Abstract
The purpose of the study was to evaluate the behavior of the venous-to-arterial CO2 tension difference (ΔPCO2) over the arterial-to-venous oxygen content difference (ΔO2) ratio (ΔPCO2/ΔO2) and the difference between venous-to-arterial CO2 content calculated with the Douglas’ equation (ΔCCO2D) over ΔO2 ratio (ΔCCO2D/ΔO2) and their abilities to reflect the occurrence of anaerobic metabolism in two experimental models of tissue hypoxia: ischemic hypoxia (IH) and hypoxic hypoxia (HH). We also aimed to assess the influence of metabolic acidosis and Haldane effects on the PCO2/CO2 content relationship. In a vascularly isolated, innervated dog hindlimb perfused with a pump-membrane oxygenator system, the oxygen delivery (DO2) was lowered in a stepwise manner to decrease it beyond critical DO2 (DO2crit) by lowering either arterial PO2 (HH-model) or flow (IH-model). Twelve anesthetized and mechanically ventilated dogs were studied, 6 in each model. Limb DO2, oxygen consumption (\({\dot{\text{V}}\text{O}}_{2}\)), ΔPCO2/ΔO2, and ΔCCO2D/ΔO2 were obtained every 15 min. Beyond DO2crit, \({\dot{\text{V}}\text{O}}_{2}\) decreased, indicating dysoxia. ΔPCO2/ΔO2, and ΔCCO2D/ΔO2 increased significantly only after reaching DO2crit in both models. At DO2crit, ΔPCO2/ΔO2 was significantly higher in the HH-model than in the IH-model (1.82 ± 0.09 vs. 1.39 ± 0.06, p = 0.002). At DO2crit, ΔCCO2D/ΔO2 was not significantly different between the two groups (0.87 ± 0.05 for IH vs. 1.01 ± 0.06 for HH, p = 0.09). Below DO2crit, we observed a discrepancy between the behavior of the two indices. In both models, ΔPCO2/ΔO2 continued to increase significantly (higher in the HH-model), whereas ΔCCO2D/ΔO2 tended to decrease to become not significantly different from its baseline in the IH-model. Metabolic acidosis significantly influenced the PCO2/CO2 content relationship, but not the Haldane effect. ΔPCO2/ΔO2 was able to depict the occurrence of anaerobic metabolism in both tissue hypoxia models. However, at very low DO2 values, ΔPCO2/ΔO2 did not only reflect the ongoing anaerobic metabolism; it was confounded by the effects of metabolic acidosis on the CO2–hemoglobin dissociation curve, and then it should be interpreted with caution.
Similar content being viewed by others
Introduction
In a landmark study, Vallet et al. demonstrated the determinant role of blood flow in the tissue hypoxia-induced increased venous-to-arterial CO2 tension difference (∆PCO2)1. Their data supported the hypothesis that increases in the venous PCO2 are primarily a function of changes in regional blood flow, independently of the degree of hypoxia. Gutierrez G has confirmed this conclusion in a mathematical model of tissue-to-blood CO2 exchange during hypoxia2. In these previous publications, the behavior of ∆PCO2 over the arterial-to-venous oxygen content difference (ΔO2) ratio (ΔPCO2/ΔO2), and the difference between venous-to-arterial CO2 content (ΔCCO2) over ΔO2 ratio (ΔCCO2/ΔO2) in a model of progressive tissue hypoxia generated by reducing either flow [ischemic hypoxia (IH)] or arterial oxygen tension [hypoxic hypoxia (HH)], were not investigated1,2.
Several clinical studies3,4,5,6,7 have shown that ΔPCO2/ΔO2 ratio, taken as a surrogate of respiratory quotient (RQ), was associated with elevated lactate levels and oxygen supply dependency considered, in those studies, as indices of global anaerobic metabolism in critically ill patients with tissue hypoperfusion. However, in an experimental study, Dubin et al. found that ΔPCO2/ΔO2 ratio was a poor indicator of anaerobic metabolism in the hemodilution model of tissue hypoxia, where anemia was associated with preserved blood flow8. Similarly, other authors suggested that ΔPCO2/ΔO2 ratio might not rise during tissue hypoxia conditions when associated with normal/high blood flow because venous blood flow seemed to guarantee a sufficient clearance of CO2 generated by the anaerobic metabolism9. Thus, it is unclear if the ΔPCO2/ΔO2 ratio would be able to depict the presence of anaerobic metabolism in patients with maintained blood flow (cardiac output).
Furthermore, one estimates that the ΔPCO2/ΔO2 ratio might be affected by other factors than anaerobic metabolism by influencing the relationship between CO2 content (CCO2) and PCO2. Indeed, metabolic acidosis can change the PCO2/CCO2 relationship so that PCO2 is higher for a given CCO2. Low oxygen saturation, by promoting more CO2 binding to hemoglobin (Haldane effect), increases the CCO2 for a given PCO210. It is not completely clear to what extent these factors would impact the PCO2/CCO2 relationship and influence the ΔPCO2/ΔO2 ratio. Answering this question would help to define the applicability of this ratio in different clinical situations.
Therefore, we used, in secondary analysis, the original study published by Vallet et al.1 with the aim to assess the behavior of ΔPCO2/ΔO2 ratio, ΔCCO2/ΔO2 ratio, and their components in the regional model of progressive tissue hypoxia generated by IH or HH1. We also investigated the metabolic acidosis (pH) and Haldane effects on the PCO2/CCO2 relationship. Since the flow was maintained unchanged in the HH model, we hypothesized that ΔPCO2/ΔO2 and ΔCCO2/ΔO2 ratios might not be able to detect the occurrence of anaerobic metabolism as the sustained blood flow would be sufficient to wash out the CO2 generated by hypoxic cells in that model.
Methods
Animal preparation
The original study was approved by the University of Alabama at Birmingham Institutional Animal Care and Use Committee. The study is reported in accordance with the ARRIVE guidelines. All experiments were performed in accordance with relevant guidelines and regulations. Twelve dogs of either sex and mixed breed were used1. All animals were anesthetized with intravenous 30 mg/kg of sodium phenobarbital and mechanically ventilated with a Harvard animal respirator at 10 breaths/min. Lamps suspended above the operating table were used to maintain core temperature near 37 °C. Tidal volume was varied to maintain systemic arterial PCO2 between 30 and 35 mmHg. The ventilator setting was kept unchanged during the rest of the experiment. A 20 mg of succinylcholine chloride was given intramuscularly and a continuous infusion (0.1 mg/mL/min) was begun. Anesthesia depth was checked regularly by vigorous toe pinching, and additional anesthetic was given if systemic blood pressure and heart rate responded.
Catheters were inserted into the pulmonary artery (through the internal jugular vein) and common carotid artery for continuous measurements of vascular pressures and blood sampling. Arterial inflow (Q) and venous outflow from the left hindlimb were isolated, as previously described1,11 (Supplemental Digital Content 1, Appendix). A roller occlusive pump directed blood flow from the right hindlimb femoral artery to the femoral artery of the vascularly isolated left hindlimb. A sampling port and pressure transducer were placed in this circuit proximal to the limb. A membrane oxygenator (model 0800-2A, Sci Med) was interposed in the perfusion circuit. A gas flow mixer (model GF-3, Cameron Instruments) supplied O2, N2, and CO2 to the oxygenator, as needed, to produce normoxia or hypoxia with normocapnia in the blood supply to the hindlimb. A water bath warmed the oxygenator so that perfusion to the isolated hindlimb was at 37 °C after heat loss through the tubing.
Measurements
Blood samples from the carotid, femoral, and pulmonary arteries and femoral vein were obtained simultaneously. Blood gas tensions and pH were measured in an acid–base analyzer (ABL-30, Radiometer, Westlake, OH) at 37 °C and later corrected to esophageal temperature at the time of sampling. Oxygen saturation was measured with a co-oximeter calibrated for dog blood (IL-282, Instrumentation Lab, Lexington, MA). Arterial oxygen content was calculated as CaO2 (mL) = 1.34 × Hb (g/dL) × SaO2 + 0.0031 × PaO2 (mmHg), where SaO2 is the oxygen saturation of arterial blood, Hb the hemoglobin concentration, and PaO2 the arterial oxygen tension. Hindlimb venous oxygen content was calculated as CvO2 (mL) = 1.34 × Hb (g/dL) × SvO2 + 0.0031 × PvO2 (mmHg), where PvO2 is the hindlimb venous oxygen tension, and SvO2 is the hindlimb venous oxygen saturation. ΔO2 was calculated as CaO2 – CvO2. Hindlimb VO2 (\({\dot{\text{V}}\text{O}}_{2}\))was calculated as the product of Q (leg blood flow) and ΔO2. Hindlimb oxygen delivery (DO2) was calculated by using the formula: DO2 (mL/min) = CaO2 × Q × 10. Hindlimb oxygen extraction (OE) was defined as: OE = \({\dot{\text{V}}\text{O}}_{2} {\text{/DO}}_{2}\).
∆PCO2 was calculated as the difference between the hindlimb venous carbon dioxide tension (PvCO2) and hindlimb arterial PCO2 (PaCO2). In the original study, the hindlimb difference between venous-to-arterial CO2 content (CvCO2 − CaCO2) was calculated with the McHardy equation (as proposed by Neviere et al.12): ΔCCO2 = 11.02 × [(PvCO2)0.396 − (PaCO2)0.396] − (15 − Hb) × 0.015 × (PvCO2 − PaCO2) − (95 − SaO2) × 0.064. However, the most used equation to calculate the blood CO2 content is the Douglas equation13, which includes pH:
where plasma CCO2 = 2.226 × S × plasma \({\text{PCO}}_{2} \times (1 + 10^{{{\text{pH}}{-}{\text{pK}}^{\prime}}} )\), CCO2 is CO2 content, SO2 is oxygen saturation, S is the plasma CO2 solubility coefficient, and pK′ is the apparent pK.
S and pK′ were calculated as follow:
and
where T is the temperature expressed as °C.
The difference between venous-to-arterial CCO2 calculated with the Douglas equation was: ΔCCO2D = CvCO2D − CaCO2D.
To investigate the metabolic acidosis and Haldane effects on the PCO2/CCO2 relationship, default (Def) values of blood CCO2 were calculated with the Douglas’s equation by using only the resting values of pH and SvO2 for each dog as following: DefpH-ΔCCO2D = DefpH-CvCO2D − DefpH-CaCO2D, and DefSvO2-ΔCCO2D = DefSvO2-CvCO2D − DefSvO2-CaCO2D.
Leg blood flow, DO2, and \({\dot{\text{V}}\text{O}}_{2}\) were reported per kilogram of muscle mass.
We also calculated the hindlimb ΔPCO2/ΔO2, ΔCCO2/ΔO2, and ΔCCO2D/ΔO2 ratios.
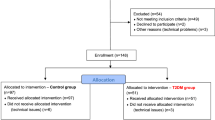
Experimental protocol
The experimental model was already described previously1. After all pressures and flows were stable for at least 30 min, the experiment began with a 30-min control period, during which measurements were obtained every 15 min. In the progressive ischemic hypoxia (IH) group, Q was then decreased every 15 min to produce Q values of ~ 60, 45, 40, 30, 20, 15, and 10 mL/kg/min. In the hypoxic hypoxia (HH) group, Q was set at 60 mL/kg/min and limb DO2 was reduced by decreasing arterial PO2 from 100 to ~ 15 mmHg (i.e., CaO2 of 17 to 2 mL O2/100 mL) in eight steps at 15-min intervals. A flow rate of 60 mL/kg/min was chosen for progressive hypoxia because it is within the range of resting blood flow to normal skeletal muscle and for the practical reason that a moderate flow was necessary to achieve the desired low PO2 values using the membrane oxygenator. Oxygen and CO2-derived variables were determined every 15 min, 13 min after the change in hindlimb arterial flow or PO2.
For each experiment, regression lines were fitted to the delivery independent and dependent portions of the delivery-uptake curve using a dual-line, least squares method14. The intercept of these two lines defined the critical DO2 (DO2crit), that is, the delivery at which \({\dot{\text{V}}\text{O}}_{2}\) began to fall with any further decline in DO2.
Statistical analysis
All data are expressed as mean ± SEM after assessed for normality using the Kolmogorov–Smirnov test.
Comparisons of data within and between groups were performed using a mixed ANOVA. Post-hoc paired and unpaired t tests were used, as appropriate, for one-time comparisons. The Bonferroni method was used to adjust for multiple comparisons.
Statistical analysis was performed using GraphPad Prism 6.0 software for windows (San Diego, California, USA). p < 0.006 and p < 0.007 were considered statistically significant for the between-group and within-group (with the baseline) comparisons, respectively. All reported p values are two-sided.
Results
Systemic hemodynamics and oxygen-derived variables remain unchanged throughout the protocol with no differences between the IH and HH models (Supplemental Digital Content 2, Table S1).
In both groups, the \({\dot{\text{V}}\text{O}}_{2}\)/DO2 graph depicts the typical biphasic relationship (Supplemental Digital Content 3, Figure S1). There was no statistically significant difference between the mean DO2Crit in the HH and IH models (6.9 ± 0.6 vs. 6.0 ± 0.5 mL/kg/min, p = 0.28, respectively). SvO2 at DO2Crit was not statistically different between the two groups (25 ± 1.7% in HH vs. 26 ± 1.5% in IH, p = 0.66). However, for the lower DO2 values, SvO2 was significantly higher in the IH model than in the HH group (Supplemental Digital Content 4, Figure S2). EO2 at DO2Crit was significantly higher in the IH group than in the HH model (74 ± 2% vs. 60 ± 4%, p = 0.01) and increased continuously and similarly in both groups (Supplemental Digital Content 5, Figure S3). ΔPCO2 risen significantly in the IH model and did not change in the HH model (Supplemental Digital Content 6, Figure S4).
Time course of venous-to-arterial CCO2 difference
ΔCCO2 calculated with the McHardy equation increased progressively along with the decrease in DO2 in the IH group but remained unchanged and even significantly decreased at the lowest DO2 value on the HH group (Fig. 1A). At DO2Crit, ΔCCO2 was significantly higher in the IH group than in the HH group (7.5 ± 0.66 vs. 4.6 ± 0.5 mL, p = 0.006, respectively), and it was significantly different from the baseline only in the IH group (p = 0.0023).
Hindlimb venous-to-arterial CO2 content difference (ΔCCO2) calculated with McHardy equation (A) and with Douglas equation (ΔCCO2D) (B) as a function of hindlimb oxygen delivery (DO2) for ischemic hypoxia model (IH) and hypoxic hypoxia model (HH). *p < 0.006 vs. HH, #p < 0.007 vs. baseline, mixed ANOVA.
ΔCCO2D calculated with the Douglas equation, in the IH group, increased with the decrease in DO2 down to DO2crit. However, beyond DO2crit, ΔCCO2D started to decrease with the further decline in DO2 to become not significantly different from its baseline value at the lowest value of DO2 (Fig. 1B). In the HH group, ΔCCO2D had the same pattern as ΔCCO2 calculated with the McHardy equation (Fig. 1A,B), which remained unchanged in parallel with the decreases in DO2 to become significantly lower than its baseline (p < 0.001) only at the end of the experiment. At DO2crit, ΔCCO2D was greater in the IH group compared to the HH group (11.0 ± 0.88 vs. 7.0 ± 0.56 mL, p = 0.003, respectively), and it was significantly higher than its baseline value (p < 0.001) only in the IH group (Fig. 1B).
pH and Haldane effects on the PCO2/CCO2 relationship
Hindlimb venous pH (pHv) remained unchanged with the decline in DO2 down to DO2crit in both groups (Fig. 2). However, beyond DO2crit, pHv decreased significantly only in the IH group and remained stable in the HH group (Fig. 2).
The venous CCO2 calculated, with the Douglas equation, by acknowledging the changes in pHv (CvCO2D) increased first with the rise in PvCO2, but then after, it stabilized despite further increases in PvCO2, due to the fall in pHv. Eventually, despite the continuously increasing PvCO2, CvCO2D decreased due to the marked decline in pHv (Fig. 3). On the contrary, there was almost a linear increase in DefpH-CvCO2D (without accounting for the changes in pHv) with the increase in PvCO2 (Fig. 4). Also, DefpH-ΔCCO2D increased linearly with the decreases in DO2 in the IH group, while it remained unchanged in the HH group (Supplemental Digital Content 7, Figure S5).
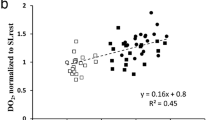
Hindlimb venous-to-arterial PCO2 difference (ΔPCO2) over the arterial-to-venous O2 difference (ΔO2) ratio (ΔPCO2/ΔO2) as a function of hindlimb oxygen delivery (DO2) for ischemic hypoxia model (IH) and hypoxic hypoxia model (HH). At DO2crit, ΔPCO2/ΔO2 was significantly higher in HH model (1.82 ± 0.09) than IH model (1.39 ± 0.06). *p < 0.006 vs. HH, #p < 0.007 vs. baseline, mixed ANOVA.
The relationship between PvCO2 and CCO2 calculated without accounting for the changes in SvO2 was the same as that if we acknowledged the variations in SvO2 (Supplemental Digital Content 8, Figure S6).
Time course of ΔPCO2/ΔO2, ΔCCO2/ΔO2, and ΔCCO2D/ΔO2 ratios
ΔO2 increased significantly in the IH and decreased in the HH in parallel with the decreases in DO2 (Supplemental Digital Content 9, Figure S7).
At DO2crit, ΔPCO2/ΔO2 ratio was significantly higher in the HH group than in the IH group (1.82 ± 0.09 mmHg/mL vs. 1.39 ± 0.06 mmHg/mL, p = 0.002, respectively). In both groups, ΔPCO2/ΔO2 ratio increased significantly only after reaching DO2crit (Fig. 4). Also, the increase in ΔPCO2/ΔO2 ratio was significantly higher in the HH than in the IH group.
ΔCCO2/ΔO2 ratio increased after DO2crit was reached in both groups, with a trend to decrease by the end of the experiment in the HH group (Supplemental Digital Content 10, Figure S8). At DO2crit, there was no significant difference between the two groups (IH: 0.59 ± 0.02 vs. HH: 0.67 ± 0.03, p = 0.05).
In both groups, ΔCCO2D/ΔO2 ratio increased significantly after reaching DO2crit. However, in the HH group, at lower values of DO2, ΔCCO2D/ΔO2 ratio started to decline but remained significantly higher than its baseline value. In the IH group, beyond DO2crit, ΔCCO2D/ΔO2 ratio begun to decrease at a higher value of DO2 than in the HH group, to become not significantly different from its baseline value at the end of the experiment (Fig. 5). At DO2crit, ΔCCO2D/ΔO2 was not significantly different between the two groups (0.87 ± 0.05 for IH vs. 1.01 ± 0.06 for HH, p = 0.09).
Hindlimb venous-to-arterial CO2 content difference calculated with Douglas equation (ΔCCO2D) over the arterial-to-venous O2 difference (ΔO2) ratio (ΔCCO2D/ΔO2) as a function of hindlimb oxygen delivery (DO2) for ischemic hypoxia model (IH) and hypoxic hypoxia model (HH). At DO2crit, there was no significantly difference between HH model (1.01 ± 0.06) and IH model (0.87 ± 0.05). *p < 0.006 vs. HH, #p < 0.007 vs. baseline, mixed ANOVA.
In both groups, DefpH-ΔCCO2D/ΔO2 (without accounting for pH changes) increased similarly and linearly in parallel with the decrease in DO2 (Supplemental Digital Content 11, Figure S9). The increase in DefpH-ΔCCO2D/ΔO2 in IH occurred before reaching DO2crit.
Discussion
The main findings of our study were that: (1) in both groups, ΔPCO2/ΔO2 as well as ΔCCO2/ΔO2, and ΔCCO2D/ΔO2 increases significantly in parallel with the decreases in DO2 only after reaching DO2crit; (2) beyond DO2crit, the time course of ΔPCO2/ΔO2 ratio was different from that of ΔCCO2D/ΔO2 or ΔCCO2/ΔO2 ratio, in both groups; (3) metabolic acidosis, but not Haldane effect influenced significantly the PCO2/CCO2 relationship explaining the discrepancy between ∆PCO2 and ΔCCO2D; (4) the method of CCO2 calculation had a considerable impact on the results and yielded different conclusions.
Anaerobic metabolism occurrence is usually due to cellular hypoxia15. Whenever oxygen delivery decreases relative to demand, and the compensatory mechanism is exhausted, extra-mitochondrial anaerobic glycolysis occurs, and lactic acidosis develops16. We aimed to investigate if ΔPCO2/ΔO2 and ΔCCO2D/ΔO2 could reflect the development of anaerobic metabolism in two regional models of tissue hypoxia: IH, where the oxygen delivery progressively decreased by decreasing the blood flow, and HH, where the blood flow was maintained unchanged, and the oxygen delivery was reduced by decreasing the arterial oxygen content.
In experimental conditions of tissue hypoxia, the drop in VO2 leads to decreased total VCO2 generation, mainly related to the decrease in aerobic CO2 production. However, under situations of hypoxia, tissue CO2 increases as hydrogen ions generated by anaerobic sources of energy (hydrolysis of high-energy phosphates) are buffering by bicarbonate existing in the cells (anaerobic CO2 production)17. Therefore, VCO2 being reduced less than VO2, the RQ (VCO2/VO2) should increase. Accordingly, the increase in RQ has been shown to be a useful marker of global tissue hypoxia18,19. Indeed, Groeneveld et al.18 observed, in an experimental model of a graded increase in positive end-expiratory pressure-induced a decrease in cardiac output and oxygen delivery in pigs, that the decline in VCO2 (by 21 ± 2%) was less than in VO2 (by 27 ± 2%).
However, airway RQ measurement necessitates a specific monitoring device (indirect calorimetry) that many hospitals might not have. Recently, there has been a growing interest in the ΔPCO2/ΔO2 ratio as a surrogate of the RQ to detect the development of global anaerobic metabolism in critically ill patients3,4,5,6,7. Indeed, several studies found an association between increased ΔPCO2/ΔO2 ratio and hyperlactatemia5 and decreased lactate clearance6,7, which were taken as markers of anaerobic metabolism activation. We4 and other authors3 have also shown that ΔPCO2/ΔO2 ratio had an excellent ability to detect the presence of VO2/DO2 dependency phenomenon, better than central venous oxygen saturation and blood lactate levels, in septic shock patients. Recently, Mesquida et al.20 reported an association between ΔPCO2/ΔO2 ratio and ICU mortality in septic shock patients. In contrast, in other studies, ΔPCO2/ΔO2 was unable to predict hyperlactatemia, poor lactate clearance, or VO2/DO2 dependency and was not associated with outcome in septic shock or cardiac surgery patients9,21,22,23. Thus, the relationship between ΔPCO2/ΔO2 and the presence of tissue hypoxia is controversial.
Indeed, the use of ΔPCO2/ΔO2 ratio as a surrogate of RQ supposes that the PCO2/CCO2 relationship is quasi-linear, which may be true over the physiological range of PCO224. However, this relationship can be influenced by the degree of metabolic acidosis25, hematocrit26, and oxygen saturation (Haldane effect)8,27, and it becomes nonlinear if these factors change28. Indeed, severe metabolic acidosis, low hematocrit, and high oxygen saturation can increase PCO2 for a given CCO2 since less CO2 is bound to hemoglobin8. Thus, ∆PCO2 and ΔPCO2/ΔO2 ratio might be increased due to several factors unrelated to the blood flow and anaerobic metabolism. We found that metabolic acidosis influenced the PCO2/CCO2 relationship significantly. Indeed, when the changes in pHv were ignored, the PCO2/CCO2 relationship was almost linear (Fig. 3). However, CCO2 was not linearly related to PCO2 when the changes in pH were acknowledged. In fact, PCO2 and CCO2 changed in opposite directions as metabolic acid was added to the blood by the hypoxic cells (Fig. 3). That is because metabolic acidosis causes plasma and red blood cell CCO2 and bicarbonates to decrease29. In our study, the Haldane effect did not influence the PCO2/CCO2 relationship as the latter was the same, taking into account or not for the changes in SvO2 (Supplemental Digital Content 8, Figure S6).
Our findings suggest that, in situations with moderate/severe metabolic acidosis, an elevated ∆PCO2 might not reflect only low or inadequate blood flow but could also be ascribed to modifications of the CO2–hemoglobin dissociation curve. Our results are in line with previous studies. Indeed, Sun et al.29 found that, in healthy subjects, during heavy exercise, changes in pH had a significant influence on the PCO2/CCO2 relationship with CCO2 not linearly related to PCO2 and even varied in opposite directions after the lactic acidosis threshold was reached. However, in that study, changes in SO2 (Haldane effect) had a minor influence on the PCO2/CCO2 relationship. Also, in septic shock patients, Mesquida et al.20 observed that pH was the only best predictor of the discrepancy found between ΔPCO2/ΔO2 and ΔCCO2D/ΔO2; venous oxygen saturation (Haldane effect) had a minimal effect.
We observed that ΔPCO2/ΔO2, and ΔCCO2D/ΔO2 significantly increased at DO2crit and not before (Figs. 4 and 5), suggesting that these variables were able to depict the occurrence of oxygen supply dependency (DO2crit) in both IH and HH groups. The increases in these variables were mainly due to the decline in ΔO2 in the HH group and the rise in ∆PCO2 and ΔCCO2 in the IH group induced by the decrease in blood flow. In contrast, in an experimental study of hemodilution model of tissue hypoxia, Dubin et al.8 found that ΔPCO2/ΔO2 significantly increased before the fall in VO2 and the sharp increase in RQ (measured by indirect calorimetry), and thus, it was a misleading indicator of anaerobic metabolism. The authors explained this finding by the effects of low hemoglobin on the CO2–hemoglobin dissociation curve8. However, it is hard to compare these results together as the two tissue hypoxia models (HH and hemodilution) are different. Indeed, the effects of anemia on the CO2–hemoglobin dissociation curve could be different from that of the low oxygen saturation (Haldane effect). Also, the magnitude of the decrease in venous oxygen saturation would be much more pronounced in the HH model, where the flow was maintained constant, than in the hemodilution model, where cardiac output increased by 126%8. Beyond DO2crit, we observed a discrepancy between the evolutions of ΔPCO2/ΔO2 and ΔCCO2D/ΔO2 in both groups (Figs. 4 and 5). That might be explained by the different behavior of ∆PCO2 and ΔCCO2D at lower DO2 values. Indeed, in the IH group, these two variables changed in opposite directions: ∆PCO2 continued to increase, whereas ΔCCO2D fell caused by metabolic acidosis (decreases in bicarbonate levels). In the HH model, ∆PCO2 remained unchanged, whereas ΔCCO2D decreased at lower DO2 values (Fig. 1B and Supplemental Digital Content 6, Figure S4). Therefore, below DO2crit, and at very low DO2 values, ΔPCO2/ΔO2 ratio is confounded by the changes in the CO2–hemoglobin curve induced by metabolic acidosis, and it does not reliably reflect the oxygen supply dependency phenomenon and the activation of anaerobic metabolism, especially in the IH tissue hypoxia model. However, in clinical practice, in such cases with very low DO2, the clinical diagnosis of tissue hypoxia would be obvious without the need for such markers.
It is worth to note that the method of calculation of the difference in CCO2 matters as the McHardy equation12, and Douglas equation13 yielded different findings (Figs. 5 and Supplemental Digital Content 10, Figure S8). However, we think that the Douglas equation is much more used in research papers, and more accurate as it accounts for much more factors such as pH.
There is no reported data, in the literature, on the behavior of ΔCCO2D/ΔO2 ratio beyond DO2crit at very low DO2 values. This ratio tended to decrease in both tissue hypoxia models, even in the presence of anaerobic CO2 production. It is possible that in case of advanced tissue hypoxia with massive decreases in VO2, the anaerobic sources of CO2 becoming much less important than the dramatically decreased aerobic ones leading to a reduction in VCO2/VO2 ratio.
We acknowledge several limitations to our study. First, our study was a secondary analysis that is subject to inherent limitations. Second, computation of CCO2 is subject to an important potential risk of measurement errors due to the number of variables included in the equation30 that might amplify during the calculation of ΔCCO2D. Nevertheless, ΔCCO2D/ΔO2 ratio was already shown to be associated with mortality in septic shock patients9, suggesting that the influence of measurement errors might be limited.
Conclusions
In both IH and HH regional models of tissue hypoxia, ΔPCO2/ΔO2 and ΔCCO2D/ΔO2 ratios both widened significantly only at the beginning of oxygen supply dependency. The hypoxic tissue hypoxia model yielded higher increases in ΔPCO2/ΔO2 than the IH model. At advanced stages of tissue hypoxia (very low DO2), ΔPCO2/ΔO2 did not only reflect the ongoing anaerobic metabolism, but it was confounded by the effects of metabolic acidosis on the CO2–hemoglobin dissociation curve, and then it should be interpreted with caution. For clinical practice, in severe metabolic acidosis situations, elevated ∆PCO2 may not reflect the degree of tissue hypoperfusion. In these cases, calculating the difference in CCO2 with the Douglas equation is advisable.
Abbreviations
- CO2 :
-
Carbon dioxide
- VO2 :
-
Oxygen consumption
- VCO2 :
-
Carbon dioxide production
- DO2 :
-
Oxygen delivery
- RQ:
-
Respiratory quotient
- ∆PCO2 :
-
Venous-to-arterial carbon dioxide tension difference
- CCO2 :
-
CO2 content
- ΔCCO2 :
-
Venous-to-arterial carbon dioxide content difference
- CCvCO2 :
-
Venous CO2 content
- CCaCO2 :
-
Arterial CO2 content
- ΔO2 :
-
Arterial-to-venous oxygen content difference
- PaCO2 :
-
Partial arterial carbon dioxide tension
- PvCO2 :
-
Partial venous carbon dioxide tension
- SvO2 :
-
Venous oxygen saturation
- SaO2 :
-
Arterial oxygen saturation
- PaO2 :
-
Partial arterial oxygen tension
- PvO2 :
-
Partial venous oxygen tension
- Hb:
-
Hemoglobin
References
Vallet, B., Teboul, J. L., Cain, S. & Curtis, S. Venoarterial CO(2) difference during regional ischemic or hypoxic hypoxia. J. Appl. Physiol. 89, 1317–1321 (2000).
Gutierrez, G. A mathematical model of tissue-blood carbon dioxide exchange during hypoxia. Am. J. Respir. Crit. Care Med. 169, 525–533 (2004).
Monnet, X. et al. Lactate and venoarterial carbon dioxide difference/arterial–venous oxygen difference ratio, but not central venous oxygen saturation, predict increase in oxygen consumption in fluid responders. Crit. Care Med. 41, 1412–1420 (2013).
Mallat, J. et al. Ratios of central venous-to-arterial carbon dioxide content or tension to arteriovenous oxygen content are better markers of global anaerobic metabolism than lactate in septic shock patients. Ann. Intensive Care 6, 10 (2016).
Mekontso-Dessap, A. et al. Combination of venoarterial PCO2 difference with arteriovenous O2 content difference to detect anaerobic metabolism in patients. Intensive Care Med. 28, 272–277 (2002).
Mesquida, J. et al. Central venous-to-arterial carbon dioxide difference combined with arterial-to-venous oxygen content difference is associated with lactate evolution in the hemodynamic resuscitation process in early septic shock. Crit. Care 19, 126 (2015).
He, H. W., Liu, D. W., Long, Y. & Wang, X. T. High central venous-to-arterial CO2 difference/arterial–central venous O2 difference ratio is associated with poor lactate clearance in septic patients after resuscitation. J. Crit. Care 31, 76–81 (2016).
Dubin, A. et al. Venoarterial PCO2-to-arteriovenous oxygen content difference ratio is a poor surrogate for anaerobic metabolism in hemodilution: An experimental study. Ann. Intensive Care 7, 65 (2017).
Ospina-Tascón, G. A. et al. Combination of arterial lactate levels and venous–arterial CO2 to arterial–venous O2 content difference ratio as markers of resuscitation in patients with septic shock. Intensive Care Med. 41, 796–805 (2015).
Teboul, J. L. & Scheeren, T. Understanding the Haldane effect. Intensive Care Med. 43, 91–93 (2016).
Cain, S. M. & Chapler, C. K. Oxygen extraction by canine hindlimb during hypoxic hypoxia. J. Appl. Physiol. 46, 1023–1028 (1979).
Neviere, R. et al. Carbon dioxide rebreathing method of cardiac output measurement during acute respiratory failure in patients with chronic obstructive pulmonary disease. Crit. Care Med. 22, 81–85 (1994).
Douglas, A. R., Jones, N. L. & Reed, J. W. Calculation of whole blood CO2 content. J. Appl. Physiol. 65, 473–477 (1988).
Samsel, R. & Schumacker, P. T. Determination of the critical O2 delivery from experimental data: Sensitivity to error. J. Appl. Physiol. 64, 2074–2082 (1988).
Cohen, P. J. The metabolic function of oxygen and biochemical lesions of hypoxia. Anesthesiology 37, 148–177 (1972).
Ronco, J. J. et al. Identification of the critical oxygen delivery for anaerobic metabolism in critically ill septic and nonseptic humans. JAMA 270, 1724–1730 (1993).
Mallat, J., Lemyze, M., Tronchon, L., Vallet, B. & Thevenin, D. Use of venous-to-arterial carbon dioxide tension difference to guide resuscitation therapy in septic shock. World J. Crit. Care Med. 5, 47–56 (2016).
Groeneveld, A. B., Vermeij, C. G. & Thijs, L. G. Arterial and mixed venous blood acid-base balance during hypoperfusion with incremental positive end- expiratory pressure in the pig. Anesth. Analg. 73, 576–582 (1991).
Cohen, I. L., Sheikh, F. M., Perkins, R. J., Feustel, P. J. & Foster, E. D. Effect of hemorrhagic shock and reperfusion on the respiratory quotient in swine. Crit. Care Med. 23, 545–552 (1995).
Mesquida, J. et al. Respiratory quotient estimations as additional prognostic tools in early septic shock. J. Clin. Monit. Comput. 32, 1065–1072 (2018).
Muller, G. et al. Prognostic significance of central venous-to-arterial carbon dioxide difference during the first 24 hours of septic shock in patients with and without impaired cardiac function. Br. J. Anaesth. 119, 239–248 (2017).
Abou-Arab, O. et al. The ratios of central venous to arterial carbon dioxide content and tension to arteriovenous oxygen content are not associated with overall anaerobic metabolism in postoperative cardiac surgery patients. PLoS ONE 13, e0205950 (2018).
Fischer, M. O. et al. Assessment of macro- and micro-oxygenation parameters during fractional fluid infusion: A pilot study. J. Crit. Care 40, 91–98 (2017).
Cavaliere, F. et al. Comparison of two methods to assess blood CO2 equilibration curve in mechanically ventilated patients. Respir. Physiol. Neurobiol. 146, 77–83 (2005).
Jakob, S. M., Groeneveld, A. B. & Teboul, J. L. Venous–arterial CO2 to arterial–venous O2 difference ratio as a resuscitation target in shock states?. Intensive Care Med. 41, 91–93 (2015).
Chiarla, C. et al. Significance of hemoglobin concentration in determining blood CO2 binding capacity in critical illness. Respir. Physiol. Neurobiol. 172, 32–36 (2010).
Jakob, S. M., Kosonen, P., Ruokonen, E., Parviainen, I. & Takala, J. The Haldane effect—An alternative explanation for increasing gastric mucosal PCO2 gradients?. Br. J. Anaesth. 83, 740–746 (1999).
Mchardy, G. J. The relationship between the differences in pressure and content of carbon dioxide in arterial and venous blood. Clin. Sci. 32, 299–309 (1967).
Sun, X. G., Hansen, J. E., Stringer, W. W., Ting, H. & Wasserman, K. Carbon dioxide pressure-concentration relationship in arterial and mixed venous blood during exercise. J. Appl. Physiol. 90, 1798–1810 (2001).
Mallat, J. et al. Repeatability of blood gas parameters, PCO2 gap, and PCO2 gap to arterial-to-venous oxygen content difference in critically ill adult patients. Medicine (Baltimore) 94, e415 (2015).
Author information
Authors and Affiliations
Contributions
J.M., and B.V. designed the study. J.M. conducted statistical analyses. J.M. and B.V. participated in manuscript writing and reviewing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mallat, J., Vallet, B. Ratio of venous-to-arterial PCO2 to arteriovenous oxygen content difference during regional ischemic or hypoxic hypoxia. Sci Rep 11, 10172 (2021). https://doi.org/10.1038/s41598-021-89703-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-89703-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.