Abstract
Stroke and cognitive impairment are common in older population. They often occur together and their combined effects significantly increase disability in both basic (BADLs) and instrumental (IADLs) activities of daily living. We investigated the individual and combined impacts of stroke and cognitive impairment on BADLs and IADLs. A total of 3331 community-dwelling older adults were enrolled from the Taiwan longitudinal study on aging in 2011. Both BADLs and IADLs were analyzed. Combination of stroke and cognitive impairment increased severity of ADL disabilities, but similar prevalence, similar numbers of summed BADL and IADL tasks with disability, and similar levels of difficulty for each BADL and IADL task were found between the stroke group and cognitive impairment group. The former had more difficult in dressing while the latter had more difficult in using the telephone, transport, and managing finances. A hierarchy of ADLs was also observed in all groups. ADL skill training supplemented with cognitive and physical interventions should focus on secondary prevention of dementia and improve motor functional capacity to reduce loss of ADLs.
Similar content being viewed by others
Introduction
Approximately 70% of stroke patients have cognitive impairment in the first year after the stroke1, 2. The prevalence at 3 years post-stroke ranges from 50 to 58%3, indicating that the prevalence of cognitive impairment after a stroke is very high and may progress to dementia. On the other hand, cognitive decline is also a risk factor of stroke. Lower cognitive function is associated with a higher risk of incident stroke4. There seems to be a reciprocal relationship between stroke and cognitive impairment. Both stroke and cognitive impairment impact cognitive and physical functions and contributes to disability5, 6. They interact resulting in disability that is greater than the sum of the independent contributions from either stroke or cognitive impairment alone7.
Basic activities of daily living (ADLs; BADLs) refer to the basic tasks of living that is an indicator of a person’s functional status, while instrumental activities of daily living (IADLs) address a higher level of ADLs that consist of more complex daily tasks that must be performed to continue living independently in the community8. Individuals with ADL disabilities have poor life satisfaction9, quality of life10, and find it difficult to return to the community.
Previous studies showed that 40% of acute stroke survivors had total or severe ADL disabilities at hospital discharge11. Nearly 40% of patients at 6 years post-stroke still had dependence in BADLs12. Stroke patients who had the worse ability to perform IADL tasks tended to have a poorer walking capacity, upper limb strength, and neurological recovery11. The majority of chronic stroke patients need assistance with bathing, and half of them cease such activities as preparing meals, doing housework, shopping, and walking outdoors13. As for dementia patients, around 40% of them are unable to perform any of the IADL tasks14. IADLs are usually impaired in the early stage of cognitive decline, but BADLs are affected later in the course of the condition15. The proportions of those independent in BADL tasks among mildly, moderately, and severely demented patients were 63%, 36%, and 0%, respectively16. Deficits in ADLs were correlated with memory, psychomotor speed17, 18, and executive functions19.
The majority of previous studies examined the effects of either stroke or cognitive impairment on ADL performances, but limited research has investigated the combined effects of both, although many studies have reported that cognitive impairments after a stroke can aggravate ADL limitations20, 21. Only one population study analyzed the combined effects of stroke and dementia on ADLs, and the results showed that individuals with stroke and dementia comorbidity had 1.8 out of 7 ADL limitations, compared to 1.4 for those with dementia, 0.6 for those with a stroke, and 0.3 for healthy controls without further analysis or comparison7. Therefore, using data obtained from a national representative sample, we aimed to investigate the individual and combined impacts of stroke and cognitive impairment on both BADLs and IADLs.
Results
Baseline characteristics
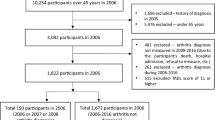
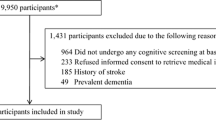
The original sample comprised 3727 people, 396 people with incomplete SPMSQ data were excluded, and therefore 3331 adults were included in the current study. There were significant differences among the control, stroke, cognitive impairment, and combination groups in all baseline characteristics including sex, educational level, age, marital status, numbers of comorbidities, cognitive functions, and upper and lower limb functions (all p < 0.001) (Table 1). About 3.5% of the participants were stroke survivors, 11.7% had cognitive impairments, and 1.8% had both conditions. Compared to similar ratios of males to females in the control and combination groups, greater proportions were male in the stroke group and female in the cognitive impairment group. More than 90% of individuals in the cognitive impairment group had lower educational attainment, and they were generally older and living without partners. The stroke and combination groups had more comorbidities. Half of the individuals in the cognitive impairment and combination groups had only mild cognitive decline. Compared to the worst limb functions in the combination group, a slightly larger proportion of individuals in the stroke group had poorer upper limb function, while those in the cognitive impairment group had poorer lower limb function.
Prevalence of disabilities among groups
Prevalence of disabilities in BADLs and IADLs significantly differed among the groups (X2 = 690.985, p < 0.001). More than 60% of individuals in the combination group had both BADL and IADL disabilities, but only 30% of individuals in either the stroke or cognitive impairment groups had both kinds of disabilities. The proportion of individuals in the control group who had disabilities in both BADLs and IADLs was only 5% (Table 2). The hierarchical relationship between IADLs and BADLs was observed in all groups, in which IADLs were first affected, followed by both IADLs and BADLs.
BADL disabilities among groups
Among the six BADL tasks, the number of disabilities of BADL tasks was significantly different among groups (F(3,3322) = 126.836, p < 0.001). The post-hoc analysis showed that the combination group had the greatest number of disabilities of BADL tasks (2.56 ± 0.73) compared to the cognitive impairment (0.95 ± 1.88, p < 0.001), stroke (1.04 ± 0.73, p < 0.001), and control groups (0.14 ± 0.73, p < 0.001), but there was no difference between the stroke and cognitive impairment groups (p = 0.296). Moreover, the level of difficulty in all BADL tasks was significantly different among groups (F(3,3322) = 115.998, p < 0.001 in bathing, F(3,3322) = 110.196, p < 0.001 in dressing, F(3,3322) = 54.061, p < 0.001 in eating, F(3,3322) = 89.260, p < 0.001 in transferring, F(3,3322) = 81.289, p < 0.001 in indoor walking, and F(3,3322) = 86.873, p < 0.001 in toileting). The combination group had the greatest difficulty in all BADL tasks than all of the other groups (all p < 0.001). No differences were found again in the majority of BADL tasks between the stroke and cognitive impairment groups, but the stroke group had a significantly greater difficulty than the cognitive impairment group in dressing (p = 0.04) (Fig. 1). Regardless of the group, the most difficult BADL task was bathing, while the least difficult task was eating.
IADL disabilities among groups
Among the nine IADL tasks, the number of disabilities of IADL tasks was significantly different among groups (F(3,3322) = 230.389, p < 0.001). The post-hoc analysis showed that the combination group had the greatest number of IADL tasks with disabilities (6.00 ± 3.05) compared to the cognitive impairment (3.25 ± 3.11, p < 0.001), stroke (2.34 ± 3.11, p < 0.001), and control groups (0.61 ± 1.51, p < 0.001), but there was no difference between the stroke and cognitive impairment groups (p = 0.195). Furthermore, the level of difficulty in all IADL tasks was significantly different among groups (F(3,3322) = 110.229, p < 0.001 in light house work, F(3,3322) = 58.100, p < 0.001 in heavy housework, F(3,3322) = 156.482, p < 0.001 in transport, F(3,3322) = 131.282, p < 0.001 in managing finances, F(3,3322) = 106.933, p < 0.001 in shopping, F(3,3322) = 129.330, p < 0.001 in laundry, F(3,3322) = 133.894, p < 0.001 in medication, F(3,3322) = 133.155, p < 0.001 in food preparation, and F(3,3322) = 194.000, p < 0.001 in using the telephone). The combination group had the greatest difficulty in all IADL tasks compared to the other groups (all p < 0.001). No differences were found in the majority of IADL tasks between the stroke and cognitive impairment groups, but the cognitive impairment group had a significantly greater difficulty than the stroke group in using the telephone (p < 0.001), transport (p = 0.002), and managing finances (p < 0.001) (Fig. 2). Regardless of the group, the most difficult IADL task was heavy housework, while the least difficult was taking medications.
Discussion
In this nationally representative sample of middle-aged and older community-dwelling adults, we found that individuals with a combination of stroke and cognitive impairment had the highest prevalence of disabilities in both BADLs and IADLs, while individuals with either stroke or cognitive impairment had the lowest prevalence. Similar prevalences were found in the stroke and cognitive impairment groups. Individuals with a combination of stroke and cognitive impairment had the greatest number of total BADL and IADL tasks with disability compared to those with either of these conditions alone. The level of difficulty in all tasks experienced by individuals with stroke or cognitive impairment was less than the sum of the combined contributions from stroke and cognitive impairment. However, in most cases there were no differences between the stroke and cognitive impairment groups, but the former had more difficulty with a BADL task (dressing) and the latter had more difficulty in some IADL tasks (using the telephone, transport, and managing finances). Regardless of the group, the most difficult BADL and IADL tasks were respectively bathing and heavy housework, while the least difficult ones were eating and taking medication.
The prevalence of disabilities in people with combined stroke and cognitive impairment was higher than those with either of these conditions alone. Previous studies concluded that stroke patients with cognitive impairments having worse ADL disabilities than those without20, 21. However, the prevalence in either the stroke or cognitive impairment group in the current study were relatively lower than those in previous studies12, 16, 22. This could be because individuals in the present study were community-dwelling adults, who may have had better functional statuses and independent abilities with better cognitive and physical functions than individuals living in the institutions. Another interesting finding was the hierarchical relationship between IADL and BADL disabilities that existed in all groups. Prior research reported the sequential relationship of the majority of older adults having mobility limitations first and then IADLs being affected, and finally BADLs being impaired23. Hoeymans and colleagues further categorized disability into four levels-no disability, IADL disabilities only, combination of IADL disabilities and mobility limitations, and both IADL and BADL disabilities24, 25. Yeh and colleagues further determined cutoff points of dependence with IADLs and BADLs when individuals had difficulties with four and seven of nine items, respectively, in the physical mobility domain23.
Individuals with combined stroke and cognitive impairment had the greatest number of summed BADL and IADL tasks with disabilities compared those with either of these conditions alone, which is in line with previous studies7. The current study additionally analyzed the level of difficulty with each IADL and BADL task among groups, and unsurprisingly showed that the combination group had the highest levels of difficulty compared to all other groups. It is worth noting that no differences were found in the majority of BADL and IADL tasks between the stroke and cognitive impairment groups, but the stroke group had more difficulty than the cognitive impairment group with dressing. Dressing requires upper limb function, which was reported to be more associated with ADLs, while lower limb function is more related to IADLs26. The stroke group in the current study had worse upper limb function than the cognitive impairment group, and this might be the reason. Although similar motor recovery of the upper and lower limbs following stroke, usually the upper limb has slower recovery rate compared to the lower limb27. On the contrary, the cognitive impairment group had more difficulty than the stroke group in using the telephone, transport, and managing finances, which require high cognitive demands. Using the telephone needs a series of actions to be performed, including picking up the phone, checking the number, making a call, and communicating with people. Transportation requires not only correct orientation but also driving or organizing other means of transport. Managing finances also requires more-complex thinking and organizational skills, such as paying bills and managing financial assets. Recent evidence showed that non-demented individuals with mild cognitive impairment (MCI) already have increasing difficulties with IADL tasks, particularly in using the telephone, transportation, taking medications, and handling their finances, which are more likely to be vulnerable to early cognitive decline28, 29. Nearly 60% of our participants in the cognitive impairment group had mild cognitive dysfunction, and therefore they had begun to have difficulty in the above-mentioned tasks. In fact, IADLs require greater interactions with physical and social environments and a greater degree of skill (e.g., problem-solving and social skills) than basic self-care tasks. Any underlying impairment in a person’s sensorimotor, cognitive-perceptual, or psychosocial capacity tends to affect the performance of IADL tasks to a greater degree than they affect basic self-care. Thus, individuals with cognitive impairment reasonably have more difficulties or need more assistance with IADL tasks.
It is also important to note that the most difficult BADL and IADL tasks were bathing and heavy housework respectively while the least difficult ones were eating and medication, regardless of the groups. It seems that some of the BADL or IADL tasks are inherently difficult or easy, and disorder only increases difficulty rather than changes the order of difficulty. Morris and colleagues reported a hierarchy of ADLs: the early loss function is hygiene, the mid-loss functions are toilet use and locomotion, and the late loss function is eating30, which is consistent with our findings. It was observed in clinical practice that bathing is the most difficult and least independent task in BADLs for disabled people because bathing involves a complex interplay of factors. Bathing can only be done in the bathroom, an environment that is relatively dangerous where people are most prone to falling. It may also require assistive devices and more procedures to complete the activity.
The difficulty of IADL tasks is more closely associated with cognitive demands. The more difficult IADLs require higher cognitive abilities. Loss of the ability to complete IADL tasks can be among the earliest signs of MCI, especially those cognitively demanding tasks31 or ones involving memory or complex reasoning, whereas more-basic activities might not yet be affected32. In the current study, only 30% of individuals in the cognitive impairment group were independent in BADLs and IADLs, but 60% of them had only mild cognitive dysfunction, indicating that cognitive function has great impacts on IADLs. In fact, a previous report showed that problems with IADLs could be indicative of an early cognitive disorder, and those with self-reported IADL impairment are more likely to convert to dementia26.
There are some limitations to this study. First, individuals in the present study were community-dwelling middle-aged and older adults, who may have had relatively better functional statuses and independent abilities with better cognitive and physical functions than individuals living in institutions. This limits the generalizability of our results to institution-living older populations and likely overestimated the disability measures. Second, for the cross-sectional design, because the exposure and outcome are simultaneously assessed, there is generally no evidence of a temporal relationship between exposure and outcome. In our study, therefore, we could not determine the causal relationship between the impairment and the disability. Third, because information was retrieved using questionnaires, the severity of the stroke and the post-stroke duration were unknown. Fourth, although this is a nationally representative sample with a sample size that exceeded 3000, the stroke group only accounted for 4%, the cognitive impairment group for 12%, and the combination group for 2% of the sample.
In summary, individuals with comorbidities of stroke and cognitive impairment had the highest prevalence of disabilities in both BADLs and IADLs, the greatest number of summed BADL and IADL tasks with disabilities, and the highest level of difficulty for each BADL and IADL task. However, similar prevalence, similar numbers of summed BADL and IADL tasks with disability, and similar levels of difficulty for each BADL and IADL task were found between the stroke group and cognitive impairment group, but the former had more difficult in dressing and the latter had more difficult in using the telephone, transport, and managing finances. For all participants, the most difficult BADL and IADL tasks were bathing and heavy housework respectively, while the least difficult ones were eating and taking medications. Our findings suggest that medical practitioners and clinical therapists should develop interventions or compensatory strategies, such as cognitive and physical training as well as ADL skill training, focus on secondary prevention of dementia and improve motor functional capacity to reduce loss of ADLs. Additionally, assessments and training of cognitive function after a stroke are important and necessary to reduce the severity of disabilities caused by the combined contributions from stroke and cognitive impairment.
Methods
Data source and study population
Data were obtained from the Taiwan Longitudinal Study on Aging (TLSA), Health and Welfare Data Science Center, Ministry of Health and Welfare (HWDC, MOHW), a nationwide representative survey conducted since 1989 with a follow-up every 3–4 years and a response rate up to 90%. The survey was initiated by the Taiwan Health Promotion Administration, Ministry of Health and Welfare as a collaborative effort with the University of Michigan. Details of the study design have been described previously33,34,35.The first interviews were conducted in 1989 (cohort I), and people aged 60 years and older living in the community were recruited. Follow-up surveys were conducted in 1993, 1996, 1999, 2003, 2007, and 2011. In 1996 (cohort II) and 2003 (cohort III), new samples of individuals aged 50 years and above were respectively interviewed. Death was the major cause of the decline in the sample size. Participants lost to attrition were more likely to have been older adults, males, and individuals who were socially inactive and had poorer physical functioning36. Data were collected through face-to-face interviews in Mandarin Chinese and included background information, household information, work history, and health status. The data used in this research were from the 2011 TLSA survey, which included the first, second, and third cohorts respectively enrolled in 1989, 1996, and 2003. The original sample comprised 3727 people, and those with incomplete demographic data, comorbidities, cognitive function, physical function, BADLs, or IADLs were excluded. The Taipei Medical University Joint Institutional Review Board (JIRB no. N201905090) approval and waivers for informed consent were obtained. This study was conducted in accordance with the Declaration of Helsinki.
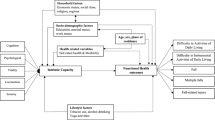
Participants were categorized into four groups: control, stroke, cognitive impairment, and combination of stroke and cognitive impairment groups according to their history of stroke and scores on the Short Portable Mental State Questionnaire (SPMSQ)37, which has been commonly used in stroke survivors38, 39.A stroke diagnosis was either self- or proxy-reported affirmative to the question: “Has this disease been diagnosed by a doctor?” Cognitive impairment was identified based on the SPMSQ with more than three errors. Individuals without stroke or cognitive impairment served as a reference population (i.e., controls), while individuals with stroke and cognitive impairment comorbidity were classified into the combination group.
Outcome measurements
Demographic data
Demographic characteristics were age (categorized as 55–65, 65–75, 75–85, and > 85 years), sex (male and female), marital status, educational level, comorbidities, cognitive function, and upper and lower limb functions. Marital status was categorized into married (married or living with a partner) and single (living without a partner such as separated, divorced, widowed, or never married). Educational level was determined by asking the participants how many years of formal education they had received and categorizing the answers into elementary school (including those who had received no formal education), junior high school, senior high school, and college and above. Self-reported comorbidities, including hypertension, diabetes, heart disease, cancer, lung disease, arthritis, and hyperlipidemia, were transformed into a comorbidity count classified as 0–2 and ≥ 3. Cognitive function was determined by the SPMSQ, which is a 10-item measure focusing on orientation, memory, and concentration. The Chinese version of SPMSQ has been validated with 0.70 for the test–retest reliability and 0.72 for the split-half coefficient of alpha40, 41. Scoring reflects the number of errors: 0–2 errors indicates normal mental functioning; 3 or 4 errors mild cognitive impairment; 5–7 errors moderate cognitive impairment, and ≥ 8 errors severe cognitive impairment. The internal consistency reliability of the SPMSQ in this study was 0.781. Upper limb function was defined by asking whether participants were able to hold or twist things with their fingers, while lower limb function was defined by asking whether participants were able to walk a distance of 200–300 m without the assistive device. The upper and lower limb functions used a 4-point Likert-scale in which a response of 0 indicated no difficulty and a response of 3 an inability to perform the function.
BADLs and IADLs
BADLs are commonly measured using the barthel index (BI)42, and various studies involving this index have been published in older adults43, patients with stroke11, and those with cognitive impairment44. Validity and reliability of Chinese version of BI have been substantiated in both Taiwanese and Chinese older adults45, 46. The current study used a six-item modified version of the original 10 items. Items included bathing, dressing, eating, transferring, indoor walking, and toileting. On the other hand, the Lawton-Brody Instrumental Activities of Daily Living Scale8 is a popular assessment of IADLs, which has been validated in a previous study47, and multiple studies involving this measurement have been published in older adults48, patients with stroke49, and those with cognitive impairment50. The current study used a nine-item modified version of the original eight items, with housework subdivided into light and heavy housework, and additionally including transport, managing finances, shopping, laundry, medication, food preparation, and using the telephone. Both BADLs and IADLs used a four-point Likert-scale with no difficulty (score of 0), some difficulty (1), great difficulty (2), and inability (3). Any item of BADLs or IADLs rated as having any degree of difficulty (> 0) was defined as a disability. For participants affected by cognitive impairment or illiteracy, a proxy respondent was used. The internal consistency reliabilities of the BADL and IADL measures in the present study were 0.930 and 0.921, respectively, determined by the Cronbach's alpha.
Statistical analysis
Categorical variables are expressed as numbers and percentages, and continuous variables are expressed as means and standard deviations (SDs) without adjustments in the text, figures and tables. A Chi-squared test was used to identify differences in demographic factors, comorbidities, and cognitive and physical functions among the control, stroke, cognitive impairment, and combination groups. The same test was used again to compare prevalence of disabilities in BADLs and IADLs among the groups. In order to compare the numbers of disabled BADL and IADL tasks and the level of difficulty in each BADL and IADL task among groups, an analysis of covariance (ANCOVA) with demographics (sex, education, age, marital status, and number of comorbidities) as the covariates were implemented. In order to reduce the chance of a type I error, the more conservative Bonferroni post-hoc test was used. SPSS version 19 (SPSS, IBM, Armonk, NY, USA) was used, and the alpha level of statistical significance was set to 0.05.
References
Ihle-Hansen, H. et al. Incidence and subtypes of MCI and dementia 1 year after first-ever stroke in patients without pre-existing cognitive impairment. Dement. Geriatr. Cognit. Disord. 32, 401–407 (2011).
Rasquin, S. M. C., Verhey, F. R. J., VanOostenbrugge, R. J., Lousberg, R. & Lodder, J. Demographic and CT scan features related to cognitive impairment in the first year after stroke. J. Neurol. Neurosurg. Psychiatry 75, 1562–1567 (2004).
Sachdev, P. S. et al. Clinical determinants of dementia and mild cognitive impairment following ischaemic stroke: the Sydney stroke study. Dement. Geriatr. Cognit. Disord. 21, 275–283 (2006).
Rajan, K. B., Aggarwal, N. T., Wilson, R. S., Everson-Rose, S. A. & Evans, D. A. Association of cognitive functioning, incident stroke, and mortality in older adults. Stroke 45, 2563–2567 (2014).
Heshmatollah, A., Mutlu, U., Koudstaal, P. J., Ikram, M. A. & Ikram, M. K. Cognitive and physical impairment and the risk of stroke—a prospective cohort study. Sci. Rep. 10, 6274 (2020).
IJmker, T. & Lamoth, C. J. C. Gait and cognition: the relationship between gait stability and variability with executive function in persons with and without dementia. Gait Posture 35, 126–130 (2012).
Stamm, B. J., Burke, J. F., Lin, C. C., Price, R. J. & Skolarus, L. E. Disability in community-dwelling older adults: exploring the role of stroke and dementia. J. Prim. Care Community Health 10, 2150132719852507 (2019).
Lawton, M. P. & Brody, E. M. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9, 179–186 (1969).
Hartman-Maeir, A., Soroker, N., Ring, H., Avni, N. & Katz, N. Activities, participation and satisfaction one-year post stroke. Disabil. Rehabil. 29, 559–566 (2007).
Mayo, N. E., Wood-Dauphinee, S., Coˆte, R., Durcan, L. & Carlton, J. Activity, participation, and quality of life 6 months poststroke. Arch. Phys. Med. Rehabil. 83, 1035–1042 (2002).
Carod-Artal, F. J., González-Gutiérrez, J. L., Herrero, J. A. E., Horan, T. & De Seijas, E. V. Functional recovery and instrumental activities of daily living: follow-up 1-year after treatment in a stroke unit. Brain Inj. 16, 207–216 (2002).
Hackett, M. L., Duncan, J. R., Anderson, C. S., Broad, J. B. & Bonita, R. Health-related quality of life among long-term survivors of stroke: results from the Auckland stroke study, 1991–1992. Stroke 31, 440–447 (2000).
Wilkinson, P. R. et al. A long-term follow-up of stroke patients. Stroke 28, 507–512 (1997).
Liu, K. P. Y. et al. Activities of daily living performance in dementia. Acta Neurol. Scand. 116, 91–95 (2007).
Njegovan, V., Man-Son-Hing, M., Mitchell, S. L. & Molnar, F. J. The hierarchy of functional loss associated with cognitive decline in older persons. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 56, M638–M643 (2001).
Juva, K. et al. Staging the severity of dementia: comparison of clinical (CDR, DSM-III-R), functional (ADL, IADL) and cognitive (MMSE) scales. Acta Neurol. Scand. 90, 293–298 (1994).
Barberger-Gateau, P., Fabrigoule, C., Rouch, I., Letenneur, L. & Dartigues, J.-F. Neuropsychological correlates of self-reported performance in instrumental activities of daily living and prediction of dementia. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 54, P293–P303 (1999).
Tuokko, H., Morris, C. & Ebert, P. Mild cognitive impairment and everyday functioning in older adults. Neurocase 11, 40–47 (2005).
Mariani, E. et al. Influence of comorbidity and cognitive status on instrumental activities of daily living in amnestic mild cognitive impairment: results from the ReGAl project. Int. J. Geriatr. Psychiatry 23, 523–530 (2008).
Babulal, G. M., Huskey, T. N., Roe, C. M., Goette, S. A. & Connor, L. T. Cognitive impairments and mood disruptions negatively impact instrumental activities of daily living performance in the first three months after a first stroke. Top. Stroke Rehabil. 22, 144–151 (2015).
Blomgren, C. et al. Long-term performance of instrumental activities of daily living in young and middle-aged stroke survivors—impact of cognitive dysfunction, emotional problems and fatigue. PLoS ONE 14, e0216822 (2019).
Singam, A., Ytterberg, C., Tham, K. & von Koch, L. Participation in complex and social everyday activities six years after stroke: predictors for return to pre-stroke level. PLoS ONE 10, e0144344 (2015).
Yeh, T.-T., Wang, C.-Y., Lin, C. F. & Chen, H.-Y. The hierarchical relationship between mobility limitation and ADL disability in older Taiwanese persons. Formos. J. Phys. Ther. 35, 1–7 (2010).
Hoeymans, N., Feskens, E. J., Van denBos, G. A. & Kromhout, D. Age, time, and cohort effects on functional status and self-rated health in elderly men. Am. J. Public Health 87, 1620–1625 (1997).
Hoeymans, N., Wouters, E. R. C. M., Feskens, E. J. M., van denBos, G. A. M. & Kromhout, D. Reproducibility of performance-based and self-reported measures of functional status. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 52, M363–M368 (1997).
Barberger-Gateau, P., Rainville, C., Letenneur, L. & Dartigues, J.-F. A hierarchical model of domains of disablement in the elderly: a longitudinal approach. Disabil. Rehabil. 22, 308–317 (2000).
Paci, M., Nannetti, L., Casavola, D. & Lombardi, B. Differences in motor recovery between upper and lower limbs: does stroke subtype make the difference?. Int. J. Rehabil. Res. 39, 185–187 (2016).
Cromwell, D. A., Eagar, K. & Poulos, R. G. The performance of instrumental activities of daily living scale in screening for cognitive impairment in elderly community residents. J. Clin. Epidemiol. 56, 131–137 (2003).
Kim, K. R. et al. Characteristic profiles of instrumental activities of daily living in different subtypes of mild cognitive impairment. Dement. Geriatr. Cognit. Disord. 27, 278–285 (2009).
Morris, J. N., Berg, K., Fries, B. E., Steel, K. & Howard, E. P. Scaling functional status within the interRAI suite of assessment instruments. BMC Geriatr. 13, 128 (2013).
Reppermund, S. et al. The relationship of neuropsychological function to instrumental activities of daily living in mild cognitive impairment. Int. J. Geriatr. Psychiatry 26, 843–852 (2011).
Perneczky, R. et al. Impairment of activities of daily living requiring memory or complex reasoning as part of the MCI syndrome. Int. J. Geriatr. Psychiatry A J. Psychiatry Late Life Allied Sci. 21, 158–162 (2006).
Zimmer, Z., Martin, L. G. & Chang, M.-C. Changes in functional limitation and survival among older Taiwanese, 1993, 1996, and 1999. Popul. Stud. (N.Y.) 56, 265–276 (2002).
Hsu, H.-C. Gender disparity of successful aging in Taiwan. Women Health 42, 1–21 (2005).
Chiu, C.-J., Wray, L. A. & Ofstedal, M. B. Diabetes-related change in physical disability from midlife to older adulthood: evidence from 1996–2003 survey of health and living status of the elderly in Taiwan. Diabetes Res. Clin. Pract. 91, 413–423 (2011).
Chiao, C., Botticello, A. & Fuh, J.-L. Life-course socio-economic disadvantage and late-life cognitive functioning in Taiwan: results from a national cohort study. Int. Health 6, 322–330 (2014).
Pfeiffer, E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J. Am. Geriatr. Soc. 23, 433–441 (1975).
Stein, J. et al. Use of a standardized assessment to predict rehabilitation care after acute stroke. Arch. Phys. Med. Rehabil. 96, 210–217 (2015).
Han, Y. et al. Chinese family caregivers of stroke survivors: determinants of caregiving burden within the first six months. J. Clin. Nurs. 26, 4558–4566 (2017).
Chi, I. & Boey, K. W. Hong Kong validation of measuring instruments of mental health status of the elderly. Clin. Gerontol. 13, 35–51 (1993).
Chou, K.-L. Hong Kong Chinese everyday competence scale: a validation study. Clin. Gerontol. 26, 43–51 (2003).
Mahoney, F. I. &Barthel, D. W. Functional evaluation: the Barthel Index: a simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md. State Med. J. (1965).
Sainsbury, A., Seebass, G., Bansal, A. & Young, J. B. Reliability of the barthel index when used with older people. Age Ageing 34, 228–232 (2005).
Wang, Z. et al. Influence of lifestyles on mild cognitive impairment: a decision tree model study. Clin. Interv. Aging 15, 2009–2017 (2020).
Chen, Y. J., Dai, Y. T., Yang, C. T., Wang, T. J. &Teng, Y. H. A review and proposal on patient classification in long-term care system. Dep. Heal. Repub. China Taipei, Taiwan (1995).
Hou, D. Z., Zhang, Y., Wu, J. L., Li, Y. & An, Z. P. Study on reliability and validity of Chinese version of Barthel Index. Clin. Focus 27, 219–221 (2012).
Tong, A. Y. C. & Man, D. W. K. The validation of the Hong Kong Chinese version of the Lawton instrumental activities of daily living scale for institutionalized elderly persons. OTJR Occup. Particip. Heal. 22, 132–142 (2002).
Brigola, A. G., Ottaviani, A. C., Alexandre, T. S., Luchesi, B. M. & Pavarini, S. C. I. Cumulative effects of cognitive impairment and frailty on functional decline, falls and hospitalization: a four-year follow-up study with older adults. Arch. Gerontol. Geriatr. 87, 105 (2020).
van deVen, R. M. et al. The influence of computer-based cognitive flexibility training on subjective cognitive well-being after stroke: A multi-center randomized controlled trial. PLoS ONE 12, e0187582 (2017).
Ashendorf, L. et al. Clinical utility of select neuropsychological assessment battery tests in predicting functional abilities in dementia. Arch. Clin. Neuropsychol. Off. J. Natl. Acad. Neuropsychol. 33, 530–540 (2018).
Acknowledgements
This work was supported by the Taipei Medical University (Grant Number TMU106-AE1-B50).
Author information
Authors and Affiliations
Contributions
P.H.L. designed the study, H.Y.Y. performed the statistical analysis, W.L.H. and V.J.Y.C. interpreted the results and prepared the tables and figures. P.H.L., T.T.Y. and S.C.L. drafted the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, PH., Yeh, TT., Yen, HY. et al. Impacts of stroke and cognitive impairment on activities of daily living in the Taiwan longitudinal study on aging. Sci Rep 11, 12199 (2021). https://doi.org/10.1038/s41598-021-91838-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91838-4
This article is cited by
-
Evaluation of the functional outcome and mobility of patients after stroke depending on their cognitive state
Scientific Reports (2024)
-
Dynamic changes and lifetime effect of functional disability profiles for stroke patients: real-world evidence from South Korea
Quality of Life Research (2024)
-
Long-term psychological outcomes following stroke: the OX-CHRONIC study
BMC Neurology (2023)
-
Change in functional disability and its trends among older adults in Korea over 2008–2020: a 4-year follow-up cohort study
BMC Geriatrics (2023)
-
Functional disability and its associated factors among the elderly in rural India using LASI Wave 1 data
Journal of Public Health (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.