Abstract
Congenital Heart Defects (CHDs) are associated with different patterns of malnutrition and growth retardation, which may vary worldwide and need to be evaluated according to local conditions. Although tetralogy of Fallot (TOF) is one of the first described CHDs, the etiology outcomes in growth and development of TOF in early age child is still unclear in most cases. This study was designed to investigate the growth retardation status of Chinese pediatric TOF patients under 5 years old. The body height, body weight and body mass index (BMI) of 262 pediatric patients (138 boys and 124 girls) who underwent corrective surgery for TOF between 2014 and 2018 were measured using conventional methods. The average body height, body weight and BMI of the patients were significantly lower than WHO Child Growth Standards, while the most affected was body height. Meanwhile, higher stunting frequency and greater deterioration of both the body height and weight happened in elder age (aged 13–60 months) rather than in infant stage (aged 0–12 months) among these patients. Our results confirmed that intervention should be given at early age to prevent the growth retardation of TOF patients getting severer.
Similar content being viewed by others
Introduction
Tetralogy of Fallot (TOF) is one of the most common Congenital Heart Defects (CHDs), named for French physician Dr. Etienne-Louis Arthur Fallot, who described a panel of three cyanotic patients in 1888 with four anatomical features: (1) stenosis of the pulmonary artery, (2) interventricular communication (VSD), (3) deviation of the origin of the aorta (overriding aorta), and (4) concentric right ventricular hypertrophy1,2,3,4. Based on a meta-analysis in 2011, TOF is the fourth prevailing CHD type worldwide with a prevalence of 0.34‰, constituting approximately 4% of CHD cases overall5. Situation of TOF in China differs. According to the national wide epidemiological survey of CHD in China directed by Hubei Women and Child Healthcare Hospital between 2015 and 2017, TOF is the most prevailing CHD type in new born children in China6.
Children with a range of chronic systemic health conditions often has significant adverse effects on body growth and development7. Indeed, different CHD types are associated with different patterns of malnutrition and growth retardation, which may be caused by prenatal and genetic factors, hypoxia and hemodynamic factors, and those relating to nutritional intake, metabolic requirements, and nutrient absorption7,8,9,10,11,12. As some of these factors may vary worldwide, CHD’s effects on growth and development needs to be evaluated according to local conditions. The impact of CHD on growth and development has been almost eliminated in benefit of modern medical advantages and well concern on patients in developed countries8. But most of the CHD cases are diagnosed and treated late due to poor resource availability in developing countries9. The understanding and prevention of the effect of CHD on patients’ growth and development status in developing countries still needs improvement. Although TOF is the most prevalent fetal CHD type in China, its outcomes on pediatric growth and development are not well investigated. This study was designed to specially evaluate the growth and development of children under 5 years old with TOF in China.
Results
The age information, mean z score and standard deviation (SD) of height, weight and BMI of all the 262 pediatric patients included in this study are summarized in Table 1 and detailed shown in Table S1. Growth charts of girls and boys with TOF are shown in Figs. 1 and 2 independently.
Growth charts for boys with TOF (total number = 138). (A) Height for age in TOF patient boys compared with normal chart. (B) Weight for age in TOF patient boys compared with normal chart. (C) BMI for age in TOF patient boys compared with normal chart. The dotted line represents the world standard value for the height, the green dotted line represents + 2SD, the blue dotted line represents Median, and the red represents -2SD. The data are calculated based on gender and age and calculated in the R Programming Language.
Growth charts for girls with TOF (total number = 124). (A) Height for age in TOF patient girls compared with normal chart. (B) Weight for age in TOF patient girls compared with normal chart. (C) BMI for age in TOF patient girls compared with normal chart. The dotted line represents the world standard value for the height, the green dotted line represents + 2SD, the blue dotted line represents Median, and the red represents -2SD. The data are calculated based on gender and age and calculated in the R Programming Language.
Growth and development status of children with TOF
The patients’ body height, body weight and BMI were compared to the WHO Child Growth Standards released in 2006. In order to evaluate the age specific growth and development status, the patients were set to two groups including infant patients (aged 0–12 months) and child patients (aged 13–60 months). The data of girls and boys were analyzed independently (Table 1). For the girl patients, the average z scores of body height, body weight and BMI were about 0.44, 0.52 and 0.37 less than the value from Growth Standards, respectively. The differences of average z-scores of body height, body weight and BMI were greater in child groups than infant groups (− 0.87 vs. − 0.22 for HAZ, P = 0.176; − 0.88 vs. 0.03 for WAZ, P = 0.22; − 0.41 vs. − 0.31 for BMIZ, P = 0.379). For the boy patients, the average z-scores of body height, body weight and BMI were about 0.44, 0.34 and 0.31 less than the value from Growth Standards, respectively. Moreover, the differences of average z scores of body height and body weight were greater in child groups than infant groups (− 0.80 vs. − 0.04 for HAZ, P = 0.551; − 0.88 vs. − 0.25 for WAZ, P = 0.612). The differences of average BMIZ didn’t show big variation between child groups and infant groups (− 0.29 vs. − 0.0.33, P = 0.04).
Growth retardation patterns of the pediatric TOF patients
To further define the effects of TOF on growth and development, stunting (low HAZ), underweight (low WAZ) and wasting (low BMIZ) frequencies were evaluated. A cut-off z score of ≤ − 2 was used to classify stunting, underweight and wasting, while a cut off z score of ≤ − 3 was classified as severe stunting, severe underweight and severe wasting8,10. The stunting, underweight and wasting frequencies of girl patients and boy patients are shown in Table 2.
Of the 262 patients, 56 cases (21.4%) were stunting, including 16 cases (6.1%) were severe stunting (Table 2). Underweight frequency was lower than the frequency of stunting, 38 (14.5%) patients were stunting with 12 (4.6%) severe cases (Table 2). 26 cases (9.9%) were wasting, including 11 severe wasting cases (4.2%) (Table 2). Stunting was the most occurred growth retardation pattern both in girls (n = 29, 23.4%) and boys (n = 27, 19.6%), while severe stunting show the highest frequency in boys (n = 13, 9.4%).
The detailed distribution of stunting, underweight and wasting patient numbers are summarized in Fig. 3. There were totally 39 girl patients (31.5% of the 124 girl patients) had growth retardation, including 12 patients (9.7%) had both stunting and underweight, 4 patients (3.2%) had both underweight and wasting. Of the 138 boy patients, 45 cases had growth retardation, including 4 cases (2.9%) had all the three patterns, 10 cases (7.2%) had both stunting and underweight, and 2 cases (1.4%) had both underweight and wasting.
As shown in Table 2, there was an increasing trend of stunting in child groups of both in girl (26.7% in child vs. 18.7% in infant, P = 0.286) and boy patients (26.0% in child vs. 12.3% in infant, P = 0.011). The underweight frequency of child group of boy patients was significantly increased compared with infant group (20.5% in child vs. 7.7% in infant, P = 0.032). Interestingly, the wasting frequencies exhibited a decrease trend in child group compared with infant group (10.2% in child vs. 4.0% in infant, P = 0.262) of girl patients.
Discussion
Increasing evidences suggest that different types of cardiac defects are associated with different patterns of growth retardation, while the situation also varies among nations11,12,13. Our study specially evaluated the growth and development of children with TOF, the most prevailing CHD type in China.
A survey in United States reported in 1962 showed that 27% of the children with CHD would fall below the third percentile (equal to a z score of − 1.881) for height and weight14. But updated researches indicated that the impact of CHD on growth and development has been almost eliminated in developed countries, but still needed more concern in other counties8,9. The recent study in Egypt showed the relative proportions of stunting, underweight and wasting of CHD patients were 61.9%, 14.3% and 23.8%, respectively15. Okoromah et al. reported in 2011 that the relative proportions of stunting, underweight and wasting (z score ≤ − 2, defined as malnutrition) of surveyed CHD children in Nigeria were 28.8%, 20.5%, and 41.1%, respectively8. For Asia countries, a study in 2011 reported that 22.6% of CHD patients were below the fifth percentile (equal to a z-score of − 1.645) for height, while 40.3% of patients were below the fifth percentile for weight in Iran10. In the same year, Ratanachu et al. revealed that relative proportions of stunting, underweight and wasting in Thailand children with CHD were 16%, 28% and 22%, respectively16. In our study, the relative proportions of stunting, underweight and wasting of children with TOF in our study were 21.4%, 14.5% and 9.9%, respectively. Our findings were somehow lower than those recent reports from other countries.
Despite that the other reports were about CHD and we specifically focused on TOF, the reason of the differences in the proportion and the pattern of growth retardation among each independent studies possibly due to different cut-off z scores, CHD type and Nations, which are effectors mentioned in previous reports8,17,18. Hassan, B. A. et al. reported that stunting was the most common type of malnutrition and was more linked to acyanotic CHD, while wasting was more associated with cyanotic CHD (~ 50% patients with TOF) in their study15. In contrast, Okoromah et al. reported that children with cyanotic CHD (~ 44% patients with TOF) were more likely to be stunting8. However, they haven’t distinguished the malnutrition pattern of children with TOF separately. In our study, body height was more affected in children with TOF. It has been reported that TOF affects body height severer than acyanotic CHD, might be due to the long period of hypoxemia19. The four defects caused by TOF results in short of blood in lung to get oxygen, and oxygen-poor blood effects the metabolic in body tissues, finally leads to the defects of growth and development.
Although it is generally thought that catch-up growth is better in patients operated at early age, FM Schuurmans et al.’s study found no significant relationship between the age when the child having surgical intervention and the catch-up growth20. They also reported that the most severe growth defection occurred in the 0–4 months old and turn to be slighter in elder age. In agreement with this report, Mohammad Dalili et al. found children older than 12 months had slighter defections than infant (0–12 months) 10. These reports suggested that growth retardation has already happened at early age (0–12 months) and will get slighter when grow up, which indicates early age is not a crucial time point for surgical intervention. In contrast, we found stunting frequency significantly raised from 14.9% in infant (aged 0–12 months) with TOF to 26.4% in children (aged 13–60 months) with TOF. Meanwhile, the underweight frequency raised from 10.5% to 17.6%, although is not significant. On the other hand, reduces of mean body height and body weight TOF patients from the standard value were amplified in children group (aged 13–60 months). Our results suggest greater deterioration of both the body height and weight of TOF patients happen in elder age rather than infant stage in China. Thus, early intervention for TOF patient may help to prevent the growth retardation getting severer. The average values of BMI and the frequencies of wasting didn’t show big variation between child and infant groups in our study. It is possibly due to some patients simultaneously have low body height (stunting) and low body weight (underweight).
It is reported that not only diseases, but also multiple factors, such as ethnicity, socioeconomic, even the education level of parents and the feeding behavior can effect growth and development status of children21,22,23,24. Thus, the cause and intervention for growth retardation may varied among different countries. However, for the growth retardation caused by CHD, surgical operation together with nutritional optimization are of the effective prevention strategy25,26. Based on our results, at least in the situation of China, intervention for patient with TOF, such as surgical operation and aggressive nutritional optimization should be considered at earlier age27,28.
Methods
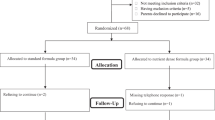
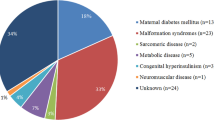
The study includes 262 pediatric patients aging from 1 month to 5 years who undergo corrective surgery for TOF at the department of pediatric cardiology, TEDA International Cardiovascular Hospital, Tianjin, China between 2014 and 2018. All the patients had not undergone palliative stenting or shunts or had undergone corrective surgery before coming to our hospital for treatment. The age information is shown in Table S1.
This study was carried out in accordance with the recommendations of clinical practice guidelines of China (Chinese Medical Association) with written informed consent from all subjects. Informed consent was obtained from the children’s guardian. The protocol was approved by the Ethical Committee of TEDA International Cardiovascular Hospital. All patients’ cardiac diagnoses were made based on clinical and laboratory examinations. Informed consent was obtained from the children’s guardian. A full medical history as well as a complete cardiac examination were documented for all children. Complete physical examination was performed for all patients by pediatric cardiologists and standardized measurements of body length、height and weight were done by trained nurses. Body mass index (BMI) was calculated by weight/height2.
Z scores for height for age (HAZ), weight for age (WAZ) and body mass index (BMIZ) were calculated using the Anthropometric calculator module of WHO Anthro software (based on the WHO child growth standards). Briefly, the z score refers to the ratio of the difference between the measured value and the standard median value recommended by the WHO child growth standards (2006). The z score was calculated by the following formula: z score = (real measured value—median value of the standards)/standard deviation of the WHO child growth standards. Bigger z score indicates the value is farther from the median level. The three common indicators related to height and weight are HAZ, WAZ, BMIZ. In a series of growth curves, between plus and minus 2 standard deviations (> − 2SD and < 2SD) is considered as normal. According to the Assessment for growth status of children under 5 years of age issued by National Health Commission of the People’s Republic of China in 2013, HAZ ≤ − 2 is classified as stunting, WAZ ≤ − 2 is classified as underweight, BMIZ ≤ − 2 is classified as wasting. The WHO global database on child growth and malnutrition (under-nutrition) also recommends a cut-off z score of ≤ − 2 to classify low HAZ (stunting), low WAZ (underweight), and low BMIZ (wasting).
Statistical analysis: In each group, the data was analyzed based on gender. Body height and weight and of each group were compared with standard values for the same age group. Data were analyzed using the Statistical Package for Social Sciences (SPSS) release16 and presented as mean ± SD. A P-value of < 0.05 was considered statistically significant.
References
Chen, C. W., Li, C. Y. & Wang, J. K. Growth and development of children with congenital heart disease. J. Adv. Nurs. 47, 260–269. https://doi.org/10.1111/j.1365-2648.2004.03090.x (2004).
Morgenthau, A. & Frishman, W. H. Genetic origins of tetralogy of fallot. Cardiol. Rev. 26, 86–92. https://doi.org/10.1097/CRD.0000000000000170 (2018).
Di Felice, V. & Zummo, G. Tetralogy of fallot as a model to study cardiac progenitor cell migration and differentiation during heart development. Trends Cardiovasc. Med. 19, 130–135. https://doi.org/10.1016/j.tcm.2009.07.004 (2009).
Apitz, C., Webb, G. D. & Redington, A. N. Tetralogy of fallot. Lancet 374, 1462–1471. https://doi.org/10.1016/S0140-6736(09)60657-7 (2009).
van der Linde, D. et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J. Am. Coll. Cardiol. 58, 2241–2247. https://doi.org/10.1016/j.jacc.2011.08.025 (2011).
Chen, X., Zhao, S. & X. Yang. A national survey of fetal congenital heart diseases in China. In 25th World Congress on Ultrasound in Obstetrics and Gynecology (2015).
Wray, J. Intellectual development of infants, children and adolescents with congenital heart disease. Dev. Sci. 9, 368–378. https://doi.org/10.1111/j.1467-7687.2006.00502.x (2006).
Okoromah, C. A. et al. Prevalence, profile and predictors of malnutrition in children with congenital heart defects: a case-control observational study. Arch. Dis. Child. 96, 354–360. https://doi.org/10.1136/adc.2009.176644 (2011).
Anuradha, S. M. K. C. B. & Kumar, G. T. Nutritional challenges in pediatric congenital cardiac car. Int. J. Sci. Healthc. Res. 3, 8 (2018).
Dalili, M. et al. Growth status of Iranian children with hemodynamically important congenital heart disease. Acta Med. Iran 49, 103–108 (2011).
Ferentzi, H., Pfitzer, C., Rosenthal, L. M., Berger, F. & Schmitt, K. R. L. Long-term early development research in congenital heart disease (LEADER-CHD): a study protocol for a prospective cohort observational study investigating the development of children after surgical correction for congenital heart defects during the first 3 years of life. BMJ Open 7, e018966. https://doi.org/10.1136/bmjopen-2017-018966 (2017).
Dinleyici, E. C. et al. Serum IGF-1, IGFBP-3 and growth hormone levels in children with congenital heart disease: relationship with nutritional status, cyanosis and left ventricular functions. Neuro Endocrinol. Lett. 28, 279–283 (2007).
Davis, D. et al. Feeding difficulties and growth delay in children with hypoplastic left heart syndrome versus d-transposition of the great arteries. Pediatr. Cardiol. 29, 328–333. https://doi.org/10.1007/s00246-007-9027-9 (2008).
Mehrizi, A. & Drash, A. Growth disturbance in congenital heart disease. J. Pediatr. 61, 418–429. https://doi.org/10.1016/s0022-3476(62)80373-4 (1962).
Hassan, B. A. et al. Nutritional status in children with un-operated congenital heart disease: an egyptian center experience. Front. Pediatr. 3, 53. https://doi.org/10.3389/fped.2015.00053 (2015).
Ratanachu-Ek, S. & Pongdara, A. Nutritional status of pediatric patients with congenital heart disease: pre- and post cardiac surgery. J Med Assoc Thai 94(Suppl 3), S133-137 (2011).
results from the Demographic and Health Survey. Democratic republic of Egypt 2008. Stud. Fam. Plann. 41, 153–158 (2010).
results from the Demographic and Health Survey. Egypt 2005. Stud. Fam. Plann. 37, 299–304 (2006).
Manzoor, N., Rehan, A., Akmal, M., Khalid, T. B. & Jamal, A. Congenital cytomegalovirus infection and tetralogy of fallot: an unusual association in a three-month-old baby. Cureus 11, e4949. https://doi.org/10.7759/cureus.4949 (2019).
Schuurmans, F. M., Pulles-Heintzberger, C. F., Gerver, W. J., Kester, A. D. & Forget, P. P. Long-term growth of children with congenital heart disease: a retrospective study. Acta Paediatr. 87, 1250–1255. https://doi.org/10.1080/080352598750030933 (1998).
Jones, L. L. et al. A comparison of the socio-economic determinants of growth retardation in South African and Filipino infants. Public Health Nutr. 11, 1220–1228. https://doi.org/10.1017/S1368980008002498 (2008).
Mujica-Coopman, M. F., Navarro-Rosenblatt, D., Lopez-Arana, S. & Corvalan, C. Nutrition status in adult Chilean population: economic, ethnic and sex inequalities in a post-transitional country. Public Health Nutr. 23, s39–s50. https://doi.org/10.1017/S1368980019004439 (2020).
Zhao, A. et al. Inappropriate feeding behavior: one of the important causes of malnutrition in 6- to 36-month-old children in myanmar. Am. J. Trop. Med. Hyg. 95, 702–708. https://doi.org/10.4269/ajtmh.16-0019 (2016).
Frozanfar, M. K. et al. Acute malnutrition among under-five children in Faryab, Afghanistan: prevalence and causes. Nagoya J. Med. Sci. 78, 41–53 (2016).
Medoff-Cooper, B. & Ravishankar, C. Nutrition and growth in congenital heart disease: a challenge in children. Curr. Opin. Cardiol. 28, 122–129. https://doi.org/10.1097/HCO.0b013e32835dd005 (2013).
Lim, C. Y. S. et al. The impact of pre-operative nutritional status on outcomes following congenital heart surgery. Front. Pediatr. 7, 429. https://doi.org/10.3389/fped.2019.00429 (2019).
Maymone-Martins, F. A. Tetralogy of Fallot after repair: A heritage of modern cardiac surgery. Rev. Port. Cardiol. 37, 781–782. https://doi.org/10.1016/j.repc.2018.08.004 (2018).
Spijkerboer, A. W. et al. Health-related Quality of Life in children and adolescents after invasive treatment for congenital heart disease. Qual. Life Res. 15, 663–673. https://doi.org/10.1007/s11136-005-3692-z (2006).
Acknowledgements
This study was supported by Technological Support Projects of Tianjin Binhai New Area Health and Family Planning Commission YJ-KY-Lix01-2018006 and 2017BWKZ008 to XinLi, Research Fund for Lin He’s Academician Workstation of New Medicine and Clinical Translation in Jining Medical University JYHL2019MS05 and Supporting Fund for Teacher’s Research of Jining Medical University JY2016KJ020Y and JY2017JS050 to Jin Zhu, National Natural Science Foundation of China (NSFC) Grant 31701247 and Supporting Fund for Teacher’s Research of Jining Medical University JYFC2018JS004 to XL. We are grateful to the study participants and data collectors, Hongyue Zheng, Yeshuang Wang, Bowen Zhang and Yajun Wang.
Author information
Authors and Affiliations
Contributions
X.L., Y.W. and X.L. conceived and designed the study. X.L. and J.A. collected data. X.L., J.Z., Y.W., Y.W. and X.L. performed statistical analysis and interpretation of data as well as wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, X., Zhu, J., An, J. et al. Growth and development of children under 5 years of age with tetralogy of Fallot in a Chinese population. Sci Rep 11, 14255 (2021). https://doi.org/10.1038/s41598-021-93726-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93726-3
This article is cited by
-
The ‘Ironclad friendship’ of China-Cambodia, lays the first step in the foundation of early diagnosis and treatment of asymptomatic congenital heart Defects- A multi-national screening and intervention project, 2017–2020
BMC Cardiovascular Disorders (2023)
-
Effect of feeding with standard or higher-density formulas on anthropometric measures in children with congenital heart defects after corrective surgery: a randomized clinical trial
European Journal of Clinical Nutrition (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.