational age in Southern China and its comparison with the INTERGROWTH-21st Standard. Sci. Rep. 8(1), 7567 (2018).
Villar, J. et al. INTERGROWTH-21st very preterm size at birth reference charts. Lancet 387(10021), 844–845 (2016).
Villar, J. et al. Body composition at birth and its relationship with neonatal anthropometric ratios: The newborn body composition study of the INTERGROWTH-21st project. Pediatr. Res. 82(2), 305–316 (2017).
Olsen, I. E. et al. BMI curves for preterm infants. Pediatrics 135(3), e572–e581 (2015).
Zhang, Y. Q. et al. The 5th national survey on the physical growth and development of children in the nine cities of China: Anthropometric measurements of Chinese children under 7 years in 2015. Am. J. Phys. Anthropol. 163(3), 497–509 (2017).
Zong, X. N. & Li, H. Establishment of growth standards for Chinese newborns by gestational ages: Study design and statistical methods. Chin. J. Evid. Based Pediatr. 15(4), 401–410 (2020) ((in Chinese)).
Rigby, R. A. & Stasinopoulos, D. M. Automatic smoothing parameter selection in GAMLSS with an application to centile estimation. Stat. Methods Med. Res. 23(4), 318–332 (2014).
Royston, P. & Wright, E. M. Goodness-of-fit statistics for age-specific reference intervals. Stat. Med. 19(21), 2943–2962 (2000).
van Buuren, S. & Fredriks, M. Worm plot: A simple diagnostic device for modelling growth reference curves. Stat. Med. 20(8), 1259–1277 (2001).
Hoftiezer, L. et al. Defining small-for-gestational-age: Prescriptive versus descriptive birthweight standards. Eur. J. Pediatr. 175(8), 1047–1057 (2016).
Qiao, J. et al. A Lancet Commission on 70 years of women’s reproductive, maternal, newborn, child, and adolescent health in China. Lancet S0140–6736(20), 32708–32712 (2021).
Schlaudecker, E. P. et al. Small for gestational age: Case definition & guidelines for data collection, analysis, and presentation of maternal immunisation safety data. Vaccine 35(48 Pt A), 6518–6528 (2017).
Taal, H. R. et al. Small and large size for gestational age at birth, infant growth, and childhood overweight. Obesity (Silver Spring) 21(6), 1261–1268 (2013).
Karlberg, J. & Albertsson-Wikland, K. Growth in full-term small-for-gestational-age infants: From birth to final height. Pediatr. Res. 38(5), 733–739 (1995).
Barbier, A. et al. New reference curves for head circumference at birth, by gestational age. Pediatrics 131(4), e1158–e1167 (2013).
Beune, I. M. et al. Consensus Based Definition of Growth Restriction in the Newborn. J. Pediatr. 196, 71–6.e1 (2018).
Schmelzle, H. R., Quang, D. N., Fusch, G. & Fusch, C. Birth weight categorization according to gestational age does not reflect percentage body fat in term and preterm newborns. Eur. J. Pediatr. 166(2), 161–167 (2007).
Davidson, S. et al. Body mass index and weight-for-length ratio references for infants born at 33–42 weeks gestation: A new tool for anthropometric assessment. Clin. Nutr. 30(5), 634–639 (2011).
Ferguson, A. N. et al. BMI is a better body proportionality measure than the ponderal index and weight-for-length for preterm infants. Neonatology 113(2), 108–116 (2018).
Williamson, A. L. et al. Longitudinal BMI growth curves for surviving preterm NICU infants based on a large US sample. Pediatrics 142(3), e20174169 (2018).
Villar, J. et al. The differential neonatal morbidity of the intrauterine growth retardation syndrome. Am. J. Obstet. Gynecol. 163(1 Pt 1), 151–157 (1990).
Cole, T. J., Henson, G. L., Tremble, J. M. & Colley, N. V. Birthweight for length: Ponderal index, body mass index or Benn index?. Ann. Hum. Biol. 24(4), 289–298 (1997).
Landmann, E., Reiss, I., Misselwitz, B. & Gortner, L. Ponderal index for discrimination between symmetric and asymmetric growth restriction: Percentiles for neonates from 30 weeks to 43 weeks of gestation. J. Matern. Fetal Neonatal Med. 19(3), 157–160 (2006).
Acknowledgements
We thank all participating hospitals and medical staff and all newborn babies and their parents for their cooperation in sample collection and physical measurement.
Expert Committee of the China National Newborn Growth Standards Project: Capital Institute of Pediatrics (Hui Li, principal investigator, Zong-Han Zhu, Ting Zhang, Yao-Hua Dai); Peking University First Hospital (Geng-Li Zhao, Qi Feng); Peking Union Medical College Hospital (Dan-Hua Wang); Beijing Obstetrics and Gynecology Hospital, Capital Medical University (Wei Zhang); Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (Jun Zhang); Children’s Hospital of Fudan University (Chao Chen); Shanghai Children’s Medical Center, Shanghai Jiao Tong University School of Medicine (Fan Jiang); Tongji Hospital Affiliated to Tongji Medical College, Huazhong University of Science and Technology (Xiao-Ping Luo); School of Public Health, Peking University (Ying-Dong Zheng); Chinese Center for Disease Control and Prevention (Shui-Gao Jin, Hui-Shan Wang, Li-Yun Zhao); Beijing Children’s Hospital, Capital Medical University (Jie Mi).
The Working Committee of the China National Newborn Growth Standards Project: We thank all administrative staff of Department of Maternal and Child Health of the National Health Commission of the People's Republic of China and health authorities of the surveyed cities.
Funding
This study was supported by the Maternal and Child Health Program of the National Health Commission of the People’s Republic of China (2015–42).
Author information
Authors and Affiliations
Consortia
Contributions
H.L., principal investigator, conceptualized and designed the study, supervised data collection and data analyses and reviewed the manuscript; X.N.Z. participated in study design and data collection, carried out the initial analyses and drafted the initial manuscript; Y.Q.Z. participated in study design, coordinated data collection, carried out the initial analyses and reviewed the manuscript; H.H.W. participated in study design and data collection and reviewed the manuscript; G.L.Z. participated in study design and coordinated data collection and reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zong, XN., Li, H., Zhang, YQ. et al. Construction of China national newborn growth standards based on a large low-risk sample. Sci Rep 11, 16093 (2021). https://doi.org/10.1038/s41598-021-94606-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94606-6
This article is cited by
-
Growth and development of children in China: achievements, problems and prospects
World Journal of Pediatrics (2024)
-
Height and body mass index trajectories from 1975 to 2015 and prevalence of stunting, underweight and obesity in 2016 among children in Chinese cities: findings from five rounds of a national survey
World Journal of Pediatrics (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.