Abstract
High pulse pressure (PP) is a valid indicator of arterial stiffness. Many studies have reported that vitamin D concentration is inversely associated with vascular stiffening. This association may differ depending on sex and body mass index (BMI). This study investigated the associations between vitamin D and PP and evaluated whether these associations differ according to sex and BMI, using data for individuals aged ≥ 50 years from the National Health and Nutrition Examination Survey (NHANES) 2007–2010. Serum 25-hydroxyvitamin D (25(OH)D) concentrations were used as biomarkers of vitamin D levels. High PP was defined as ≥ 60 mmHg. Total 25(OH)D concentrations were dose-dependently associated with lower odds ratios (ORs) for high PP (p-trend = 0.01), after controlling for sociodemographic, behavioral, and dietary factors. When stratified by sex, there was a dose-dependent association between total 25(OH)D concentrations and lower risk of high PP (p-trend < 0.001) in females, but not in males. When stratified by BMI, there was a dose-dependent association between total 25(OH)D concentrations and lower risk of high PP (p-trend < 0.001) in non-overweight subjects, but not in overweight subjects. Improving the vitamin D status could delay elevation of PP and vascular stiffening in female and non-overweight subjects.
Similar content being viewed by others
Introduction
Hypertension is an important public health issue that is highly prevalent in the elderly population. According to the 2015–2016 National Center for Health Statistics (NCHS) data, the prevalence of hypertension was 29.0% among adults, and it increased with age (63.1% in adults aged 60 years and older)1. In the elderly population, hypertension is characterized by an elevated systolic blood pressure (SBP) with a normal or low diastolic blood pressure (DBP) caused by age-associated stiffening of the large arteries. Thus, pulse pressure (PP)2, defined as the difference between SBP and DBP, is a valid indicator of arterial stiffness in older adults3. Because increased arterial stiffness is known to be associated with an increased risk of cardiovascular disease as well as overall mortality4,5, PP management is very important in the elderly population to prevent cardiovascular diseases such as stroke, heart attack, and heart failure6,7.
Several studies have reported that vitamin D improves endothelial function8, and vitamin D levels are inversely associated with vascular stiffening9,10. It is possible that vitamin D improves general arterial health and increases arterial elasticity, resulting in improved arterial compliance and decreased PP11. Although there is abundant plausible biological evidence to support that vitamin D plays a role in hypertension and vascular health, previous epidemiological and intervention studies have presented inconsistent results12,13.
Therefore, the primary goal of the present study was to investigate the association between vitamin D and PP in middle-aged and older adults using data from the National Health and Nutrition Examination Survey (NHANES) 2007–2010. The secondary goal of the study was to evaluate if sex and body mass index (BMI) influence the association between vitamin D and PP.
Results
Descriptive statistics
A total of 4565 subjects (2316 males and 2249 females) were included in the analysis. Table 1 shows the general characteristics of the subjects according to sex. In males, the mean ± standard error (± SE) age was 62.4 (± 0.2) years, and 55.4% of this group had hypertension. The geometric mean (95% CIs) of the total 25-hydroxyvitamin D (25(OH)D), 25(OH)D3, and 25(OH)D2 concentrations in males were 64.4 nmol/L (95% CIs 62.4, 66.4), 59.7 nmol/L (95% CIs 57.9, 61.6), and 2.22 nmol/L (95% CIs 2.09, 2.36), respectively. In females, the mean (± SE) age was 63.5 (± 0.3), and 58.4% of this group had hypertension. The geometric mean (95% CIs) of total 25(OH)D, 25(OH)D3 and 25(OH)D2 concentrations in women were 66.7 nmol/L (95% CIs 64.4, 69.1), 60.1 nmol/L (95% CIs 58.0, 62.2), and 2.49 nmol/L (95% CIs 2.29, 2.71), respectively. The males were significantly younger and had significantly lower total 25(OH)D, 25(OH)D2, and PP values and higher DBP, height, weight, physical activity, total energy intake, potassium, calcium, magnesium, and sodium intake values than females. In addition, alcohol consumption, smoking status, and education levels were significantly different depending on sex.
Vitamin D and blood pressure in all subjects
Table 2 presents the results of multiple linear regression analyses for the associations of vitamin D with blood pressure. In all sequential models, higher total 25(OH)D and 25(OH)D3 concentrations were dose-dependently associated with lower mean SBP and PP (p-trend < 0.05). In the fully adjusted model (model B), subjects with sufficient total 25(OH)D (≥ 75 nmol/L) had a significant 2.95 (95% CIs 1.39, 4.50) mmHg lower SBP and 2.52 (95% CIs 1.10, 3.95) mmHg lower PP than did those with deficient total 25(OH)D (< 50 nmol/L). The results for the associations between 25(OH)D3 concentrations and blood pressure were similar to the associations between total 25(OH)D concentrations and blood pressure.
Vitamin D and high PP in all subjects
Table 3 presents the results of multiple logistic regression analyses of the associations of vitamin D with high PP. In all sequential models, higher total 25(OH)D and 25(OH)D3 concentrations were dose-dependently associated with lower odd ratios (ORs) for high PP (p-trend < 0.05). In the fully adjusted models (model B), the ORs for high PP were 0.76 (95% CIs 0.61, 0.95) in the higher total 25(OH)D concentrations (≥ 75 nmol/L) group compared to the group with lower total 25(OH)D concentrations (< 50 nmol/L). The results for the associations between 25(OH)D3 concentrations and high PP were similar to the associations between total 25(OH)D concentrations and high PP. These associations were similar after adjusting for additional dietary factors such as the intakes of total fat, saturated fat, and cholesterol (data not shown).
Total 25(OH)D concentration and blood pressure stratified by sex and BMI
Figure 1 shows the results of multiple linear regression analyses for the association of total 25(OH)D levels with blood pressure stratified by sex and BMI in the fully adjusted models.
Multiple linear regression of blood pressure with vitamin D concentrations in the subgroups by sex and BMI. p-trend < 0.05 considered significant. Adjusted for age, sex, race/ethnicity, education, season of examination, physical activity, alcohol consumption, smoking status, dietary covariates (intakes of total energy, potassium, calcium, magnesium, and sodium), height, weight, and diabetes.
When stratified by sex, the SBP decreased significantly in a dose-dependent manner with an increase in the total 25(OH)D concentration in males (p-trend = 0.02), and the SBP and PP decreased significantly in a dose-dependent manner with an increase in the total 25(OH)D concentration in females (p-trend = 0.003 and 0.001). The males with sufficient total 25(OH)D concentrations had a significant 2.39 mmHg (95% CIs 0.05, 4.74) lower SBP than those with deficient total 25(OH)D concentrations, while the females with sufficient total 25(OH)D concentrations had a significant 3.19 mmHg (95% CIs 0.79, 5.59) lower SBP and 3.26 mmHg (95% CIs 1.13, 5.38) lower PP than those with deficient total 25(OH)D concentrations.
When stratified by BMI, significant dose-dependent decreases in SBP and PP (p-trend = 0.002 and 0.005) with total 25(OH)D concentrations were observed in non-overweight subjects, and significant dose-dependent decreases in SBP and PP (p-trend = 0.006 and 0.003) with total 25(OH)D concentrations were observed in overweight subjects. Non-overweight subjects with sufficient total 25(OH)D concentrations had a significant 6.16 mmHg (95% CIs 2.22, 10.1) lower SBP and 4.22 mmHg (95% CIs 1.33, 7.12) lower PP than those with deficient total 25(OH)D concentrations. Overweight subjects with sufficient total 25(OH)D concentrations had a significant 2.01mmHg (95% CIs 0.41, 3.60) lower SBP and 2.04 mmHg (95% CIs 0.64, 3.44) lower PP than those with deficient total 25(OH)D concentrations.
Total 25(OH)D concentration and high PP stratified by sex and BMI
Figure 2 shows the results of the multiple logistic regression analyses for the associations of total 25(OH)D concentration with high PP stratified by sex and BMI in the fully adjusted models. Dose-dependent associations between total 25(OH)D concentration and high PP (p-trend < 0.001 and < 0.001) were observed in females and in non-overweight subjects.
Multiple logistic regression of high pulse pressure with total 25(OH)D concentrations in the subgroups by sex and BMI. *p-trend < 0.05 considered significant. Adjusted for age, sex, race/ethnicity, education, season of examination, physical activity, alcohol consumption, smoking status, dietary covariates (intakes of total energy, potassium, calcium, magnesium, and sodium), height, weight, and diabetes.
When stratified by sex, females had a significantly lower OR for high PP were 0.58 (95% CIs 0.42, 0.79) in subjects with sufficient total 25(OH)D concentrations (versus deficient subjects), whereas males had a higher OR for high PP were 1.10 (95% CIs 0.84, 1.45) in subjects with sufficient total 25(OH)D concentrations. The associations between total 25(OH)D concentration and high PP significantly differed according to sex (p for interaction = 0.005).
When stratified by BMI, non-overweight subjects had a significantly lower OR for high PP were 0.38 (95% CIs 0.22, 0.67) in subjects with sufficient total 25(OH)D concentrations (versus deficient subjects), whereas overweight subjects showed no significant difference in the risk for high PP according to the total 25(OH)D concentrations. The associations between total 25(OH)D concentration and high PP significantly differed according to BMI (p for interaction = 0.004).
Participant characteristics according to the three BMI classifications are presented in Supplemental Table 1. In sensitivity analysis, when stratified by the three BMI classifications (obese, overweight, and, non-overweight), subjects with overweight and obesity showed no significant difference in the risk of high PP based on total 25(OH)D concentrations in Supplemental Table 2.
Discussion
In a nationally representative sample of middle-aged and older adults, we found that vitamin D sufficiency is associated with a lower risk of high PP. When stratified by sex and BMI, females and non-overweight subjects presented significant associations between vitamin D sufficiency and lower risk of high PP, whereas the risk for high PP did not vary significantly with the 25(OH)D concentrations in males and overweight subjects. Aging is associated with a progressive increase in vascular stiffness and PP2. High PP has been attributed to elastic fiber degeneration and aortic dilation, which transfers the hemodynamic load to stiffer collagen14; this condition is associated with an increased risk for cardiovascular disease and overall mortality15,16. Therefore, effective management of PP is very important to prevent cardiovascular disease and to ensure a healthy life in the elderly6,7. Several studies have reported that serum vitamin D concentrations are inversely associated with vascular stiffening9,10. It is possible that vitamin D improves general arterial health and increases arterial elasticity, which results in improvement in arterial compliance and decrease in PP11. Additionally, vitamin D may improve endothelial function by modulating inflammation-related cytokines and by increasing the expression of vascular endothelial growth factors17. One experimental study conducted by Pelham et al. investigated whether vitamin D deficiency leads to impaired function in the resistance artery by altering the phenotype of perivascular adipose tissue (PVAT). They reported that vitamin D deficiency enhances angiotensin II-induced vasoconstriction and impairs the normal ability of PVAT, whereas, the intake of supplementary vitamin D can protect against vascular dysfunction caused by impaired PVAT function due to hypoxia18.
Although epidemiological evidence consistently shows that vitamin D affects musculoskeletal health19, there has been a recent debate regarding the role of vitamin D deficiency in blood pressure based on conflicting observational and intervention studies20,21,22. Inconsistent results of the association between vitamin D and PP, particularly in clinical studies, may have been caused by differences in the study population and design, i.e., differences in the definition of vitamin D deficiency, supplementary vitamin D dose, and/or serum 25(OH)D concentrations, along with differences in the study period23,24,25,26. Nevertheless, a clinical study by Raed et al. reported that high doses of vitamin D (> 18,000 IU) for women with vitamin D deficiency (< 20 ng/mL) were effective in reducing PP27, which may, in part, support our hypothesis.
The current study suggests that the role of vitamin D deficiency in PP may differ depending on sex and BMI. Accordingly, the following interpretations could be made. The differences in results between males and females observed in the current study may be due to the fact that males have a higher visceral fat percentage than females. An increase in the visceral fat component of the body leads to an increase in the secretion of free fatty acids28, which degrades vascular function29. Males also have a higher level of insulin resistance than females28. Increased insulin resistance is a major risk factor that lowers vascular elasticity30. In addition, the androgen levels in males are higher than that in females. A study reported that androgens may upregulate the renin-angiotensin system and may play an important role in the pathogenesis of hypertension, which could cause endothelial injury31. Moreover, a recent study conducted by Varakantham et al. suggested the sex-specific role of CYP24A1 genetic variants related to vitamin D metabolism and reported that the risk of hypertension is increased in men with the rs2762939 CC variant; however, this risk of hypertension is decreased in women with the rs2762939 CC variant. This difference is thought to be due to the different effects of CYP24A1 genetic variants on 25(OH)D and renin concentrations in a sex-dependent manner32. Overall, males are metabolically vulnerable to lower vascular elasticity compared to females; thus, the vascular elasticity status may not reflect the vitamin D activity.
Different findings according to weight may be explained by the fact that vitamin D is a fat-soluble vitamin, and is deposited in fat cells; this leads to a decrease in the bioavailability of vitamin D in obese individuals33. Obesity may reduce the elasticity of blood vessels by increasing oxidative stress and inflammation34. A recent study suggested that the effect variations of vitamin D are due to the differences in volume of distribution35. Obese individuals with a high volume of distribution require a higher dose of vitamin D compared to non-obese individuals36. Differences in the volume of distribution and in the bioavailability of vitamin D depending on body weight, and decrease in vascular elasticity due to obesity status, may possibly explain why an association between vitamin D concentrations and blood pressure parameters was not observed in overweight subjects in our study.
Several major strengths of this study should be noted. The primary strength was the use of a nationally representative survey of middle-aged and older adults in the US, and the inclusion of a large sample size. Vitamin D concentration was assessed using serum 25(OH)D and 25(OH)D3 concentrations, which are accepted as biomarkers of the vitamin D status and vitamin D intake over a period of 4 years37,38; the concentrations were measured using UHPLC-MS/MS, which is an accurate and precise method. In addition, our models included the adjustment for various potential confounders, including sociodemographic, behavioral, and dietary factors, and also included interaction terms to reflect participants’ heterogeneity.
Several limitations of the results must also be considered. First, because of the cross-sectional design, we cannot infer temporal causality. Second, findings from the large proportion of non-Hispanic whites in the study population should be taken with caution when generalizing to other ethnic populations. Third, although we adjusted our model for a variety of covariates, there is a possibility of residual confounding. For example, parathyroid hormone is thought to be a factor that can affect the association between serum vitamin D concentration and blood pressure39, although we did not adjust for serum parathyroid hormone due to the lack of availability of pertinent data in the NHANES 2007–2010. Additionally, nitric oxide may be generated in the skin through ultraviolet (UV)-A radiation exposure40 and regulated by physical exercise41,42, which may affect the reduction in vascular stiffness. However, we did not adjust for subcutaneous nitrogen compounds due to no available data in the NHANES. Fourth, it might be argued that our observed associations may differ depending on race/ethnicities and/or season of examination. Indeed, in our sensitivity analyses, the associations between total 25(OH)D and high PP were stronger in non-Hispanic Whites (see Supplemental Table 3) and during the warm season (see Supplemental Table 4). As solar UV radiation doses are high during the summer and there is an effect of solar UV radiation on blood pressure due to the release of nitric oxide, one needs to consider different seasons while interpreting our findings. Finally, although the NHANES includes dietary data for the first and the second day, we used dietary data for the first day alone because the method used to obtain dietary data on the second day (phone interview) differed from that used on the first day (face-to-face interview).
In summary, this study shows that vitamin D sufficiency is associated with a lower risk of high PP, possibly due to decreased arterial stiffness, in middle-aged and older adults. In particular, the association between vitamin D status and a lower risk of high PP was stronger among females and non-overweight subjects. Adequate sunlight exposure (5–30 min, 2–3 time/week)43, intake of foods naturally high in vitamin D (sun-dried mushrooms; egg yolks; oily fish such as salmon, sardines, mackerel; and meat)44 and foods fortified with vitamin D (milk and cereals)45, and vitamin D supplementation are likely to improve the vitamin D status and delay the elevation of PP and vascular stiffening in middle-aged and older adults.
Methods
Study population
The data used in this study pertained to participants aged ≥ 50 years and were obtained from the NHANES 2007–2010. The NHANES, conducted by the Centers for Disease Control and Prevention (CDC), is a health-related survey research program that assesses the health and nutritional status of a sample of the national civilian non-institutionalized United States (US) population. The survey uses a complex, multi-stage, stratified, clustered design with oversampling of Hispanic, non-Hispanic Black, and low-income White populations, as well as those aged ≥ 80 years. The survey includes interviews based on demographic, socioeconomic, and dietary questionnaires, as well as medical interviews and physical examinations including medical, dental, and physiological measurements46,47. The current study used the two most recent NHANES cycles (2007–2010), which included data on serum vitamin D concentration. We did not include prior NHANES cycles because their vitamin D concentration data were obtained using a method (i.e., radio-immunoassay) that was different from the one used in the 2007–2010 NHANES cycles.
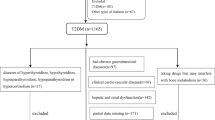
Among the initially enrolled subjects (n=20686) in the NHANES 2007–2010, complete data on both interviews and examinations were available for 20015 participants. For the present study, we selected adults aged ≥ 50 years, which resulted in 5644 participants. We additionally excluded subjects lacking information on SBP, DBP (n=45), serum vitamin D concentration (n=601), and other covariates (n=433); a total of 4565 subjects (2316 males and 2249 females) were included in our analysis. Details are illustrated in Figure 3. The study protocol was approved by the National Centers for Health Statistics Research Ethics Review board (Continuation of Protocol #2005-06). Written informed consent was obtained from all the NHANES participants. The NHANES is a publicly available dataset. Additional details on study procedures, data documentation, and questionnaires are available elsewhere46,47.
Measurement of 25-hydroxyvitamin D
Blood samples for the measurement of serum vitamin D concentration were collected from participants at mobile examination centers (MECs). The blood samples were immediately frozen at − 30 °C and were subsequently shipped to the National Center for Environmental Health (CDC, Atlanta, Georgia, USA) for analysis.
The serum (25(OH)D3 and 25(OH)D2 concentrations were measured using ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS; ThermoElectron Corp, West Palm Beach, FL)37,38. Total 25(OH)D concentrations (in SI units of nmol/L) were calculated by adding the 25(OH)D3 and the 25(OH)D2 concentrations. If information on either the 25(OH)D3 or 25(OH)D2 concentrations was not available, then the total 25(OH)D value was not computed. The coefficient of variation for the NHANES 2007–2010 was in the range of 3.0–3.8% for 25(OH)D3, and 3.8–6.5% for 25(OH)D2 estimations. The range of serum concentrations was 5.41–213 nmol/L for total 25(OH)D, 3.02–212 nmol/L for 25(OH)D3, and 1.45–183 nmol/L for 25(OH)D2. For statistical analysis, participants were categorized into three groups based on the total 25(OH)D and 25(OH)D3 concentrations, as follows: deficient, < 50 nmol/L; suboptimal, 50–74.9 nmol/L; and sufficient, ≥ 75 nmol/L, based on the cut-off points recommended by the US Endocrine Society48. We did not analyze 25(OH)D2 concentrations separately because the detection range for the analyte was very low.
Blood pressure
SBP and DBP were measured at the MECs using the Omron HEM 907 XL apparatus (Omron Healthcare, Kyoto, Japan). Blood pressure was measured after the participant had rested for 5 min in a seated position; the maximum inflation level was recorded. We computed the mean SBP and DBP of three consecutive SBP and DBP values. PP was calculated as the difference between SBP and DBP, and high PP was defined as a PP value of ≥ 60 mmHg49.
Body mass index
BMI was computed as weight in kilograms divided by height in meters squared (kg/m2). We defined “overweight” as a BMI of ≥ 25 kg/m2 and “non-overweight” as a BMI of < 25 kg/m2 in main analysis.
Covariates
We considered participants’ age, height, weight, race/ethnicity, education, season of examination, physical activity, alcohol consumption, smoking status, diabetes, and dietary intake (total energy, potassium, calcium, magnesium, and sodium) as potential confounders. Age was categorized as 20–29, 30–39, 40–49, 50–59, 60–69, and ≥ 70 years. Race/ethnicity was categorized as non-Hispanic White (reference), Mexican American, non-Hispanic Black, and others. Education was classified as less than 9th grade (reference), high school graduate or less, and more than a high school graduate. Smoking status was classified as never (reference), former, or current smoker. Alcohol consumption was categorized as never (reference), < 1 day a week, 1–2 days/week, 3–4 days/week, or ≥ 5 days/week. The season of examination was classified as November–April (reference) or May–October. Diabetes was defined as a self-reported physician diagnosis or the current use of antidiabetic medication. Physical activity was self-reported for three activity types (walking, moderate activity, and vigorous activity), and weekly metabolic equivalent (MET) values for each activity type were calculated as the MET value × day × min. Total MET scores were computed by summing the weekly MET values for each activity type50. Information on dietary intake (total energy, potassium, calcium, magnesium, and sodium) was obtained through a 24-h dietary recall interview. The 24-h recall data were analyzed using USDA's Food and Nutrient Database for Dietary Studies as a food composition database51.
Statistical analysis
Data analyses were performed using the SAS survey procedure (version 9.4; SAS Institute Inc., Cary, NC) to account for the complex survey design and sample weights of the NHANES 2007–2010. All p-values were two-sided, and a p-value of < 0.05 was considered statistically significant.
In the descriptive analysis, we presented weighted mean and SE for continuous variables and weighted percentages (%) for categorical variables. We further used the survey t-test for evaluating continuous variables and the Rao-Scott χ2 test for evaluating categorical variables. Serum 25(OH)D, 25(OH)D2, and 25(OH)D3 concentrations were right-skewed, and thus presented as geometric mean.
Pearson correlations between 25(OH)D (total 25(OH)D and 25(OH)D3) concentration and blood pressure were examined (r = − 0.03, p = 0.08 for total 25(OH)D; r = − 0.04, p = 0.005 for 25(OH)D3). The associations between 25(OH)D (total 25(OH)D and 25(OH)D3) concentration and blood pressure were examined using multiple linear regression models (PROC SURVEYREG). We evaluated two sequential models: model A adjusted for age, sex, and race/ethnicity; and model B adjusted for model A covariates plus season of examination, physical activity, alcohol consumption, smoking status, dietary covariates (intakes of total energy, potassium, calcium, magnesium, and sodium), height, weight, and diabetes. In addition, the associations between 25(OH)D concentration and high PP were examined using multiple logistic regression models (PROC SURVEYLOGISTIC).
All regression and logistic analyses were evaluated in subgroups stratified by sex (males vs. females) or BMI (≥ 25 vs. < 25 kg/m2). In addition, we estimated multiplicative interactions between serum 25(OH)D concentration and sex or BMI and computed the interaction p value using the Wald test.
Sensitivity analyses
First, when we modeled subgroups stratified by BMI, we used an alternative classification of three levels of BMI (obese; BMI ≥ 30 kg/m2, overweight; 25–29.99 kg/m2, and non-overweight; BMI < 25 kg/m2). Second, we performed sensitivity analysis on the association between total vitamin D levels and PP in subgroups stratified by race/ethnicity (non-Hispanic White, non-Hispanic Black, Mexican American, and other ethnicity) and the season of examination (November–April and May–October). Third, we conducted another sensitivity analysis after adjusting for additional dietary factors such as total fat, saturated fat, and cholesterol as potential confounders because these dietary factors are linked to blood pressure and are associated with elevated cardiovascular disease52,53,54.
Data availability
The datasets generated during and/or analyzed during the current study are available in the NHANES repository [https://wwwn.cdc.gov/nchs/nhanes/Default.aspx].
References
Fryar, C. D., Ostchega, Y., Hales, C. M., Zhang, G. & Kruszon-Moran, D. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS Data Brief 289, 1–8 (2017).
Said, M. A., Eppinga, R. N., Lipsic, E., Verweij, N. & van der Harst, P. Relationship of arterial stiffness index and pulse pressure with cardiovascular disease and mortality. J. Am. Heart. Assoc. 7, e007621 (2018).
Niiranen, T. J., Kalesan, B., Mitchell, G. F. & Vasan, R. S. Relative contributions of pulse pressure and arterial stiffness to cardiovascular disease. Hypertension 73, 712–717 (2019).
Vasan, R. S. et al. Interrelations between arterial stiffness, target organ damage, and cardiovascular disease outcomes. J. Am. Heart. Assoc. 8, e012141 (2019).
Sharif, S. et al. Arterial stiffness as a risk factor for cardiovascular events and all-cause mortality in people with type 2 diabetes. Diabet. Med. 36, 1125–1132 (2019).
Tajeu, G. S. et al. Incident cardiovascular disease among adults with blood pressure < 140/90 mm Hg. Circulation 136, 798–812 (2017).
Rodriguez, C. J. et al. Systolic blood pressure levels among adults with hypertension and incident cardiovascular events: The atherosclerosis risk in communities study. JAMA. Intern. Med. 174, 1252–1261 (2014).
Gepner, A. D. et al. A randomized controlled trial of the effects of vitamin D supplementation on arterial stiffness and aortic blood pressure in Native American women. Atherosclerosis 240, 526–528 (2015).
Gu, J. W. et al. Relationship between plasma levels of 25-hydroxyvitamin D and arterial stiffness in elderly Chinese with non-dipper hypertension: An observational study. Medicine (Baltimore) 99, e19200 (2020).
Jablonski, K. L., Chonchol, M., Pierce, G. L., Walker, A. E. & Seals, D. R. 25-Hydroxyvitamin D deficiency is associated with inflammation-linked vascular endothelial dysfunction in middle-aged and older adults. Hypertension 57, 63–69 (2011).
Liu, Z. M., Woo, J., Wu, S. H. & Ho, S. C. The role of vitamin D in blood pressure, endothelial and renal function in postmenopausal women. Nutrients 5, 2590–2610 (2013).
Rodriguez, A. J., Scott, D., Srikanth, V. & Ebeling, P. Effect of vitamin D supplementation on measures of arterial stiffness: A systematic review and meta-analysis of randomized controlled trials. Clin. Endocrinol. (Oxf.) 84, 645–657 (2016).
McMullan, C. J., Borgi, L., Curhan, G. C., Fisher, N. & Forman, J. P. The effect of vitamin D on renin-angiotensin system activation and blood pressure: A randomized control trial. J. Hypertens. 35, 822–829 (2017).
Torjesen, A. A. et al. Pulse pressure relation to aortic and left ventricular structure in the Age, Gene/Environment Susceptibility (AGES)-Reykjavik Study. Hypertension 64, 756–761 (2014).
Havulinna, A. S. et al. A blood pressure genetic risk score is a significant predictor of incident cardiovascular events in 32,669 individuals. Hypertension 61, 987–994 (2013).
Ecobici, M. & Voiculescu, M. Importance of arterial stiffness in predicting cardiovascular events. Rom. J. Intern. Med. 55, 8–13 (2017).
Dong, J. et al. Calcitriol protects renovascular function in hypertension by down-regulating angiotensin II type 1 receptors and reducing oxidative stress. Eur. Heart J. 33, 2980–2990 (2012).
Pelham, C. J., Drews, E. M. & Agrawal, D. K. Vitamin D controls resistance artery function through regulation of perivascular adipose tissue hypoxia and inflammation. J. Mol. Cell. Cardiol. 98, 1–10 (2016).
Charoenngam, N., Shirvani, A. & Holick, M. F. Vitamin D for skeletal and non-skeletal health: What we should know. J. Clin. Orthop. Trauma. 10, 1082–1093 (2019).
Reis, J. P., Von Mühlen, D., Miller, E. R., Michos, E. D. & Appel, L. J. Vitamin D status and cardiometabolic risk factors in the United States adolescent population. Pediatrics 124, e371–e379 (2009).
Reis, J. P., von Mühlen, D., Kritz-Silverstein, D., Wingard, D. L. & Barrett-Connor, E. Vitamin D, parathyroid hormone levels, and the prevalence of metabolic syndrome in community-dwelling older adults. Diabetes Care 30, 1549–1555 (2007).
Kunutsor, S. K., Burgess, S., Munroe, P. B. & Khan, H. Vitamin D and high blood pressure: Causal association or epiphenomenon?. Eur. J. Epidemiol. 29, 1–14 (2014).
Bressendorff, I. et al. The effect of high dose cholecalciferol on arterial stiffness and peripheral and central blood pressure in healthy humans: A randomized controlled trial. PLoS ONE 11, e0160905 (2016).
Grove-Laugesen, D. et al. Effect of 9 months of vitamin D supplementation on arterial stiffness and blood pressure in Graves’ disease: A randomized clinical trial. Endocrine 66, 386–397 (2019).
Arora, P. & Wang, T. J. Effect of vitamin D supplementation on arterial stiffness and central blood pressure indexes: Demystifying the evidence. J. Am. Heart. Assoc. 6, e007466 (2017).
Beveridge, L. A. et al. Effect of vitamin d supplementation on markers of vascular function: A systematic review and individual participant meta-analysis. J. Am. Heart. Assoc. 7, e008273 (2018).
Raed, A. et al. Dose responses of vitamin D3 supplementation on arterial stiffness in overweight African Americans with vitamin D deficiency: A placebo controlled randomized trial. PLoS ONE 12, e0188424 (2017).
Geer, E. B. & Shen, W. Gender differences in insulin resistance, body composition, and energy balance. Gend. Med. 6, 60–75 (2009).
Ghosh, A., Gao, L., Thakur, A., Siu, P. M. & Lai, C. W. Role of free fatty acids in endothelial dysfunction. J. Biomed. Sci. 24, 1–15 (2017).
Jia, G. et al. Vascular stiffness in insulin resistance and obesity. Front. Physiol. 6, 231 (2015).
Quan, A. et al. Androgens augment proximal tubule transport. Am. J. Physiol. Renal Physiol. 287, F452–F459 (2004).
Varakantham, V., Ale, K., Sailoo, A., Nagalla, B. & Bharatraj, D. K. Sex-specific role of CYP24A1 rs2762939 in the risk of essential hypertension based on the serum vitamin D and total renin concentrations. Genomics 112, 764–768 (2020).
Wortsman, J., Matsuoka, L. Y., Chen, T. C., Lu, Z. & Holick, M. F. Decreased bioavailability of vitamin D in obesity. Am. J. Clin. Nutr. 72, 690–693 (2000).
Aroor, A. R., Jia, G. & Sowers, J. R. Cellular mechanisms underlying obesity-induced arterial stiffness. Am. J. Physiol. Regul. Integr. Comp. Physiol. 314, R387–R398 (2018).
Gallagher, J. C., Yalamanchili, V. & Smith, L. M. The effect of vitamin D supplementation on serum 25(OH)D in thin and obese women. J. Steroid Biochem. Mol. Biol. 136, 195–200 (2013).
Ekwaru, J. P., Ohinmaa, A. & Veugelers, P. J. The effectiveness of a preventive health program and vitamin D status in improving health-related quality of life of older Canadians. Qual. Life Res. 25, 661–668 (2016).
CDC. National Health and Nutrition Examination Survey 2007–2008. Laboratory procedure manual: 25-hydroxivitamin D3, C3-epi-25-hydroxyvitamin D3, and 25-hydroxyvitamin D2 in serum by ultra high performance liquid chromatography-tandem mass spectrometry. http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/VID_E_met_Vitamin_D.pdf (2010).
CDC. National Health and Nutrition Examination Survey 2009–2010. Laboratory procedure manual: 25-hydroxivitamin D3, C3-epi-25-hydroxyvitamin D3, and 25-hydroxyvitamin D2 in serum by ultra high performance liquid chromatography-tandem mass spectrometry. http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/VID_F_met_Vitamin_D.pdf (2010).
Karadag, M. K. & Secen, O. Relationship of vitamin D and parathyroid hormone with the nocturnal blood pressure decline in hypertension. Blood Press. Monit. 22, 322–327 (2017).
Weller, R. B. et al. Does incident solar ultraviolet radiation lower blood pressure?. J. Am. Heart. Assoc. 9, e013837 (2020).
Otsuki, T., Namatame, H., Yoshikawa, T. & Zempo-Miyaki, A. Combined aerobic and low-intensity resistance exercise training increases basal nitric oxide production and decreases arterial stiffness in healthy older adults. J. Clin. Biochem. Nutr. 66, 62–66 (2020).
Fujie, S. et al. Aerobic exercise training induced irisin secretion is associated with the reduction of arterial stiffness via nitric oxide production in adults with obesity. Appl. Physiol. Nutr. Metab. 45, 715–722 (2020).
WHO. World Health Organization; 2020. Radiation: The known health effects of ultraviolet radiation. http://www.who.int/uv/faq/uvhealtfac/en/index1.html (2020).
Crowe, F. L. et al. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: results from the EPIC-Oxford study. Public Health Nutr. 14, 340–346 (2011).
Guo, J., Lovegrove, J. A. & Givens, D. I. 25(OH)D3-enriched or fortified foods are more efficient at tackling inadequate vitamin D status than vitamin D3. Proc. Nutr. Soc. 77, 282–291 (2018).
CDC. National Health and Nutrition Examination Survey 2007–2008. Data, Documentation, Codebooks, SAS Code. http://wwwn.cdc.gov/Nchs/Nhanes/Search/nhanes07_08.aspx (2018).
CDC. National Health and Nutrition Examination Survey 2009–2010. Data, Documentation, Codebooks, SAS Code. http://wwwn.cdc.gov/Nchs/Nhanes/Search/nhanes09_10.aspx (2018).
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 1911–1930 (2011).
Kim, J. K. & Crimmins, E. M. Blood pressure and mortality: Joint effect of blood pressure measures. J. Clin. Cardiol. Cardiovasc. Ther. 2, 1009 (2020).
Armstrong, T. & Bull, F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ). J. Public Health. 14, 66–70 (2006).
USDA Agricultural Research Service. Food and nutrient data base for dietary studies [Internet]. http://www.ars.usda.gov/Services/docs.htm?docid=12085. (Accessed 26 Jan 2021).
Gulseth, H. L. et al. Dietary fat modifications and blood pressure in subjects with the metabolic syndrome in the LIPGENE dietary intervention study. Br. J. Nutr. 104, 160–163 (2010).
Hooper, L. et al. Reduction in saturated fat intake for cardiovascular disease. Cochrane. Database. Syst. Rev. 5, CD011737 (2020).
Mente, A. et al. Association of dietary nutrients with blood lipids and blood pressure in 18 countries: A cross-sectional analysis from the PURE study. Lancet. Diabetes. Endocrinol. 5, 774–787 (2017).
Acknowledgements
This study analyzed data provided by the National Health and Nutrition Examination Survey 2007–2010. This work was supported by the National Research Foundation of Korea (NRF) funded by the Korea Ministry of Education (Grant numbers 2013R1A6A3A04059556 and 2017R1A6A3A11034504) and the Korea Ministry of Science and ICT (Grant number 2020R1A2C1101703).
Author information
Authors and Affiliations
Contributions
J.H.K. designed and created the study concept; J.H.K acquired the data, performed the statistical analysis and wrote the paper; Y.-H.C. contributed critical advice and revisions of the manuscript; J.H.K. and Y.-H.C. had responsibility for the entire content of the manuscript and obtained funding; Y.-H.C. supervised the study; and both authors had full access to the study data and read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kwak, J.H., Choi, YH. Sex and body mass index dependent associations between serum 25-hydroxyvitamin D and pulse pressure in middle-aged and older US adults. Sci Rep 11, 9989 (2021). https://doi.org/10.1038/s41598-021-88855-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88855-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.