Abstract
We investigated association between epidemiological and clinical characteristics of coronavirus disease 2019 (COVID-19) patients and clinical outcomes in Korea. This nationwide retrospective cohort study included 5621 discharged patients with COVID-19, extracted from the Korea Disease Control and Prevention Agency (KDCA) database. We compared clinical data between survivors (n = 5387) and non-survivors (n = 234). We used logistic regression analysis and Cox proportional hazards model to explore risk factors of death and fatal adverse outcomes. Increased odds ratio (OR) of mortality occurred with age (≥ 60 years) [OR 11.685, 95% confidence interval (CI) 4.655–34.150, p < 0.001], isolation period, dyspnoea, altered mentality, diabetes, malignancy, dementia, and intensive care unit (ICU) admission. The multivariable regression equation including all potential variables predicted mortality (AUC = 0.979, 95% CI 0.964–0.993). Cox proportional hazards model showed increasing hazard ratio (HR) of mortality with dementia (HR 6.376, 95% CI 3.736–10.802, p < 0.001), ICU admission (HR 4.233, 95% CI 2.661–6.734, p < 0.001), age ≥ 60 years (HR 3.530, 95% CI 1.664–7.485, p = 0.001), malignancy (HR 3.054, 95% CI 1.494–6.245, p = 0.002), and dyspnoea (HR 1.823, 95% CI 1.125–2.954, p = 0.015). Presence of dementia, ICU admission, age ≥ 60 years, malignancy, and dyspnoea could help clinicians identify COVID-19 patients with poor prognosis.
Similar content being viewed by others
Introduction
Since the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China, COVID-19 has become a major global health problem. Clusters of COVID-19 pneumonia cases led to the eventual identification of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020. As of December 29, 2020, there were 81,278,104 confirmed cases from 220 countries, with 1,774,388 deaths, and an overall projected case fatality rate of 2.2%1.
The COVID-19 pandemic has led to shortages of medical resources, including hospital beds, ventilators, and personal protective equipment in several countries2,3,4. Therefore, accurate diagnosis and outcome prediction are essential to decrease the burden on national healthcare systems and provide optimal care for COVID-19 patients.
During the early period of the outbreak, some case series from China reported the epidemiological and clinical characteristics of COVID-195,6,7. Since then, some cohort studies have described potential predictors of mortality and poor clinical outcomes among patients with COVID-198,9,10. Recently, some large cohort studies including nationwide data (United Kingdoms, Germany and France, respectively) reported the clinical characteristics and factors associated with outcomes among COVID-19 patients11,12,13. Although this nationwide COVID-19 evidence has emerged, there are still controversies about risk factors of mortality and poor clinical outcomes among COVID-19 patients.
By using the data collected by the Korea Disease Control and Prevention Agency (KDCA), we presented details of all patients with laboratory-confirmed COVID-19 and a definite clinical outcome (survival discharge or death) as of April 30, 2020. We aimed to explore the risk factors of mortality and fatal adverse outcomes among COVID-19 patients in Korea.
Results
Demographic and clinical characteristics
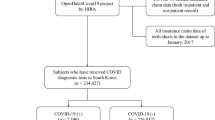
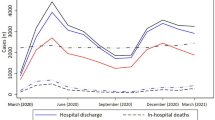
A total of 5628 patients with confirmed COVID-19 were recorded in the KDCA registry during the study period. After excluding 7 patients who underwent laboratory tests for COVID-19 but died before the final confirmation of SARS-CoV-2 [using real-time reverse transcription polymerase chain reaction (RT-PCR) methods], we included 5621 patients in the final analysis (Fig. 1). Of the 5621 patients, 5387 were discharged while 234 died in the hospital (Table 1 and Fig. 1). The most common age group was 50–59 years, followed by 20–29 and 60–69 years. Of the 5621 patients, 2317 (41.2%) were men. Comorbidities were present in nearly half of the patients, including hypertension (21.3%), diabetes (12.3%), dementia (4.0%), chronic cardiac disease (3.2%), and malignancy (2.5%). The most common symptoms at presentation were cough and sputum, followed by fever and headache. Overall, the median isolation period was 24 days [interquartile range (IQR) 18–32]. The median survival (isolation) period among non-survivors was 11 days (IQR 6–21) after confirmation of COVID-19. Comparisons of clinical and epidemiological characteristics between survivors and non-survivors are shown in Table 1. Supplementary Table 1 presents the levels of complications that occurred during the isolation period among all patients. Patients who had no limitation of activity were 4482 (79.7%) while those requiring oxygen supply was 809 (14.4%).
Kaplan–Meier survival curves according to age and sex
Mortality was significantly higher in elderly patients (age ≥ 65 years) than in younger patients (age < 65 years) (log-rank test, p < 0.001) (Fig. 2a) and in male patients than in female patients (log-rank test, p < 0.001) (Fig. 2b).
Factors associated with mortality and fatal adverse outcomes
Logistic regression analysis
In univariable logistic regression analysis, the odds of mortality were higher in patients aged ≥ 60 years, and those with altered mentality, dementia, heart failure, and chronic kidney disease (Table 2). Sex, isolation period, obesity, heart rate, body temperature, fever, dyspnoea, diabetes, hypertension, chronic cardiac disease, asthma, chronic obstructive pulmonary disease, malignancy, and leucocytosis, were also associated with mortality (Table 2). Multivariable logistic regression analysis results showed increasing odds of mortality with age ≥ 60 years, short isolation period, dyspnoea, altered mentality, diabetes, malignancy, dementia, intensive care unit (ICU) admission, and lower levels of lymphocyte, haemoglobin, or platelet (Table 2). The multiple regression equation including all the potential variables effectively predicted mortality in COVID-19 patients [area under the curve (AUC) = 0.979, 95% confidence interval (CI) 0.964–0.993].
Univariate analysis showed that the odds of fatal adverse outcomes were higher in patients aged ≥ 60 years, and those with altered mentality, dementia, heart failure, and chronic kidney disease (Table 3). Sex, isolation period, obesity, heart rate, body temperature, fever, dyspnoea, diabetes, hypertension, chronic cardiac disease, asthma, chronic obstructive pulmonary disease, malignancy, and leucocytosis, were also associated with fatal adverse outcomes (Table 3). Multivariable logistic regression analysis showed increasing odds of fatal adverse outcomes associated with age ≥ 60 years, short isolation period, dyspnoea, altered mentality, diabetes, hypertension, malignancy, dementia, ICU admission, and lower levels of lymphocytes, haemoglobin, or platelets (Table 3).
Cox proportional hazards model
The multivariable Cox proportional hazards model showed increasing hazards of mortality with dementia, ICU admission, age ≥ 60 years, malignancy, and dyspnoea (Table 4). The hazard ratio plot for mortality using the multivariable Cox proportional hazards model is presented in Fig. 3a. Body mass index (BMI) 18.5–22.9 or 23.0–24.9, headache, and higher levels of lymphocytes or platelets were associated with decreasing mortality hazards. The multivariable Cox proportional hazards model showed that increasing hazards of fatal adverse outcomes were associated with dementia, ICU admission, age ≥ 60 years, malignancy, and dyspnoea (Table 5). The hazard ratio plot for fatal adverse outcomes using the multivariable Cox proportional hazards model is presented in Fig. 3b. BMI, 18.5–22.9 or 23.0–24.9, and higher levels of lymphocytes or platelets were associated with decreasing hazards of fatal adverse outcomes.
Discussion
To our knowledge, this is one of the largest nationwide cohort studies in COVID-19 patients with definite clinical outcomes. This nationwide retrospective cohort study identified the risk factors of mortality and fatal adverse outcomes among patients with laboratory-confirmed COVID-19 in Korea. In particular, dementia, ICU admission, age ≥ 60 years, malignancy, and dyspnoea, were associated with higher odds of mortality. In addition, BMI 18.5–22.9 or 23.0–24.9, and higher levels of lymphocytes or platelets, were associated with lower odds of poor clinical outcomes.
The present study showed that older age (≥ 60 years) was associated with mortality and fatal adverse outcomes in patients with COVID-19. Although individuals > 65 years comprise 17% of the total population in the United States, they account for 31% of COVID-19 patients, 45% of hospitalized patients, 53% of those on intensive care unit admission, and 80% of those that died due to COVID-1914. This suggests that older individuals are susceptible to developing COVID-19 and have poor clinical outcomes compared with the general population. Our results showed that individuals ≥ 60 accounted for 32% of COVID-19 and 92% of deaths due to COVID-19. In accordance with our study, recent studies reported that older age is significantly associated with mortality among COVID-19 patients9,10.
Previous studies reported that male sex is significantly associated with mortality9,15. Our data showed that although mortality was significantly higher in male patients than in female patients in the Kaplan–Meier survival curve analysis, male sex was not a significant risk factor for mortality in the Cox proportional hazards model. We recommend a larger worldwide cohort study to explore this discrepancy between our results and those of previous studies.
The risk of serious disease and mortality in COVID-19 increases with the presence of comorbidities16,17,18,19,20. Our data showed malignancy as an independent risk factor for mortality in the multivariable Cox proportional hazards model with a hazard ratio (HR) of 3.054. According to a recent study from China, cancer patients with COVID-19 had 3.5 times higher risk of requiring ICU admission or mechanical ventilation, compared to the general population21. Cancer patients are generally immunocompromised and are at higher risk of COVID-19-related fatal events in comparison to the cancer-free population21,22.
Our study also showed that dementia was associated with mortality and fatal adverse outcomes. Some reasons can be proposed to explain our results. First, most of the patients suffering dementia are old and have other comorbidities that could result in poor clinical outcomes23. Second, people with dementia would require the support of dementia caregivers in order to keep preventive and healthcare measures. However, this COVID-19 pandemic has made the availability of caregivers limited24. Third, persistent inflammatory state of dementia patients may increase peripheral blood white blood cells and neutrophil counts, which was associated with higher mortality from COVID-1925. Fourth, the ApoE e4 genotype, which were associated with patients with dementia26, can increase the risk of having acute respiratory distress syndrome in COVID-19 patients. Similar to our data, a previous study reported that mortality due to COVID-19 was significantly higher in elderly patients with dementia27. Another study reported an in-hospital mortality of 61% among hospitalized patients with dementia and COVID-1928. In our study, mortality during the isolation period was 33.5% among patients with COVID-19. Two large cohort studies from the United Kingdom showed that pre-existing dementia was a significant predictor of COVID-19 mortality11,20. Furthermore, a recent study, including global big data on dementia and COVID-19 in 185 countries revealed a significant correlation between dementia burden and COVID-19-related death29.
In the present study, although diabetes mellitus (DM) was not a predictor of mortality in the Cox proportional hazards model, it was associated with mortality and fatal adverse outcomes in multivariable logistic regression analysis. Some case series reported that patients with pre-existing DM are vulnerable to infection and are at a higher risk of death from COVID-195,15,30,31,32. According to a recent meta-analysis, diabetes in patients with COVID-19 is associated with a two-fold increase in mortality as well as severity of COVID-19, as compared to those in non-diabetics33. Similar to the prior meta-analysis, our results showed that DM was associated with increased odds of mortality of 2.728 and fatal adverse outcomes of 1.838 in multivariable logistic regression analysis.
Our study demonstrated that dyspnoea and ICU admission were associated with mortality and fatal adverse outcomes in both the multivariable logistic regression analysis and Cox proportional hazards model. Data from urban communities in the United States revealed that patients admitted to the ICU had a higher incidence of respiratory failure requiring invasive mechanical ventilation and mortality compared with patients in the general ward9. Another study showed that dyspnoea at presentation was associated with hospitalization and the need for ICU management9. According to a recent meta-analysis, dyspnoea was the only symptom predictive of severe COVID-19 and ICU admission19. Similar to the previous meta-analysis, our study showed that dyspnoea was the only symptom predictive of fatal adverse outcomes.
A recent study using a systemic review and meta-analysis showed that hematologic and inflammatory markers such as procalcitonin, C-reactive protein, D-dimer, and lactate dehydrogenase and decreased albumin could help predict severe outcomes in COVID-1934. Our study showed that lower levels of lymphocytes or platelets were associated with increasing hazards of mortality and fatal adverse outcomes. COVID-19 patients with low levels of lymphocyte and platelets should be monitored closely to minimize the risk of progression to severe disease.
The present study has some limitations. First, due to the retrospective nature of the study design and data extraction procedure, some laboratory data were missing or unavailable. Therefore, their influence might have been underestimated in predicting mortality and fatal adverse outcomes. Second, our data did not include information regarding radiologic findings, which might reveal prognostic factors35. Third, although treatment strategy can have a significant impact on clinical outcome36,37,38, we assumed that enrolled patients all had adequate and timely management. Fourth, although our study included over 5600 patients with COVID-19 from Korea, there was a lack of time-series analysis for potential variables. Fifth, by excluding patients still under isolation as of April 30, 2020, the case fatality ratio in our data could not reflect the true mortality of COVID-19. Sixth, our study did not include data regarding the status of therapy for each comorbidity. For instance, metformin use was associated with reduced mortality39, but statin use was not40.
Conclusions
This nationwide cohort study showed that dementia, ICU admission, age ≥ 60 years, malignancy, and dyspnoea were strong predictors of death and fatal adverse outcomes in COVID-19 patients. The multiple regression equation including clinical and epidemiological variables predicted mortality in such patients. These findings can help clinicians to identify COVID-19 patients with poor prognosis.
Methods
Study design and population
This retrospective cohort study included a nationwide cohort data of COVID-19 patients collected by KDCA, Korea. All patients who were diagnosed with COVID-19 were screened, and those who died or were discharged between January 20, 2020 (i.e., when the first patients were diagnosed in Korea), and April 30, 2020, were included in the present study. Since KDCA is a governmental institution responsible for surveillance and control of COVID-19 in Korea, our study enrolled all the patients who were diagnosed with COVID-19 and had a definite clinical outcome (discharged or dead) at the early stage of the outbreak.
This study was conducted according to the principles of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of the Korea University Ansan Hospital (IRB number 2020AS0245). The requirement for informed consent was waived by the IRB because of the retrospective nature of the study.
Data source
Clinical, epidemiological, demographic, laboratory, and outcome data were collected by KDCA since the diagnosis of the first patients with COVID-19 on January 20, 2020. All data were checked by the physicians and the KDCA preventive medicine experts. We obtained permission to access the encoded KDCA server for three weeks to extract and analyse the data during the limited period. These data cannot be shared publicly according to the KDCA directive, which prohibits researchers from such. KCDA provided anonymised clinical data for the public interest.
Laboratory results
For the laboratory confirmation of SARS-CoV-2, real-time RT-PCR was performed using throat-swab specimens. The criteria for discharge were two negative throat-swab samples for SARS-CoV-2 RNA, absence of fever for at least 3 days, definite improvement of pneumonia on chest computed tomography, and stable vital signs. Routine blood examination included a complete blood count.
Definitions
We defined fever as an axillary temperature of at least 37.5 °C. Fatal adverse outcomes were defined as at least one of invasive mechanical ventilation, multi-organ failure (MOF), ECMO, or death during the isolation period. In the present study, MOF refers to altered function in two or more organ systems after the diagnosis of COVID-19.
Statistical analysis
Statistical analyses were performed using R 4.0.2 (the R Foundation for Statistical Computing, Vienna, Austria). For all analyses, a 2-tailed test with a p value < 0.05 was considered statistically significant. Continuous variables were presented as median (IQR) or mean [standard deviation (SD)], and categorical variables were presented as frequencies (percentages). We used the t test, Mann–Whitney U test, χ2 test, or Fisher’s exact test to compare differences between survivors and non-survivors, as appropriate. The risk factors for death and fatal adverse outcomes in patients were determined using univariable and multivariable logistic regression models and presented as odds ratios (ORs) and 95% CIs. We excluded variables from the univariable logistic regression analysis if their between-group differences (the t test, Mann–Whitney U test, χ2 test, or Fisher’s exact test) were not significant. We considered variables with p ≤ 0.05 in the univariate analysis as candidate variables for the multivariable analysis. Kaplan–Meier curves and log-rank tests for age and sex were also performed for survival analyses. To explore whether potential variables were independently associated with shortened survival, we used univariable and multivariable Cox proportional-hazards models to calculate the HR and 95% CI for each variable.
Data availability
The data that support the findings of this study are available from KDCA but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of KDCA. Data cannot be shared publicly according to the KDCA directive, which prohibits researchers from such. KCDA provided anonymised clinical data for the public interest.
References
Coronavirus Resource Center. Coronavirus COVID‐19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University, https://coronavirus.jhu.edu/map.html (2020).
Ranney, M. L., Griffeth, V. & Jha, A. K. Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. N. Engl. J. Med. 382, e41. https://doi.org/10.1056/NEJMp2006141 (2020).
Zhou, W. et al. Impact of hospital bed shortages on the containment of COVID-19 in Wuhan. Int. J. Environ. Res. Public Health 17, 8560. https://doi.org/10.3390/ijerph17228560 (2020).
Gondi, S. et al. Personal protective equipment needs in the USA during the COVID-19 pandemic. Lancet 395, e90–e91. https://doi.org/10.1016/s0140-6736(20)31038-2 (2020).
Guan, W. J. et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382, 1708–1720. https://doi.org/10.1056/NEJMoa2002032 (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506. https://doi.org/10.1016/s0140-6736(20)30183-5 (2020).
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395, 507–513. https://doi.org/10.1016/s0140-6736(20)30211-7 (2020).
Liu, J. et al. Clinical outcomes of COVID-19 in Wuhan, China: a large cohort study. Ann. Intensive Care 10, 99. https://doi.org/10.1186/s13613-020-00706-3 (2020).
Suleyman, G. et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit. JAMA Netw. Open 3, e2012270. https://doi.org/10.1001/jamanetworkopen.2020.12270 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395, 1054–1062. https://doi.org/10.1016/s0140-6736(20)30566-3 (2020).
Docherty, A. B. et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 369, m1985. https://doi.org/10.1136/bmj.m1985 (2020).
Nachtigall, I. et al. Clinical course and factors associated with outcomes among 1904 patients hospitalized with COVID-19 in Germany: an observational study. Clin. Microbiol. Infect. 26(12), 1663–1669. https://doi.org/10.1016/j.cmi.2020.08.011 (2020).
Piroth, L. et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir. Med. 17, 251–259. https://doi.org/10.1016/S2213-2600(20)30527-0 (2020).
Shahid, Z. et al. COVID-19 and older adults: what we know. J. Am. Geriatr. Soc. 68, 926–929. https://doi.org/10.1111/jgs.16472 (2020).
An, C. et al. Machine learning prediction for mortality of patients diagnosed with COVID-19: a nationwide Korean cohort study. Sci. Rep. 10, 18716. https://doi.org/10.1038/s41598-020-75767-2 (2020).
Gosain, R. et al. COVID-19 and cancer: a comprehensive review. Curr. Oncol. Rep. 22, 53. https://doi.org/10.1007/s11912-020-00934-7 (2020).
Ejaz, H. et al. COVID-19 and comorbidities: deleterious impact on infected patients. J. Infect. Public Health 13, 1833–1839. https://doi.org/10.1016/j.jiph.2020.07.014 (2020).
Callender, L. A. et al. The impact of pre-existing comorbidities and therapeutic interventions on COVID-19. Front. Immunol. 11, 1991. https://doi.org/10.3389/fimmu.2020.01991 (2020).
Jain, V. & Yuan, J. M. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int. J. Public Health 65, 533–546. https://doi.org/10.1007/s00038-020-01390-7 (2020).
Atkins, J. L. et al. Preexisting comorbidities predicting COVID-19 and mortality in the UK Biobank Community Cohort. J. Gerontol. A Biol. Sci. Med. Sci. 75, 2224–2230. https://doi.org/10.1093/gerona/glaa183 (2020).
Liang, W. et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 21, 335–337. https://doi.org/10.1016/s1470-2045(20)30096-6 (2020).
Ueda, M. et al. Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J. Natl. Compr. Cancer Netw. 18, 1–4. https://doi.org/10.6004/jnccn.2020.7560 (2020).
Bonanad, C. et al. The effect of age on mortality in patients with COVID-19: a meta-analysis with 611,583 subjects. J. Am. Med. Dir. Assoc. 21(7), 915–918. https://doi.org/10.1016/j.jamda.2020.05.045 (2020).
Dang, S. et al. Caring for caregivers during COVID-19. J. Am. Geriatr. Soc. https://doi.org/10.1111/jgs.16726 (2020).
Elshazli, R. M. et al. Diagnostic and prognostic value of hematological and immunological markers in COVID-19 infection: a meta-analysis of 6320 patients. PLoS ONE 15(8), e0238160. https://doi.org/10.1371/journal.pone.0238160 (2020).
Kuo, C., Pilling, L. C., Atkins, J. L., Kuchel, G. A. & Melzer, D. ApoE e2 and aging-related outcomes in 379,000 UK Biobank participants. Aging 12, 12222–12233. https://doi.org/10.18632/aging.103405 (2020).
McMichael, T. M. et al. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N. Engl. J. Med. 382, 2005–2011. https://doi.org/10.1056/NEJMoa2005412 (2020).
Yao, J. S., Dee, E. C., Milazzo, C., Jurado, J. & Paguio, J. A. Covid-19 in dementia: an insidious pandemic. Age Ageing 49, 713–715. https://doi.org/10.1093/ageing/afaa136 (2020).
Azarpazhooh, M. R. et al. Correlations between COVID-19 and burden of dementia: an ecological study and review of literature. J. Neurol. Sci. 416, 117013. https://doi.org/10.1016/j.jns.2020.117013 (2020).
Onder, G., Rezza, G. & Brusaferro, S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 323, 1775–1776. https://doi.org/10.1001/jama.2020.4683 (2020).
Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 8, 475–481. https://doi.org/10.1016/s2213-2600(20)30079-5 (2020).
Centers for Disease Control Prevention. National Diabetes Statistics Report, 2020: Estimates of Diabetes and Its Burden in the United States, https://www.cdc.gov/diabetes/data/statistics-report/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdiabetes%2Fdata%2Fstatistics%2Fstatistics-report.html (2020).
Kumar, A. et al. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab. Syndr. 14, 535–545. https://doi.org/10.1016/j.dsx.2020.04.044 (2020).
Hariyanto, T. I. et al. Inflammatory and hematologic markers as predictors of severe outcomes in COVID-19 infection: a systematic review and meta-analysis. Am. J. Emerg. Med. 41, 110–119. https://doi.org/10.1016/j.ajem.2020.12.076 (2021).
Yuan, M., Yin, W., Tao, Z., Tan, W. & Hu, Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS ONE 15, e0230548. https://doi.org/10.1371/journal.pone.0230548 (2020).
Ahn, D. G. et al. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19). J. Microbiol. Biotechnol. 30, 313–324. https://doi.org/10.4014/jmb.2003.03011 (2020).
Chen, P. L., Lee, N. Y., Cia, C. T., Ko, W. C. & Hsueh, P. R. A review of treatment of coronavirus disease 2019 (COVID-19): therapeutic repurposing and unmet clinical needs. Front. Pharmacol. 11, 584956. https://doi.org/10.3389/fphar.2020.584956 (2020).
Chakraborty, C., Sharma, A. R., Sharma, G., Bhattacharya, M. & Lee, S. S. SARS-CoV-2 causing pneumonia-associated respiratory disorder (COVID-19): diagnostic and proposed therapeutic options. Eur. Rev. Med. Pharmacol. Sci. 24, 4016–4026. https://doi.org/10.26355/eurrev_202004_20871 (2020).
Hariyanto, T. I. & Kurniawan, A. Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection. Obesity Med. 19, 100290. https://doi.org/10.1016/j.obmed.2020.100290 (2020).
Hariyanto, T. I. & Kurniawan, A. Statin and outcomes of coronavirus disease 2019 (COVID-19): a systematic review, meta-analysis, and meta-regression. Nutr. Metab. Cardiovasc. Dis. https://doi.org/10.1016/j.numecd.2021.02.020 (2021).
Acknowledgements
The Korea Disease Control and Prevention Agency (KDCA) kindly provided data for the current study. The authors would like to thank KDCA for their cooperation. This study was supported by Korea University Medicine, funded by COVID-19 research (Grant No. O2001201). This research was also funded by the National Research Foundation of Korea (NRF) through a grant from the Korean government (MSIT) (Grant No. 2020R1C1C1010362). The funding bodies had no role in the study design, conduct, review, or report or in the decision to submit the article for publication. In addition, we would like to thank Editage (www.editage.co.kr) for English language editing.
Author information
Authors and Affiliations
Contributions
J.S. and D.W.P. conceived and designed the study. J.S., H.S., J.Y.K., and J.P. processed and analysed the data. J.C., J.S., and H.J. performed the statistical analysis. J.S. and H.J. wrote the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Song, J., Park, D.W., Cha, Jh. et al. Clinical course and risk factors of fatal adverse outcomes in COVID-19 patients in Korea: a nationwide retrospective cohort study. Sci Rep 11, 10066 (2021). https://doi.org/10.1038/s41598-021-89548-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-89548-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.