Abstract
In patients intubated for hypoxemic acute respiratory failure (ARF) related to novel coronavirus disease (COVID-19), we retrospectively compared two weaning strategies, early extubation with immediate non-invasive ventilation (NIV) versus standard weaning encompassing spontaneous breathing trial (SBT), with respect to IMV duration (primary endpoint), extubation failures and reintubations, rate of tracheostomy, intensive care unit (ICU) length of stay and mortality (additional endpoints). All COVID-19 adult patients, intubated for hypoxemic ARF and subsequently extubated, were enrolled. Patients were included in two groups, early extubation followed by immediate NIV application, and conventionally weaning after passing SBT. 121 patients were enrolled and analyzed, 66 early extubated and 55 conventionally weaned after passing an SBT. IMV duration was 9 [6–11] days in early extubated patients versus 11 [6–15] days in standard weaning group (p = 0.034). Extubation failures [12 (18.2%) vs. 25 (45.5%), p = 0.002] and reintubations [12 (18.2%) vs. 22 (40.0%) p = 0.009] were fewer in early extubation compared to the standard weaning groups, respectively. Rate of tracheostomy, ICU mortality, and ICU length of stay were no different between groups. Compared to standard weaning, early extubation followed by immediate NIV shortened IMV duration and reduced the rate of extubation failure and reintubation.
Similar content being viewed by others
Introduction
The rapid pandemic spread of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) represents a global public health emergency. A large number of COVID-19 patients require hospitalization for hypoxemic acute respiratory failure (ARF)1,2,3, with about 15% of cases needing invasive mechanical ventilation (IMV) in intensive care unit (ICU)3. While the best strategy of mechanical ventilation is still debated4,5,6, data on how to wean COVID-19 patients from IMV are even more scarce.
Usually, weaning off IMV starts with a spontaneous breathing trial (SBT) to test whether the patient is able to maintain spontaneous unassisted breathing7. Non-invasive ventilation (NIV) has been proposed as a valid tool to reduce the time spent on invasive ventilation in patients recovering from hypercapnic ARF8,9. More recently, early extubation followed by immediate NIV, in patients still dependent on relatively high level of positive end-expiratory pressure and inspiratory assistance, has been safely and effectively used in selected patients recovering from hypoxemic ARF, with a reduction of IMV duration and hospital length of stay, and a decrease of pulmonary infections (ventilator associated pneumonia or tracheobronchitis), compared to standard weaning through the endotracheal tube10,11.
In principle, early extubation followed by immediate NIV might be useful in intubated COVID-19 patients with ARF. In this retrospective multicenter observational study, we therefore compared early extubation followed by immediate NIV and standard weaning with respect to duration of IMV (primary endpoint), rate of extubation failure, reintubation, and tracheostomy, intensive care unit (ICU) mortality, and length of stay (additional endpoints).
Results
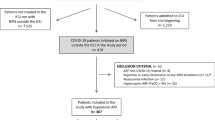
From March 1st to April 30th, 2020, 531 patients were admitted to the participant ICUs, of whom 121 were enrolled and finally analyzed (Fig. 1).
COVID-19, coronavirus disease 2019; ICU, intensive care unit; ARF, acute respiratory failure; NIV, non-invasive ventilation; IMV, invasive mechanical ventilation; SBT, spontaneous breathing trial.
Among these, 55 patients were extubated according to standard weaning strategy after encompassing SBT, whereas 66 patients underwent early extubation and immediate NIV. Demographic and baseline clinical characteristics are reported in Table 1. In the standard weaning group, a higher incidence of active smoking (p < 0.001), chronic arterial hypertension (p = 0.001), ischemic heart disease (p = 0.008), and other medical disease (p = 0.045) were reported, compared to the early extubation group. Also, the length of NIV before intubation was longer in the standard weaning group (p = 0.003).
Clinical outcomes are presented in Table 2. In the standard weaning group, the length of IMV was longer (p = 0.034) and the extubation failure (p = 0.002) and reintubation rate (p = 0.009) were higher compared to the early weaning group.
The Kaplan–Meier curves indicating the time to liberation from IMV are depicted in Fig. 2.
Kaplan–Meier curves indicating the time lag from intubation to IMV discontinuation. The Kaplan–Meier curve showing median and interquartile range are depicted: red line represents early extubation group while turquoise line refers to standard weaning group; P values refer to Log-Rank test. Kaplan–Meier curve constructed without (a) or with adjusting for propensity score (b).
The Kaplan–Meier curve showing median and interquartile range are depicted: red line represents early extubation group while turquoise line refers to standard weaning group; P-values refer to Log-Rank test. Kaplan–Meier curve constructed without (a) or with adjusting for propensity score (b).
According to Kaplan–Meier analysis (Fig. 2a), IMV was interrupted after 11.0 [6.0–15.0] days in the standard weaning group and after 9.0 [6.0–11.0] days in the early extubation group (p = 0.002). When the Kaplan–Meier curve was constructed adjusting for propensity score (Fig. 2b), IMV duration was of 11.0 [10.0–12.0] days in the standard weaning group and 9.0 [7.0–10.0] days in the early extubation group (p = 0.010).
The main medical treatments employed during ICU stay are listed in Table 3. In the standard weaning group, the use of anti-viral medications was less frequent (p = 0.004), while there was a higher use of steroids than in the early extubation group (p = 0.044), respectively. The mechanical ventilation settings and advanced therapy are reported in Supplementary material 1 (for missing data eTable1).
In the standard weaning group, SBT duration was of 40.0 [30.0–60.0] min. SBT was conducted through T-tube or PSV + CPAP mode in more than 70% of the cases (eFigure 1). In the same group, IMV was discontinued after 1.0 [1.0–2.0] SBT attempts (range 1.0–3.0).
In the standard weaning group, prophylactic NIV was used in 33 (60.0%) patients (eTable2), while 16 (29.1%) patients received NIV as rescue treatment of post-extubation respiratory failure. When NIV was used in standard weaning group, its duration was of 2.0 [0.5–4.0] days, whereas, in patients early extubated, NIV duration was of 2.0 [1.0–4.3] days (p = 0.554). In the early extubation group, NIV was administrated soon after extubation through PSV in 52 (78.8%) patients and or CPAP mode in 14 (21.2%) patients.
Blood tests at hospital admission and during ICU stay are presented in Table 4 (for missing data eTable3). The two groups were homogenous for white cells and lymphocytes counts as well as for lactate-dehydrogenase and procalcitonin serum concentration and PaO2/FiO2. At extubation C-reactive protein serum levels were lower in the standard weaning group than in the early extubation group (p = 0.0003). In both groups PaO2/FiO2 at extubation was improved compared to hospital admission (p < 0.0001 for all comparisons) and time of intubation (p < 0.0001 for all comparisons).
Discussion
In the present retrospective multicentric investigation in patients undergoing IMV for severe COVID-19 related ARF, early extubation followed by immediate NIV application improved clinical outcomes respect to standard weaning strategy with SBT, by reducing the length of IMV and decreasing both extubation failure and reintubation rate, without affecting ICU length of stay and ICU mortality. These results are of particular interest in the COVID-19 pandemic, characterized by an imbalance between the high number of patients needing immediate ventilatory assistance and the prompt availability of ICU beds and ventilator machines12,13,14. While reducing the risk of pulmonary infections is important for all intubated patients regardless of the underlying disease, reducing the days of mechanical ventilation and the length of ICU stay is of paramount importance when high numbers of patients require ICU admission for receiving IMV, determining the need for elevated ICU surge capacity, as it occurs during the COVID-19 outbreak12,13,14. Indeed, any strategy aimed to improve the prompt availability of ICU beds and ventilators is desired12,13,14.
NIV for facilitating IMV discontinuation has been suggested by guidelines only in patients admitted for hypercapnic ARF9 since it reduces the incidence of tracheostomy and ventilator-associated pneumonia, and shortens IMV duration, ICU, and hospital length of stay, compared to standard weaning15. Recently, however, in selected patients recovering from hypoxemic ARF, the application of NIV, immediately after early extubation, demonstrated to reduce the length of IMV, as opposed to standard weaning10,11. The present investigation suggests that COVID-19 patients may also benefit of this approach to weaning. Moreover, differently from the aforementioned study on hypoxemic ARF patients10,11, in our COVID-19 patients early extubation was able to significantly decrease the rate of extubation failure and reintubation, compared to standard weaning.
Extubation failure approximatively occurs in 10–15% of cases, in patients deemed ready for IMV discontinuation16 and in more than 20% of the cases, in patients considered at risk for reintubation16,17. NIV is recommended to prevent extubation failure in patients considered at risk for reintubation9, as it has been demonstrated that the prophylactic use of NIV is able to reduce the rate of reintubation, compared to standard oxygen therapy18,19. Also, when NIV is combined with high flow nasal oxygen therapy in patients older than 65 years or with an underlaying cardiac or respiratory disease, the rate of reintubation is lower than with high flow nasal oxygen therapy only20. Previous works18,19,20 have reported that the rate of reintubation with NIV ranged from 5 to 8.3% within the 48 h after extubation and achieved 12% at ICU discharge. In our population, the application of NIV immediately after early extubation decreased the rate of extubation failure and reintubation compared to standard weaning group, despite 60% of the patients were prophylactically assisted after IMV discontinuation. However, in our setting, failure of a planned extubation and need for reintubation occurred much more frequently than previously described in mixed populations of hypoxemic and hypercapnic ARF patients18,19,20. Indeed, the 40% reintubation rate is definitely high, compared to the usual rates reported in studies not involving COVID-19 patients18,19,20. That said, to our knowledge, no study has reported insofar the rate of extubation failure and reintubation in COVID-19 patients. In a recent RCT aimed at comparing standard weaning vs. early extubation + immediate NIV application in a population of non-COVID-19 hypoxemic patient recovering from non-hypercapnic acute respiratory failure11, we had a rate of treatment failure in the conventional weaning group of 18%, which is definitely lower than the 40% reported here. Noteworthy, the rate of failure in the early extubation + NIV group in that study was 8%11, which is also much lower than the 18.2% reported here. In our series, the vast majority of early extubation + NIV data were collected in centers also enrolling for the aforementioned study11, which indirectly suggests that the rate of extubation failure in COVID-19 patients might exceed that generally observed in non-COVID-19 patients.
This multicenter retrospective investigation has several limitations that must be considered. First, data were retrospectively obtained from medical records with a limited sample size. Accordingly, the lack of a randomization in study population sampling—i.e., sampling bias—could make our results not generalized to other settings. Second, the participating centers that applied a protocol of early extubation, were highly skilled in NIV assistance, which might raise questions about generalizability. Third, SBT was conducted in more than 45% of the cases in T-tube mode. This procedure might have adversely affected the weaning outcome as previously described21. Also, the progressive reduction of ventilatory assistance in standard weaning group could have negatively affected clinical outcomes. Fourth, also the rate of ventilator-associated pneumonia, tracheobronchitis, and other severe events, such as pneumothorax, pulmonary embolism, and hemorrhagic, septic, cardiac, renal, or neurologic episodes were not recorded. Fifth, knowing how resource availability has changed during the study period is an interesting piece of information that might have influenced physician’s attitude for IMV and NIV. Unfortunately, we did not record this information. Unfortunately, we did not record this information. Finally, our results should be considered specific for COVID-19 population, and thus are not generalizable under other conditions.
In conclusion, in scenarios needing too early extubation as that of our cohort of patients receiving IMV for severe COVID-19 related hypoxemic ARF, direct extubation to NIV seems to perform better than ordinary SBT because it has the potentiality to improve clinical outcomes compared to standard weaning, by shortening IMV duration and reducing the rate of extubation failure and reintubation.
Methods
The study was approved by local Ethics Committees of coordinator center (Comitato Etico Interaziendale Novara, Italy – CE 120/20) and collaborators hospitals. The present multicenter retrospective study was conducted according to the Helsinki Declaration principles in 12 ICUs, 6 of which were highly skilled in early extubation followed by immediate NIV application. Due to the retrospective nature of the investigation, the need for informed consent from individual patients was waived by local Ethics Committees of coordinator center (Comitato Etico Interaziendale Novara, Italy – CE 120/20) and collaborators hospitals.
Patients
All consecutive adult patients, intubated for severe COVID-19 related ARF from March 1st to April 30th, 2020, and subsequently weaned from IMV, were considered eligible. Laboratory confirmation for SARS-CoV-2 infection was defined as a positive result of reverse transcriptase-polymerase chain reaction (RT-PCR) assay of naso-pharyngeal swabs obtained on hospital admission. In case of negative result, RT-PCR assay from lower respiratory tract aspirate/bronco-alveolar lavage was carried out after intubation in ICU22.
Patients were evaluated for IMV discontinuation when they met the following criteria: (1) assisted ventilation mode with a total inspiratory pressure < 30 cmH2O; (2) respiratory rate ≤ 30 breathes*min-1; (3) effective cough; (4) core temperature ≤ 38.5 °C; (5) arterial partial pressure of oxygen (PaO2) to inspired oxygen fraction (FiO2) ratio (PaO2/FiO2) ≥ 150 mmHg or peripheral oxygen saturation (SpO2) between 90 and 94% with FiO2 ≤ 0.6; (65) arterial pH ≥ 7.35; 6) Glasgow Coma Scale ≥ 11 (V1tube). Patients were excluded in case of IMV lasting < 24 h and contraindications to NIV23.
The study population was divided in two groups according to weaning plan adopted:
-
1.
Standard weaning group, where extubation was performed only after having encompassed SBT in pressure support ventilation (PSV), neurally adjusted ventilatory assist (NAVA), continuous positive end-expiratory pressure (CPAP), or T-tube mode7.
-
2.
Early extubation group, where no SBT was performed and patients were early extubated and immediately supported through facial mask or helmet NIV either in PSV or CPAP mode10,11.
In the standard weaning group, patients underwent a progressive reduction of positive end-expiratory pressure (PEEP) and inspiratory pressure support during assisted mode. When PEEP ≤ 10 cmH2O and inspiratory pressure support over PEEP ≤ 12 cmH2O or NAVA gain ≤ 0.8 cmH2O*µV-1, a 30–60-min-lasting SBT was performed. Once SBT was passed according to each center institutional weaning protocol criteria, detailed in the online Supplementary material 2, patients were extubated and allowed to spontaneously breath through Venturi mask or high flow nasal cannula, with additional oxygen to maintain SpO2 between 90 and 94%. After extubation, NIV was used either in CPAP or PSV (1) as prophylactic ventilatory assistance in patients judged at high risk for extubation failure9,24, and (2) as a rescue therapy in case of post-extubation respiratory failure.
Conversely, in case of SBT failure, the assisted ventilatory mode was restored and a new SBT was attempted after 24 h.
In early extubation group, when PEEP and inspiratory pressure support over PEEP were both ≤ 15 cmH2O with a total inspiratory pressure < 30 cmH2O during assisted ventilatory mode, in presence of a respiratory rate ≤ 30 breathes*min-1, an effective cough, a core temperature ≤ 38.5 °C, a PaO2/FiO2) ≥ 150 mmHg or SpO2 between 90 and 94% with FiO2 ≤ 0.6, an arterial pH ≥ 7.35, and Glasgow Coma Scale ≥ 11 (V1tube), patients were extubated without SBT and NIV was immediately started either in PSV or CPAP mode. During NIV, the values of PEEP and inspiratory pressure support were set according to those previously set during IMV, while FiO2 was chosen to assure SpO2 varying from 90 to 94%. NIV pressure support and PEEP were progressively reduced and spontaneous breathing was allowed, with oxygen supplementation as previously described.
In both groups extubation failure was defined as the need for reintubation within the 48 h after extubation25. In the conventionally weaning group additional extubation failure criteria were considered the needing of NIV within 48 h after extubation. Prophylactic NIV and high flow nasal cannula were not considered extubation failure11.
The centers involved in the study adhered to one weaning strategy or the other according to their internal protocols.
Data collection
Clinical data were retrospectively acquired in the centers that adhered to the present investigation and sent to the coordinator center for analysis. The recorded data included the followings: age, sex, body mass index, medical comorbidities, gravity index at ICU admission (Simplified Acute Physiology Score II and/or Sequential Organ Failure Assessment) and anti-viral therapies. Length of IMV, extubation failure, reintubation and tracheostomy rate, as well as ICU length of stay and in-ICU mortality were computed. Both pre-intubation and post-extubation NIV duration were also noted. Mechanical ventilation settings (i.e., PEEP and plateau pressure after intubation, level of assistance before SBT or before early extubation) were obtained. PaO2/FiO2, total white blood cells, and lymphocytes counts as well as lactate-dehydrogenase, procalcitonin, and C-reactive protein serum concentration were recorded at hospital admission and on the day of intubation and extubation. Finally, the rate of prone positioning, nitrous oxide inhalation, and extra-corporeal membrane oxygenation application were acquired.
Statistical analysis
Because of the retrospective nature of the study, no statistical sample size calculation was computed a priori. The study population was divided in two groups: 1) standard weaning with SBT and 2) early extubation followed by immediate NIV. Continuous variables were presented as median and interquartile range, whereas categorical variables were expressed as number and percentage. Comparison between groups was assessed using Mann–Whitney’s test for continuous variables and Fisher’s exact test for categorical variables. In case of missing data, the comparison was made only with available data.
Kaplan–Meier curves, depicting the time lag from intubation to IMV discontinuation in each group, were determined and compared trough Log-Rank test. A propensity score was estimated to balance the patient’s characteristics among groups. The covariate balancing propensity score estimation was computed considering baseline characteristics: age, gender, NIV before intubation, pharmacological treatments, body mass index, SAPSII, SOFA, comorbidities, smoke, and days from hospitalization to symptoms onset. The Cox Regression model for inverse probability weight propensity adjusted survival curve was also computed.
A generalized linear mixed model adjusted for inverse probability weight propensity score was computed evaluating the marginal and interaction effect of the time (hospital admission, intubation, extubation, and NIV) and weaning plan adopted on the haemato-chemical parameters; a random intercept term on the center and patient identification number was introduced in the model accounting for both correlation within repeated measurements and within the same center. For all comparisons, a p-value < 0.05 was considered significant. Statistical analysis was carried out using R 3.6.2 (The R Foundation).
Ethics approval and consent to participate
The present investigation was approved by all the ethics committees of the centers that adhered to the study.
Data availability
In accordance to ICMJE, the data sharing has been planned as follows: Whether individual, de-identified participant data (including data dictionaries) will be shared: Yes; What data in particular will be shared: Individual participant data that underlie the results reported in this article, after deidentification (text, tables and figures). Whether additional, related documents will be made available: No; When and for how long the data will become/be available: Beginning 9 months and ending 36 months following article publication. The criteria to access the data (including who can request access and for what types of analyses, and the name of the data repository): Researchers who provide a methodologically sound proposal for individual participant data meta-analysis should contact principal investigator to gmcamma@gmail.com. Proposals may be submitted up to 36 months following article publication.
References
Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature https://doi.org/10.1038/s41586-020-2012-7 (2020).
Wang, D. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA J. Am. Med. Assoc. 323, 1061–1069 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet https://doi.org/10.1016/S0140-6736(20)30566-3 (2020).
Marini, J. J. & Gattinoni, L. Management of covid-19 respiratory distress. JAMA J. Am. Med. Assoc. https://doi.org/10.1186/cc2392 (2020).
Tobin, M. J., Laghi, F. & Jubran, A. Caution about early intubation and mechanical ventilation in COVID—19. Ann. Intensive Care https://doi.org/10.1186/s13613-020-00692-6 (2020).
Fan, E. et al. Viewpoint COVID-19-associated acute respiratory distress syndrome: Is a different approach to management warranted?. Lancet Respir. Med. 2600, 1–6 (2020).
Sklar, M. C. et al. Effort to breathe with various spontaneous breathing trial techniques. Am. J. Respir. Crit. Care Med. 195, 1477–1485 (2017).
Nava, S., Navalesi, P. & Carlucci, A. Non-invasive ventilation. Minerva Anestesiol. 75, 31–36 (2009).
Rochwerg, B. et al. Official ERS/ATS clinical practice guidelines: Noninvasive ventilation for acute respiratory failure. Eur. Respir. J. 50, 1–20 (2017).
Vaschetto, R. et al. Noninvasive ventilation after early extubation in patients recovering from hypoxemic acute respiratory failure: A single-centre feasibility study. Intensive Care Med. 38, 1599–1606 (2012).
Vaschetto, R. et al. Early extubation followed by immediate noninvasive ventilation vs. standard extubation in hypoxemic patients: A randomized clinical trial. Intensive Care Med https://doi.org/10.1007/s00134-018-5478-0 (2018).
Aziz, S. et al. Managing ICU surge during the COVID-19 crisis: Rapid guidelines. Intensive Care Med. https://doi.org/10.1007/s00134-020-06092-5 (2020).
Vitacca, M., Nava, S., Santus, P. & Harari, S. Early consensus management for non-ICU ARF SARS-CoV-2 emergency in Italy: From ward to trenches. Eur. Respir. J. 55 (2020).
Cammarota, G. et al. Critical care surge capacity to respond to the COVID-19 Pandemic in Italy: A rapid and affordable solution in the Novara Hospital. Prehosp. Disaster Med. 35, 431–433 (2020).
Burns, K. E. A., Meade, M. O., Premji, A. & Adhikari, N. K. J. Noninvasive positive-pressure ventilation as a weaning strategy for intubated adults with respiratory failure. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004127.pub3 (2013).
Thille, A. W., Richard, J. C. M. & Brochard, L. The decision to extubate in the intensive care unit. Am. J. Respir. Crit. Care Med. 187, 1294–1302 (2013).
Esteban, A. et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am. J. Respir. Crit. Care Med. 188, 220–230 (2013).
Ornico, S. R. et al. Noninvasive ventilation immediately after extubation improves weaning outcome after acute respiratory failure: A randomized controlled trial. Crit. Care 17, R39 (2013).
Nava, S. et al. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit. Care Med. 33, 2465–2470 (2005).
Thille, A. W. et al. Effect of postextubation high-flow nasal oxygen with noninvasive ventilation vs high-flow nasal oxygen alone on reintubation among patients at high risk of extubation failure: A randomized clinical trial. JAMA J. Am. Med. Assoc. 322, 1465–1475 (2019).
Subirà, C. et al. Effect of pressure support vs T-piece ventilation strategies during spontaneous breathing trials on successful extubation among patients receiving mechanical ventilation: A randomized clinical trial. JAMA - J. Am. Med. Assoc. 321, 2175–2182 (2019).
Wiersinga, W. J., Rhodes, A., Cheng, A. C., Peacock, S. J. & Prescott, H. C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA 2019, 1–13 (2020).
Adults, B. G. for the V. M. of A. H. R. F. in. Ventilatory-Management-of-Ahrf-1. 71, 4–44 (2016).
Renda, T. et al. High-flow nasal oxygen therapy in intensive care and anaesthesia. Br. J. Anaesth. 120, 18–27 (2018).
Boles, J. M. et al. Weaning from mechanical ventilation. Eur. Respir. J. 29, 1033–1056 (2007).
Author information
Authors and Affiliations
Contributions
G.C., R.V. and N.D.V. had the idea for and designed the study, had full access to all of the data in the study, took responsibility for the integrity of the data, contributed to the design of the study and to the interpretation of data for the work, and drafted the paper. G.C. and R.V. drafted and revised the paper for submission. D.A., had full access to all of the data in the study and took the responsibility for the accuracy and the data analysis and drafted the paper. F.D.C. and P.N. contributed to the design of the study and to the interpretation of data for the work and drafted the paper. CO, C.R., F.L., A.B., D.C., C.P., F.P., C.M., M.M., L.V., T.B., F.L., E.T., A.L., N.B., M.C., E.R., C.Z., I.B., F.S., F.R., V.B., I.S., Y.L., F.G., F.C., R.P., E.B., F.V., G.V., E.S., R.T., M.Z., M.M., P.B., G.S., and A.D.S. contributed to the acquisition, integrity and analysis of the data. A.B. contributed to paper drafting and revision before submission. A.M. and N.S. revised the manuscript before submission. All authors (1) agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. (2) revised the work critically for important intellectual content and (3) gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
Competing interests CO has a patent 102016000114357 with royalties paid from Intersurgical SpA. FL has a patent EP20170199831 pending. DC reports personal fees from Nestlé Healthcare nutrition and Getinge, outside the submitted work. FR personal fees for lectures from Philips Respironics outside the submitted work. PN reports personal fees from Intersurgical SpA, Resmed, Philips, Novartis, MSD, Getinge, Orion Pharma and non-financial support from Draeger, outside the submitted work. In addition, PN has a patent 102020000008305 pending to Università di Padova, and a patent 102016000114357 with royalties paid from Intersurgical S.p.A. AM reports personal fees and other from Vygon, outside the submitted work The remaining Authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cammarota, G., Vaschetto, R., Azzolina, D. et al. Early extubation with immediate non-invasive ventilation versus standard weaning in intubated patients for coronavirus disease 2019: a retrospective multicenter study. Sci Rep 11, 13418 (2021). https://doi.org/10.1038/s41598-021-92960-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-92960-z
This article is cited by
-
Effect of awake prone position on diaphragmatic thickening fraction in patients assisted by noninvasive ventilation for hypoxemic acute respiratory failure related to novel coronavirus disease
Critical Care (2021)
-
Research on SARS-COV-2 pandemic: a narrative review focused on the Italian contribution
Journal of Anesthesia, Analgesia and Critical Care (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.