Abstract
Spinal postural variability (SPV) is a prerequisite to prevent musculoskeletal complaints during functional tasks. Our objective was to evaluate SPV in cervicogenic headache (CeH) since CeH is characterized by such complaints. A non-randomized repeated-measure design was applied to compare SPV between 18 participants with reporting CeH aged 29–51 years, and 18 matched controls aged 26–52 years during a 30-min-laptop-task. Habitual spinal postures (degrees) of the cervical, thoracic and lumbar spine were analysed using 3D-Vicon motion analysis. SPV, to express variation in mean habitual spinal posture, was deducted from the postural analysis. Mean SPV of each spinal segment was lower in the CeH-group compared to the control-group. Within the CeH-group, SPV of all except one spinal segment (lower-lumbar) was higher compared to the group’s mean SPV. Within the control-group, SPV was more comparable to the group’s mean SPV. SPV differed between groups. Averaging data resulted in decreased SPV in the CeH-group compared to the control-group during the laptop-task. However, the higher within-group-SPV in the CeH-group compared to the group’s mean SPV accentuated more postural heterogeneity. It should be further determined if addressing individual SPV is a relevant intervention.
Similar content being viewed by others
Introduction
Motor variability refers to variation in postures, movements and muscle activity needed for adaptation1, 2. According to the Neuronal Group Selection Theory, primary and secondary motor variability are characteristics of normal motor development3. Primary variability means that during human development the nervous system explores a wide range of motor possibilities, which causes an enormous non-adaptive variation in motor behaviour4, 5. Secondary or adaptive variability, i.e. selection of motor behaviour which fits best the situation based on afferent information produced by behaviour and experience, is important to adapt motor behaviour to the task1, 3, 5. Such adaptive variability is hypothesized to fulfil a beneficial role in preventing development of overuse injuries and pain2. Low motor variability or stereotypical motor behaviour is related to overuse of tissue, which can progress towards peripheral maladaptation such as reduced capillary-to-fibre ratio and mitochondrial disturbance6. These processes can facilitate development of musculoskeletal disorders (MSDs) and pain2, 6.
The cost of for instance work-related upper-limb MSDs has been estimated to amount between 0.5 and 2% of the country’s Gross National Product7. According to the European Agency for Safety and Health at Work (2019), MSDs and exposure to their risk factors (e.g. sedentary behaviour, screen time, psychosocial risk factors) are still increasing8.
Within this context, it might be relevant to draw attention to musculoskeletal complaints in cervicogenic headache (CeH). Prevalence of musculoskeletal complaints, such as observed in CeH, increase when daily computer use exceeds 3 h9, 10. These complaints are presumed to be related to the rather static habitual slumped sitting posture, characterized by posterior pelvic rotation, thoracic flexion, and especially forward head posture (FHP), during laptop- and desktop-computer use11, 12. An increased load on cervical musculoskeletal structures caused by the pronounced FHP might be a possible link with the development and persistence of CeH13, 14.
Cervical spine, its structures, and CeH are neuro-anatomically related through the trigemino-cervical complex (TCC)15. Its pars caudalis receives first-order nociceptive Aδ and C afferents of the ophthalmic part of the trigeminal nerve together with first-order Aδ and C nociceptive afferents from mostly the C2 dorsal nerve root. Nociceptive inputs from the ophthalmic and C2 nerve root overlap in the TCC. Convergence of trigeminal and cervical Aδ and C fibres on the C1-C2 dorsal horn provides a neuro-anatomical base for referred pain; pain originating from the neck is perceived as headache and vice versa16, 17.
Any persisted posture (e.g. FHP) with insufficient variation is a risk factor to develop a painful condition18, 19. As a consequence, it might be hypothesized that decreased cervical spinal postural variability (SPV), due to stereotypical motor behaviour and maintaining a posture2, 7, 20, might contribute to episodic CeH. However, since the lumbar and cervical spine move jointly in opposite directions during sitting12, it seems relevant to look beyond the cervical spine when analysing postural variability. A study by Caneiro et al. (2010) revealed that three defined thoraco-lumbar sitting postures resulted in variations of muscle activation, head and neck kinematics. Slumped sitting for instance was associated with an increased cervical flexion and anterior translation of the head compared to upright sitting21. Such slumped thoraco-lumbar posture is assumed to indirectly stress the cervical spine and thereby activating the TCC. Further, based on the contemporary theory of motor adaptation to pain, patients suffering from a painful condition adopt a protective less variable posture, which may even occur in regions remote to the site of pain22, 23. Applied to episodic CeH, this implies that the adjacent thoracic and lumbar spine might freeze to protect the cervical spine. Nevertheless, such contra-productive motor behaviour can increase the cumulative load on cervical spinal structures24 and thereby activating the TCC.
Therefore, the main objective of this study was to evaluate if SPV differed between patients with episodic CeH and an asymptomatic matched control-group during a laptop-task. The study focussed on higher level aspects (i.e. kinematic models) of human movement behaviour since such analysis provides more realistic and applicable models to analyse complex multi-joint movements25.
Methodology
Design
Non-randomized longitudinal (repeated-measures) comparison of SPV between the episodic CeH-group and control-group during a 30-min-laptop-task.
Sample size
Sample size calculation was not performed to establish treatment-effect but rather to assess feasibility of evaluating SPV in the context of an exploratory study. Yet, an a priori sample size was estimated (G*Power 3.1.9.4, Kiel Germany). Based on repeated-measures at five time-points (F-test, between-factors) of the FHP (mean degrees and standard deviation) during a laptop-task, a total of 30 participants (15 participants per group, power 80%; α = 0.05) was required to detect a mean difference of 3.5° (± 1.3) in FHP between the headache-group and control-group26.
Participants
Participants for both the CeH-group and the control-group were recruited between January 2018 to August 2019. The neurological staff at the headache departments of the AZ Vesalius hospitals (Tongeren and Bilzen, Belgium) identified and referred participants meeting the study’s inclusion criteria for CeH (see below for details). Additionally, a general call was launched at the Hasselt University, Zuyd Hogeschool, and private practice of the principal researcher. These potential participants also had to be declared eligible by the neurologist. Potential participants for the control-group were recruited by convenience sampling, word-of-mouth advertising within the Zuyd Hogeschool, and in the personal network of the involved researcher (Appendix a).
Inclusion criteria for the CeH-group were: Dutch-speaking participants between 18 and 55 years, body mass index (BMI) between 18.5 and 24.9 kg/m2, diagnosed with secondary episodic CeH according to the International Classification of Headache Disorders 3 (ICHD)27 by a neurologist, minimum laptop-use of seven hours/week, normal cognitive capacity, headache provocation through manual unilateral posterior-anterior cervical pressure (Passive Accessory Intervertebral Movement) at the C0-C4 region by a manual physiotherapist.
Inclusion criteria for the control-group were: Dutch-speaking asymptomatic participants between 18 and 55 years, BMI between 18.5 and 24.9 kg/m2, minimum laptop-use of seven hours/week, normal cognitive capacity.
Exclusion criteria for both groups were: pregnancy, physiotherapy for head- or neck-related disorders in the past month before the start of the study, serious pathology (musculoskeletal, neurological, endocrine, cardiovascular, psychiatric), comorbid headache, pain radiation to the arm(s), medication overuse (intake of non-steroid anti-inflammatory drugs, opioids, acetylsalicylic acid, triptans, simple analgesics for > 10 days/month > 3 months), smoking, history of neck/head trauma, orthodontics.
Nineteen participants were recruited and selected to compose the CeH-group (Appendix a). These participants were given a four-week headache-diary. The control-group was matched for age, gender, ethnicity and socio-economic status (level of education, job).
The current study is part of phase 1 of a larger project which is registered as an observational study at ClinicalTrials.gov (NCT02887638). The Medisch Ethische ToetsingsCommissie of Zuyderland and Zuyd Hogeschool (NL. 55720.09615) and the Comité Medische Ethiek of the Ziekenhuis Oost-Limburg (B371201423025) granted approval to execute the experimental protocol. Eligible participants had to read and sign the informed consent before officially being enrolled. Protection of personal data is legally determined by the Belgian law of December 8th 1992. All test procedures involving human participants were in accordance with the ethical standards of the institutional research committees and with the 1964 Helsinki Declaration and its later amendments. An informed consent was obtained from the participant in Fig. 1 for publication of the identifying image.
Measurements, outcomes and instruments
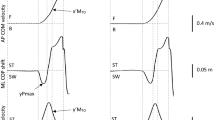
Primary outcomes. Habitual spinal postures (= the position of the spine, expressed via degrees, °) of the upper- and lower-cervical (UCx, LCx), thoracic (UTx, LTx), and lumbar (ULx, LLx) spine were evaluated with a 3D-Vicon motion analysis system (Vicon Motion Systems Ltd., Oxford, UK) and Nexus 2.1.1 software (recording, data acquisition, storage, gap filling) during the 30-min-laptop-task28, 29. The accuracy of the system is < 1° and < 1.5° root mean square in static and dynamic angular measurements, respectively30. SPV of each spinal posture, expressed by the standard deviation (SD), was deducted from the postural measurements of the habitual spinal posture during the 30-min-laptop-task. SPV expresses variation in the mean habitual spinal posture.
Secondary outcome
Headache-intensity pre and post laptop-task was measured using the 11-point Numeric Pain Rating Scale (NPRS) which ranges from 0 (no pain) to 10 (worst pain imaginable). Scores ≤ 3 correspond to mild, 4–6 to moderate, and ≥ 7 to severe pain. The meaningful clinically important change amounts to 2.5. Psychometric properties of the NPRS are solid31.
Data collection, processing and analysis
The principal researcher was responsible for the data collection. Motion analysis was performed via 12 infrared Bonita T10 and two video cameras at a sample rate of 100 Hz (low-pass Woltring filter)32. The biomechanical model, a custom labelling skeleton template, was created with Vicon Nexus and evaluated (2016–2017, Zuyd Hogeschool). This model was derived from numerous studies that examined human sitting posture33,34,35,36,37,38,39. Seven reflective markers were placed on the following anatomical landmarks to model the spine: left tragus and canthus, C7, T6, T12, L3 and S2 spinous processes. Data processing was conducted in Vicon Nexus 2.1.1. Processed trials were converted to pseudonymized c3d-files, exported to a custom developed data analysis programme (MATLAB R2019b, Natick, Massachusetts: The MathWorks Inc.), and converted to angles by an independent researcher.
Spinal posture was recorded each minute for five seconds during the 30-min-laptop-task. Angles were calculated based on the mean of the middle three seconds of the five second recording. Left sagittal angles were calculated for the: UCx, LCx, UTx, LTx, ULx, and LLx (Table 1, Fig. 1). SPV was deducted from these measurements.
Spinal angles were calculated based on following method, an example is given for angle \(\mathrm{\alpha }\)(UCx):
Let Canthus (Ca) be \(\left(\begin{array}{c}{\mathrm{x}}_{\mathrm{ca}}\\ {\mathrm{y}}_{\mathrm{ca}}\\ {\mathrm{z}}_{\mathrm{ca}}\end{array}\right)\), Tragus (Tr) \(\left(\begin{array}{c}{\mathrm{x}}_{\mathrm{tr}}\\ {\mathrm{y}}_{\mathrm{tr}}\\ {\mathrm{z}}_{\mathrm{tr}}\end{array}\right)\) and Vertical (V) \(\left(\begin{array}{c}0\\ 0\\ 1\end{array}\right)\), then vector TrCa is \(\left(\begin{array}{c}{\mathrm{x}}_{\mathrm{tr}}-{\mathrm{x}}_{\mathrm{ca}}\\ {\mathrm{y}}_{\mathrm{tr}}-{\mathrm{y}}_{\mathrm{ca}}\\ {\mathrm{z}}_{\mathrm{tr}}-{\mathrm{z}}_{\mathrm{ca}}\end{array}\right)\). Now \(\mathrm{\alpha }\) can be calculated using Eq. (1).
with \(\Vert a\Vert =\sqrt{{x}_{a}^{2}+{y}_{a}^{2}+{z}_{a}^{2}}\).
Procedure
Marker placement and static calibration
Concerning the CeH-group, a condition to be measured was a score of < 3 on the 11-point NPRS for headache-intensity on the test day22. Participants were asked not to take analgesics, muscle relaxants, and caffeine-containing beverages 24 h prior to the measurements. Prophylactic treatment(s) remained unchanged. Measurements were performed in a real-life set-up with a constant room temperature of 25° Celsius at the motion laboratory of Zuyd Hogeschool (Heerlen, The Netherlands). A static calibration of the sitting posture was performed for each participant before testing started. During the calibration participants were seated on a desk chair without back support, both feet on the floor, upper legs horizontal, lower legs vertical, feet parallel and shoulder width apart on the ground, arms uncrossed on thighs (Fig. 1)33, 40, 41. After degreasing the skin, anatomical landmarks were located by manual palpation, and marked by an experienced (> 10 years) manual therapist (= principal researcher). The most prominent bony anatomical landmarks were selected to limit soft tissue artefacts. Next, reflective markers were fixed on the skin using double-sided adhesive tape at the previously described anatomical landmarks33,34,35,36,37,38,39. Individual spinal postures were expressed relative to their static sitting posture. The principal researcher performed the test procedure for both the CeH-group and control-group.
Workstation setup
The capture volume of the Vicon system was 15 m2. A standard desk (height 74 cm; depth 80 cm; width 120 cm) (Bureau voor Normalisatie NBN-EN527) with laptop (HP ProBook 650 or HP EliteBook 6470b) and a height-adjustable office chair without back rest were placed in the centre of the capture volume42, 43. The position of the laptop, inclination of the screen and position of the chair referred to the ground could be individually adjusted44. The position of the setup had to ensure visibility of each marker by at least two infrared cameras.
Test procedure
Participants were asked to ‘sit as you normally do’. No further instructions, nor feedback was given45. Hereafter a 35-min customized laptop-task was performed. Posture was not recorded throughout the first five minutes to familiarize the participant with the work station46,47,48. During the 30-min-laptop-task the habitual spinal posture was recorded for five seconds every minute34, 49, 50, the first measurement was defined as ‘t0’. SPV was deducted from these measurements.
For the customized laptop-task the most common on- and offline laptop activities were selected (browsing, editing and typing). Participants completed nine standardised questions (Microsoft Office Word 2016), four questions accentuated typing words and numbers through open questions, five questions required an internet-search (Google Chrome or Mozilla Firefox), the use of a computer-mouse was not allowed51. Headache-intensity was questioned (NPRS) pre and post laptop-task.
The test procedure was executed and guided by the principal researcher.
Statistics
Analysis was done via JMP Pro 14 and SAS 9.4. Two-tailed tests at 5% level of significance were reported.
Demographics and group characteristics at baseline
Unpaired t-tests or non-parametric Mann–Whitney Tests, depending on the conditions (normality and equality of variances), were used to compare continuous variables. Contingency tables (Fisher’s exact test) were composed to compared distributions of categorical variables (proportions) between groups.
Mean habitual spinal angles (degrees) at t0 and during the 30-min-laptop-task were presented as means (SD). Linear mixed models for repeated measures were built based on the lowest root-mean-square error, with dependent variables (angles), fixed (time, baseline, group, headache-intensity), random (individual, time) effects, and an autoregressive covariance structure [AR(1)]: Yij = β0 + β1X1ij + … + βkXkij + μi + εij (Appendix b, Eq. b.1).
(a) Between-group-variability or mean variability at t0 was deducted from the random-intercept of the mixed model and expressed by the SD (= √variance). Mean angles (degrees) and variability of each spinal posture were compared between groups by adding a fixed group effect to the mixed model.
(b) Within-group-variability (i.e. residual variability during the laptop-task) was computed from the squares of the difference between each individual value and the mean value of the group that this individual value has come from. Within-group-variability was additionally used to compare UCx vs. LCx, UTx vs. LTx, and ULx vs. LLx variability.
(c) Intraclass correlation coefficients (ICCs) were calculated to estimate how strongly individuals in the same group (i.e. CeH-group and control-group) resemble each other. ICCs were calculated of the repeated-measurements (30 time-points) of each spinal posture. A 2-way mixed-effects model was composed (fixed effect: time, random effect: individual)52. ICCs were interpreted according to Portney et al. (2000): values < 0.50 are indicative of poor, values between 0.50 and 0.75 of moderate, values between 0.75 and 0.90 of good, and values > 0.90 of excellent reliability53.
(d) Influence of headache-intensity (NPRS) on SPV was analysed by comparing the random-intercepts (= variance) of each spinal angle between a mixed model with post-laptop-task headache-intensity (independent variable) and a mixed model without post-laptop-task headache-intensity (Appendix d, Table d.2). Only the post-laptop-task headache-intensity was included, since at baseline a condition to participate was NPRS < 3.
Mean (SD) headache-intensity (NPRS) was compared pre and post the laptop-task by using the non-parametric Wilcoxon signed-rank test. Effect sizes (ES) to quantify differences in change of headache-intensity from pre- to post-laptop-task were reported and interpreted as follows: ≤ 0.10 small, 0.21 to 0.29 medium, 0.30 to 0.49 large, ≥ 0.70 very large ES54.
Relations between the independent variables age, BMI, their interaction (continuous), socioeconomic status (categorical), and postural variables UCx, LCx, UTx, LTx, ULx, and LLx angles (dependent continuous) were evaluated via multiple linear regression: Yi = β0 + β1Xi1 + β2Xi2 + β3Xi1Xi2 + … + βkXik + εi (Appendix b, Eq. b.2). Conditions to apply linear models had to be met.
Results
Demographics and group characteristics
Demographics and group characteristics were comparable between groups, excluding headache characteristics (Table 2). One patient in the CeH-group (h,9) had to be excluded from the data-set because of technical artefacts. Age, BMI, their interaction, level of education, and employment did not significantly influence habitual spinal posture or SPV (Appendix c).
Does spinal postural variability differ between patients with episodic CeH and controls (Table 3, Fig. 2, Appendix d)?
Habitual spinal posture
Figure 3 visualises habitual spinal postural behaviour of the UCx, LCx, UTx, LTx, ULx, and LLx per minute during the 30-min-laptop-task in the CeH-group (grey) and the control-group (black). The evolution of these habitual spinal postures was rather linear in both groups (time-effect p > 0.05), meaning that time did not influence these postures. Further, none of the six habitual spinal postures differed between the CeH-group and the control-group at t0 and during the 30-min-laptop-task.
Spinal postural variability (SPV)
The mean SPV differed between the CeH-group and control-group at t0 as can be deducted from variability in intercept at t0. This difference was consistent during the 30-min-laptop-task.
Within the CeH-group, SPV (quantified by residual variability during 30 measurements) was higher compared to the group’s mean SPV, except for LLx. Concerning upper- vs. lower-spinal variability, UCx- and ULx-variability were lower compared to LCx- and LLx-variability, respectively, and UTx-variability was higher compared to LTx-variability.
ICCs ranged between 0.24 and 0.77, indicating poor to good resemblance of individual SPV in the CeH-group.
Within the control-group, SPV was more comparable to the group’s mean SPV. Concerning upper- vs. lower-spinal variability, UCx-, UTx-, and ULx-variability were lower compared to LCx-, LTx-, and LLx-variability respectively.
ICCs ranged between 0.81 and 0.99, indicating good to excellent resemblance of individual SPV in the control-group.
Does headache-intensity increase after the laptop-task?
Mean headache-intensity (SD) was significantly (p < 0.0001, ES 0.89) higher post laptop-task [NPRS 3.6 (2.1)] compared to pre [NPRS 0.7 (1)] in the CeH-group (Table 2). This difference is larger than the minimal clinical meaningful difference of 2.531.
Pain did not significantly influence UCx (p 0.63), LCx (p 0.55), UTx (p 0.87), LTx (p 0.89), ULx (p 0.61), and LLx (p = 0.85) SPV (Appendix c and d).
Discussion
Selection of the most adaptive postural adjustment to a task or perturbation characterizes adaptive variability4, 5, 55. However, if such variability fails, MSDs, as observed in episodic CeH, can develop1, 2, 17, 18, 56. Therefore, the objective of our study was to evaluate SPV in patients with episodic CeH compared to controls.
Looking beyond static cervical spinal posture in patients with cervicogenic headache: spinal postural variability
In this study, mean habitual spinal postures (= the position of the spine) did not differ between the CeH-group and the control-group, nor did such postures change during the 30-min-laptop-task within each group.
Spinal postures are often used as measurement variable to define the ideal or neutral sitting posture, in which spinal structures are minimally stressed57. However, to date, there still is no consensus on the definition of the ideal sitting posture35, 58 and attention is shifting toward analysing SPV in the specific context of MSDs56, 59, 60.
SPV, i.e. variation in the mean habitual spinal posture which clinically implies postural adjustments in the motor constituents of a task, is important for adaptation to the task demands1. Constrained postures with insufficient variation are risk factors to generate MSDs17, 18. Therefore, increasing postural variation to decrease biomechanical workload is currently the most suggested preventive intervention for the development of such MSDs61.
Several measurement variables can be used to express SPV. Counting the frequency of postural change approaches the time-domain, sampling entropy the complexity of time-series data, evaluating ranges or variance (and the derived SD) the magnitude of SPV61,62,63. We used the SD as main measure to estimate SPV since mean spinal postures were not subject to a time-effect.
Besides determining the most appropriate measurement variable we encountered a second methodological issue when analysing SPV. Comparing the mean SPV between-groups might be misleading since it could mask individual differences. Several authors stress the need to address differences between individuals, and not between groups, since individuals performing an identical task, use different motor patterns2.
Thus, although it seems relevant to analyse SPV in case of MSDs, such variability needs to be explored further.
Spinal postural variability elucidated
What would have been concluded based on this study if we only had analysed differences in the mean SPV between the CeH-group and control-group?
In our study, the mean SPV of the upper- and lower-cervical, upper- and lower-thoracic, and upper- and lower-lumbar spine was smaller in the CeH-group compared to the control-group, both at t0 and during the laptop-task. Such postural behaviour might be a protective strategy, consistent with the contemporary theory of motor adaptations to pain22. The latter suggests that pain has a general aim to protect the painful or threatened part of the body from real or impending pain by constraining movement. Such adaptations may even occur in regions remote to the site of pain22 as was shown by Falla et al. (2017)64. In that study participants with neck pain walked with a stiffer (i.e. decreased rotation) trunk. Applied to our results, this theory might imply that patients with episodic CeH want to protect their cervical spine by additionally stiffening the adjacent thoracic and lumbar region. Although decreasing SPV might be successful at short-term, at long-term (i.e. being unable to recapture variability) such behaviour is contra-productive. A minimum degree of SPV creates variation in joint load, muscle activity, and ligament stress as was postulated by the ‘variability-overuse hypothesis’22,23,24, 65.
Based on the lower cervical, thoracic and lumbar mean SPV in the CeH-group during the laptop-task, a cumulative load on the upper-cervical spine might activate the final common pathway (i.e. trigeminocervical nucleus caudatus) to CeH66.
Although our findings might give the impression that future research should build on a general decreased SPV in episodic CeH, by averaging and only reporting data on group level important postural information might be missed. It is for instance not possible to differentiate between extremes in SPV or detect specific patterns within a group67. In general, it is presumed that increased postural variability is a healthier state while decreased postural variability is related to MSDs. It should however be kept in mind that ‘too much’ postural variability can also result in overuse-injuries56. Finding a balanced SPV might reflect an individual’s self-regulatory capacity to function in an optimal individual range of postural variability. Within such optimum the window of adaptive postural variability should be determined to prevent overuse-injuries from developing56.
This hypothesis is deducted from the process of homeostasis: ‘the processes whereby the internal environment of an organism tends to remain balanced and stable’68, critical to the sustainability of living organisms68. Through feedback loops, systems are regulated and controlled to maintain the best state upon the influence of various disturbances. Variability is the key factor in sustainability, too much or little, or hyper- versus hypo-variability, could however be harmful69.
Therefore, we propose to further explore SPV within the CeH-group. Based on our results, we cannot assume that each participant with episodic CeH used an identical motor strategy, which was— at group level – a decreased SPV. Results in the CeH-group concerning within-group-variability (i.e. difference in variability caused by differences within one group) and ICC point in the direction of more heterogeneity within the CeH-group compared to the control-group. Such findings are consistent with previous work in which it was stated that motor behaviour, as a response or anticipation to pain, is not always stereotypical or even predictable2.
Changes in motor behaviour are unique, and postural responses to pain can be highly variable between and probably within individuals22, 70, 71. More research is needed to determine if an individual range of optimal SPV exists, and if moving outside such range increases the risk of developing MSDs. This hypothesis supports the importance of an individual approach which already was accentuated by results of Srinivasan and Mathiassen (2012)2. From these findings it may be questioned whether individual differences in SPV could predict if someone is more susceptible to develop MSDs72. If SPV is a protective factor against the development of MSDs2, factors that determine such variability should be explored.
Upper vs. lower spinal postural variability
It seems relevant to further explore if differences between upper and lower SPV might contribute to or protect against CeH.
Differences in upper- and lower-cervical postural variability have been suggested as a strategy to minimize load on cervical structures73,74,75. Anatomical and physiological evidence suggest greater contribution to sensorimotor control of cervical afferents from the upper- compared to lower-cervical spine76, 77. Since sensorimotor control and pain are bi-directionally related, pain can be both cause or be the consequence of disturbed sensorimotor control. This disturbance has an adverse influence on feedback and feedforward motor control and regulation of muscle stiffness70.
Additionally, such differences between upper and lower SPV might be extended to the thoracic and lumbar spine since spinal movement during functional tasks is not confined to exclusive the cervical, thoracic or lumbar spine21. High inter-regional movement coordination between the cervical and upper-thoracic spine for instance supports such idea75. In our study, lower-cervical postural variability was higher compared to upper-cervical postural variability, and upper-thoracic postural variability higher compared to lower-thoracic postural variability in the CeH-group. However, more research is needed to determine if such finding can be related to development of headache. Analysing if SPV could be an outcome measure for a longitudinal interventional study seems a next future research step.
Headache-intensity versus spinal postural variability
An obvious association to explore would be the relation between pain and decreased SPV. Several authors support the hypothesis that decreased motor variability is the motor response of patients suffering from long-term pain conditions (e.g. low back pain, unilateral patella-femoral pain, spastic hemiplegic cerebral palsy) trying to limit their movement as a protective mechanism78,79,80,81. We, however, cannot confirm that headache was the main driver for our results since a condition to be measured was a score of < 3 on the 11-point NPRS. It should also be kept in mind that participants with CeH suffer from an episodic disorder, in contrast to long-term pain conditions in previous work78,79,80,81, and headache-intensity was only questioned at the start and end of the laptop-task, not during the task. Headache-intensity increased significantly (p < 0.0001, ES 0.89) after the laptop-task in the CeH-group, scores on the 11-point NPRS evolved from 0.7 (1) before to 3.6 (2.1) at the end. This difference is larger than the minimal clinical meaningful difference of 2.531.
While all individuals perform an identical activity with some degree of motor variability, the extent of such variability differs between individuals25, 72, 82. Such differences, even between individuals of a homogeneous (age, gender, body composition) group, can for instance be due to individual anatomical and physiological characteristics25. Further, also psychological characteristics seem to influence motor variability25.
In summary, if motor variability is a personal trait linked to episodic CeH, determinants of such variability should be further explored.
Limitations and suggestions
The current work is a first but essential step to explore SPV in patients with episodic CeH. No Bonferroni corrections were applied because of the explorative nature of our study. Therefore, and because of spectrum bias, results should be interpreted with caution. The small sample size (n=36) in this study is a limitation. Future research should consider larger cohorts..
SPV can be assessed at different levels. We used higher level aspects of movement performance (i.e. kinematic models). It seems advised to additionally add lower level aspects (i.e. muscle activation)25.
More outcomes, relevant in analysing motor variability, need to be explored (e.g. fatigue, anatomical, physiological and psychosocial individual characteristics).
Longitudinal research is further needed to analyse factors that might be associated with SPV within a biopsychosocial framework, and the direction of causality before this knowledge can be integrated into guidelines for evidence-based clinical practice for CeH. In a step wise future process, case–control (n = 1) studies83 could be the next step to accentuate the individual aspect of SPV Performing an identical measurement during a headache-attack would be an interesting future step which needs to be well designed. Standardizing an identical level of headacheintensity, because of variability, will be a challenge84.
Conclusion
The mean SPV was lower in the CeH-group compared to the control-group at t0 and during the laptop-task. However, the higher within-group-variability in the CeH-group as opposed to the group’s mean SPV accentuated the heterogeneous postural profile, and might indicate that SPV is a personal trait.
Abbreviations
- BMI:
-
Body mass index
- CeH:
-
Cervicogenic headache
- FHP:
-
Forward head posture
- ICC:
-
Intraclass correlation coefficient
- ICHD:
-
International Classification of Headache Disorders
- LCx:
-
Lower-cervical spine
- LLx:
-
Lower-lumbar spine
- LTx:
-
Lower-thoracic spine
- MSD:
-
Musculoskeletal disorder
- NPRS:
-
Numeric Pain Rating Scale
- SD:
-
Standard deviation
- SPV:
-
Spinal postural variability
- TCC:
-
Trigemino-cervical complex
- UCX:
-
Upper-cervical spine
- ULx:
-
Upper-lumbar spine
- UTX:
-
Upper-thoracic spine
References
Moseley, G. L. & Hodges, P. W. Reduced variability of postural strategy prevents normalization of motor changes induced by back pain: A risk factor for chronic trouble?. Behav. Neurosci. 120, 474–476 (2006).
Srinivasan, D. & Mathiassen, S. E. Motor variability in occupational health and performance. Clin. Biomech. 27, 979–993 (2012).
Edelman, G. M. Neural Darwinism the Theory of Neuronal Group Selection (Oxford University Press, 1989).
Hadders-Algra, M. The neuronal group selection theory: An attractive framework to explain variation in normal motor development. Dev. Med. Child Neurol. 42, 566–572 (2000).
Hadders-Algra, M. Variation and variability: Key words in human motor development. Phys. Ther. 90, 1823–1837 (2010).
Cote, J. N. A critical review on physical factors and functional characteristics that may explain a sex/gender difference in work-related neck/shoulder disorders. Ergonomics 55, 173–182 (2012).
European Occupational Diseases Statistics (EODS)—Phase 1 methodology. Eurostat working papers. Population and social conditions 3/2000/E/No 19. Reference metadata on occupational diseases, compiling agency: Statistical Office of the European Communities. http://epp.eurostat.ec.europa.eu/cache/ITY_SDDS/EN/hsw_occ_dis_esms.htm (2020).
European Agency for Safety and Health at Work. Summary. Work-related musculoskeletal disorders: prevalence, costs and demographics in the EU. https://osha.europa.eu/en/highlights/work-related-musculoskeletal-disorders-prevalence-costs-and-demographics (2020).
Nakazawa, T. et al. Association between duration of daily VDT use and subjective symptoms. Am. J. Ind. Med. 42, 421–426 (2002).
Westgaard, R. H. & Winkel, J. Guidelines for occupational musculoskeletal load as a basis for intervention: A critical review. Appl. Ergon. 27, 79–88 (1996).
Pooriput, W., Bala, R. & Prawit, J. Internal oblique and transversus abdominis muscle fatigue induced by slumped sitting posture after 1 hour of sitting in office workers. Saf. Health Work. 7, 49–54 (2016).
Black, K. M., McClure, P. & Polansky, M. The influence of different sitting positions on cervical and lumbar posture. Spine. 21, 65–70 (1996).
Patwardhan, A. G. et al. Postural consequences of cervical sagittal imbalance: A novel laboratory model. Spine. 40, 783–792 (2015).
Mingels, S., Dankaerts, W. & Granitzer, M. Is there support for the paradigm 'spinal posture as a trigger for episodic headache'? A comprehensive review. Curr. Pain Headache Rep. 23, 17, https://doi.org/10.1007/s11916-019-0756-2 (2019).
Castien, R. & De Hertogh, W. A neuroscience perspective of physical treatment of headache and neck pain. Front. Neurol. 10, 279, https://doi.org/10.3389/fneur.2019.00276 (2019).
Bogduk, N. Cervicogenic headache: Anatomic basis and pathophysiologic mechanisms. Curr. Pain Headache Rep. 5, 382–386 (2001).
Bogduk, N. The neck and headaches. Neurol. Clin. 32, 471–487 (2014).
Gerr, F., Monteilh, C. P. & Marcus, M. Keyboard use and musculoskeletal outcomes among computer users. J. Occup. Rehabil. 16, 265–277 (2006).
Gerr, F., Marcus, M., Ensor, C., Kleinbaum, D. & Cohen, S. A. E. A prospective study of computer users: I. Study design and incidence of musculoskeletal symptoms and disorders. Am. J. Ind. Med. 41, 221–235 (2002).
Nordander, C. et al. Risk of musculoskeletal disorders among females and males in repetitive/constrained work. Ergonomics 52, 1226–1239 (2009).
Caneiro, J. P. et al. The influence of different sitting postures on head/neck posture and muscle activity. Man Ther. 15, 57–60 (2010).
Hodges, P. W. & Tucker, K. Moving differently in pain: A new theory to explain the adaptation to pain. Pain 152, S90–S98 (2011).
Hodges, P., van den Hoorn, W., Dawson, A. & Cholewicki, J. Changes in the mechanical properties of the trunk in low back pain may be associated with recurrence. J. Biomech. 42, 61–66 (2009).
Bartlett, R., Wheat, J. & Robins, M. Is movement variability important for sports biomechanists?. Sports Biomech. 6, 224–243 (2007).
Sandlund, J., Srinivasan, D., Heiden, M. & Mathiassen, S. E. Differences in motor variability among individuals performing a standardized short-cycle manual task. Hum. Mov. Sci. 51, 17–26 (2017).
Mingels, S., Dankaerts, W., van Etten, L., Thijs, H. & Granitzer, M. Comparative analysis of head-tilt and forward head position during laptop use between females with postural induced headache and healthy controls. J. Bodyw. Mov. Ther. 20, 533–541 (2016).
Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 38, 1–211 (2018).
Ehara, Y., Fujimoto, H., Miyakazi, S., Tanaka, S. & Yamamoto, S. Comparison of the performance of 3D camera systems. Gait Posture. 3, 166–169 (1995).
Ugbolue, U. C. et al. The evaluation of an inexpensive, 2D, video based gait assessment system for clinical use. Gait Posture. 38, 483–489 (2013).
Wong, W. Y. & Wong, M. S. Trunk posture monitoring with inertial sensors. Eur Spine J. 17, 743–753 (2008).
Young, I. A., Dunning, J., Butts, R., Cleland, J. A. & Fernández-de-Las-Peñas, C. Psychometric properties of the Numeric Pain Rating Scale and Neck Disability Index in patients with cervicogenic headache. Cephalalgia 39, 44–51 (2019).
Woltring, H. J. A FORTAN package for generalized cross-validatory spline smoothing and differentiation. Adv. Eng. Softw. 8, 104–113 (1986).
Richards, K. V., Beales, D. J., Smith, A. J., O’Sullivan, P. B. & Straker, L. M. Neck posture clusters and their association with psychosocial factors and neck pain in Australian adolescents. Phys. Ther. 96, 1576–1587 (2016).
Porto, A. B., Quirino, C. M., Moura, T. B., Faquin, B. S. & Okazaki, V. H. A. Interrater Reliability in Thoracic and Lumbar Angles Analysis Using Photogrammetry (XXIV Congress of the International Society of Biomechanics, XXV Brazilian Congress of Biomechanics, 2013).
Dankaerts, W., O’Sullivan, P., Burnett, A. & Straker, L. Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine. 31, 698–704 (2006).
Claus, A. P., Hides, J. A., Moseley, G. L. & Hodges, P. W. Is “ideal” sitting posture real? Measurement of spinal curves in four sitting postures. Man Ther. 14, 404–408 (2009).
Claus, A. P., Hides, J. A., Moseley, G. L. & Hodges, P. W. Thoracic and lumbar posture behaviour in sitting tasks and standing: Progressing the biomechanics from observations to measurements. Appl Ergon. 53, 161–168 (2016).
Edmondston, S. J. et al. Thoracic spine extension mobility in young adults: Influence of subject position and spinal curvature. J. Orthop. Sports Phys. Ther. 41, 266–273 (2011).
Claeys, K., Brumagne, S., Deklerck, J., Vanderhaeghen, J. & Dankaerts, W. Sagittal evaluation of usual standing and sitting spinal posture. J. Bodyw. Mov. Ther. 20, 326–333 (2016).
O’Sullivan, K. et al. Neutral lumbar spine sitting posture in pain-free subjects. Man Ther. 15, 557–561 (2010).
Korakakis, V., Giakas, G., Sideris, V. & Whiteley, R. Repeated end range spinal movement while seated abolishes the proprioceptive deficit induced by prolonged flexed sitting posture. A study assessing the statistical and clinical significance of spinal position sense. Musculoskelet. Sci. Pract. 31, 9–20 (2017).
Aurand, A. M., Dufour, J. S. & Marras, W. S. Accuracy map of an optical motion capture system with 42 or 21 cameras in a large measurement volume. J. Biomech. 58, 237–240 (2017).
Maletsky, L. P., Sun, J. & Morton, N. A. Accuracy of an optical active-marker system to track the relative motion of rigid bodies. J. Biomech. 40, 682–685 (2007).
Moffet, H., Hagberg, M., Hansson-Risberg, E. & Karlqvist, L. Influence of laptop computer design and working position on physical exposure variables. Clin. Biomech. 17, 368–375 (2002).
Edmondston, S. J. et al. Postural neck pain: An investigation of habitual sitting posture, perception of “good” posture and cervicothoracic kinaesthesia. Man Ther. 12, 363–371 (2007).
Villanueva, M. B., Jonai, H. & Saito, S. Ergonomic aspects of portable personal computers with flat panel displays (PC-FPDs): Evaluation of posture, muscle activities, discomfort and performance. Ind. Health. 36, 282–289 (1998).
Szeto, G. P. & Lee, R. An ergonomic evaluation comparing desktop, notebook, and subnotebook computers. Arch. Phys. Med. Rehabil. 83, 527–532 (2002).
Brink, Y., Louw, Q., Grimmer, K. & Jordaan, E. The spinal posture of computing adolescents in a real-life setting. BMC Musculoskelet. Disord. 15, 212, https://doi.org/10.1186/1471-2474-15-212 (2014).
Burnett, A. et al. An examination of the flexion-relaxation phenomenon in the cervical spine in lumbo-pelvic sitting. J. Electromyogr. Kinesiol. 19, 229–236 (2009).
Nairn, B. C., Chisholm, S. R. & Drake, J. D. What is slumped sitting? A kinematic and electromyographical evaluation. Man Ther. 18, 498–505 (2013).
Dennerlein, J. T. & Johnson, P. W. Different computer tasks affect the exposure of the upper extremity to biomechanical risk factors. Ergonomics 49, 45–61 (2006).
Shrout, P. E. & Fleiss, J. L. Intraclass correlations: Uses in assessing rater reliability. Ref. Psychol. Bull. 86, 420–428 (1979).
Portney, L. G. & Watkins, M. P. Foundations of Clinical Research: Applications to Practice (F.A Davis Company, Philadelphia, 2015).
Rosenthal, J. A. Qualitative descriptors of strength of association and effect size. J. Soc. Serv. 21, 37–59 (1996).
Hadders-Algra, M. Early human motor development: From variation to the ability to vary and adapt. Neurosci Biobehav Rev. 90, 411–427 (2018).
Hamill, J., Palmer, C. & Van Emmerik, R. E. Coordinative variability and overuse injury. Sports Med. Arthrosc. Rehabil. Ther. Technol. 4, 45, https://doi.org/10.1186/1758-2555-4-45 (2012).
Corlett, E. N. Background to sitting at work: Research-based requirements for the design of work seats. Ergonomics 49, 1538–1546 (2006).
O’Sullivan, K., O’Sullivan, P., O’Sullivan, L. & Dankaerts, W. What do physiotherapists consider to be the best sitting spinal posture?. Man Ther. 17, 432–437 (2012).
Madeleine, P. Dynamics of seated computer work before and after prolonged constrained sitting. J. Appl. Biomech. 28, 297–3030 (2012).
Vergara, M. & Page, A. Relationship between comfort and back posture and mobility in sitting-posture. Appl. Ergon. 33, 1–8 (2002).
Mathiassen, S. E. Diversity and variation in biomechanical exposure: What is it, and why would we like to know?. Appl. Ergon. 37, 419–427 (2006).
Stergiou, N. Innovative Analysis of Human Movement. (ed. Stergiou, N) (Human Kinetics, 2004).
Richman, J. S. & Moorman, J. R. Physiological time-series analysis using approximate entropy and sample entropy. Am. J. Physiol. Heart Circ. Physiol. 278, 2039–2049 (2000).
Falla, D., Gizzi, L., Parsa, H., Dieterich, A. & Petzke, F. People with chronic neck pain walk with a stiffer spine. J. Orthop. Sports Phys. Ther. 47, 268–277 (2017).
Lomond, K. V. & Cote, J. N. Movement timing and reach to reach variability during a repetitive reaching task in persons with chronic neck/shoulder pain and healthy subjects. Exp. Brain Res. 206, 271–282 (2010).
Cady, R. K. The convergence hypothesis. Headache. 47, S44–S51 (2007).
Zeskind, P. S. & Huntington, L. The effects of within-group and between-group methodologies in the study of perceptions of infant crying. Child Dev. 55, 1658–1665 (1984).
National Center for Biotechnology Information. PubMed https://www.ncbi.nlm.nih.gov/mesh/68006706 (2020).
Wright, T., Twaddle, J., Humphries, C., Hayes, S. & Kim, E. J. Variability and degradation of homeostasis in self-sustained oscillators. Math. Biosci. 273, 57–59 (2016).
Hodges, P. W., Moseley, G. L., Gabrielsson, A. & Gandevia, S. C. Experimental muscle pain changes feedforward postural responses of the trunk muscles. Exp. Brain Res. 151, 262–271 (2003).
van Dieen, J. H., Selen, L. P. & Cholewicki, J. Trunk muscle activation in low-back pain patients: An analysis of the literature. J. Electromyogr. Kinesiol. 13, 333–351 (2003).
Mathiassen, S. E., Moller, T. & Forsman, M. Variability in mechanical exposure within and between individuals performing a highly constrained industrial work task. Ergonomics 46, 800–824 (2003).
Straker, L., Skoss, R., Burnett, A. & Burgess-Limerick, R. Effect of visual display height on modelled upper and lower cervical gravitational moment, muscle capacity and relative strain. Ergonomics 52, 204–221 (2009).
Patwardhan, A. G. et al. Cervical sagittal balance: A biomechanical perspective can help clinical practice. Eur. Spine J. 27, 25–38 (2018).
Tsang, S. M., Szeto, G. P. & Lee, R. Y. Normal kinematics of the neck: The interplay between the cervical and thoracic spines. Man Ther. 18, 431–437 (2013).
Kulkarni, V., Chandy, M. & Babu, K. Quantitative study of muscle spindles in suboccipital muscles of human foetuses. Neurol. India. 49, 355–359 (2001).
Boyd Clark, L., Briggs, C. & Galea, M. Muscle spindle distribution, morphology, and density in the longis colli and multifidus muscles of the cervical spine. Spine. 27, 694–701 (2002).
Heiderscheit, B. C., Hamill, J. & van Emmerik, R. E. A. Variability of stride characteristics and joint coordination among individuals with unilateral patellofemoral pain. J. Appl. Biomech. 18, 110–121 (2002).
Georgoulis, A. D., Moraiti, C., Ristanis, S. & Stergiou, N. A novel approach to measure variability in the anterior cruciate ligament deficient knee during walking: the use of the approximate entropy in orthopaedics. J. Clin. Monit. Comput. 20, 11–18 (2006).
Jeng, S. F., Holt, K. G., Fetters, L. & Certo, C. Self-optimization of walking in nondisabled children and children with spastic hemiplegic cerebral palsy. J. Mot. Behav. 28, 15–27 (1996).
van den Hoorn, W., Bruijn, S. M., Meijer, O. G., Hodges, P. W. & van Dieen, J. H. Mechanical coupling between transverse plane pelvis and thorax rotations during gait is higher in people with low back pain. J. Biomech. 45, 342–347 (2012).
Srinivasan, D., Rudolfsson, T. & Mathiassen, S. E. Between- and within-subject variance of motor variability metrics in females performing repetitive upper-extremity precision work. J. Electromyogr. Kinesiol. 25, 121–129 (2015).
Tate, R. L. et al. Rating the methodological quality of single-subject designs and n-of-1 trials: Introducing the single-case experimental design (SCED) scale. Neuropsychol. Rehabil. 18, 385–401 (2008).
Madden, V. J., Kamerman, P. R., Catley, M. J., Bellan, V., Russek, L. N., Camfferman, D., & Lorimer Moseley, G. (2021). Variability in experimental pain studies: nuisance or opportunity?. British journal of anaesthesia, 126(2), e61–e64
Acknowledgements
The authors want to acknowledge Odekerken D, Diederen T and Koppert M for their technical support throughout the study.
Author information
Authors and Affiliations
Contributions
S.M., W.D., L.V.E., L.B. and M.G. conceived and planned the experiments. S.M. carried out the experiments and took the lead in writing the manuscript. W.D., L.V.E. and M.G. supervised and provided feedback throughout the entire research and writing phase. L.B. supported the data-analysis and provided statistical support.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mingels, S., Dankaerts, W., van Etten, L. et al. Lower spinal postural variability during laptop-work in subjects with cervicogenic headache compared to healthy controls. Sci Rep 11, 5159 (2021). https://doi.org/10.1038/s41598-021-84457-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84457-6
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.