Abstract
Sentinel lymph node biopsy (SLNB) for axillary lymph node staging in early breast cancer has been widely recognized. The combination of radio-colloids and dye method is the best method recognized. The reagents and equipment required in the process of the combined method are complex and expensive, so there are certain restrictions in the use of primary medical institutions. As a new tracer, fluorescent tracer technology has attracted much attention. We aimed to evaluate the feasibility and safety of fluorescein for SLNB in breast cancer. In this study, a total of 123 patients with breast cancer were divided into group A (n = 67) and group B (n = 56). The efficacy of Indocyanine green (ICG) combined with methylene blue (group A) and fluorescein combined with methylene blue (group B) in SLNB of breast cancer was compared, complications were observed at the same time. No local or systemic reactions were observed in the two groups. In group A, Sentinel lymph nodes of breast cancer were detected in 63 patients, with a detection rate of 94.0% (63/67), a false-negative rate of 7.5% (4/53). In group B, Sentinel lymph nodes of breast cancer were detected in 52 patients, with a detection rate of 92.9% (52/56), a false-negative rate of 7.5% (3/40). There was no significant difference in biopsy results between the two groups. This prospective clinical study suggests that SLNB using fluorescein and ultraviolet LED light is feasible in breast cancer patients. No adverse reactions were observed in this study, but larger studies are needed to properly assess the adverse reaction rate.
Similar content being viewed by others
Introduction
Sentinel lymph node biopsy (SLNB) for axillary lymph node staging in early breast cancer has been widely recognized. Blue dye, radio-colloids, or both can be used to identify the sentinel lymph node1,2. The biggest problem of SLNB using blue dye alone is that its detection rate is only 70–86%. The combination of radio-colloids and the blue dye method can significantly improve the detection rate of SLNB, which is the best method recognized in the clinic3. However, Radio-colloids are expensive, complex, require the cooperation of the nuclear medicine department, which is difficult to carry out in primary hospitals. Also, It needs to be injected preoperatively, which can cause significant pain to patients and also cause concern for patients and physicians about radiation exposure.
As a new tracer, fluorescent tracer technology has attracted much attention4. Indocyanine green (ICG) is the most commonly used fluorescent tracer5. It reflects fluorescence when excited by certain wavelengths of near-infrared light, and the signal is processed by a computer to transmit the image to a screen. Therefore, a fluorescent imaging system with a near-infrared camera is required to perform SLNB by looking at the monitor rather than the surgical field.
Fluorescein is a fluorescent tracer widely used in ophthalmology and optometry. It can be excited by ultraviolet or blue light through thin tissue to appear green and yellow light. SLNB use fluorescein requires an only blue or ultraviolet light torch, which reduces the cost of surgery and is easy to be applied in primary hospitals. Recent animal studies have shown that fluorescein can also be used to locate axillary lymph nodes in rabbits6.
In this study, the efficacy of ICG combined with methylene blue and fluorescein combined with methylene blue in SLNB of breast cancer was compared.
Materials and methods
Clinical data
From July 2019 to December 2020, 123 patients with feasible SLNB of breast cancer admitted to our hospital were studied. According to the order of admission, they were divided into group A (n = 67) and group B (n = 56). (Table 1) All of them provided written informed consent. The protocol and consent procedures were approved by the Institutional Review Board of Zibo Central Hospital affiliated with Shandong First Medical University, and all experiments were performed following relevant guidelines and regulations. The Chinese Clinical Trial Registry (available at http://www.chictr.org.cn/) approved the clinical nature of this study (registration number: ChiCTR2000036990).
Methods
First, the fluorescent dye was injected. ICG solution was used in group A (25 mg ICG powder was diluted with 9 mL of water for injection, and then 0.1 mL of the diluted solution was extracted with a 1 mL syringe and continued to be diluted to 1 mL with 0.9% normal saline), and fluorescein solution was used in group B(1:5 fluorescein solution (10% fluorescein solution 1 mL and 0.9% normal saline 4 mL were mixed into the solution, with an average pH value of 8.97 (8.95–9.02)7). The intradermal injection was made into the outer upper quadrant of the areola at 3–4 points, the total amount is about 0.1 to 0.3 ml. Group B patients were tested for fluorescein allergy (0.1 ml 10% fluorescein solution was diluted to 5 ml with 0.9% normal saline, injected intravenously, and observed for 10 min) no positive results were found8.
After 3 min, a 1 ml syringe was used to select 1–3 points on the outside of the areola for intradermal injection of methylene blue, with a total amount of about 0.1–0.3 ml.
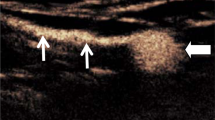
10 min later, the operating lights were turned off. The images of group A were collected using the near-infrared camera system, and group B was marked with an ultraviolet (wavelength 395 nm) LED torch (LOFTEK, China) to mark the direction of lymph vessels and the location of their disappearance (Fig. 1).
An incision was made approximately 1 cm from the distal end of lymph vessel disappearance. If there is no obvious lymph vessel, an incision is made at the inferior axillary fold. Group A was guided by an infrared probe and group B was guided by the ultraviolet LED torch to identify the fluorescent and methylene blue-stained lymph vessels, and then followed the lymph vessels to remove the sentinel lymph nodes (Fig. 2).
All lymph nodes were examined by frozen pathology and conventional paraffin pathology. For the sentinel lymph nodes with no metastatic cancer, only the lower axillary lymph nodes were dissected. Routine axillary lymph node dissection was performed in patients with sentinel lymph node metastasis.
Main outcome measures
The results of SLNB in groups A and B were compared, including detection rate, false-negative rate, number of sentinel lymph nodes.
Evaluation of complications in fluorescein group
Anaphylaxis and systemic urticaria were observed within 20 min of the operation. The skin necrosis at the injection site was observed within 1 week. Liver and kidney functions were measured 7 days after the operation. The color changes of skin and urine at the injection site were observed 2 days after the operation.
Statistical analysis
All statistics were analyzed using IBM SPSS 22.0 statistics software. (IBM Co., Armonk, NY, USA) Continuous variables are expressed as median or mean, and categorical variables as percentages. T-test was used for the comparison of measurement data and X2 test was used for the comparison of counting data. When the p-value was less than 0.05, the difference was considered statistically significant.
Results
Comparison of biopsy results between the two groups
A total of 123 eligible women with breast cancer were enrolled (Table 1). The patients ranged in age from 26 to 73 years.
No local or systemic reactions were observed in 67 patients in group A. Sentinel lymph nodes of breast cancer were detected in 63 patients, with a detection rate of 94.0% (63/67), a false-negative rate of 7.5% (4/53).
Group B was no local or systemic adverse reactions in 56 patients. Sentinel lymph nodes of breast cancer were detected in 52 patients, with a detection rate of 92.9% (52/56), a false-negative rate of 7.5% (3/40). There was no significant difference in biopsy results between the two groups (Table 2).
Sentinel lymph node biopsy details
The median time from the injection of fluorescein and ICG to the initial incision was 35 and 14 min, respectively, and the median time from the initial incision to the end of the sentinel node biopsy was 15 min with the ultraviolet LED light. There was no significant difference in the median number of sentinel lymph nodes detected between the two methods (3.0 VS 3.5, p = 0.406) . Sentinel lymph nodes were detected in 52 of the 56 patients in group B, and the detection rate was no different from that in group A (92.9% VS 94.0%, P = 1.000). In group A, SLNB found metastasis in 49 cases, axillary lymph node dissection found metastasis in 53 cases, with a false-negative rate of 7.5% (4/53).In group B, SLNB found metastasis in 37 cases, axillary lymph node dissection found metastasis in 41 cases. Among them, 1 case in the fluorescein group was unsuccessful in SLNB, and the dissected axillary lymph node had metastasis, with a false-negative rate of 7.5% (3/40), and there was no significant difference between the two groups (P = 1.000).
Complications
None of the patients showed anaphylaxis or systemic urticaria after intradermal injection of fluorescein, and no skin necrosis was observed at the injection site. Serum creatinine and liver function were in the normal range on day 1, day 8, and month 1. All patients' urine glowed yellow within 10 min of fluorescein injection, but for no more than a day. Skin discoloration also disappears within a day.
Discussion
The detection rate of the fluorescein combined with methylene blue group was 92.9%, and sentinel lymph nodes were visible under ultraviolet LED light, which was easy to be detected in most patients. Sentinel lymph node biopsy was unsuccessful in 4 cases, and axillary lymph node metastasis was found in 1 case. In the early stages of this study, it was difficult to detect sentinel lymph node using fluorescein in patients with relatively high body mass index. It is well known that weight is a predictor of failure to identify sentinel lymph node, however, once researchers were familiar with the use of fluorescein and ultraviolet LED light, BMI did not affect SLNB.
Studies on SLNB with ICG showed that this reagent was a feasible lymph node localization agent with a high detection rate and low false-negative rate9. However, because ICG emits light at a wavelength of 830 nm (nm), this is considered near-infrared, A fluorescence imaging system with a near-infrared camera is required, and SLNB should be performed by looking at the monitor rather than the field10,11,12. In contrast, fluorescein emits light with a wavelength of 512 nm, which is in the visible spectrum. Thus, surgeons can perform SLNB by visually observing the operating area without using special equipment.
The injected fluorescein is delivered to the liver and rapidly converted into fluorescein glucuronic acid, which is then excreted in the urine at a 1.75 mL /min/kg renal clearance rate13. Discoloration of the urine was observed in all patients injected with fluorescein, but this did not last for more than 24 h. There was no abnormal creatinine or liver function, no allergic reaction, or general urticaria. The commonly used intravenous dose of fluorescein for retinal angiography is 250–500 mg14. In this study, however, only 80 mg of fluorescein (4 ml 1:5 diluted 10% fluorescein) was intradermally injected for SLNB in each patient, and no systemic complications. The mean pH of 1:5 diluted 10%fluorescein was 8.96. Because it is weakly alkaline, the injection site was carefully monitored due to the intradermal injection. However, no local complications such as skin necrosis, pain, or burning were observed in any of the patients.
However, our study had several limitations. First, no patients detected sentinel lymph node in the inner breast quadrant with this drug. Therefore, the feasibility of SLNB in the inner breast quadrant with fluorescein and ultraviolet LED cannot be evaluated. Therefore, further evaluation of larger sample size is needed. Second, fluorescein emits enough light to penetrate thin tissue, but not the thick tissue that includes underarm skin and subcutaneous fat. Therefore, the exact location of the SLN cannot be observed until the skin is cut open. Besides, if techniques using fluorescein are further optimized and developed, for example, to monitor the signal intensity of reflected light in real-time, then unnecessary removal of worthless lymph nodes as sentinel lymph nodes can be avoided.
Despite the limitations, this prospective clinical study suggests that SLNB using fluorescein and ultraviolet LED light is feasible in breast cancer patients. Since the technology uses light in the visible spectrum, it is easy to use and economical, etc., if the results of further research also prove the effectiveness of the technology, it will be likely to be widely used. At the same time, no adverse reactions were observed in this study, but larger studies are needed to properly assess the adverse reaction rate.
References
Giuliano, A. E. et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: The ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA 318(10), 918–926. https://doi.org/10.1001/jama.2017.11470 (2017).
Galimberti, V. et al. Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23–01): 10-year follow-up of a randomised, controlled phase 3 trial. Lancet Oncol. 19(10), 1385–1393. https://doi.org/10.1016/s1470-2045(18)30380-2 (2018).
Simmons, R. M., Smith, S. M. & Osborne, M. P. Methylene blue dye as an alternative to isosulfan blue dye for sentinel lymph node localization. Breast J. 7(3), 181–183. https://doi.org/10.1046/j.1524-4741.2001.007003181.x (2001).
Ahmed, M., Purushotham, A. D. & Douek, M. Novel techniques for sentinel lymph node biopsy in breast cancer: A systematic review. Lancet Oncol. 15(8), e351–e362. https://doi.org/10.1016/s1470-2045(13)70590-4 (2014).
Pitsinis, V., Provenzano, E., Kaklamanis, L., Wishart, G. C. & Benson, J. R. Indocyanine green fluorescence mapping for sentinel lymph node biopsy in early breast cancer. Surg. Oncol. 24(4), 375–379. https://doi.org/10.1016/j.suronc.2015.10.002 (2015).
Ren, L. et al. 10 % fluorescein sodium vs 1 % isosulfan blue in breast sentinel lymph node biopsy. World J. Surg. Oncol. 14(1), 280. https://doi.org/10.1186/s12957-016-1031-1 (2016).
Doellman, D. et al. Infiltration and extravasation: Update on prevention and management. J. Infus. Nurs. 32(4), 203–211. https://doi.org/10.1097/NAN.0b013e3181aac042 (2009).
Hitosugi, M. et al. An autopsy case of fatal anaphylactic shock following fluorescein angiography: A case report. Med. Sci. Law 44(3), 264–265. https://doi.org/10.1258/rsmmsl.44.3.264 (2004).
Sugie, T. et al. Evaluation of the clinical utility of the ICG fluorescence method compared with the radioisotope method for sentinel lymph node biopsy in breast cancer. Ann. Surg. Oncol. 23(1), 44–50. https://doi.org/10.1245/s10434-015-4809-4 (2016).
Tanaka, E., Choi, H. S., Fujii, H., Bawendi, M. G. & Frangioni, J. V. Image-guided oncologic surgery using invisible light: Completed pre-clinical development for sentinel lymph node mapping. Ann. Surg. Oncol. 13(12), 1671–1681. https://doi.org/10.1245/s10434-006-9194-6 (2006).
Ogasawara, Y., Ikeda, H., Takahashi, M., Kawasaki, K. & Doihara, H. Evaluation of breast lymphatic pathways with indocyanine green fluorescence imaging in patients with breast cancer. World J. Surg. 32(9), 1924–1929. https://doi.org/10.1007/s00268-008-9519-7 (2008).
Kusano, M. et al. Sentinel node mapping guided by indocyanine green fluorescence imaging: A new method for sentinel node navigation surgery in gastrointestinal cancer. Dig. Surg. 25(2), 103–108. https://doi.org/10.1159/000121905 (2008).
Blair, N. P., Evans, M. A., Lesar, T. S. & Willett, M. Plasma fluorescein and fluorescein glucuronide in patients with selected eye diseases. Graefes Arch. Clin. Exp. Ophthalmol. 227(2), 114–117. https://doi.org/10.1007/bf02169781 (1989).
Spaide, R. F., Klancnik, J. M. Jr. & Cooney, M. J. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 133(1), 45–50. https://doi.org/10.1001/jamaophthalmol.2014.3616 (2015).
Author information
Authors and Affiliations
Contributions
N.G. contributed to the conception of the study and wrote the manuscript; A.Q.Y. performed the Data analysis/interpretation and Statistical analysis; W.H.X., J.C., X.N.L., J.Q.L. contributed significantly to the Literature research and Data acquisition; L.L.,Y.D. helped perform the Manuscript revision/review and Manuscript final version approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, L., Gao, N., Yang, A.Q. et al. Application of fluorescein combined with methylene blue in sentinel lymph node biopsy of breast cancer. Sci Rep 11, 12119 (2021). https://doi.org/10.1038/s41598-021-91641-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91641-1
This article is cited by
-
A systematic review and meta-analysis of diagnostic performance of fluorescein-guided sentinel lymph node biopsy in early breast cancer
Breast Cancer Research and Treatment (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.