Abstract
E-cigarettes are heavily advertised as healthier alternative to common tobacco cigarettes, leading more and more women to switch from regular cigarettes to ENDS (electronic nicotine delivery system) during pregnancy. While the noxious consequences of tobacco smoking during pregnancy on the offspring health are well-described, information on the long-term consequences due to maternal use of e-cigarettes do not exist so far. Therefore, we aimed to investigate how maternal e-nicotine influences offspring development from earliest life until adulthood. To this end, virgin female Drosophila melanogaster flies were exposed to nicotine vapor (8 µg nicotine) once per hour for a total of eight times. Following the last exposure, e-nicotine or sham exposed females were mated with non-exposed males. The F1-generation was then analyzed for viability, growth and airway structure. We demonstrate that maternal exposure to e-nicotine not only leads to reduced maternal fertility, but also negatively affects size and weight, as well as tracheal development of the F1-generation, lasting from embryonic stage until adulthood. These results not only underline the need for studies investigating the effects of maternal vaping on offspring health, but also propose our established model for analyzing molecular mechanisms and signaling pathways mediating these intergenerational changes.
Similar content being viewed by others
Introduction
Electronic cigarettes (e-cigarettes) have become increasingly popular and their use has increased worldwide. E-cigarettes are heavily advertised with the claim to support smoking cessation and as an healthier and safer alternative to regular tobacco cigarettes1,2,3. This marketing strategy obviously targets highly vulnerable populations such as adolescents and pregnant women1,4. The deleterious consequences of tobacco smoking during pregnancy on the future respiratory health of offspring are well-described5,6. In contrast, information on the long-term consequences on the biology and health of offspring effects and due to maternal use of e-cigarettes is still scarce7,8,9.
The only study currently available that collected questionnaire data on smoking and e-cigarettes in pregnant women10 suggests that the use of e-cigarettes during pregnancy in 248 women causes fetal growth restriction, which in turn is a proposed risk factor for impaired lung function development and respiratory hyper-reactivity11,12,13.
Beyond this report no other epidemiological investigations linking e-cigarette use during pregnancy to offspring health exist so far. In addition, the frequent dual use of tobacco and e-cigarettes complicates the interpretation of human studies4,14. Thus, misclassification due to reporting bias and the inability of objective markers such as cotinine or CYP1a1-expression to separate the sources of nicotine cannot be excluded with certainty10.
Delayed embryo implantation, reduced birth weight, increased neurodevelopmental vulnerability and vascular dysfunction in young offspring has been demonstrated in several mouse models of maternal e-cigarette use15,16,17,18,19. Further, it was shown that maternal e-cigarette exposure altered pulmonary global DNA methylation and cytokine expression in the offspring20 potentially increasing the risk for lung disease.
Although e-cigarettes lack tar and carbon monoxide gas21, fatal cases due to acute lung injury have been reported to the Center of Disease Control and Prevention (CDC). While tetrahydrocannabinol and Vitamin E acetate were suspected as causal agents, the liquids used in e-cigarettes contain nicotine22, heavy metals and other substances already known to be associated with adverse health effects23,24,25,26. Among these; acrolein, formaldehyde, and acetaldehyde, are examples with reported respiratory toxicity22,23,27,28,29,30,31. In addition, liquid nicotine can reach concentrations exceeding those of tobacco cigarettes32,33,34,35.
As the knowledge on the long-term effects of maternal vaping on offspring health is currently limited, we aimed to investigate in a first step how maternal e-nicotine influences offspring growth and development from earliest life until adulthood. In women and all mammalian model systems embryo-fetal development takes place inside the uterus. We therefore decided to use the fruit fly Drosophila melanogaster as they deliver embryos whose further development takes place outside of the females’ body. Therefore, this model facilitates tracking of maternal e-nicotine influence on the offspring from their earliest stages of development until adulthood in a sex-specific way, which simplifies intergenerational studies.
Materials and methods
Chemicals
Nicotine used for exposure, ( −)-Nicotine ≥ 99% (GC), was purchased from Sigma-Aldrich Chemie GmbH (Germany).
Drosophila strain and culture
Experiments were carried out with a wild type Drosophila melanogaster strain (Canton S). Virgin female flies were isolated under CO2 anesthesia 6 h post-eclosion. Flies were cultured on a standard cornmeal/molasses/yeast/agar medium and kept in 175 ml vials at a temperature of 25 °C and a relative humidity of 65% to 75% at a 12 h:12 h light:dark cycle. The flies were exposed to e-nicotine at the age of 5-days. All experiments were performed at room temperature (21–23 °C).
Nicotine exposure
A self-constructed e-nicotine-exposure system consisted of a 175 ml vial with a nylon mesh cloth inserted in the middle in order to divide the vial in half and to protect the animals from heat stress. The upper part was closed with a foam plug while the bottom part was connected to a coiled nichrome wire attached to a power supply (3.7 V, 1.9 A).
Virgin female flies were divided into e-nicotine-exposed and dH2O-control groups (100 flies/group). The flies were free of CO2-anaesthesia for 5-days prior to further manipulations. Briefly, 10 μl of nicotine (5 mM) or dH2O was pipetted on a nichrome coil which was heated for 15 s. Thereafter, the flies were allowed to rest in the exposure chamber for 2 min before being transferred back to their culture vials. The experiment was repeated once per hour for a total of 8 times. Next, e-nicotine-exposed and dH2O-control flies (100 flies per group) were transferred onto two individual grapefruit agar (GA) plates where they were mated with male flies of the same age.
Geotaxis assay
In order to determine the appropriate concentration of e-nicotine for further experiments, a negative geotaxis assay, for the detection of the flies’ locomotory behavior against gravity, was performed. Briefly, 100 age-matched female flies per treatment were divided into 10 flies/group and exposed to either dH2O (control) or 1 mM, 5 mM or 10 mM of nicotine. Thereafter, the flies from each group were transferred into 4 vials and gently tapped to the bottom of the column. The distance of 7 cm was marked on the vials and the number of flies (percentage) that were able to climb above the 7 cm mark by 10 s was recorded. The assay was repeated 3 times per group with 1 min rest between the repetitions.
Determination of oviposition
Eggs collected on (GA) plates within the first 10 h after mating were discarded and the new (GA) plates were placed into an egg collection cage. Eggs laid by treated and control groups were collected within the subsequent 2 h in order to produce synchronized embryos. Then, GA plates were washed with PBS and the eggs were poured into a 70 µl cell strainer for counting. Fecundity was characterized by the percentage of the total number of eggs observed 2 h after mating. Thereafter, eggs were transferred to standard medium and incubated as described above.
Egg morphology
The mean length of randomly selected eggs (100 eggs/experiment) deposited within 2 h after mating was estimated from the most proximal to the most distal point. Morphological measurements were taken using an OLYMPUS SZX16 stereomicroscope with Olympus cell-Sens Standard imaging software (Olympus cellSens Standard, Version 1.16, Olympus Corporation, Tokyo, Japan).
Survival rate
In order to determine the percentage of larvae hatching from the eggs and the percentage of pupae-to-eclosed adults, embryos were transferred into vials containing standard cornmeal diet food and allowed to develop into 1st-instar (L1) larvae. Each vial was plugged with cotton and maintained under conditions of controlled temperature (25 °C) and humidity (60%). After 24 h, cohorts of hatched F1 L1 larvae were counted under the OLYMPUS SZX16 stereomicroscope. In order to study the transgenerational effect of nicotine on the percentage of adult fly eclosion (the ratio of pupae-to-adult), we counted the number of emerged adults i.e. according to the number of pupae the percentage of eclosed adults was calculated in each group.
Determination of the size and weight of L1 and L3 generation
L1 and L3 larvae (20 larvae/experiment) were extracted from the vials 24 and 72 h, respectively, following egg deposition. Thereafter, the larvae were fixed in 70% ethanol, dried and then either weighed or placed on glass slides for further microscopic analysis. The measurement of the length of L1 and L3 larvae obtained from egg batches laid by e-nicotine- and water-exposed females was carried out from the most proximal to the most distal point of the body with an OLYMPUS SZX16 stereomicroscope using Olympus cell-Sens Standard imaging software (Olympus cellSens Standard, Version 1.16, Olympus Corporation, Tokyo, Japan). The weights of L3 larvae were recorded using Sartorius BP61-scale.
Tracheal length measurement
L3 larvae (10 to 15 flies) were removed from the medium with tweezers, washed in 1 × PBS and placed on a drop of glycerin on a slide. The slide was then placed on a heating plate at 70 °C for 10 s in order to kill the larvae. Thereafter, the larvae were aligned with the dorsal side facing upwards, covered with a cover-slip and analyzed with an Olympus SZX16 stereomicroscope using cell-Sens Standard imaging software (Olympus cellSens Standard, Version 1.16, Olympus Corporation, Tokyo, Japan). The third thoracic segment of the larvae was measured at a magnification of 20-fold. All images were scaled and saved as Tiff files. These microscopic images were then used to measure the length of secondary branches using ImageJ software (Version 2.1.4.7, Wayne Rasband National Institutes of Health, USA) with NeuronJ plugin (version 1.4.3). First, the images were converted to an 8-bit version and the contrast was increased until the secondary branches were clearly visible (approx. 1.5–2%). All the processed images were saved as tiff files and thereafter analyzed with NeuronJ. Secondary branches were measured using the "tracking" function of NeuronJ. The previously used scaling was used as the basis for the measurement.
Determination of the length and weight of F1 adult flies
After the eclosion, the first-generation adult female and male flies were maintained as virgins for 5 days before their weight and length was measured. Weights were recorded using a precision scale (Sartorius BP61-scale), whereas the lengths were recorded using and camera-equipped OLYMPUS SZX16 stereomicroscope and analyzed using cell-Sens Standard software (Olympus cellSens Standard, Version 1.16, Olympus Corporation, Tokyo, Japan).
Survival assay of F1 adult flies
Virgin flies collected within 24-h time-frame were separated by sex immediately after eclosion and transferred into separate 175 ml vials capped by a foam plug. A petri dish containing standard medium was attached to the bottom of the vial. The petri dish was renewed every other day except weekends and the number of dead flies was documented until no flies remained alive. Flies were transferred into new vials every two weeks without CO2-anaesthesia.
Statistical analysis
Values shown are mean ± SEM. The number of samples and the statistical test used for each data set are reported in the corresponding figure legends. Statistical analysis was evaluated by one-way ANOVA, unpaired Student’s t-test and Kaplan–Meier curve, log-rank (Mantel-Cox) in GraphPad Prism version 6.01. The probability of occurrence was selected at p < 0.05. Data show the results obtained from three independent experiments.
Results
Dose dependent reduction of Drosophila locomotor activity by e-nicotine
To quantify the sensitivity of adult female flies to e-nicotine and to determine the appropriate concentration of e-nicotine to be further used in our experiments, the locomotor behavior of female flies following their exposure to different concentrations of e-nicotine (1, 5 or 10 mM) was measured using a negative geotaxis assay36.
We detected a dose-dependent reduction in the locomotor behavior of female Drosophila flies following their exposure to different concentrations of volatilized nicotine. Water-treated and 1 mM e-nicotine-exposed groups exhibited no detectable difference in the climbing behavior where they rapidly climbed back to the top of the column. However, the groups exposed to either 5- or 10-mM of e-nicotine demonstrated a dose-dependent decrease in their climbing behavior, where only 60% and 40% of the flies in each group, respectively, could cross a distance of 7 cm in 10 s (Fig. 1a). In addition, nicotine-volatilization induced hyperactivity and excess grooming behavior at a lower dose and akinesia at the two higher doses. Therefore, a concentration of 5 mM of nicotine was selected for our further experiments since it’s the least concentration of nicotine that interferes with fly’s normal propensity to negatively geotax without leading to a complete loss of flies’ locomotor activity.
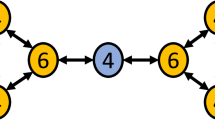
Dose dependent decrease of locomotor activity following e-nicotine exposure. (a) The locomotor activity of 10 flies/group vs time. The number (percentage) of flies that reached a height of 7 cm in 10 s following the exposure to different concentrations of nicotine as compared to the water-exposed controls was recorded (b) Experimental outline, female flies were exposed to 5 mM of volatilized nicotine for 8 times once per an hour, thereafter, the flies were mated with the males of the same age and their offspring were analysed across the timeline. Values are mean ± SEM, one-way ANOVA, **p ≤ 0.01, ****p ≤ 0.0001, n = 3 independent experiments.
Next, to investigate whether maternal exposure to e-nicotine affects the development and the growth of the offspring, female flies were exposed to 5 mM of volatilized nicotine, mated and their offspring were analyzed (Fig. 1b).
Maternal e-nicotine exposure affects the number and length of the deposited eggs
To analyze whether e-nicotine exposure affects the progeny production of F0 Drosophila females, we assessed the reproductive behavior of these flies by counting the number of eggs laid per 2 h. E-nicotine treatment led to a drastic decline in the number of deposited eggs, demonstrating therefore a significant decrease in the fecundity rate by almost 50% in comparison to water-treated controls (Fig. 2a).
E-nicotine exposure decreases the number and size of the eggs. (a) The number of eggs (%) collected per 2 h per group (b) Quantification of the egg length (mm) (c) Representative stereomicroscope image of the eggs laid on grapefruit agar (GA) per 2 h per group analysed using the image software cellSens (red line represents the measurement of the egg length). Values are mean ± SEM, unpaired t-test, **p ≤ 0.01. Bar represents 200 μm, n = 3 independent experiments.
Next, to find whether maternal exposure to volatized nicotine affects the size of the laid eggs, the deposited eggs were collected within 2 h and their size was measured. The results show that maternal e-nicotine treatment significantly reduced the length of the eggs by approximately 0.2 mm (P < 0.001) (Fig. 2a right column,c) in comparison to the control group (Fig. 2b left column,c).
The rate of eggs yielding hatched larvae
As the reduced number and size of the laid eggs is induced by the direct nicotine toxicity, we followed the survival of the deposited eggs, i.e. the egg-to-larvae development. There was a 20% (p < 0.05) decrease in the percentage of egg hatchability and therefore their development to larva following the maternal e-nicotine exposure in comparison to the percentage of larvae which hatched from the eggs laid by the control group (Fig. 3).
The effect of prenatal e-nicotine exposure on the growth of larva at different developmental stages
In order to analyze whether maternal e-nicotine exposure affects the size of the hatched F1-generation larvae, the length of 1st instar larvae was measured 24 h post-hatching and compared to water-treated controls. The average body length of F1 1st instar larvae from mothers who had been exposed to e-nicotine (Fig. 4b,c; right column) was decreased by around 100 μm in comparison to the control groups (Fig. 4a,c; left column).
The length of F1 1st instar larvae in the control and nicotine-exposed groups. (a,b) Stereomicroscope image of the 1st instar larvae from the control (a) and maternal nicotine-treated (b) groups analysed using the image software cellSens (yellow line represents the measurement of the body length) (c) Quantification of the length (μm) of 1st instar larvae from maternal nicotine-treated (gray) and control (blue) groups. Values are mean + /-SEM, unpaired t-test, **p < 0.01, n = 3 independent experiments. Bar represents 500 μm.
This growth reduction was maintained until the 3rd-instar larval stage (p < 0.01) (Fig. 5a,b). Moreover, the weight of the 3rd-instar larvae from the e-nicotine exposed mothers (Fig. 5c; right column) was significantly decreased (p < 0.01) as compared to the water controls. No other obvious morphological anomalies were observed. Since maternal tobacco smoking is related to lung function deficits, we measured the tracheal length of L3 larvae which was significantly reduced in comparison to the control L3 larvae (Fig. 5d) which nonetheless did not affect lifespan (see Supplementary Fig. S1). To obtain first insight into the mechanisms underlying the reduced larval airway length, we analyzed the expression level of genes involved in forming the tracheal tubes from early embryonic stages throughout larval life37,38,39,40,41. Although these genes are major players in length development of the Drosophila trachea, none of the investigated genes showed altered expression by maternal e-nicotine exposure (see Supplementary Fig. S2 (female larvae), Fig. S3 (male larvae)).
The length, weight and the extent of the airways of F1 3rd-instar larvae. (a) Stereomicroscope image of 3rd-instar larvae from the maternal nicotine-treated (gray) and control (blue) groups (red line represents the measurement of the body length) (b) Quantification of the 3rd-instar larvae body length (mm) (c) Weight of F1 3rd-instar larva (mg) from the control and e-nicotine-exposed mothers (d) Length (mm) of the L3 larvae airways measured using a stereomicroscope analysed using the image software cellSens. Values are mean ± SEM, unpaired t-test, *p < 0.05, ***p < 0.001, n = 3 independent experiments. Bar represents 500 μm.
Effect of maternal e-nicotine-exposure on the size and weight of adult female and male flies
Since the reduced length and weight of L3 larvae were unlikely to still reflect direct nicotine toxicity, we hypothesized that the growth reduction could be sustained in adult flies. Indeed, maternal exposure to e-nicotine induced a reduction in the average body length of 5-day old F1 virgin female flies by around 80 μm (p < 0.01) (Fig. 6b,c; right column) as compared to the flies from the control group (Fig. 6a,c; left column). Similarly, we observed a decrease in the weight of these F1 female flies from around 1.4 mg in the control group (Fig. 6d; left column) to 1.2 mg in the maternal e-nicotine-treated groups (p < 0.0001) (Fig. 6d; right column).
The length and weight of F1 adult flies. (a,b) Stereomicroscope image of the F1 female adult flies from the maternal e-nicotine-treated (b) and control (a) groups. (c,d) quantification of the length (μm) (c) and weight (mg) (d) of F1 adult female flies. (e,f) Stereomicroscope images of F1 male adult flies from the maternal e-nicotine-treated (f) and control (e) groups analysed using the image software cellSens. (g,h) quantification of the length (μm) and weight (mg) of the adult male flies. (a,b,e,f) red line represents the measurement of the adult fly body length. Values are mean ± SEM, unpaired t-test, **p = 0.001, ****p < 0.0001, n = 3 independent experiments. Bar represents 500 μm.
Similar to female F1 virgins, the average body length of F1 adult male flies was decreased by approximately 270 μm (p < 0.0001) (Fig. 6f,g; right column) as compared to the flies from the control groups (Fig. 6e,g; left column). Of note this decrease was more pronounced as compared to F1 females. In line, the body weight of these F1 male flies decreased from approximately 1.1 to 0.8 mg in the maternal-treated groups (p < 0.0001) (Fig. 6h, right column).
Weight to length ratio in F1 adult flies
Since the size of F1 male seemed to be strongly affected by maternal e-nicotine as compared to F1 females, we hypothesized that maternal e-nicotine exposure could affect both sexes differently and therefore calculated weight-to-length ratios (Fig. 7a,b). Indeed the difference in the weight/length ratios of the F1 adult females from the control and e-nicotine group was smaller (mean ± SEM 0.0363 ± 0.00659) as compared to the male flies (mean ± SEM 0.0495 ± 0.00839) (Fig. 7c) indicating that prenatal e-nicotine exposure affects males more negatively than females.
Ratio of weight-to-length in F1 adult flies. (a,b) Ratios of weight-to-length in F1 females (a) and males (b) following the maternal nicotine exposure as compared to the control group. (c) ratio of weight-to-length in females/males following the exposure to the maternal e-nicotine only. Values are mean ± SEM, unpaired t-test, ****p < 0.0001, n = 3 independent experiments.
Discussion
The adverse health effects of prenatal exposure to tobacco smoke has been recognized for many years42,43,44,45,46,47,48,49,50. Therefore, women are turning to other forms of nicotine, the electronic nicotine delivery systems, with the perception of relative safety of e-cigarettes51,52,53. In spite of this, the knowledge about the hazardous prenatal effects of e-cigarettes and their effect on early human development has received undue limited attention. Moreover, studies on the effects of e-cigarette exposure on the intergenerational health could span generations. Thus, a model to study the postnatal outcomes of prenatal e-cigarette exposure is warranted and critically important for safety surveillance of any nicotine-containing product.
Our data demonstrate that females exposed to e-nicotine exhibit nicotine sensitivity where their ability to climb in a negative geotaxis assay was impaired in a dose dependent manner. Moreover, they exhibit a reduced fertility as shown by a lower egg-deposition. In addition, eggs and hatching larvae from the e-nicotine-exposed mothers have shorter length. These findings may reflect direct effect of e-nicotine on the female organism. However, flies undergo a marked metamorphosis during pupation, in which organs and tissues are completely rebuilt from stem cells54. Thus, any changes beyond pupation induced by maternal e-cigarettes cannot be explained by acute toxicity.
Climbing is an innate behavior in which fruit flies climb the wall due to their natural tendency for negative geotaxis36. The behavior that we observed in female flies following nicotine-volatilization is in accordance with the previous studies which showed that acute exposure of Drosophila to nicotine impairs their climbing behavior as well as induces their hyperactivity and spasmodic movements36,55,56.
Borkovec (1966), reported that the decrease in fecundity following the exposure could be induced by rapid absorption of the compound through the cuticle thus affecting gonadal cells of the young flies which are in a state of division57. Several meta-analyses have shown that smoking reduces fertility among women58,59,60. Despite the increasing prevalence of e-cigarette use, the data regarding the effects of e-cigarettes on female fertility are lacking1. Even if fetuses were exposed to fewer toxins through e-cigarettes as compared to tobacco, the exposure to nicotine still causes measurable adverse fertility and pregnancy outcomes61,62. Moreover, there is also a limited number of experimental studies showing the effects of prenatal e-cigarette exposure in rodents. A recent study in female mice demonstrated that e-cigarette use delayed embryo implantation, thus delaying and reducing fertility18. Moreover, maternal exposure to e-nicotine was shown to adversely influence the structure and the physiology of the oviduct thus impairing the likelihood of pregnancy63,64,65. Therefore, prenatal exposure to nicotine compromises fetal gonadal development, affects pathways playing a role in uterine receptivity, impairs early embryo development and fertility18,66. Therefore it is likely that maternal e-cigs affect fertility in humans and this urgently needs to be addressed in the future studies.
We also observed a reduction in the length of the deposited eggs as well as a decrease in egg hatchability following the maternal exposure to e-nicotine. This could be attributed to the inhibitory properties of nicotine on chitin, the main component of cuticle and larval mouth-hook synthesis67. Nicotine could interfere with the cuticle and mouth hook development, which starts during embryogenesis, rendering them less rigid and thus depriving the larva from rupturing the egg and escaping67.
The size of F1 1st-instar and 3rd-instar larvae as well as the weight of the latter was significantly decreased following the exposure to maternal e-nicotine in comparison to control groups. There is considerable evidence from animal studies that perinatal exposure to e-cigarettes induces pup weight reduction18,68,69. Another study demonstrated that pups prenatally exposed to nicotine show delayed rate of physical maturation and growth restriction, which is in accordance with our findings showing a reduction in the length of L1 and L3 larvae following the maternal e-nicotine exposure19,70. The authors claim that postnatal delay in the development observed in prenatally nicotine treated pups is induced by the long lasting effect of prenatal nicotine exposure which delays motor development and physical maturation70. A single study in humans also showed that maternal e-nicotine might reduce birthweight, but it remained unclear if the combined use of tobacco and e-cigarettes confounded this outcome10.
Maternal smoking is known to affect lung function development in children46,47,71. Here we show that maternal e-cigarette use reduced the airway length in F1 flies indicating that maternal e-cigarette use impairs early airway development.
To identify which developmental genes are regulated by maternal nicotine and could thus explain the reduced airway length of Drosophila larvae we investigated known candidates that are involved in forming the tracheal tubes from early embryonic stages throughout the larval life37,38,39,40,41. Forming the correct tracheal length requires an exactly equilibrated balance between these genes37,72. Since these genes did not showed any difference in response to maternal e-nicotine, we assume that the dysregulation either occurs earlier during development or is more complex (see Supplementary Fig. S2 and S3).
A limitation of our study is the difficulty to estimate how the dose of e-nicotine applied relates to human exposure. Although the fly has homologues of the human cytochrome P450 CYP1A1 which is necessary for xenobiotic metabolism, the cotinine levels in the fly remained below detection limits (data not shown). Despite reduced airway length, F1 generation showed a normal lifespan (see Supplementary Fig. S1), therefore indicating that maternal exposure was not overly strong. Moreover, maternal life span was not reduced as opposed to stronger smoke or nicotine exposure models73,74 indicating that these are subthreshold concentrations for mortality with significant physiological effects.
We show here for the first time that maternal exposure to nicotine resulted in decreased weight gain and a reduction in body size even in adult females and males of the F1 generations in D. melanogaster. Therefore, our data suggest that maternal e-cigarette use can modulate long-term health outcomes in offspring. Our results are consistent with murine studies showing that prenatal exposure to nicotine affects metabolic function in F1 adult mice18 and that prenatal exposure to e-cigarettes influences body weight gain through genetic and epigenetic programming20,75,76.
The body weight-to-length ratio differed between female and male flies of F1 generation showing increased vulnerability of male offspring to maternal e-nicotine. This could be attributed to the fact that female Drosophila flies exhibit higher oxidative stress resistance as well as possess higher antioxidant defense mechanism in comparison to male flies and therefore could tolerate maternal nicotine exposure much better77. In line with this, maternal smoking triggers changes in DNA methylation resulting in methylation differences that are more apparent in male offspring78,79. Therefore, it is possible that epigenetic modifications induced by environmental stressors may at least in part be more apparent in males who show higher susceptibility to toxins than females79,80,81.
Our results demonstrate that maternal exposure to e-cigarette is associated with fetal abnormalities that persist into adulthood in flies. Currently, there are no prospective epidemiological studies in humans that examine long-term effects of maternal e-cigarette smoke exposure on the health of the offspring until adulthood and across generations. We hope that our results underline the need for human studies investigating the effects of maternal vaping on the respiratory health of their offspring.
References
Suter, M. A., Mastrobattista, J., Sachs, M. & Aagaard, K. Is there evidence for potential harm of electronic cigarette use in pregnancy?. Birth Defects Res. A Clin. Mol. Teratol. 103, 186–195 (2014).
Simonavicius, E., McNeill, A., Arnott, D. & Brose, L. S. What factors are associated with current smokers using or stopping e-cigarette use?. Drug Alcohol Depend. 173, 139–143 (2017).
Patel, D. et al. Reasons for current E-cigarette use among US adults. Prevent. Med. 93, 14–20 (2016).
Cardenas, V. M., Fischbach, L. A. & Chowdhury, P. The use of electronic nicotine delivery systems during pregnancy and the reproductive outcomes: A systematic review of the literature. Tobacco Induc. Dis. 17, 52 (2019).
Svanes, C. et al. Early life origins of chronic obstructive pulmonary disease. Thorax 65, 14–20 (2010).
Martinez, F. D. Early-life origins of chronic obstructive pulmonary disease. N. Engl. J. Med. 375, 871–878 (2016).
Pisinger, C. & Dossing, M. A systematic review of health effects of electronic cigarettes. Prev. Med. 69, 248–260 (2014).
Spindel, E. R. & McEvoy, C. T. The role of nicotine in the effects of maternal smoking during pregnancy on lung development and childhood respiratory disease. Implications for dangers of e-cigarettes. Am. J. Respir. Crit. Care Med. 193, 486–494 (2016).
Li, G., Saad, S., Oliver, B. G. & Chen, H. Heat or burn? Impacts of intrauterine tobacco smoke and e-cigarette vapor exposure on the offspring’s health outcome. Toxics 6, 2 (2018).
Cardenas, V. M. et al. Use of electronic nicotine delivery systems (ENDS) by pregnant women I: Risk of small-for-gestational-age birth. Tobacco Induc. Dis. 17, 44 (2019).
Ronkainen, E., Dunder, T., Kaukola, T., Marttila, R. & Hallman, M. Intrauterine growth restriction predicts lower lung function at school age in children born very preterm. Arch. Dis. Childh. Fetal Neonatal Ed. 101, 412–417 (2016).
Greenough, A., Yuksel, B. & Cheeseman, P. Effect of in utero growth retardation on lung function at follow-up of prematurely born infants. Eur. Respir. J. 24, 731–733 (2004).
Pike, K. C. et al. Prenatal development is linked to bronchial reactivity: Epidemiological and animal model evidence. Sci. Rep. 4, 4705 (2014).
Greene, R. M. & Pisano, M. M. Developmental toxicity of e-cigarette aerosols. Birth Defects Res. 111, 1294–1301 (2019).
Dwyer, J. B. et al. Prenatal nicotine sex-dependently alters adolescent dopamine system development. Transl. Psychiatry 9, 304 (2019).
Sifat, A. E. et al. Prenatal electronic cigarette exposure decreases brain glucose utilization and worsens outcome in offspring hypoxic-ischemic brain injury. J. Neurochem. 2, e14947 (2019).
Nguyen, T. et al. Maternal e-cigarette exposure results in cognitive and epigenetic alterations in offspring in a mouse model. Chem. Res. Toxicol. 31, 601–611 (2018).
Wetendorf, M. et al. E-cigarette exposure delays implantation and causes reduced weight gain in female offspring exposed in utero. J. Endocr. Soc. 3, 1907–1916 (2019).
Orzabal, M. R. et al. Chronic exposure to e-cig aerosols during early development causes vascular dysfunction and offspring growth deficits. Transl. Res. 207, 70–82 (2019).
Chen, H. et al. Maternal e-cigarette exposure in mice alters DNA methylation and lung cytokine expression in offspring. Am. J. Respir. Cell Mol. Biol. 58, 366–377 (2018).
Goniewicz, M. L., Hajek, P. & McRobbie, H. Nicotine content of electronic cigarettes, its release in vapour and its consistency across batches: Regulatory implications. Addiction 109, 500–507 (2014).
Werner, A. K. et al. Hospitalizations and deaths associated with EVALI. N. Engl. J. Med. 382, 1589–1598 (2020).
Armendariz-Castillo, I. et al. Genotoxic and carcinogenic potential of compounds associated with electronic cigarettes: A systematic review. Biomed. Res. Int. 2019, 1386710 (2019).
Bahl, V. et al. Comparison of electronic cigarette refill fluid cytotoxicity using embryonic and adult models. Reprod. Toxicol. 34, 529–537 (2012).
Kim, H. J. & Shin, H. S. Determination of tobacco-specific nitrosamines in replacement liquids of electronic cigarettes by liquid chromatography-tandem mass spectrometry. J. Chromatogr. A 1291, 48–55 (2013).
Vardavas, C. I. et al. Short-term pulmonary effects of using an electronic cigarette: Impact on respiratory flow resistance, impedance, and exhaled nitric oxide. Chest 141, 1400–1406 (2012).
Auer, R., Concha-Lozano, N., Jacot-Sadowski, I., Cornuz, J. & Berthet, A. Heat-not-burn tobacco cigarettes: Smoke by any other name. JAMA Intern. Med. 177, 1050–1052 (2017).
Samburova, V. et al. Aldehydes in exhaled breath during e-cigarette vaping: Pilot study results. Toxics 6, 2 (2018).
Cassee, F. R., Groten, J. P. & Feron, V. J. Changes in the nasal epithelium of rats exposed by inhalation to mixtures of formaldehyde, acetaldehyde, and acrolein. Fundam. Appl. Toxicol. 29, 208–218 (1996).
Li, L., Lin, Y., Xia, T. & Zhu, Y. Effects of electronic cigarettes on indoor air quality and health. Annu. Rev. Public Health 41, 363–380 (2020).
Haussmann, H. J. Use of hazard indices for a theoretical evaluation of cigarette smoke composition. Chem. Res. Toxicol. 25, 794–810 (2012).
Talih, S. et al. Effects of user puff topography, device voltage, and liquid nicotine concentration on electronic cigarette nicotine yield: Measurements and model predictions. Nicotine Tobacco Res. 17, 150–157 (2015).
Fuoco, F. C., Buonanno, G., Stabile, L. & Vigo, P. Influential parameters on particle concentration and size distribution in the mainstream of e-cigarettes. Environ. Pollut. 184, 523–529 (2014).
Schroeder, M. J. & Hoffman, A. C. Electronic cigarettes and nicotine clinical pharmacology. Tobacco Control 23, 30–35 (2014).
Cameron, J. M. et al. Variable and potentially fatal amounts of nicotine in e-cigarette nicotine solutions. Tobacco Control 23, 77–78 (2014).
Bainton, R. J. et al. Dopamine modulates acute responses to cocaine, nicotine and ethanol in Drosophila. Curr. Biol. 10, 187–194 (2000).
Beitel, G. J. & Krasnow, M. A. Genetic control of epithelial tube size in the Drosophila tracheal system. Development 127, 3271–3282 (2000).
Paul, S. M., Ternet, M., Salvaterra, P. M. & Beitel, G. J. The Na+/K+ ATPase is required for septate junction function and epithelial tube-size control in the Drosophila tracheal system. Development 130, 4963–4974 (2003).
Wu, V. M. & Beitel, G. J. A junctional problem of apical proportions: Epithelial tube-size control by septate junctions in the Drosophila tracheal system. Curr. Opin. Cell. Biol. 16, 493–499 (2004).
Forster, D. & Luschnig, S. Src42A-dependent polarized cell shape changes mediate epithelial tube elongation in Drosophila. Nat. Cell. Biol. 14, 526–534 (2012).
Nelson, K. S. et al. Drosophila Src regulates anisotropic apical surface growth to control epithelial tube size. Nat. Cell. Biol. 14, 518–525 (2012).
Nash, J. E. & Persaud, T. V. Embryopathic risks of cigarette smoking. Exp. Pathol. 33, 65–73 (1988).
Windham, G. C., Hopkins, B., Fenster, L. & Swan, S. H. Prenatal active or passive tobacco smoke exposure and the risk of preterm delivery or low birth weight. Epidemiology 11, 427–433 (2000).
Jaakkola, J. J., Jaakkola, N. & Zahlsen, K. Fetal growth and length of gestation in relation to prenatal exposure to environmental tobacco smoke assessed by hair nicotine concentration. Environ. Health Perspect. 109, 557–561 (2001).
Hanrahan, J. P. et al. The effect of maternal smoking during pregnancy on early infant lung function. Am. Rev. Respir. Dis. 145, 1129–1135 (1992).
Moshammer, H. et al. Parental smoking and lung function in children: an international study. Am. J. Respir. Crit. Care Med. 173, 1255–1263 (2006).
Gilliland, F. D., Berhane, K., Li, Y. F., Rappaport, E. B. & Peters, J. M. Effects of early onset asthma and in utero exposure to maternal smoking on childhood lung function. Am. J. Respir. Crit. Care Med. 167, 917–924 (2003).
Duijts, L. et al. Fetal exposure to maternal and paternal smoking and the risks of wheezing in preschool children: The Generation R Study. Chest 141, 876–885 (2012).
Burke, H. et al. Prenatal and passive smoke exposure and incidence of asthma and wheeze: Systematic review and meta-analysis. Pediatrics 129, 735–744 (2012).
den Dekker, H. T. et al. Tobacco smoke exposure, airway resistance, and asthma in school-age children: The generation R study. Chest 148, 607–617 (2015).
U.S. Department of Health and Human Services, U.S.D.o.H.a.H. The health consequences of smoking: 50 Years of progress - a report of the surgeon general. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; (2014).
Carroll Chapman, S. L. & Wu, L. T. E-cigarette prevalence and correlates of use among adolescents versus adults: A review and comparison. J. Psychiatr. Res. 54, 43–54 (2014).
Wagner, N. J., Camerota, M. & Propper, C. Prevalence and perceptions of electronic cigarette use during pregnancy. Matern. Child Health J. 21, 1655–1661 (2017).
Rolff, J., Johnston, P. R. & Reynolds, S. Complete metamorphosis of insects. Philos. Trans. R. Soc. Lond. B Biol. Sci. 374, 20190063 (2019).
Rothenfluh, A. et al. Distinct behavioral responses to ethanol are regulated by alternate RhoGAP18B isoforms. Cell 127, 199–211 (2006).
Zhang, Y., Guo, J., Guo, A. & Li, Y. Nicotine-induced acute hyperactivity is mediated by dopaminergic system in a sexually dimorphic manner. Neuroscience 332, 149–159 (2016).
Borkovec, A. B. Insect chemosterilants. Adv. Pest Control Res. 7, 1–143 (1966).
Services, S.U.U.D.o.H.a.H. Women and smoking. The U.S. Surgeon General's report. in Mayo Clin Womens Healthsource, Vol. 5 3 (2001).
Augood, C., Duckitt, K. & Templeton, A. A. Smoking and female infertility: A systematic review and meta-analysis. Hum. Reprod. 13, 1532–1539 (1998).
Wilks, D. J. & Hay, A. W. Smoking and female fecundity: The effect and importance of study design. Eur. J. Obstet. Gynecol. Reprod. Biol. 112, 127–135 (2004).
Dawkins, L. & Corcoran, O. Acute electronic cigarette use: Nicotine delivery and subjective effects in regular users. Psychopharmacology 231, 401–407 (2014).
Etter, J. F. Levels of saliva cotinine in electronic cigarette users. Addiction 109, 825–829 (2014).
Neri, A. & Marcus, S. L. Effect of nicotine on the motility of the oviducts in the rhesus monkey: A preliminary report. J. Reprod. Fertil. 31, 91–97 (1972).
Yoshinaga, K., Rice, C., Krenn, J. & Pilot, R. L. Effects of nicotine on early pregnancy in the rat. Biol. Reprod. 20, 294–303 (1979).
Jin, Z., Jin, M., Nilsson, B. O. & Roomans, G. M. Effects of nicotine administration on elemental concentrations in mouse granulosa cells, maturing oocytes and oviduct epithelium studied by X-ray microanalysis. J. Submicrosc. Cytol. Pathol. 30, 517–520 (1998).
Mamsen, L. S. et al. Cigarette smoking during early pregnancy reduces the number of embryonic germ and somatic cells. Hum. Reprod. 25, 2755–2761 (2010).
Poulson, D. F. Histogenesis, organogenesis and differentiation in the embryo of Drosophila melanogaster Meigen. Demerec 2, 168–274 (1950).
Gruslin, A. et al. Effect of nicotine exposure during pregnancy and lactation on maternal, fetal, and postnatal rat IGF-II profile. Reprod. Sci. 16, 875–882 (2009).
Wang, T. et al. Growth retardation of fetal rats exposed to nicotine in utero: Possible involvement of CYP1A1, CYP2E1, and P-glycoprotein. Environ. Toxicol. 24, 33–42 (2009).
Ajarem, J. S. & Ahmad, M. Prenatal nicotine exposure modifies behavior of mice through early development. Pharmacol. Biochem. Behav. 59, 313–318 (1998).
Hollams, E. M., de Klerk, N. H., Holt, P. G. & Sly, P. D. Persistent effects of maternal smoking during pregnancy on lung function and asthma in adolescents. Am. J. Respir. Crit. Care Med. 189, 401–407 (2014).
Samakovlis, C. et al. Development of the Drosophila tracheal system occurs by a series of morphologically distinct but genetically coupled branching events. Development 122, 1395–1407 (1996).
Velazquez-Ulloa, N. A. A Drosophila model for developmental nicotine exposure. PLoS ONE 12, e0177710 (2017).
Prange, R. et al. A Drosophila model of cigarette smoke induced COPD identifies Nrf2 signaling as an expedient target for intervention. Aging 10, 2122–2135 (2018).
Chen, H. et al. Modulation of neural regulators of energy homeostasis, and of inflammation, in the pups of mice exposed to e-cigarettes. Neurosci. Lett. 684, 61–66 (2018).
McGrath-Morrow, S. A. et al. The effects of electronic cigarette emissions on systemic cotinine levels, weight and postnatal lung growth in neonatal mice. PLoS ONE 10, e0118344 (2015).
Niveditha, S., Deepashree, S., Ramesh, S. R. & Shivanandappa, T. Sex differences in oxidative stress resistance in relation to longevity in Drosophila melanogaster. J. Comparat. Physiol. 187, 899–909 (2017).
Breton, C. V. et al. Prenatal tobacco smoke exposure affects global and gene-specific DNA methylation. Am. J. Respir. Crit. Care Med. 180, 462–467 (2009).
Murphy, S. K. et al. Gender-specific methylation differences in relation to prenatal exposure to cigarette smoke. Gene 494, 36–43 (2012).
Pliushch, G. et al. Extreme methylation values of imprinted genes in human abortions and stillbirths. Am. J. Pathol. 176, 1084–1090 (2010).
Khashan, A. S. et al. Risk of affective disorders following prenatal exposure to severe life events: A Danish population-based cohort study. J. Psychiatr. Res. 45, 879–885 (2011).
Acknowledgements
We thank the International Balzan Price Foundation for supporting this work and further Beate Höschler and Janin Braun for excellent technical assistance.
Funding
Open Access funding enabled and organized by Projekt DEAL.. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
S.K.-E. and N.E.-M. conceived the manuscript. N.E.-M. analyzed the data and had the primary responsibility for writing the manuscript. A.K. and H.A. performed the experiments. N.E.-M., K.U., S.P., T.R., K.F.R., C.W., H.A. participated in critical data interpretation. S.K.-E. designed and supervised the study. All authors contributed to writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Merhie, N., Krüger, A., Uliczka, K. et al. Sex dependent effect of maternal e-nicotine on F1 Drosophila development and airways. Sci Rep 11, 4441 (2021). https://doi.org/10.1038/s41598-021-81607-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-81607-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.