Abstract
To characterize the new SARS-Co-V-2 related multisystem inflammatory syndrome in children (MIS-C) among Israeli children and to compare it with Kawasaki disease (KD). We compared, in two medical centers, the clinical and laboratory characteristics of MIS-C, KD and an intermediate group, which met the case definitions of both conditions. MIS-C patients were older, were more likely to be hypotensive, to have significant gastrointestinal symptoms, lymphopenia and thrombocytopenia and to have non-coronary abnormal findings in their echocardiogram. Lymphopenia was an independent predictor of MIS-C. Most of our MIS-C patients responded promptly to corticosteroid therapy. KD incidence in both centers was similar in 2019 and 2020. Although there is clinical overlap between KD and MIS-C, these are separate entities. Lymphopenia clearly differentiates between these entities. MIS-C patients may benefit from corticosteroids as first-line therapy.
Similar content being viewed by others
Introduction
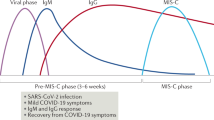
Soon after the COVID-19 pandemic started, a new entity—termed multisystem inflammatory syndrome in children (MIS-C; also referred to as pediatric inflammatory multisystem syndrome, PIMS) was reported from many countries1,2,3,4,5. Separate case definitions were developed by the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO)6,7. Both sets require fever, elevated inflammatory markers and involvement of at least two systems, with evidence of prior SARS-CoV-2 infection or exposure, as well as exclusion of other potential etiologies. Since Kawasaki disease (KD) shares some of the clinical and laboratory features with this new entity (fever, rash, conjunctival injection, elevated inflammatory markers), and both rely for their diagnosis on a set of non-specific criteria, it was suggested that both KD and MIS-C are in fact part of the spectrum of SARS-CoV-2-related inflammatory illness2,8. This question has prognostic as well as therapeutic implications. While in KD the initial standard of care requires a single dose of intravenous immune globulin (IVIG)9, the optimal management of patients meeting the MIS-C criteria is unclear. Per published guidelines both IVIG and corticosteroids may be used as first-line therapies, either alone or in combination with biologic agents like anakinra (recombinant human IL-1 receptor antagonist) or tocilizumab (humanized monoclonal antibody against IL-6 receptor)10. Our aim is to report our experience during the COVID-19 pandemic with pediatric patients presenting with fever and inflammation (without known etiology) and characterize features that may help differentiating KD from MIS-C.
Methods
The first case of COVID-19 in Israel was recorded in February 21, 2020. We have collected data of all pediatric patients, meeting the CDC and/or WHO case definitions for MIS-C, who presented to two medical centers serving Jerusalem and the Southern plains of Israel. The Jerusalem area had the highest incidence of COVID-19 in the country11. In the Jerusalem medical center we also collected data of all patients who met the KD diagnostic algorithm9 during the COVID-19 epidemic. SARS-Cov-2 RT-PCR on nasal swabs was performed for all febrile patients requiring admission. Serology was performed using a commercial kit, which detects IgG against nucleoprotein (Abbott SARS-CoV-2 IgG, Abbott Diagnostics, Abbott Park, IL, USA). The incidence rate of KD was calculated as the number of KD patients, seen in both centers, between January 2019 and October 2020, adjusted per 1000 admissions. During the first lockdown in Israel beginning in March 2020, the number of pediatric admissions dropped by > 60%, therefore for March through June we used the admission numbers of March-June 2019 in each center as the denominator for adjusting KD rates.
The Shaare-Zedek Medical Center (SZMC) and Kaplan Medical Center (KMC) Helsinki Committees have approved this study and its experimental protocol (approval #459/20).
The research was performed in full accordance with relevant guidelines and regulations. Informed consent was waived since all patient data were de-identified.
Analysis of variance (ANOVA) was used to determine whether age, temperature, length of stay in the hospital and mean values of the laboratory tests differed between MIS-C, KD or MIS-C/KD patients. Chi-square test was used to compare the categorical variables between the groups. For all analyses, a 2-sided probability < 0.05 was considered statistically significant. To identify independent predictors for MIS-C, logistic regression model was constructed with MIS-C as the dependent variable (MIS-C vs. KD or MIS-C/KD patients). Variables selected by the univariable analyses were included as independent variables. All analyses were done using SPSS version 25.0.
Results
Between February 2020 to October 2020, there were 13 patients with KD, 10 with MIS-C and 5 who met both MIS-C and KD case definitions. The clinical and demographic characteristics of the cohort are presented in Table 1.
MIS-C patients were predominantly male, aged 5 to 17 years. Eight had positive SARS CoV-2 serology, 3 had positive RT-PCR and all had known exposure to COVID-19. All patients had asymptomatic or mildly symptomatic prior COVID-19 infection. Median time from COVID-19 infection (when known) to presenting with MIS-C and/or KD was 25 days (17–90). One patient without cardiovascular symptoms had severe headache with magnetic resonance imaging (MRI) showing a cytotoxic lesion in the corpus callosum, which was interpreted as a non-specific finding12. Most patients (8/10) had acute gastrointestinal (GI) symptoms—all had significant abdominal pain (one had acute abdomen and undergone laparotomy) and 3 with diarrhea. All patients had clinical signs that could resemble those of KD, mainly red eyes and rash (8 and 6 patients, respectively), but none had > 3 clinical KD criteria, and none met the criteria for incomplete KD. Eight of the 10 patients were admitted to the intensive care unit. All received corticosteroid therapy (initially IV methylprednisolone 2 mg/kg/day) with 3 receiving it in conjunction with IVIG. Overall, 70% (7/10) responded promptly, with defervescence of fever after 1–4 doses of corticosteroids. Three patients had continued fever and inflammation and received pulse methylprednisolone (30 mg/kg/day for 3 days) combined with anakinra. All MIS-C patients were well after median follow up of 29 days (7–105). All were successfully weaned from corticosteroids, had normal acute phase reactants and did not develop coronary artery aneurysms (CAA).
KD patients
Seven (54%) patients had complete KD, the rest met the criteria for incomplete KD. None had myocardial involvement or hypotension. All responded to treatment with IVIG, with 4/13 (30%) requiring a second dose. None developed CAA after median follow up of 23 days (8–115).
Patients meeting both KD and MIS-C criteria
Five patients met both KD criteria and MIS-C. Of these, 4 had coronary artery dilation and 3 had valvular regurgitation. One 16 year-old patient had all 5 typical clinical KD signs, but also had lymphopenia, thrombocytopenia and excessively elevated troponin. His echo showed left ventricular (LV) dysfunction with no coronary involvement. Of note, he had negative SARS-CoV-2 PCR and serology but resided in an area with a very high incidence of COVID-19. He defervesced after 2 doses of IVIG combined with 2 mg/kg/day of methylprednisolone. A follow-up cardiac MRI demonstrated an area of myocardial scar tissue. Two patients developed uveitis after hospital discharge and required systemic or topical steroids. Over a follow up of 1–2 weeks after discharge, none have developed CAA.
MIS-C vs. KD
Several characteristics differentiated MIS-C patients from those with KD: MIS-C patients were older, were more likely to be hypotensive and have significant GI symptoms, have lymphopenia and thrombocytopenia, and have non-coronary abnormal findings in their echocardiogram (LV dysfunction, valvular regurgitation, pericardial effusion or retrograde aortic diastolic flow). Interestingly, the “intermediate” group of patients, who met both sets of criteria, had intermediate values for most clinical and laboratory variables (Table 1, Fig. S1). In multivariate analysis lymphopenia (lymphocyte count < 1500 µL) was an independent predictor of MIS-C, with an adjusted odds ratio of 24 (95% CI 1.3–326, p = 0.02).
KD incidence
The overall rate of KD admissions in 2019 was 4.8 and 1.2 cases/1000 admissions in SZMC and KMC, respectively, compared with 4.7 and 0.9 in 2020 (calculated until the end of October 2020 and adjusted for the decrease in admissions during the lockdown). Seasonality followed data previously reported from Israel13 (Fig. 1).
Kawasaki Disease (KD) rates per 1000 admissions in the two medical centers, in 2019 (solid line) and 2020 (dashed line), compared with number of COVID-19 cases diagnosed in Israel (bars; COVID-19 numbers obtained from Israel Ministry of Health data at: www.data.gov.il). multisystem inflammatory syndrome in children (MIS-C) cases represented by squares.
Discussion
Our report provides further support from Israeli patients to the new entity of MIS-C, witnessed in many countries, and further characterizes its distinction from the well-defined KD. There is a phenotypic overlap between MIS-C and KD. In particular, considerable similarities exist between MIS-C and KD shock syndrome (KDSS), which is characterized by prominent cardiovascular involvement2,5. However, several distinctions help to differentiate these conditions. MIS-C patients were older, had prominent GI symptoms and had lymphopenia and thrombocytopenia, which are not common in KDSS. In fact, we found that lymphopenia was an independent predictor of MIS-C. The clinical presentation in our patients is in line with the MIS-C case series reported so far1,2,3,4,5. These reports enrolled patients with positive viral RNA RT-PCR and respiratory symptoms as well as patients with positive serology and/or exposure to COVID-19 patients. Therefore it is possible that some case series represent a mix of patients with acute SARS-CoV-2 infection along with patients with post-infectious inflammation. Furthermore, as COVID-19 becomes endemic in many areas, positive PCR, serology or exposure may merely represent a concurrent phenomenon, and not necessarily explain the clinical presentation.
Focusing on the GI and myocardial involvement was recently suggested to be useful in differentiating MIS-C from other “look-alike” clinical entities14. Our report adds lymphopenia as a useful simple aid to differentiate between MIS-C and KD. This differentiation is not semantic but has therapeutic and prognostic implications. All of our MIS-C patients responded to corticosteroid therapy with 7/10 responding promptly to standard high dose and 3/10 only after IV pulse methylprednisolone was added. The present guidelines for immunomodulatory treatment in MIS-C are mainly derived from real-life experience and from high-quality data on the treatment of KD10. These guidelines recommend IVIG and/or corticosteroids, either alone or in combination, as first-line agents in MIS-C. In KD patients, corticosteroids have a role only as adjunctive therapy to IVIG in certain circumstances indicating a high risk for coronary involvement and/or non-response, or as a rescue therapy (usually after failing to respond to a 2nd dose of IVIG)15. Therefore, patients who meet criteria for both KD (usually incomplete) and MIS-C, should be treated with IVIG as first line treatment. A recent retrospective, propensity-score matched study found that MIS-C patients that received combined treatment of IVIG plus methylprednisolone had a better course of fever compared with those treated with IVIG alone16.
Further support to the concept of KD and MIS-C as separate entities, is provided by the relatively stable rate of KD cases during 2020 compared with 2019 at our two medical centers. If SARS-CoV-2 was a trigger to KD, we probably would have found an increase in the incidence of KD by now.
Our report represents the experience of two centers, located in regions with high COVID-19 incidence rates. As the COVID-19 epidemic continues to spread, there is an urgent need to improve our understanding of this new disease, particularly developing a more accurate diagnostic criteria that also clearly differentiate this entity from KD. Other multicenter control or “real-life” consensus treatment plan (CTP) studies should focus on determining the optimal treatment modality.
References
Riphagen, S., Gomez, X., Gonzalez-Martinez, C., Wilkinson, N. & Theocharis, P. Hyperinflammatory shock in children during covid-19 pandemic. The Lancet 395, 1607–1608 (2020).
Verdoni, L. et al. An outbreak of severe kawasaki-like disease at the italian epicentre of the SARS-COV-2 epidemic: An observational cohort study. Lancet 395, 1771–1778 (2020).
Whittaker, E. et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-COV-2. JAMA 324, 259–269 (2020).
Cheung, E. W. et al. Multisystem inflammatory syndrome related to covid-19 in previously healthy children and adolescents in New York city. JAMA 324, 294–296 (2020).
Feldstein, L. R. et al. Multisystem inflammatory syndrome in U.S. Children and adolescents. N. Engl. J. Med. 383, 334–346 (2020).
World Health Organization. Multisystem Inflammatory Syndrome in Children and Adolescents with Covid-19: Scientific Brief (WHO, 2020).
(HAN). CfDCaPHAN. Multisystem Inflammatory Syndrome in Children (mis-c) Associated with Coronavirus disease 2019 (COVID-19). https://emergency.cdc.gov/han/2020/han00432.asp. Accessed 25 Jun 2021.
Moraleda, C. et al. Multi-inflammatory syndrome in children related to SARS-COV-2 in Spain. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa1042 (2020).
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: A scientific statement for health professionals from the American Heart Association. Circulation 135, e927–e999 (2017).
Henderson, L. A. et al. American college of rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS-COV-2 and hyperinflammation in pediatric COVID-19: Version 1. Arthritis Rheumatol. 72, 1791 (2020).
Pease, C. et al. The latent tuberculosis infection cascade of care in Iqaluit, Nunavut, 2012–2016. BMC Infect. Dis. 19, 890 (2019).
Starkey, J., Kobayashi, N., Numaguchi, Y. & Moritani, T. Cytotoxic lesions of the corpus callosum that show restricted diffusion: Mechanisms, causes, and manifestations. Radiographics 37, 562–576 (2017).
Bar-Meir, M., Haklai, Z. & Dor, M. Kawasaki disease in Israel. Pediatr. Infect. Dis. J. 30, 589–592 (2011).
Rowley, A. H. Diagnosing sars-cov-2 related multisystem inflammatory syndrome in children (mis-c): Focus on the gastrointestinal tract and the myocardium. Clin. Infect. Dis. 72, e402 (2020).
Kobayashi, T. et al. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (raise study): A randomised, open-label, blinded-endpoints trial. The Lancet 379, 1613–1620 (2012).
Ouldali, N. et al. Association of intravenous immunoglobulins plus methylprednisolone vs immunoglobulins alone with course of fever in multisystem inflammatory syndrome in children. JAMA 325, 855–864 (2021).
Author information
Authors and Affiliations
Contributions
M.B.M. and O.M. conceptualized the study, supervised the data collection, and analyzed the data. A.G., O.G. and M.G. collected and interpreted data and have critically read the manuscript, A.S. collected data and wrote the first draft, P.H. supervised the data collection and critically read the draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bar-Meir, M., Guri, A., Godfrey, M.E. et al. Characterizing the differences between multisystem inflammatory syndrome in children and Kawasaki disease. Sci Rep 11, 13840 (2021). https://doi.org/10.1038/s41598-021-93389-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93389-0
This article is cited by
-
Multisystem inflammatory syndrome in children and Kawasaki disease; comparison of their clinical findings and one-year follow-up—a cross-sectional study
Italian Journal of Pediatrics (2023)
-
Kawasaki disease (KD) and multisystem inflammatory syndrome in children (MIS-C) in a Middle Eastern patient cohort
Pediatric Rheumatology (2023)
-
Multisystem inflammatory syndrome in children (MIS-C) and neonates (MIS-N) associated with COVID-19: optimizing definition and management
Pediatric Research (2023)
-
Italian intersociety consensus on management of long covid in children
Italian Journal of Pediatrics (2022)
-
Differences and similarities of multisystem inflammatory syndrome in children, Kawasaki disease and macrophage activating syndrome due to systemic juvenile idiopathic arthritis: a comparative study
Rheumatology International (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.