Abstract
Mycobacterium abscessus is emerging as a cause of recalcitrant chronic pulmonary infections, particularly in people with cystic fibrosis (CF). Biofilm formation has been implicated in the pathology of this organism, however the role of biofilm formation in infection is unclear. Two colony-variants of M. abscessus are routinely isolated from CF samples, smooth (MaSm) and rough (MaRg). These two variants display distinct colony morphologies due to the presence (MaSm) or absence (MaRg) of cell wall glycopeptidolipids (GPLs). We hypothesized that MaSm and MaRg variant biofilms might have different mechanical properties. To test this hypothesis, we performed uniaxial mechanical indentation, and shear rheometry on MaSm and MaRg colony-biofilms. We identified that MaRg biofilms were significantly stiffer than MaSm under a normal force, while MaSm biofilms were more pliant compared to MaRg, under both normal and shear forces. Furthermore, using theoretical indices of mucociliary and cough clearance, we identified that M. abscessus biofilms may be more resistant to mechanical forms of clearance from the lung, compared to another common pulmonary pathogen, Pseudomonas aeruginosa. Thus, the mechanical properties of M. abscessus biofilms may contribute to the persistent nature of pulmonary infections caused by this organism.
Similar content being viewed by others
Introduction
In the cystic fibrosis (CF) lung, due to genetic mutations in the cystic fibrosis transmembrane regulator (CFTR) ion channel responsible for this disease, the mucus lining of the airways becomes dehydrated and highly viscous, leading to impaired clearance and accumulation. This provides a niche that can be readily colonized by inhaled microorganisms, which form biofilm aggregates within the accumulated mucus layer1,2. These biofilms lead to recurrent progressive infections, inflammation, bronchiectasis and, eventually, respiratory failure. Nontuberculous mycobacteria (NTM) are an increasingly common complication in CF, now ranking as the third most frequent cause of lung infection in people with CF3,4,5. Mycobacterium abscessus infection is particularly challenging, infecting younger people with CF and resulting in a poorer prognosis than those infected with other NTM3,4,6,7,8. However, the mechanisms underlying the rising incidence of M. abscessus infection in people with CF remain ill-defined9,10.
Mycobacterium abscessus has two distinct colony variants, based on the presence (smooth morphotype; MaSm) or absence (rough morphotype; MaRg) of cell wall glycopeptidolipids (GPLs)11,12. The prevailing view of chronic M. abscessus infection is that MaSm is a noninvasive, biofilm-forming, persistent phenotype, and MaRg is an invasive phenotype that is unable to form biofilms. We have previously shown, however, that MaRg is hyper-aggregative and is capable of forming biofilm aggregates, which are significantly more tolerant than planktonic M. abscessus to acidic pH, hydrogen peroxide, or antibiotic treatment11. These studies indicate that development of biofilm aggregates contribute to the persistence of M. abscessus in the face of antimicrobial agents, regardless of morphotype. Antibiotic regimens that reliably cure M. abscessus infections are lacking. A better understanding of the the biofilm biology of this organism and its ability to cause persistent pulmonary infections is needed to explore new treatment strategies13,14.
The study of biofilm mechanics has gained interest, as it is being realized that these properties are important for understanding biofilm biology and how biofilms respond to chemical and mechanical forms of eradication15. Interestingly, changes in colony morphology have been correlated to differences in biofilm formation16, and differences in biofilm mechanics17,18. We therefore hypothesized that the biofilms of MaSm and MaRg may have different mechanical properties, due to their distinct colony morphologies, and that these properties may help to account for the persistence of infection caused by this organism. In the present study, we used mechanical indentation and shear rheometry to evaluate the viscoelastic properties of MaSm and MaRg biofilms. We also use known concepts of mucus viscoelasticity to predict how effectively M. abscessus biofilms may be cleared from the lung by mucociliary and cough clearance. Our findings support the hypothesis that biofilm viscoelasticity could contribute to the persistence of biofilm-associated infefctions15,19, and provides novel insight into why M. abscessus may be such a persistent pathogen in airway infection in people with CF.
Results
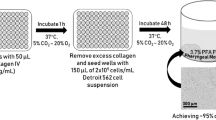
Ma colony-biofilms maintain the distinct morphologies of Ma Sm and Ma Rg variants
Mycobacterium abscessus is a rapidly growing NTM, typically showing colony morphology by 4 days on agar media. To test the hypothesis that biofilms of MaSm and MaRg variants might differ in their mechanical properties, uniaxial indentation and shear rheology was performed on 4 day M. abscessus colony-biofilms (See Supplementry Methods). As this is the first time that we have used this biofilm model for M. abscessus, we examined the colony-biofilms after 4 days of growth (Fig. 1). Macroscopically, biofilm formation was evident, covering the filter. Biofilm morphology maintained the characteristic phenotypes of each variant11. That is, biofilms of MaSm, had a smooth, almost mucoid appearance (Fig. 1A), while MaRg biofilms showed a cauliflower-like morphology (Fig. 1B) in agreement with our previous study showing cording at the periphery of MaRg colonies11. Importantly, when these colony-biofilms were disrupted, and plated to observe single cells, the number of cells within the biofilm was similar across the two variants, and no reversion across phenotypes was observed during this time (Fig. 1C), demonstrating that during the 4 day biofilm growth period, each variant was stable.
Morphology of MaSm and MaRg colony-biofilms. (A) MaSm and (B) MaRg were grown on nitrocellulose membranes for 4 days, transferring the membranes onto fresh media after 48 h. Colony-biofilms were then imaged to visualize the macroscopic morphology. Scale bar indicates 5 mm, and 0.5 mm for the zoomed insets. (C) To assess the biomass and if each variant was stable during biofilm formation, 4 day M. abscessus biofilms were enumerated for CFUs. Evidence of phenotypic changes of the colony morphologies for either was not observed at 37ºC over 4 days. Statistical analysis was performed using a Student’s t-test; ns indicated not significant. N = 3.
Ma Rg biofilms are stiffer than Ma Sm biofilms in uniaxial compression
To determine the stiffness of M. abscessus biofilms under a normal force (force that is applied perpendicular to the surface), uniaxial indentation was performed on 4 day M. abscessus colony-biofilms. During this analysis, biofilms are compressed and the required force is measured. This analysis is also used to determine the biofilm thickness, which revealed that biofilms of each variant were of similar thickness (Fig. 2A), consistent with the observation that biofilms had a similar number of CFUs (Fig. 1C). Stress–strain curves revealed that MaSm and MaRg biofilms displayed a ‘J-shaped’ curve, where the biofilms became progressively stiffer as they were compressed (Fig. S1). Stress–strain curves also revealed that there were significant mechanical differences between MaSm and MaRg biofilms (Fig. 2B; p = 0.0049). To quantify these differences, the Young’s modulus was determined from the lower linear portions of the curve, which revealed that the Young’s modulus of MaRg biofilms was approximately two-fold greater than MaSm biofilms. This indicates that MaRg biofilms were significantly stiffer under uniaxial compression, compared to MaSm biofilms (Fig. 2C; p = 0.0004).
MaRg colony-biofilms are stiffer compared to MaSm biofilms in compression. (A) Thickness and (B) stress–strain curves of 4 day M. abscessus colony-biofilms determined from uniaxial indentation analysis. (C) Young’s modulus of M. abscessus biofilms, determined from the lower linear potion of the force–displacement curve, corresponding to 0–30% strain. The full stress–strain curve, up to 100% strain is represented in Fig. S1. N = 4; data presented as individual data points with mean ± SD. Statistical analysis was performed using a Student’s t-test; ns indicates not significant.
M. abscessus biofilms are highly viscoelastic and Ma Sm biofilms are more pliant than Ma Rg under shear
To examine the mechanical properties of M. abscessus colony-biofilms in further detail, MaSm and MaRg biofilms were analyzed using spinning-disc rheology. For these analyses a shear force (a force that is applied parallel to a surface) is applied and the resulting stress or strain is measured (See Supplementary Methods). Oscillatory strain sweeps were performed, where the oscillatory strain was incrementally increased and the storage (G’) and loss (G”) moduli measured, which reflect the elastic and viscous response, respectively15. The measured storage and loss moduli plateaus were similar for MaSm and MaRg biofilms (Fig. 3A,B), suggesting that biofilms of each variant behaved similarly within the linear viscoelastic region. From this analysis we determined the yield strain, which represents the strain where the biofilm integrity begins to break down, due to the increasing applied strain, and transitions to fluid-like behavior20. Interestingly, the yield strain of MaSm biofilms was significantly greater than MaRg biofilms (Fig. 3C; p = 0.0098). This suggests that MaSm biofilms are more pliant than MaRg biofilms, and that MaSm biofilms can be deformed to a greater extent before cohesive failure occurs. This is also consistent with the Young’s modulus of these biofilms, which indicated that MaSm biofilms can be compressed more readily compared to MaRg biofilms (Fig. 2C).
MaSm colony-biofilms are more pliant than MaRg biofilms in shear. Strain sweep profiles of 4 day (A) MaSm and (B) MaRg colony-biofilms. N = 4; data presented as mean ± SD; G’ = storage modulus and G” = loss modulus. (C) Yield strain of M. abscessus colony-biofilms determined from (A) and (B). N = 4; data presented as individual data points with mean ± SD. Statistical analysis was performed using a Student’s t-test.
Oscillatory frequency sweeps were also performed, where the oscillatory frequency was incremented under a consistent applied strain, and the storage and loss moduli measured. Across the range of frequencies analyzed, the storage and loss moduli were relatively independent of frequency, with the storage modulus greater than the loss modulus for both M. abscessus variant biofilms (Fig. 4A,B). This indicates that both MaSm and MaRg biofilms displayed elastic behavior that was dominant across the analyzed conditions. There were no significant differences between the mechanical behavior of MaSm and MaRg biofilms using this analysis (Fig. 4C,D). However, compared to MaSm biofilms, MaRg biofilms trended toward a reduced loss modulus across the analyzed frequencies (Fig. 4D).
M. abscessus colony-biofilms are highly viscoelastic. Frequency sweep profiles of 4 day (A) MaSm and (B) MaRg colony-biofilms. G‘ = storage modulus and G” = loss modulus (C) Storage and (D) and loss moduli values at 1 and 100 rad/s. N = 4; data presented as mean ± SD. Statistical analysis was performed using a Student’s t-test; ns indicates not signficant.
Theoretical indices suggest that M. abscessus biofilms, independent of morphotype, may resist clearance from the lung
To determine if the mechanical properties of M. abscessus biofilms may correlate with recalcitrance of M. abscessus in pulmonary infections, we calculated the mucociliary (MCI) and cough (CCI) clearance index, according to Eqs. (2) and (3), using values from the frequency sweep analysis of these biofilms (Fig. 4). The MCI and CCI were developed to correlate sputum viscoelasticity to predicted levels of clearance from the lung via either mechanism21,22. The MCI and CCI of MaSm and MaRg biofilms were similar. However, due to the highly viscoelastic behavior of both colony variant biofilms (Fig. 4A,B), the indices were less than the MCI and CCI reported for sputum collected from people with CF (Fig. 5; line).
M. abscessus colony-biofilms have reduced theoretical mucociliary and cough clearance index. (A) Mucociliary and (B) cough clearance index of 4-day M. abscessus and P. aeruginosa (P.a) colony-biofilms. Lines at (A) and (B) are the MCI (0.81 ± 0.09) and CCI (1.3 ± 0.46), respectively, of sputum collected from patients with CF, previously determined by54. N = 4; data presented as individual data points with mean ± SD. Statistical analysis was performed using a one-way ANOVA with a Tukey’s post-hoc test; ns indicates not significant.
To compare M. abscessus biofilms to the biofilms of another common pathogen causing chronic pulmonary infections in people with CF, we analyzed 4 day wild type Pseudomonas aeruginosa colony-biofilms23. P. aeruginosa is considered a model organism for biofilm formation, and we have previously determined the MCI and CCI for this organism17. Using the same testing conditions for M. abscessus biofilms described here, we performed oscillatory frequency sweeps on 4 day wild type P. aeruginosa colony-biofilms (See Supplmentary Results; Fig. S2), and similarly determined the MCI and CCI for comparison (Fig. 5). The indices of MaSm and MaRg biofilms were significantly less than that determined for wild type P. aeruginosa biofilms (Fig. 5). This suggests that M. abscessus biofilms may be more resistant to mechanical clearance from the lung, compared to other common pulmonary pathogens, such as P. aeruginosa.
Discussion
Compared to other biofilm forming organisms, such as P. aeruginosa, the understanding of biofilm formation and the role of biofilms in infection of NTMs is limited. It is important to understand biofilm mechanics from a biofilm biology stand-point, as these properties dictate the stability of the three-dimensional community structure15. We therefore set out to analyze the mechanical properties of M. abscessus in vitro biofilms to gain a better understanding of the biofilm biology of this organism. We found that MaRg colony-biofilms were stiffer under normal forces (Fig. 2C), while MaSm colony-biofilms were more pliable under both normal and shear forces (Figs. 2C, 3C). In constrast to the uniaxial indentation analysis (Fig. 2), oscillatory frequency sweeps indicated that there were no significant difference in the viscoelasticity of MaSm and MaRg biofilms under shear forces (Fig. 4). This indicates that M. abscessus biofilms were anisotropic, in that they have different mechanical properties when exposed to either a normal or shear force.
Earlier research by others suggested that only MaSm variants formed biofilms and speculated that GPL expression enhanced sliding motility in CF mucus, making it better adapted to behave as a colonizing, biofilm-forming phenotype24,25. However, we have previously shown that the rough morphotype is hyper-aggregative11, indicating that each colony morphology variant is capable of forming biofilm aggregates. The finding here that MaSm colony-biofilms were more pliable under both normal and shear forces (Figs. 2C, 3C) suggests that GPL likely affects the mechanical properties of M. abscessus biofilms. Further studies are needed to better understand the relationship of M. abscessus cell wall determinants, such as lipids, GPLs, and extracellular polyermic substance (EPS) with biofilm function and is the focus of future studies.
Uniaxial indentation, revealed that MaSm and MaRg biofilms each displayed a ‘J-shaped’ curve in response to increasing compression (Fig. 2B). This response is typical of biological materials, and has previously been observed for a number of different types of bacterial biofilms17,26,27,28. The Young’s modulus of MaSm and MaRg colony-biofilms, determined here, is similar to that reported for Streptococcus mutans hydrated biofilms29, P. aeruginosa colony-biofilms17, and surface adhered Staphylococcus aureus, Staphylococcus epidermidis and Streptococcus salivarius cells30.
Interestingly, MaSm and MaRg colony-biofilms have a storage modulus, which describes the elastic solid-like behavior31, approximately tenfold greater than that previously observed for other bacterial biofilms (Fig. S2A)17,18,20,32,33,34,35,36,37,38,39,40. This suggests that M. abscessus biofilms, regardless of the morphotype, are highly viscoelastic, and much stiffer than biofilms formed by other bacterial pathogens. It would, therefore, be of interest to compare the mechanical properties of other NTM biofilms, as well as other biofilms that have a lipid dominant EPS, to determine the contributions of lipid content to the EPS and to the biofilm mechanical properties. It is interesting to speculate that different host niches in the lung (or other infection sites) may favor stiffer or softer biofilms depending on different shear and chemical micro environments. However, this requires further clinical work.
Viscoelasticity is a property common to biofilms, suggesting that it is an adaptive trait of these mircobial communites15. It has therefore been predicted that biofilm viscoelasticity, not only is important from a biofilm biology stand-point, but also when considering microbial survival41. Understanding how biofilm mechanics impacts microbial survival in an infection is still unclear. However, there is a growing consensus that these properties are important for resisting both mechanical and chemical methods of eradication15,19. To gain further insight into how the mechanics of M. abscessus biofilms may influence the recalictrance of these infections, we used known, well-established concepts of mucus viscoelasticity to draw new hypotheses that may be relevant to M. abscessus biofilms in vivo, in the context of mechanical clearance from the lung. Changes in mucus viscoelasticity in CF are attributed to mucus hyper-secretion and changes to mucus composition, impeding mucus clearance by both mucociliary and cough clearance42. MCI and CCI are theoretical indices that were developed from in vitro lung clearance models to correlate viscoelastic properties of expectorated mucus with predicted levels of clearance from the lung21,22. These indices have been used to assess the efficiency of mucolytics for therapy regimes for people with CF43. MCI predicts that mucus elasticity correlates to improved mucociliary clearance by promoting efficient cilia beating21,44, while CCI predicts that mucus viscosity correlates to improved cough clearance by promoting mucus-airflow interactions44,45. We previously used these known relationships between mucus viscoelasticity and clearance, and applied these concepts to P. aeruginosa colony-biofilms, to determine if the viscoelastic properties of bacterial biofilms could likewise theoretically impact mechanical clearance from the lung17. We identified that elastic non-mucoid P. aeruginosa biofilms had a reduced CCI, while mucoid P. aeruginosa biofilms that had a low viscosity, had both a reduced MCI and CCI17. Here we determined the MCI and CCI of M. abscessus biofilms, and observed that they had an even lower or negative CCI compared to P. aeruginosa, attributed to the high viscoelasticity of these biofilms (Fig. 5B). This indicates that M. abscessus biofilms of each morphotype may resist clearance from the lung by cough. These findings provide novel insight into possible reasons why M. abscessus is a persistent and difficult to treat pulmonary pathogen.
A longitudinal rheological study of sputum from CF patients indicated that both viscosity and elasticity increase during pulmonary exacerbations, suggesting that CF sputum viscoelasticity is linked to disease state and airflow obstruction46. By applying known concepts of mucus rheology to biofilm mechanics and infection, our findings provide a novel way to understand M. abscessus biofilms and their recalcitrance. Moving forward, it will be important to develop in vitro and in vivo models of biofilm-mucus interactions to explore the hypotheses drawn from this work. More broadly, the impact of evaluating bacterial biofilm mechanical properties offers new avenues for the treatment of intractable pulmonary infections. Disruption of M. abscessus aggregates increased susceptibility to several antibiotics13. Moreover, liposomes, lipid nanoparticles and nanoparticle lipid carriers are being evaluated for pulmonary use47. This approach has been used on biofilms of Burkholderia cepacia complex, as well as S. aureus and P. aeruginosa biofilms in vitro48,49. These products not only have the potential to reduce exposure to high concentrations of antimicrobial agents following aerosol administration by reducing toxicity, but particularly relevant to NTM antibiotic therapy, might ameliorate the severe side effects often associated with antimycobacterial treatment. This strategy could further be used to target NTM, which have a high lipid content, to facilitate cohesive failure of biofilm aggregates in the lung in adddtion to delivering targeted antibiotics.
Materials and methods
M. abscessus culture and biofilm model
The colony-biofilm model was used here due to the established utility of this model for rheological analysis of biofilms17,50 (See Supplementary Methods). Colony-biofilms were grown as previously described with modifications17. Briefly, M. abscessus cultures were prepared by inoculating a 10 μL loop of isolated MaSm or MaRg from 7H10 agar plates into 7H9 without tween media and a single cell suspension prepared as described11. Cultures were normalized to an OD600 of 0.15–0.2 and 100 μL was pipetted onto sterile nitrocellulose filter membranes (25 mm, 0.45 μm pore size; Millipore) and incubated at 37 °C, 5% CO2 under humidified conditions for 4 days. This time point was selected as it provided sufficent biomass necessary for rheological analysis, while maintaining the characteristic morphology of MaSm or MaRg variants. Colony-biofilms of PAO1 P. aeruginosa were grown as previously described17.
Colony-biofilms were imaged using a Stereo Microscope (AmScope) fitted with a Microscope Digital Color CMOS camera (AmScope). Images were processed in FIJI51. Figure was complied in Biorender.com.
To assess the number of CFU/cm2 on sterile membranes after 4 days, colony-biofilms were scraped and transferred to 5 mL of 7H9 + tween 80 and vortexed with glass beads to disperse cells from the biofilm11. Cell suspensions were serially diluted and enumerated for CFUs in triplicate on 7H10 agar plates. To determine if either variant converted/reverted to another colony variant during biofilm growth, colony morphology was also assessed and verified by sub-culturing three colonies per replicate to ensure that the colony morphology was stable. CFUs were plated to 108 dilution and colonies were streaked to isolation to validate colony variants.
Rheometry apparatus
A Discovery Hybrid Rheometer-2 with a heat exchanger attached to the Peltier plate (TA Instruments) was used for all rheological measurements. For uniaxial indentation and spinning disc measurements (See Supplementary Methods), the rheometer was fitted with an 8 mm and 25 mm sand-blasted Smart Swap geometry, respectively. All measurements were performed at 37 °C, with the Peltier plate covered with a moist Kimwipe to prevent dehydration of the colony-biofilm. TRIOS v4 (TA instruments) software was used.
Uniaxial indentation measurements
Uniaxial indentation measurements were performed under compression using an approach rate of 1 μm/s. Two colony-biofilms were analyzed per biological replicate (total of 4 biofilms analyzed), with two measurements per biofilm. The point of contact with the biofilm was determined to be where the force began to increase after the initial point of pull-on adhesion. Force–displacement curves were converted to stress–strain curves, for ease of comparison, as previously described17. The Young’s modulus was calculated according to Eq. (1)52:
where v is the assumed Poisson’s ratio of a biofilm (v = 0.5)27 and r is the radius of the geometry. The slope is of the force–displacement curve, and was taken at the lower linear region corresponding to 0–30% strain where R2 ≥ 0.9.
Spinning-disc rheology
To normalize for differences in biofilm thickness across replicates, prior to analysis, colony-biofilms were compressed to a normal force of 0.01 N. For all analyses a total of 4 biofilms were analyzed, 2 per biological replicate.
Strain sweeps were performed by incrementing the oscillatory strain from 0.01 to 100% at a frequency of 1 Hz. The yield strain was taken where the storage (G’) and loss (G”) modulus intersected. Frequency sweeps were performed by incrementing the oscillating frequency from 0.1 to 100 rad/s at a constant strain of 0.1%. This strain was determined to be within the linear viscoelastic region of the strain sweeps for both MaSm and MaRg colony-biofilms.
Theoretical mucociliary clearance index (MCI) and cough clearance index (CCI), developed from in vitro models of mucus clearance32,33, were calculated according to Eqs. (2) and (3), respectively, using the relationship between the complex modulus (G*) and tanδ values determined from frequency sweep measurements21,22,53. The MCI and CCI was calculated from values determined at an angular frequency of 1 rad/s and 100 rad/s, respectively.
Statistical analysis
Data are presented as mean ± SD. Statistical significance was determined using either an One-way ANOVA with a Tukey’s post-hoc test or a Student’s t-test. Analyses were performed using GraphPad Prism v.7 (Graphpad Software). Statistical significance was determined using a p-value < 0.05.
Data availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).
References
Lam, J., Chan, R., Lam, K. & Costerton, J. W. Production of mucoid microcolonies by Pseudomonas aeruginosa within infected lungs in cystic fibrosis. Infect. Immun. 28, 546–556 (1980).
Singh, P. K. et al. Quorum-sensing signals indicate that cystic fibrosis lungs are infected with bacterial biofilms. Nature 407, 762–764. https://doi.org/10.1038/35037627 (2000).
Park, I. K. & Olivier, K. N. Seminars in Respiratory and Critical Care Medicine 217 (NIH Public Access).
Furukawa, B. S. & Flume, P. A. Seminars in Respiratory and Critical Care Medicine 383–391 (Thieme Medical Publishers, New York, 2018).
Foundation, C. F. Cystic Fibrosis Foundation Patient Registry; 2018 Annual Data Report. (Bethesda, Maryland, 2019).
Swenson, C., Zerbe, C. S. & Fennelly, K. Host variability in NTM disease: implications for research needs. Front. Microbiol. 9, 2901 (2018).
Floto, R. A. et al. Audit, research and guideline update: US Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus recommendations for the management of non-tuberculous mycobacteria in individuals with cystic fibrosis: executive summary. Thorax 71, 88 (2016).
Daniel-Wayman, S. et al. Advancing translational science for pulmonary nontuberculous mycobacterial infections. A road map for research. Am. J. Respir. Crit. Care Med. 199, 947–951 (2019).
Scott, J. P., Ji, Y., Kannan, M. & Wylam, M. E. Inhaled granulocyte–macrophage colony-stimulating factor for Mycobacterium abscessus in cystic fibrosis. Eur. Respir. J. 51, 1702127 (2018).
Wu, M.-L., Aziz, D. B., Dartois, V. & Dick, T. NTM drug discovery: status, gaps and the way forward. Drug Discov. Today 23, 1502–1519 (2018).
Clary, G. et al. Mycobacterium abscessus smooth and rough morphotypes form antimicrobial-tolerant biofilm phenotypes but are killed by acetic acid. Antimicrob. Agents Chemother. 62, e01782-e11717 (2018).
Rhoades, E. R. et al. Mycobacterium abscessus glycopeptidolipids mask underlying cell wall phosphatidyl-myo-inositol mannosides blocking induction of human macrophage TNF-α by preventing interaction with TLR2. J. Immunol. 183, 1997–2007 (2009).
Kolpen, M. et al. Biofilms of Mycobacterium abscessus complex can be sensitized to antibiotics by disaggregation and oxygenation. Antimicrob. Agents Chemother. 64, e01212 (2020).
Yam, Y.-K., Alvarez, N., Go, M.-L. & Dick, T. Extreme drug tolerance of Mycobacterium abscessus “Persisters”. Front. Microbiol. 11, 359 (2020).
Gloag, E. S., Fabbri, S., Wozniak, D. J. & Stoodley, P. Biofilm mechanics: Implications in infection and survival. Biofilm https://doi.org/10.1016/j.bioflm.2019.100017 (2019).
Branda, S. S., Vik, A., Friedman, L. & Kolter, R. Biofilms: the matrix revisited. Trends Microbiol. 13, 20–26 (2005).
Gloag, E. S., German, G. K., Stoodley, P. & Wozniak, D. J. Viscoelastic properties of Pseudomonas aeruginosa variant biofilms. Sci. Rep. 8, 9691. https://doi.org/10.1038/s41598-018-28009-5 (2018).
Kovach, K. et al. Evolutionary adaptations of biofilms infecting cystic fibrosis lungs promote mechanical toughness by adjusting polysaccharide production. Npj Biofilms Microbiomes 3, 1 (2017).
Peterson, B. W. et al. Viscoelasticity of biofilms and their recalcitrance to mechanical and chemical challenges. FEMS Microbiol. Rev. 39, 234–245 (2015).
Klapper, I., Rupp, C. J., Cargo, R., Purvedorj, B. & Stoodley, P. Viscoelastic fluid description of bacterial biofilm material properties. Biotechnol. Bioeng. 80, 289–296. https://doi.org/10.1002/bit.10376 (2002).
King, M. Relationship between mucus viscoelasticity and ciliary transport in guaran gel/frog palate model system. Biorheology 17, 249 (1980).
King, M., Brock, G. & Lundell, C. Clearance of mucus by simulated cough. J. Appl. Physiol. 58, 1776–1782 (1985).
Ciofu, O., Tolker-Nielsen, T., Jensen, P. O., Wang, H. & Hoiby, N. Antimicrobial resistance, respiratory tract infections and role of biofilms in lung infections in cystic fibrosis patients. Adv. Drug Deliv. Rev. 85, 7–23. https://doi.org/10.1016/j.addr.2014.11.017 (2015).
Howard, S. T. et al. Spontaneous reversion of Mycobacterium abscessus from a smooth to a rough morphotype is associated with reduced expression of glycopeptidolipid and reacquisition of an invasive phenotype. Microbiology (Reading, England) 152, 1581–1590 (2006).
Nessar, R., Reyrat, J.-M., Davidson, L. B. & Byrd, T. F. Deletion of the mmpL4b gene in the Mycobacterium abscessus glycopeptidolipid biosynthetic pathway results in loss of surface colonization capability, but enhanced ability to replicate in human macrophages and stimulate their innate immune response. Microbiology (Reading, England) 157, 1187–1195 (2011).
Devaraj, A. et al. The extracellular DNA lattice of bacterial biofilms is structurally related to Holliday junction recombination intermediates. Proc. Natl. Acad. Sci. USA 116, 25068–25077 (2019).
Rmaile, A. et al. Microbial tribology and disruption of dental plaque bacterial biofilms. Wear 306, 276–284 (2013).
Stoodley, P., Lewandowski, Z., Boyle, J. D. & Lappin-Scott, H. M. Structural deformation of bacterial biofilms caused by short-term fluctuations in fluid shear: an in situ investigation of biofilm rheology. Biotechnol. Bioeng. 65, 83–92 (1999).
Fabbri, S. et al. Streptococcus mutans biofilm transient viscoelastic fluid behaviour during high-velocity microsprays. J. Mech. Behav. Biomed. Mater. 59, 197–206 (2016).
Chen, Y., Norde, W., van der Mei, H. C. & Busscher, H. J. Bacterial cell surface deformation under external loading. mBio 3, e00378-e1312 (2012).
Ferry, J. D. Viscoelastic Properties of Polymers (Wiley, New York, 1980).
Grumbein, S., Opitz, M. & Lieleg, O. Selected metal ions protect Bacillus subtilis biofilms from erosion. Metallomics 6, 1441–1450 (2014).
Lieleg, O., Caldara, M., Baumgärtel, R. & Ribbeck, K. Mechanical robustness of Pseudomonas aeruginosa biofilms. Soft Matter 7, 3307–3314 (2011).
Pavlovsky, L., Younger, J. G. & Solomon, M. J. In situ rheology of Staphylococcus epidermidis bacterial biofilms. Soft Matter 9, 122–131. https://doi.org/10.1039/c2sm27005f (2013).
Wloka, M., Rehage, H., Flemming, H.-C. & Wingender, J. Structure and rheological behaviour of the extracellular polymeric substance network of mucoid Pseudomonas aeruginosa biofilms. Biofilms 2, 275–283 (2005).
Yan, J. et al. Bacterial biofilm material properties enable removal and transfer by capillary peeling. Adv. Mater. 30, 1804153 (2018).
Waters, M. S., Kundu, S., Lin, N. J. & Lin-Gibson, S. Microstructure and mechanical properties of in situ Streptococcus mutans biofilms. ACS Appl. Mater. Interfaces. 6, 327–332. https://doi.org/10.1021/am404344h (2014).
Cense, A. W. et al. Mechanical properties and failure of Streptococcus mutans biofilms, studied using a microindentation device. J. Microbiol. Methods 67, 463–472. https://doi.org/10.1016/j.mimet.2006.04.023 (2006).
Houari, A. et al. Rheology of biofilms formed at the surface of NF membranes in a drinking water production unit. Biofouling 24, 235–240. https://doi.org/10.1080/08927010802023764 (2008).
Di Stefano, A. et al. Viscoelastic properties of Staphylococcus aureus and Staphylococcus epidermidis mono-microbial biofilms. Microb. Biotechnol. 2, 634–641 (2009).
Rupp, C. J., Fux, C. A. & Stoodley, P. Viscoelasticity of Staphylococcus aureus biofilms in response to fluid shear allows resistance to detachment and facilitates rolling migration. Appl. Environ. Microbiol. 71, 2175–2178 (2005).
Marriott, C. Mucus and mucociliary clearance in the respiratory tract. Adv. Drug Deliv. Rev. 5, 19–35. https://doi.org/10.1016/0169-409X(90)90005-D (1990).
King, M. Interrelation between mechanical properties of mucus and mucociliary transport: Effect of pharmacologic interventions. Biorheology 16, 57 (1979).
Voynow, J. A. & Rubin, B. K. Mucins, mucus, and sputum. Chest 135, 505–512. https://doi.org/10.1378/chest.08-0412 (2009).
King, M. The role of mucus viscoelasticity in cough clearance. Biorheology 24, 589–597 (1986).
Ma, J. T., Tang, C., Kang, L., Voynow, J. A. & Rubin, B. K. Cystic fibrosis sputum rheology correlates with both acute and longitudinal changes in lung function. Chest 154, 370–377 (2018).
Cipolla, D., Shekunov, B., Blanchard, J. & Hickey, A. Lipid-based carriers for pulmonary products: Preclinical development and case studies in humans. Adv. Drug Deliv. Rev. 75, 53–80 (2014).
Messiaen, A.-S., Forier, K., Nelis, H., Braeckmans, K. & Coenye, T. Transport of nanoparticles and tobramycin-loaded liposomes in Burkholderia cepacia complex biofilms. PLoS ONE 8, e79220 (2013).
Dong, D. et al. Distribution and inhibition of liposomes on Staphylococcus aureus and Pseudomonas aeruginosa biofilm. PLoS ONE 10, e0131806 (2015).
Jones, W. L., Sutton, M. P., McKittrick, L. & Stewart, P. S. Chemical and antimicrobial treatments change the viscoelastic properties of bacterial biofilms. Biofouling 27, 207–215. https://doi.org/10.1080/08927014.2011.554977 (2011).
Schindelin, J. et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 9, 676 (2012).
Timoshenko, S. & Goodier, J. Theory of Elasticity 3rd edn. (McGraw Hill Higher Education, New York, 1970).
Zayas, J. G., Man, G. C. & King, M. Tracheal mucus rheology in patients undergoing diagnostic bronchoscopy. Am. Rev. Respir. Dis. 141, 1107–1113 (1990).
Dasgupta, B. & King, M. Reduction in viscoelasticity in cystic fibrosis sputum in vitro using combined treatment with nacystelyn and rhDNase. Pediatr. Pulmonol. 22, 161–166. https://doi.org/10.1002/(sici)1099-0496(199609)22:3 (1996).
Acknowledgements
Funding to LHS was provided by the Ohio State University College of Medicine Office of Research Bridge Funding Program and by the Cystic Fibrosis Foundation (HALLST18I0). ESG was funded by an American Heart Association Career Development Award (19CDA34630005). DJW and PS were funded by the National Institute of Health (R01AI134895 and R01AI143916; DJW) (R01GM124436; PS).
Author information
Authors and Affiliations
Contributions
E.S.G. and L.H.S. developed the hypothesis, designed the study, and performed the experiments. E.S.G., L.H.S. and P.S. performed the data analysis and interpretation. E.S.G., L.H.S., D.J.W. and P.S. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gloag, E.S., Wozniak, D.J., Stoodley, P. et al. Mycobacterium abscessus biofilms have viscoelastic properties which may contribute to their recalcitrance in chronic pulmonary infections. Sci Rep 11, 5020 (2021). https://doi.org/10.1038/s41598-021-84525-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84525-x
This article is cited by
-
A review of bacterial biofilm formation and growth: rheological characterization, techniques, and applications
Korea-Australia Rheology Journal (2023)
-
Omadacycline for management of Mycobacterium abscessus infections: a review of its effectiveness, place in therapy, and considerations for use
BMC Infectious Diseases (2022)
-
The biofilm life cycle: expanding the conceptual model of biofilm formation
Nature Reviews Microbiology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.