Abstract
This study compared the results of the minimally invasive coracoclavicular (CC) fixation with a single TightRope (MITR) procedure and the hook plate (HP) procedure for acute acromioclavicular (AC) joint dislocation treatment. Sixteen patients with a mean age of 44.9 ± 11 years were treated with the MITR procedure. Nineteen patients with a mean age of 40.2 ± 8.7 years were treated using the HP procedure. Clinical outcomes were evaluated with the Visual Analog Scale (VAS) for pain, Constant–Murley Score (CMS), and University of California at Los Angeles (UCLA) Shoulder score. Vertical displacement of the clavicle with reference to the height of the acromion was measured in standard anteroposterior radiographs. The mean follow-up was 27 months in the MITR group and 30 months in the HP group. No statistically significant differences were found between the MITR group and the HR group in terms of VAS score (0.4 ± 0.6 vs 0.7 ± 0.6, P = 0.138), UCLA Shoulder score (33.9 ± 2.5 vs 33.7 ± 1.5, P = 0.843), or CMS (95.7 ± 7.3 vs 93.7 ± 6.6, P = 0.400). No redislocation was identified in the HP group, while redislocation occurred in 1 of 16 (6.3%) patients in the MITR group. One patient in the HP group (5.3%) had acromial osteolysis, while no acromial osteolysis was found in the MITR group. No other adverse events, such as infections, tunnel widening, fractures, or implant-related complications, were observed. Both procedures provided satisfactory results. The HP procedure provided better reduction, while the MITR procedure provided a slightly lower tendency of pain. Long-term follow-up is needed to investigate the clinical outcomes and radiological outcomes of both groups.
Similar content being viewed by others
Introduction
Acromioclavicular (AC) joint dislocations are common injuries, particularly in the active population. The Rockwood classification is the most widely used method to classify for AC joint dislocations, and it is used to grade AC joint dislocations from type I to VI based on the degree and direction of distal clavicle displacement1. Nonsurgical treatment is usually recommended for Rockwood type I and II AC joint dislocations. Type III AC joint dislocations are further classified into type IIIA (horizontally stable) and IIIB (horizontally unstable) injuries2. Nonsurgical treatment is suggested for type IIIA injuries, while surgical treatment is advocated for type IIIB injuries2. In addition, several studies recommend operations for type III injuries in heavy manual laborers and athletes3,4. Surgery is usually recommended for Rockwood type IV, V and VI AC joint injuries5,6,7.
Various surgical procedures have been proposed for the management of AC dislocations, including the Weaver–Dunn procedure; coracoclavicular (CC) joint screw fixation; CC or AC joint reconstruction with autografts, allografts or synthetic grafts; tension banding; hook plate (HP) fixation; EndoButton fixation; K-wire fixation; and so on8,9,10,11,12,13,14,15. Although the aforementioned treatment options all play a role in the management of AC joint dislocations, no gold standard of management has yet been identified.
Currently, the HP procedure and the TightRope (TR) procedure are the two most widely used methods in the management of AC dislocations. Both techniques offer safe and effective outcomes. However, the HP procedure has some disadvantages, including pain, functional limitations, subacromial impingement, rotator cuff tears, and a second operation to remove the plate15,16. In a recent systematic review, Moatshe et al.12 reported that HP and K-wire treatment had a complication rate of 26.3% and a reoperation rate of 1.2% in both acute and chronic cases. TR procedures include single TR (STR) and double TR (DTR) procedures. STR procedures require fewer tunnels, whereas DTR procedures provide better stabilization6.
According to a newly published meta-analysis by Lloyd et al.17, the TR technique resulted in better functional outcomes and a reduced Visual Analog Scale (VAS) pain score than the HP technique, whereas other studies did not come to this conclusion18,19. The present study aimed to compare the clinical and radiological results of a minimally invasive CC fixation with an STR (MITR) technique and the HP technique for acute AC joint dislocation treatment. It was hypothesized that the MITR technique would provide clinical and radiological results that were comparable with those of the HP technique.
Patients and methods
Patient data
The study protocol was approved by the Institutional Review Board of the Second Affiliated Hospital of Soochow University. All patients provided informed consent for the procedure and study inclusion in written format. All methods were carried out in accordance with relevant guidelines and regulations.
From July 2016 to October 2018, 41 patients with acute AC joint dislocations (type III and V) were treated with surgery in our department. Eighteen patients underwent MITR (the MITR group) (Fig. 1a), and 23 patients were treated with open reduction and internal fixation using an HP (the HP group) (Fig. 1b). We conducted a retrospective study to compare MITR and HP results for acute AC joint dislocation treatment.
Inclusion criteria were as follows: (1) Rockwood type III injuries (only manual workers, overhead workers or active individuals); (2) Rockwood type V injuries; (3) acute injuries (< 3 weeks after injury); (4) age 18–60 years; (5) first-time injury of the AC joint; (6) primary treatment with HP fixation or MITR reconstruction; (7) follow-up time of at least 15 months; and (8) implants removed at the last follow-up in the HP group.
Exclusion criteria were as follows: (1) chronic injuries (> 3 weeks after injury); (2) previous AC joint injuries; (3) associated diseases that could influence assessment (e.g., cognitive impairment, psychiatric disorders, neuromuscular, and rheumatological disease); (4) abnormal shoulder function before the injury, with an inability to freely use shoulder joints in work and life (e.g., neuromuscular disorder); (5) fractures and/or dislocations in other parts of the ipsilateral limb; and (6) association with vascular or nerve injury.
HP fixation surgical technique
The patient was placed in a beach-chair position under general anesthesia. A 6-cm transverse skin incision was made along the distal clavicle to the acromion, and the AC joint was subsequently exposed. Then, any articular cartilage debris or hematoma in the AC joint was debrided. The hook end of a prebent plate (3.5 mm, titan, DePuy Synthes, Switzerland) was inserted underneath the acromion, and the proximal end of the plate was temporarily fixed to the clavicle with a Kocher forceps. Thus, the AC joint was reduced. The AC joint reduction status, hook depth and plate position were confirmed with intraoperative fluoroscopy in two views. Then, the HP was fixed to the clavicle with at least 3 locking screws. Intraoperative fluoroscopy was used to recheck the reduction status, plate position, hook depth and screw length. The CC ligament was not exposed. We repaired the AC joint capsule with absorbable sutures.
Pain was an indication to remove the implant. If the patient had pain after surgery, the HP was removed within 3 months. If the patient did not have pain, the recommended time of removal was 6 to 8 months after the operation.
MITR surgical technique
The patient was positioned in a beach-chair position. The AC joint was reduced and fixed with a 2.0-mm Kirschner wire. A 2-cm skin incision and a 3-cm skin incision were made to prepare the clavicle and the coracoid process, respectively. A 2.0-mm Kirschner wire was introduced from the clavicle to the coracoid. Then, a 4.0-mm drill bit was drilled from the clavicle to the base of the coracoid. A nitinol suture passing wire was advanced down through the cannulated drill bit. The drill bit was removed, and two white traction sutures were inserted into the bone tunnels through the wire loop of the nitinol suture passing wire. The oblong button was transported from the upper surface of the clavicle to the bottom of the coracoid with the two white traction sutures. The position of the oblong button was verified. Then, the round button was advanced down to the upper surface of the clavicle. Finally, the TR was fixed with sutures. The reduction was controlled with intraoperative fluoroscopy (Fig. 2).
MITR operative procedure. (a) AC joint dislocation. (b) Closed reduction and fixation of AC joint dislocation with a Kirschner wire. (c) A 2.0-mm Kirschner wire is introduced through the clavicle and coracoid. (d) A 4.0-mm drill bit is drilled into the base of the coracoid. (e) A nitinol suture passing wire is advanced down through the cannulated drill bit. (f) The drill bit is removed, and the two white traction sutures are inserted into the bone tunnels through the wire loop of the nitinol suture passing wire. (g) The TR system is introduced, and the reduction and stabilization of the AC joint are completed. (h) Final frontal view of AC joint fixed with the TR system.
Rehabilitation
The rehabilitation methods were the same in the HP group and the MITR group. Pendulum exercises and fully active movement of the elbow, wrist and hand were allowed after surgery. The arm was immobilized for one month with a sling. During the first 3 weeks, passive motion was allowed up to 45° flexion and abduction. Between 3 and 6 weeks, active-assisted movements were allowed up to 60° flexion and abduction. After the 7th week, patients were allowed to move freely. Muscle-strengthening exercises were started after 10 to 12 weeks. Heavy lifting and other strenuous activities that would lead to significant downward traction of the operated arm were prohibited within 4 months postoperatively.
Clinical evaluation
Two examiners performed follow-up evaluations (orthopedic surgeons of our department) but did not perform operations. Clinical outcomes were assessed at the last follow-up with the VAS20, Constant–Murley score (CMS)21, and University of California at Los Angeles (UCLA) Shoulder score22.
Radiographic evaluation
Standard anteroposterior radiographs of the operated shoulder were obtained at the final follow-up visit to evaluate any remaining vertical AC joint instability. The vertical displacement of the clavicle with reference to the height of the acromion was measured. We considered no displacement, displacement < 50%, and displacement > 50% with reference to the height of the acromion as reduction, subluxation and redislocation, respectively.
Statistical analysis
Statistical analyses were performed with SPSS software (ver. 20.0, IBM Inc., Chicago, USA). Continuous variables are reported as the mean ± standard deviation (SD). An independent Student’s t test or the Mann–Whitney U test was conducted to compare continuous variables with normal or non-normal distribution, respectively. The chi-square test was used to compare the categorical variables. Data are reported as the mean ± SD or median (range, minimum–maximum). Differences between the two groups were considered significant at P < 0.05.
Results
Study population
There were 16 patients (11 males, 5 females) in the MITR group and 19 patients (10 males, 9 females) in the HP group, with mean ages of 44.9 ± 11 years and 40.2 ± 8.7 years, respectively. The follow-up periods were 27 months (range 15–42 months) and 30 months (range 16–40 months) in the MITR group and HP group, respectively. Four patients (3 in the HP group and 1 in the MITR group) were lost to follow-up, and 2 patients (1 in the HP group and 1 in the MITR group) refused to participate. The right arm was affected in 6 and 9 patients in the MITR group and HP group, respectively. The length of time from injury to operation was 6.8 ± 3.1 days and 7.1 ± 2.2 days for the MITR group and HP group, respectively. There were no significant between-group differences in age, sex, laterality or the length of time from injury to operation (Table 1). The HPs were removed within 8 months postoperatively.
Clinical outcomes
Clinical outcome measures at the final follow-up are shown in Table 2. There were no significant differences in the mean VAS score, UCLA Shoulder score or CMS between the two groups.
Radiographic follow-up
In the MITR group, the anatomic reduction was finally obtained in 93.7% (15/16) of patients. In the HP group, no redislocation or subluxation was identified. There were no statistically significant differences in redislocation between the two groups (P = 0.457).
Complications
In the MITR group, one case of redislocation was observed 1 day after the operation, but the patient refused to undergo revision surgery (Fig. 3). In the HP group, one patient had acromial erosion. No other adverse events, such as infections, tunnel widening, fractures, or implant-related complications, were observed.
Discussion
The most important findings of the present study are that we found that good-to-excellent functional outcomes can be obtained with both the MITR and the HP fixation to treat type III and V AC dislocations. Additionally, this study found no significant differences in pain or functional outcomes, as evaluated using the UCLA scale, VAS and CMS, at the short-term follow-up postoperatively. However, the authors acknowledged a slightly higher tendency to a VAS for HP procedure could be observed, probably due to the stress effect of the HP on the lower surface of the acromion and the second operation for implant removal.
The HP technique is popular for the treatment of AC joint dislocation. Many studies have reported satisfying results with HP fixation16,18,23. In a prospective study, 27 acute high-grade (Rockwood grade IV/V) AC joint dislocations were treated with the HP technique. After a 24-month follow-up, satisfactory outcomes (CMS: 90.19 ± 7.79) were obtained16. Jensen et al.18 treated 30 acute Rockwood type III/V AC joint separations using the HP technique, with a median CMS of 92.4 and a median Taft score of 10. Satisfactory outcomes resulted from the superiority of the HP technique in achieving reduction in both the vertical and horizontal planes. McConnell et al.24 reported that the HP technique most closely restored the biomechanics of the AC joint to normal values. However, despite these good to excellent outcomes, several studies have reported many complications of the HP technique, such as metal breakage, clavicle and coracoid fractures, subacromial erosions, rotator cuff injury, redislocation and AC degeneration25,26,27,28. In the present study, one patient sustained subacromial erosion. No redislocation or subluxation was observed. The mean CMS was 93.7 in the HP group, which was comparable to that reported by Arirachakaran et al.25.
The TR method has been used as a surgical technique for treating AC dislocations for more than 10 years29. Whereas the TR technique is used to reconstruct disrupted CC ligaments, the HP technique is used to reconstruct the AC joint. The most crucial advantage of the TR method is that there is no need for a second operation to remove the implant. Some studies reported better results with the TR technique than the HP technique16,17. Lloyd et al.17 conducted a systematic review including 6 clinical studies with 285 patients and reported that the suture-button (including TR) technique resulted in higher CMSs and lower VAS scores. The TR procedures include both open and arthroscopic procedures. MITR was an open TR procedure performed with minimal invasiveness, with only two incisions. Abdelrahman et al.30 found that the differences in outcomes, in terms of pain, function, the length of hospitalization, and CC distance, between MITR and arthroscopic procedure were statistically nonsignificant. However, they found a higher cost and longer surgical time with the arthroscopic procedure, but the arthroscopic technique had a longer learning curve. In the present study, good to excellent early clinical results, with a mean CMS of 95.7 at the final follow-up, were achieved in the MITR group. Comparable results were reported by Jensen et al.18 in 2014, who performed arthroscopically assisted reduction of the AC joint with the DTR technique for patients with Rockwood type III and V acute injuries.
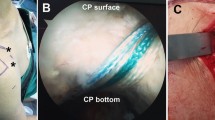
Despite the good postoperative results of the TR technique, complications have also been reported, probably owing to an initial malreduction, button displacement or inadequate healing of the disrupted ligaments31. Redislocation is a common complication of the TR technique32. In the present study, vertical redislocation with complete loss of reduction was identified in 1 patient (6.3%) in the MITR group. There are three causes of redislocation. The No. 5 suture of the TR system can sometimes be too weak, leading to redislocation. Thus, the sutures should be replaced by stronger sutures33. The 4.0 mm bone tunnel is a bit large; thus, the buttons can sometimes sink into the bone tunnel of the clavicle or coracoid34. Therefore, we designed a modified MITR procedure with a 2.5-mm bone tunnel replacing the 4.0-mm bone tunnel (Fig. 4). Finally, bone tunnel enlargement, which may be caused by residual anteroposterior instability, can lead to redislocation. Therefore, if the preoperative CT scan shows posterior displacement of the distal clavicle (type IV), additional AC fixation with two strong sutures is recommended.
MITR modified operative procedures. (a) The TR system is dismantled. (b) A 2.5-mm Kirschner wire is introduced through the clavicle and coracoid. (c,d) The two white traction sutures are passed through the tunnels using a nitinol suture passing wire. (e,f) The TR system is introduced through the tunnels using the two white traction sutures and then reassembled. (h) Final frontal view of AC joint fixation with the TR system.
The present study has several limitations that should be noted. The first limitation is the lack of preoperative scores for comparison. Second, this is a retrospective, nonrandomized control study. Third, athletic and work outcomes such as return to play or return to work may have added to the study. Fourth, the limited patient number and relatively short follow-up duration might weaken the strength of the results.
Conclusion
Both the MITR technique and the HP technique were excellent choices for treating acute AC dislocations (type III and V). The MITR procedure and HP procedure showed similar radiological and clinical results in the present study. However, the MITR procedure provided a slightly lower tendency of pain and more convenience. Long-term follow-up is needed to investigate the clinical outcomes and radiological outcomes of both groups.
References
Rockwood, C. A. & Green, D. P. Fractures in Adults 860–919 (JB Lippincott, 1984).
Beitzel, K. et al. ISAKOS Upper Extremity Committee Consensus Statement on the need for diversification of the rockwood classification for acromioclavicular joint injuries. Arthroscopy 30, 271–278 (2014).
Johansen, J. A., Grutter, P. W., McFarland, E. G. & Petersen, S. A. Acromioclavicular joint injuries: Indications for treatment and treatment options. J. Shoulder Elbow Surg. 20, S70–S82 (2011).
Seijas, R., Sallent, A. & Ares, O. Rockwood type III acromioclavicular joint dislocation; are we still fighting?. J. Investig. Surg. 31, 234–235 (2018).
Verstift, D. E., Welsink, C. L., Spaans, A. J. & van den Bekerom, M. P. J. Return to sport after surgical treatment for high-grade (Rockwood III-VI) acromioclavicular dislocation. Knee Surg. Sports Traumatol. Arthrosc. 27, 3803–3812 (2019).
Xu, J. et al. A retrospective comparative study of arthroscopic fixation in acute Rockwood type IV acromioclavicular joint dislocation: Single versus double paired Endobutton technique. BMC Musculoskelet. Disord. 19, 170 (2018).
Xue, C. et al. Truly anatomic coracoclavicular ligament reconstruction with 2 Endobutton devices for acute Rockwood type V acromioclavicular joint dislocations. J. Shoulder Elbow Surg. 27, E196–E202 (2018).
Carkci, E., Polat, A. E. & Gurpinar, T. The frequency of reduction loss after arthroscopic fixation of acute acromioclavicular dislocations using a double-button device, and its effect on clinical and radiological results. J. Orthop. Surg. Res. 15, 136 (2020).
Huang, Y. C., Yang, S. W., Chen, C. Y., Lin, K. C. & Renn, J. H. Single coracoclavicular suture fixation with Mersilene tape versus hook plate in the treatment of acute type V acromioclavicular dislocation: A retrospective analysis. J. Orthop. Surg. Res. 13, 110 (2018).
Kany, J. & Selim, H. A. Arthroscopic coracoacromial ligament transfer augmented with suspensory V-shaped fixation system for chronic acromioclavicular joint dislocation. Arthrosc. Tech. 8, e697–e703 (2019).
Lobao, M. H., Canham, R. B., Melvani, R. T., Parks, B. G. & Murthi, A. M. Synthetic coracoclavicular ligament vs coracoclavicular suspensory construct for treatment of acromioclavicular dislocation: A biomechanical study. J. Shoulder Elbow Surg. 29, 1440–1449 (2020).
Moatshe, G. et al. Acromioclavicular and coracoclavicular ligament reconstruction for acromioclavicular joint instability: A systematic review of clinical and radiographic outcomes. Arthroscopy 34, 1979–1995 (2018).
Morikawa, D. et al. Reconstruction of the acromioclavicular ligament complex using dermal allograft: A biomechanical analysis. Arthroscopy 36, 108–115 (2020).
Murray, I. R. et al. Open reduction and tunneled suspensory device fixation compared with nonoperative treatment for type-III and type-IV acromioclavicular joint dislocations: The ACORN prospective, randomized controlled trial. J. Bone Jt. Surg. Am. 100, 1912–1918 (2018).
Wang, C., Meng, J. H., Zhang, Y. W. & Shi, M. M. Suture button versus hook plate for acute unstable acromioclavicular joint dislocation: A meta-analysis. Am. J. Sports Med. 48, 1023–1030 (2019).
Stein, T. et al. Stabilization of acute high-grade acromioclavicular joint separation: A prospective assessment of the clavicular hook plate versus the double double-button suture procedure. Am. J. Sports Med. 46, 2725–2734 (2018).
Lloyd, A. J., Hurley, E. T., Davey, M. S., Pauzenberger, L. & Mullet, H. Arthroscopic suture-button versus hook-plate fixation for acromioclavicular joint injuries—A systematic review of comparative studies. Arthrosc. Sports Med. Rehabil. 2, e671–e676 (2020).
Jensen, G., Katthagen, J. C., Alvarado, L. E., Lill, H. & Voigt, C. Has the arthroscopically assisted reduction of acute AC joint separations with the double tight-rope technique advantages over the clavicular hook plate fixation?. Knee Surg. Sports Traumatol. Arthrosc. 22, 422–430 (2014).
Eschler, A., Gradl, G., Gierer, P., Mittlmeier, T. & Beck, M. Hook plate fixation for acromioclavicular joint separations restores coracoclavicular distance more accurately than PDS augmentation, however presents with a high rate of acromial osteolysis. Arch. Orthop. Trauma Surg. 132, 33–39 (2012).
Hawker, G. A., Mian, S., Kendzerska, T. & French, M. Measures of adult pain: Visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res. (Hoboken) 63, S240–S252 (2011).
Constant, C. R. & Murley, A. H. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 214, 160–164 (1987).
Kirkley, A., Griffin, S. & Dainty, K. Scoring systems for the functional assessment of the shoulder. Arthroscopy 19, 1109–1120 (2003).
Hemmann, P., Koch, M., Guehring, M., Bahrs, C. & Ziegler, P. Acromioclavicular joint separation treated with clavicular hook plate: A study of radiological and functional outcomes. Arch. Orthop. Trauma Surg. 141, 603–610 (2021).
McConnell, A. J., Yoo, D. J., Zdero, R., Schemitsch, E. H. & McKee, M. D. Methods of operative fixation of the acromio-clavicular joint: A biomechanical comparison. J. Orthop. Trauma. 21, 248–253 (2007).
Arirachakaran, A. et al. Post-operative outcomes and complications of suspensory loop fixation device versus hook plate in acute unstable acromioclavicular joint dislocation: A systematic review and meta-analysis. J. Orthop. Traumatol. 18, 293–304 (2017).
Chung, H. et al. Evaluation of three-dimensional in vivo scapular kinematics and scapulohumeral rhythm between shoulders with a clavicle hook plate and contralateral healthy shoulders. Int. Orthop. 43, 379–386 (2019).
Vajapey, S. P., Bong, M. R., Peindl, R. D., Bosse, M. J. & Ly, T. V. Evaluation of the Clavicle hook plate for treatment of acromioclavicular joint dislocation: A cadaveric study. J. Orthop. Trauma. 34, e20–e25 (2020).
Xu, D. et al. Outcomes of surgery for acromioclavicular joint dislocation using different angled hook plates: A prospective study. Int. Orthop. 41, 2605–2611 (2017).
Walz, L., Salzmann, G. M., Fabbro, T., Eichhorn, S. & Imhoff, A. B. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: A biomechanical study. Am. J. Sports Med. 36, 2398–2406 (2008).
Abdelrahman, A. A., Ibrahim, A., Abdelghaffar, K., Ghandour, T. M. & Eldib, D. Open versus modified arthroscopic treatment of acute acromioclavicular dislocation using a single tight rope: Randomized comparative study of clinical outcome and cost-effectiveness. J. Shoulder Elbow Surg. 28, 2090–2097 (2019).
Salzmann, G. M. et al. Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am. J. Sports Med. 38, 1179–1187 (2010).
Tauber, M. et al. Arthroscopic stabilization of chronic acromioclavicular joint dislocations: Triple- versus single-bundle reconstruction. Am. J. Sports Med. 44, 482–489 (2016).
Flinkkila, T. E. & Ihanainen, E. Results of arthroscopy-assisted tightrope repair of acromioclavicular dislocations. Shoulder Elbow. 6, 18–22 (2014).
Zhang, L. F., Yin, B., Hou, S., Han, B. & Huang, D. F. Arthroscopic fixation of acute acromioclavicular joint disruption with TightRope (TM): Outcome and complications after minimum 2 (2–5) years follow-up. J. Orthop. Surg. (Hong Kong) 25, 1–6 (2017).
Acknowledgements
This research was supported by the Jiangsu Province’s Young Medical Talents Program (No. QNRC2016880), Training project of “national tutor system” for young health talents in Suzhou (20042), Gusu Health Talents (GSWS2020033), the National Natural Science Foundation of China (No. 81874018), and Jiangsu Province Clinical Medical Science and Technology Project (No. BE2019661).
Author information
Authors and Affiliations
Contributions
G.S. and H.Z. conceived and designed the study. G.S. wrote the article. S.S. and G.S. measured, recorded and analyzed the data. C.T. drew two figures (Figs. 2, 4). Y.X., L.L., W.X. and H.Z. reviewed and edited the manuscript. All authors read and approved the manuscript. G.S. and S.S. contributed equally to this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shen, G., Sun, S., Tang, C. et al. Comparison of the TightRope system versus hook plate in acute acromioclavicular joint dislocations: a retrospective analysis. Sci Rep 11, 11397 (2021). https://doi.org/10.1038/s41598-021-90989-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-90989-8
This article is cited by
-
Clinical outcomes for grades III–V acromioclavicular dislocations favor double-button fixation compared to clavicle hook plate fixation: a systematic review and meta-analysis
European Journal of Orthopaedic Surgery & Traumatology (2023)
-
Acromioclavicular joint suture button repair leads to coracoclavicular tunnel widening
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.