Abstract
Healthcare workers (HCWs) are at increased risk of being infected with SARS-CoV-2, yet limited information is available on risk factors of infection. We pooled data on occupational surveillance of 10,654 HCW who were tested for SARS-CoV-2 infection in six Italian centers. Information was available on demographics, job title, department of employment, source of exposure, use of personal protective equipment (PPEs), and COVID-19-related symptoms. We fitted multivariable logistic regression models to calculate odds ratios and 95% confidence intervals of infection. The prevalence of infection ranged from 3.0 to 22.0%, and was correlated with that of the respective areas. Women were at lower risk of infection compared to men. Fever, cough, dyspnea and malaise were the symptoms most strongly associated with infection, together with anosmia and ageusia. No differences in the risk of infection were detected according to job title, or working in a COVID-19 designated department. Reported contact with a patient inside or outside the workplace was a risk factor. Use of a mask was strongly protective against risk of infection as was use of gloves. The use of a mask by the source of exposure (patient or colleague) had an independent effect in reducing infection risk.
Similar content being viewed by others
Introduction
Healthcare workers (HCWs) are a group at high risk of infection in general1 and specifically of SARS-CoV-2 infection2,3. However, few studies have been reported on prevalence of COVID-19, and on related risk factors in this group of workers4, including a study of 1654 HCWs from England5, one on 72 infected HCWs from China6, and two small studies of HCWs from Switzerland and Singapore who had a contact with a case7,8. Given the lack of information on determinants of infection in this important occupational group, and the relevance of such data for other groups of the population, we undertook an analysis of clinical and occupational data collected among more than 10,000 Italian HCWs who were tested for presence of SARS-CoV-2 during March and April 2020. The project was conducted in seven academic centers under the auspices of the Scientific Committee of the Italian Society of Occupational Medicine.
Results
A total of 10,654 HCWs were included in the analysis. Period of testing, incidence and mortality rates of COVID-19 infection in the general population of the study areas are shown in Table 1. Key characteristics of the study population are included in Table 2. Women represented two thirds of HCWs included in the analysis (which reflects the HCW demographics in Italy); average age ranged from 34 to 47 years, with overall mean of 45.4 years (sd 0.53). In all centers, nurses and doctors represented two thirds or more of HCWs tested for SARS-CoV-2.
Overall, 843 (10.3%) HCWs tested positive among 8,203 subjects included in surveillance systems. With the exclusion of the center in Genoa, in which only faculty members and residents who presented a clinical picture suggestive for COVID-19 (suspected cases) were tested (34% positive), the prevalence of HCW positive for SARS-CoV-2 ranged from 3% in Bari and Pisa to 22% in Brescia, while this prevalence in the other centers was between 5 and 7% (Table 3): There was a strong correlation between prevalence of infection in HCWs and COVID-19 incidence (r = 0.93, p = 0.002) and mortality (r = 0.99, p = 0.0001) in the overall population of the study areas.
The ORs of SARS-CoV-2 infection for sex, age, and self-reported symptoms are reported in Table 4. Female HCWs were at lower risk of infection than male HCWs; no differences were detected according to age. Self-reported (or measured) fever was strongly associated with infection; additional symptoms associated with SARS-CoV-2 infection include cough, dyspnea, malaise, and ageusia or anosmia; information on the latter two symptoms was available only for a subset of HCWs, but they showed a very strong association with infection. Conversely, self-reported sore throat and diarrhea were not associated with infection in this population.
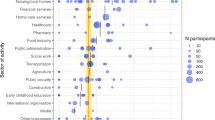
Results on the association between SARS-CoV-2 infection and job-related circumstances of exposure are reported in Table 5. No differences in the risk of infection were detected for job titles, although there was some heterogeneity in results among centers (not shown in detail). Working in a COVID-19 designated department was not a risk factor for infection. The analysis on the potential source of infection indicated that contact with a patient was associated with a higher risk of SARS-CoV-2 infection compared to contact with a colleague, which represented the majority of contacts at the workplace.
The use of surgical mask was associated with a reduced risk of infection, while the use of a filtering facepiece 2 or 3 (FFP2/FFP3) mask did not appear to confer additional protection. Use of gloves was also associated with a reduced risk of infection, while no difference was detected for use of face shield or gown. After adjusting for personal use of mask, the fact that the contact (patient or colleague) wore a mask was associated with a strong reduction in risk of infection (OR 0.52; 95% CI 0.32–0.85). If both the HCW and the contact wore a mask, the risk of infection was strongly reduced (OR 0.31; 95% CI 0.17–0.57) compared to the situation in which neither did.
The results of the two-stage meta-analyses replicated those of the pooled analyses; for example, the meta-OR for employment as health care attendant was 1.08 (95% CI 0.80–1.36; p-value of test for heterogeneity = 0.73), that for using a medical mask was 0.61 (95% CI 0.41–0.81, p heterogeneity = 0.92).
Discussion
This analysis revealed that the prevalence of infection in HCWs varied across centers, with results collected in centers with comparable protocols ranging from 3.0 to 22.0%, and was strongly correlated with that of the respective geographic areas. These figures fitted the prevalence of infection and mortality from COVID-19 in the general population of the study areas. Despite the limitations in the available data, in particular those from the general population9, these results confirm and quantify the variability in the risk of infection experienced by HCW according to the distribution of SARS-CoV-2 infection in the patient population of the hospitals where they worked. A survey of 1097 HCWs from six hospitals in the Netherlands also reported ample variability between regions10.
In general, national guidelines for testing HCW were followed in all centers, although the number of available PCR tests was low in the early phase of the epidemic. At the beginning, PCR tests were limited to symptomatic HCWs, and eventually HCWs reporting a contact were also tested. Although there were differences among the centers, they were relatively minor. In addition, these changes would not affect the association between exposure circumstances and probability of a positive result, which was the main goal of our analysis. It is important to note that we did not intend to provide a direct comparison of the proportion of positive PCR results between HCWs and the population at large in each study area, rather to show that the proportion of positivity among HCWs tested according to a similar protocol varied among areas, and this variation was similar to that observed in the population at large.
Middle-aged women in Italy experienced during the first wave of the epidemic a slightly higher incidence of SARS-CoV-2 infection compared to men, although incidence at older age and the proportion of cases of severe COVID-19 and death across in the whole age range were lower. For example, as of June 3rd, 2020, the female/male ratio in the number of cases in the age range 30–69 was 1.0711. compared to a ratio of 1.02 in the Italian population. In this population of HCWs, on the other hand, the risk of infection was lower in women compared to men; however, in the subset of HCWs with information on source of contact, no difference in risk was shown according to gender (OR 0.97; 95% CI 0.74–1.27 after adjustment for contact with colleague and patient). This suggests that any difference may be due to circumstance of exposure rather than gender differences. In a study of 72 HCWs from Wuhan, China, men were at higher risk of infection compared to women6. Age was not associated with risk of exposure in this population, similar to a small study from Wuhan, China6. These results suggest that differences by age observed in the general population11 might be due either to higher opportunity of exposure, or to higher number of tests performed.
Information on symptoms was available for most HCWs undergoing testing for SARS-CoV-2 infection. Fever and, to a lesser extent, cough, dyspnea and malaise were the symptoms most strongly associated with infection, while sore throat and diarrhea did not predict a positive results. Information on ageusia and anosmia was collected in a few centers, and only after several weeks of testing: even if they were available on a relatively small number of HCWs, these symptoms were strongly predictive of infection12.
The analysis by job title and department of employment represents one of the most important contributions of this study. The lack of a clear pattern in risk according to job categories indicates that all HCWs, at least those in the centers included in the analysis, were at comparable risk of becoming infected. The lack of information on the denominators, that include also HCWs who were not tested because they did not fulfill the criteria initially established by the Italian Ministry of Health13 or were tested outside the occupational surveillance system, limits our ability to draw conclusions on the absolute risk in the different occupational groups. To address this question, we analyzed a group of HCWs from one center (Bari) who were tested outside the protocol based on contact and symptoms. Among 2373 such HCWs, 11 cases of SARS-CoV-2 infection were detected, of whom three among 831 nurses, seven among 798 physicians (OR 4.1; 95% CI 1.0–16.4) and one among 381other health care professionals (OR 0.7; 95% CI 0.1–6.5). The lack of difference in infection prevalence by job is consistent with the results of a study of 1654 HCWs from England5. The lack of difference in risk between HCWs who worked in designated COVID-19 departments and those who worked in other departments is reassuring as it indicates that working in high-risk environment did not entail a higher risk of infection, probably because of increased awareness and proper use of PPEs by the employees. For example, the proportion of HCWs employed in COVID-19 departments who reported using surgical mask or FFP2/3 was 87%, compared to 78% of other HCWs. Our results are also comparable to those reported in a study of 183 SARS-CoV-2 positive US HCWs, among whom the prevalence of infection was comparable between frontline and non-frontline HCWs14.
Although the group of HCWs from Genoa was restricted to physicians, we do not think that this selection has introduced bias. Physicians in Genoa were tested according to the same criteria used in other centers, and job title was adjusted for in the analyses. The analysis of circumstances of exposure with a COVID-19 case suggested a role for contact with a patient compared to contact with a colleague or a contact outside the workplace.
The effect of PPE use on the risk of becoming infected with SARS-CoV-2 varied according to the device. The use of a surgical mask or a FFP2/3 mask appeared to be the single most effective approach to reduce risk. We found no difference in the effect of using a FFP2/3 instead of using a surgical mask (results not shown in detail). Reported use of gloves was also associated with a reduced risk of infection, although the result did not reach the formal level of statistical significance, while use of face shield or disposable gown was not associated with reduced risk of infection. It is important to note that this information was self-reported by the HCWs, and might be subject to some degree of misclassification, which is likely to be non-differential with respect to infection, since it was collected before the HCWs knew about their status. Such misclassification would likely reduced the measured protective effect of PPEs. An original and important finding of our analysis is the strong protection offered by the use of a surgical or FFP2/3 mask by both the HCW and the patient: the effects of the two devices appear to be additive, with a measured risk of SARS-CoV-2 infection that was less than one third when both were used compared to when neither was. The World Health Organization recommends that HCWs caring for inpatient COVID-19 patients wear a medical mask, gown, gloves and eye protection15. Wearing a medical-grade mask is consistent with our findings, there is strong evidence in the literature that use of medical-grade masks protects against viral infection in both outpatient and inpatient settings16,17, including infection with Coronaviruses18. When we searched for randomized trials comparing the protective effects of surgical vs. FFP2/3 masks against Coronaviruses, we did not identified any for novel SARS-CoV-2 causing COVID-19. The debate concerning the comparison of the protection exerted by FFP2/3 masks compared to surgical masks is still ongoing and needs further research19,20. No data were available in the literature on the effect of mask wearing by the source of exposure (patient or colleague). The evidence concerning which characteristics of other PPEs affect their effectiveness in preventing SARS-CoV-2 infection is still limited17,21.
Our study suffers from some limitations. Data were collected independently in the different centers; the harmonization process might have generated some misclassification, which however was likely non-differential with respect to infection status since information on risk factors was collected before tests were conducted. Although standard protocols were established at the national level to test HCWs, it is possible that some individuals were tested outside such protocols. In addition, rhinopharyngeal swabs detect the presence of SARS-CoV-2 at the time of the test, and it is possible that some HCWs who tested negative had been previously infected and developed an asymptomatic disease. In addition, the test itself has estimated sensitivity of 80% or less, while the specificity is as high as 99%22. Information on SARS-CoV-2 infection status among contacts of HCWs was not available. Finally, no information was available on the viral load of positive tests, comorbidities, or hospital admissions of HCWs included in the study was not available. However, none of them died from COVID-19. In general, HCWs represent a healthier group compared to the population at large.
Advantages of our study include, in addition to the large number of HCWs and the heterogeneity of their jobs and exposure circumstances, the availability of data on multiple potential determinants of SARS-CoV-2 infection, and the prospective collection of information, that reduces the likelihood of reporting bias. Each center followed the guidelines issued by the National Institute of Public Health; there were some minor differences decided by regional health authorities; the policy regarding PPE use was quite homogeneous among centers, although the availability of equipment was limited in the initial phase of the epidemic.
In conclusion, our study showed the importance of studying SARS-CoV-2 infection in HCWs with potential high exposure to the virus, and identified several determinants of infection that are also relevant to other occupational groups and the population at large. More large-scale studies are warranted on HCWs from other countries which experienced a range of severity of the COVID-19 epidemic and implemented different approaches for the prevention of infection in HCWs.
Methods
We pooled the data on SARS-CoV-2 infection collected by the occupational medicine centers involved in the surveillance of HCWs in large urban Italian hospitals in Bari, Bologna, Brescia, Genoa, Pisa and Turin. The study centers are shown in Fig. 1, together with the regional cumulative incidence of SARS-CoV-2 infection as of 6 May 2020. Starting in March 2020, surveillance systems were established in each center to monitor HCWs for possible infection with SARS-CoV-2, including testing them with swabs to detect SARS-CoV-2 RNA by RT-PCR, in Regional Reference Laboratories, and databases were established to monitor and follow them up. No information on viral load was available.
In all centers, HCWs were tested for SARS-COV-2 infection using either a rhinopharyngeal or an-oro-pharyngeal swab23. Samples were analyzed according to the guidelines proposed by the World Health Organization13. In general, HCWs were tested if matched one of the following case definitions, although some details differed across different centers, and definitions changed slightly over time:
-
(i)
patients with severe acute respiratory illness (fever and at least one sign or symptom of respiratory disease, i.e., cough, shortness of breath, and requiring hospitalization) in the absence of an alternative diagnosis that fully explains the clinical presentation;
-
(ii)
patients with acute respiratory illness (fever and at least one sign/symptom of respiratory disease, e.g., cough, shortness of breath), and a history of travel to or residence in a location reporting community transmission of COVID-19 disease prior to symptom onset;
-
(iii)
subjects with or without acute respiratory illness or symptoms, who have been in contact with a confirmed or probable COVID-19 case in the absence of adequate protection.
Tests were repeated for most subjects with a positive result to monitor the infection; a proportion of subjects with a negative result were re-tested because of repeated contact with a COVID-19 case. In one center (Bari) additional HCWs, including subcontract workers, who did not fulfill the inclusion criteria described above, were also tested. In another center (Genoa) only physicians (faculty members and residents) who presented a clinical picture suggestive for COVID-19 (suspected cases) were tested. These subjects were excluded from the analysis of prevalence of SARS-CoV-2 infection, but were retained in the analysis of determinants of infection. The period during which tests included in this analysis were performed, as well as key characteristics of the COVID-19 epidemic in the provinces (intermediate administrative units) where the centers are located.
HCWs in centers located in heavily affected areas (Bologna, Brescia, Genoa, Turin) started to be tested at the beginning of March 2020, while testing started in subsequent weeks in centers located in less affected areas (Bari, Pisa). The present analysis included results of tests performed up to April or early May 2020, depending on center.
Different formats were used to collect data in each center, we established a minimum data record whit this set of variables: basic demographic data, job title, hospital department or department of employment, including working in a designated COVID-19 department, self-reported circumstances of contact with a case, self-reported use of personal protection equipment (PPE), including, in one center, use of PPEs by the contact person, and selected self-reported (or measured) symptoms. The list of variables is specified in Supplementary Table S1.
We retained in the analysis HCWs with at least one valid test result; the outcome of the analysis was the presence of at least one positive result. Multivariable logistic regression models were fitted to the data to estimate odds ratios (ORs) of positive result in at least one test, together with 95% confidence intervals (CIs). All models included sex, age group and center as potential confounders. Models including additional potential confounders were also run, but in general there was little evidence of reciprocal confounding between exposure variables. In a secondary analysis, center-specific ORs for selected risk factors were combined using a random-effects meta-analysis24 to assess the validity of the data pooling approach.
The study was reviewed and considered exempt by the Ethics Committee of the University of Bologna.
Ethical approval
All methods were carried out in accordance with relevant guidelines and regulations. The study was reviewed and considered exempt by the Ethics Committee of the University of Bologna. Informed consent was not deemed necessary by the Ethics Committee of the University of Bologna.
References
Baker, M. G., Peckham, T. K. & Seixas, N. S. Estimating the burden of United States workers exposed to infection or disease: A key factor in containing risk of COVID-19 infection. PLoS ONE 15, e0232452 (2020).
Wu, Z. & McGoogan, J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323, 1239 (2020).
Zhou, P. et al. Protecting Chinese healthcare workers while combating the 2019 novel coronavirus. Infect. Control Hosp. Epidemiol. 41, 745 (2020).
Wander, P. L., Orlov, M., Merel, S. E. & Enquobahrie, D. A. Risk factors for severe COVID-19 illness in healthcare workers: Too many unknowns. Infect. Control Hosp. Epidemiol. 45, 652 (2020).
Hunter, E. et al. First experience of COVID-19 screening of health-care workers in England. Lancet 395, e77–e78 (2020).
Ran, L. et al. Risk Factors of healthcare workers with Corona Virus Disease 2019: A retrospective cohort study in a designated hospital of Wuhan in China. Clin. Infect. Dis. 71, 2218 (2020).
Canova, V. et al. Transmission risk of SARS-CoV-2 to healthcare workers—Observational results of a primary care hospital contact tracing. Swiss Med. Wkly. 150, w20257 (2020).
Ng, K. et al. COVID-19 and the risk to healthcare workers: A case report. Ann. Intern. Med. 172, 766 (2020).
Boccia, S., Ricciardi, W. & Ioannidis, J. P. A. What other countries can learn from Italy during the COVID-19 pandemic. JAMA Intern. Med. 180, 927 (2020).
Reusken, C. B. et al. Rapid assessment of regional SARS-CoV-2 community transmission through a convenience sample of healthcare workers, the Netherlands, March 2020. Euro Surveill. 25, 2000334 (2020).
Riccardo, F. et al. Epidemia COVID-19—Aggiornamento nazionale3 giugno2020–ore 15:00 (Istitute Superiore di Santià, 2020).
Passarelli, P. C., Lopez, M. A., Mastandrea Bonaviri, G. N., Garcia-Godoy, F. & D’Addona, A. Taste and smell as chemosensory dysfunctions in COVID-19 infection. Am. J. Dent. 33, 135–137 (2020).
World Health Organization. Laboratory Testing for Coronavirus Disease (COVID-19) in Suspected Human Cases Interim Guidance (WHO, 2020).
Mani, N. S. et al. Prevalence of COVID-19 infection and outcomes among symptomatic healthcare workers in Seattle, Washington. Clin. Infect. Dis. 71, 2702 (2020).
World Health Organization. Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19): Interim Guidance (WHO, 2020).
Garcia Godoy, L. R. et al. Facial protection for healthcare workers during pandemics: A scoping review. BMJ Glob. Health 5, e002553 (2020).
Mermel, L. A. Eye protection for preventing transmission of respiratory viral infections to healthcare workers. Infect. Control Hosp. Epidemiol. 39, 1387 (2018).
Seto, W. H. et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet 361, 1519–1520 (2003).
Violante, T. & Violante, F. Surgical masks vs respirators for the protection against coronavirus infection: State of the art. Med. Lav. 111, 365 (2020).
Chu, D. K. et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 395, 1973 (2020).
Verbeek, J. H. et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst. Rev. 5, 011621 (2020).
Zitek, T. The appropriate use of testing for COVID-19. West J. Emerg. Med. 21, 470–472 (2020).
US Centers for Disease Control and Prevention. Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens for COVID-19 2020 (US CDC, 2020).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 7, 177–188 (1986).
Funding
The study was funded with internal resources of the participating institutions.
Author information
Authors and Affiliations
Consortia
Contributions
P.B., F.V., P.A., P.D. and G.S.: design of the study. F.V., P.D., L.V., G.D.P., A.Cr. and E.Pi.: supervision of data collection. G.D., E.Sal., M.Co., S.T., L.D.M., A.Ca., S.S., C.M., C.Z., G.D.F., G.V., E.A., E.San., C.T., A.B., L.C., A.D.B., M.M.T., E.Pa., S.R., M.Ca., G.I., B.B., N.D., A.M., A.R., A.O., V.R., A.G., M.D., I.M., N.M., G.Ga., A.S., G.Gu., V.G., L.F. and C.B.: data collection. G.I.: coordination of laboratory testing of SARS-CoV-2. P.B., FV., L.V., G.D.P., A.Cr., E.Pi., E.S., C.T. and I.M.: data harmonization, statistical analysis. P.B.: drafting of the manuscript. P.B., F.V., P.A., P.D., G.S., L.V., G.D.P., A.Cr., E.Pi., G.D. and G.I.: review of each phase of the study. All authors: review and approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boffetta, P., Violante, F., Durando, P. et al. Determinants of SARS-CoV-2 infection in Italian healthcare workers: a multicenter study. Sci Rep 11, 5788 (2021). https://doi.org/10.1038/s41598-021-85215-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-85215-4
This article is cited by
-
Impact of Covid-19 pandemic on children with special needs requiring general anaesthesia for the treatment of dental disease: the experience of the Brescia Children’s Hospital, Lombardy, Italy
European Archives of Paediatric Dentistry (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.