Abstract
The Saudi Cancer Registry reported in 2007 the 5-year observed survival for the most common cancer sites for the years 1994–2004. In this report we looked at the cancer survival in the period 2005–2009 and evaluated the trend over the 15 years period from 1994 to 2009. Cases of the top 14 cancer sites reported by the population based Saudi Cancer Registry from 1 January 2005 to December 31, 2009, were submitted for survival analysis. The vital status of those patients was collected. Analysis of survival for the above period was compared with the prior reported 2 periods (1994–1999, 2000–2004). In addition, analysis was done according to age, sex, disease stage and the province. Data of 25,969 patients of the commonest cancer sites were submitted. Of those 14,146 patients (54%) had complete demographic data available and vital status was reported. Thyroid cancer had the highest 5- year observed survival of 94% (95% confidence interval (CI) 93–95%)), followed by Breast (72%, 95% CI 71–74%). In hematological malignancies, Hodgkin’s Lymphoma had the highest 5-year survival of 86% (95% CI 84–88%). Survival rates has improved in most of the cancers sites for the studied periods except for lung, uterine and Hodgkin’s lymphoma which plateaued. Our study confirms a steady improvement in the 5-year observed survival over time for the majority of cancers. Our survival data were comparable to western countries. This data should be used by policy makers to improve on cancer care in the kingdom.
Similar content being viewed by others
Introduction
National cancer statistics represent important data on which decision makers depend for national cancer control strategies. The most frequently reported statistic is the cancer incidence, reported as the age standardized rate per 100,000. Less commonly, data on mortality and survival are reported. Changes in cancer incidence in a country might reflect the efficacy of the measures for primary cancer prevention adopted in that country. On the other hand, survival statistics likely represent the efficacy of the preventive measures and therapeutic measures done for cancer in any population. Contrary to other chronic illnesses, survival in cancer patients represents one of the most significant outcome measures to be followed, despite the fact of its complexity being related the stage at diagnosis, the treatment offered, and other factors related to the health care system in the country.
The Kingdom of Saudi Arabia has an established national cancer registry since 1994 which reports mainly cancer incidence of the different cancer types and in the different regions of the Kingdom. Several attempts have been made to collect mortality data but were not successful. Despite an initial increase in cancer incidence, the Saudi cancer age standardized rate has plateaued and remains one of the lowest in the region. In 2007 the Saudi cancer registry reported the 5-year observed survival of the most common cancers for the years 1994–2004. The data represented the first national survival data reported across the region.
The health care system in Saudi Arabia is rapidly evolving with new medical cities and comprehensive cancer centers being established in most of the regions of the country over the past 10 years. In this report we have looked at the changing trend in survival for the most common cancers in Saudi Arabia between 1994 and 2009. Survival was calculated at 5-year intervals to establish the presence of change in recent years. In addition, we have looked at recent survival in different regions of the country to correlate with the availability of a comprehensive cancer care in each region.
Methods
Saudi citizens diagnosed with cancer are registered by the Saudi Cancer Registry (SCR). Cancer registration is an active process. Through the Cancer Registry offices located in the various provinces within the country, trained registrars are dispatched to every hospital, clinic or laboratory and register every newly diagnosed cancer patient. Large cancer centers with hospital-based registries transfer their data electronically to the main office of the Saudi Cancer Registry. The Saudi cancer registry collects demographic data including full name, national identification number, date of birth, region where diagnosis was made and topography of the cancer. First line management and vital status at follow up are collected only if time permits and accordingly are not complete. Cancers are defined according to the International Classification of Disease-Oncology. The SCR uses the CanReg-4 program provided by the International Agency for Research on Cancer (IARC, Lyon, France). Cancer incidence data are reported annually, and reports are published at the Saudi Health Council website. In addition, SCR data are reported in the Cancer in the Five Continents series with the latest being volume X1. In order to know the vital status of each patient diagnosed, a communication was done with Elm Company, a digital transformation company that delivers an integrated business solution for both public and private sectors in many different fields, including various data services for individuals and vehicles thru its partnership with the National Information Center.
Elm provided data related to cancer patients, including the date of death of those deceased. An abstract of all registered (01 January 2005 through 31 December 2009) cases from a list of the most common cancers (top 14 cancer sites) was requested from the SCR database. The abstract included each case’s name, national identification number, date of birth and type of cancer. The vital status of those patients diagnosed was collected on 28 August 2019 and this date was considered the censoring date for those who were alive. In order for Elm company to report the vital status on the SCR abstract given to them, the patient’s name (full name in Arabic which includes given name, father’s name, grandfather’s name, and family name), national identification number and date of birth had to match. Those with un-matching data were not reported to us.
The study was approved by the institutional review board at King Abdulaziz University Hospital. Since these were national data, we were exempted from obtaining informed consent from patients by the Ethics Committee at King Abdulaziz University Hospital. Patient data were treated with strict confidentiality. Data were analyzed anonymously.
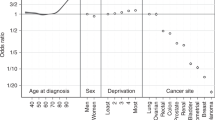
Survival was calculated from date of diagnosis to date of death or date of data capture (censoring) by the National Information Center. The Kaplan–Meier plot was used to calculate the survival according to age at diagnosis (≤ 40 years and > 40 years), sex, the province where the cancer diagnosis was made and disease stage. JMP statistical program (JMP version 15.0, 100 SAS Campus Drive, Cary, NC 27,513 USA) was used for the Kaplan–Meier plots. Since the data for the period 1994–2004 were already published, the above analysis was made only for the later period of 2005–2009.
Results
A total of 31,285 patients diagnosed with the studied cancer sites were registered by the SCR between 1 January 2005 and 31 December 2009. Of those, 5,316 were excluded initially due to unavailability of complete national ID. Accordingly, 25,969 patients were submitted to Elm for vital status verification. The number of patients submitted per cancer site is illustrated in Table 1. A total of 14,146 patients (54%) of the submitted (45.2% of the total diagnosed with the studied cancer sites for the above period) were analyzed after Elm reported back to us on their vital status. We excluded patients with illogical date of diagnosis in relation to date of death in 228 patients (0.9%), and patients with secondary malignancy in 148 patients (0.6%). Reasons for not reporting the rest by Elm were (1) un-matching patient data with Elm records in 11,135 patients (43%), (2) missing other data (such as date of birth) in 106 patients (0.4%), and (3) duplicate national ID in 206 patients (0.8%). Breakdown of the number submitted and analyzed per age, sex and stage is also illustrated in Table 1. It is apparent that the analyzed cases reflect a similar demographic distribution to the submitted cohort. The exception was thyroid cancer where 45.8% of the submitted cohort were more than 40 years while it was 86.2% in the analyzed cohort. Similarly, males represented 21.3% of the submitted cohort vs 37.9% of the analyzed one. The analysis below is based on the 14,146 patient cases returned.
5-year observed survival for the different cancers diagnosed in the period 2005–2009 is provided in Table 2. The Kaplan Meier curves of selected common cancer sites is represented in Fig. 1. Of note, the highest survival in solid tumors was observed in thyroid cancer with a 5-year observed survival of 94% (95% confidence interval (CI) 93–95%), followed by breast (72%,95% CI 71–74%), followed by uterine cancer (68%, 95% CI 63–72%), followed by bladder cancer (59%, 95% CI 55–64%) followed by ovarian cancer (54%, 95% CI 49–59%). In hematological malignancies, Hodgkin’s Lymphoma had the highest 5-year survival (86%, 95% CI 84–88%), followed by leukemia (acute and chronic, 67%, 95% CI 64–69%) followed by non-Hodgkin’s lymphoma (64%, 95% CI 62–66%).
The 5-year observed survival for different cancer sites in relation to age (≤ 40 years versus > 40 years) is illustrated in Table 3. Of note, patients ≤ 40 years of age did better in almost all cancer sites except for breast and prostate cancer and both results were not statistically significant.
Table 4 illustrate the 5- year observed survival for the different cancer sites according to sex. Findings indicate that males had worse survival in the following primary cancer sites (stomach, liver, lung, skin, thyroid, non-Hodgkin lymphoma and leukaemia). However, colo-rectal, bladder cancers and Hodgkin’s Lymphoma did not have a significant difference between males and females.
Survival according to stage of disease is shown in Table 5. As expected, the 5-year observed survival was higher for localized disease in all cancers followed by regional and metastatic disease.
Table 6 demonstrates the 5-year observed survival for each cancer site in relation to Saudi Arabia’s provinces. Significant Difference between provinces were noticed in breast cancer in the Northern Province as they had a lower 5-year observed survival by approximately 10% than other provinces in the Kingdom. Similarly, bladder cancer had lower 5 year observed survival in both the Western and Southern provinces compared to other provinces by > 25% relatively.
The 5-year observed survival for different cancer sites was also compared to previously reported survival for the same cancers by the SCR. Table 7 shows the 5-year observed survival for the different time periods of 1994–1999, 2000–2004 and 2005–2009. Despite drop in survival for many cancers for the period 2000–2004, the 5-year observed survival was consistently better in all cancers in the period 2005–2009.
Discussion
This is the first study evaluating population-based cancer survival in the Kingdom of Saudi Arabia. The study reports the 5-year observed survival for Saudi patients diagnosed with different cancers in the period from 2005 to 2009. It also examined the difference in the survival according to age, sex, disease stage, province, and the temporal trend over a 15-year period.
In general, most registries report 5-year age standardized relative survival. Unfortunately, the required data to calculate this was not available for Saudi Arabia; hence, we are reporting 5- year observed survival.
Thyroid cancer had the best survival rate among solid tumors, similar to most reported registries. Thyroid cancer represents the second most common cancer in females and the third in the population in Saudi Arabia in the years reported2,3. Breast cancer represents the commonest cancer in Saudi females and in the Saudi population in general. Despite a 5-year observed survival of 72%, this represents a slightly lower value than western countries, though most of them report relative 5-year survival4,5. Reasons behind a lower survival are likely related to a relatively high percentage of presentation in advanced stage (12.5%) and low rate of screening6. Screening for breast cancer has developed in several phases yet has not materialized into a national screening program7,8,9,10. Several opportunistic screening campaigns took place in several cities of Saudi Arabia mostly by non-governmental organizations10.
Uterine cancer is generally related to nulliparity11, which is uncommon is the Saudi population. 5-year observed survival is similar to some western countries, while appears inferior to others like USA and UK which reported cancer specific survival4,12,13. Urinary bladder cancer is seen mostly in males with 84.4% of diagnosed cases in our study of male sex. Despite 10.7% of the patients studied being in metastatic stage, which is around double what is seen in the USA14, the 5-year observed survival of 59% was similar to that reported in the Spanish population based cancer survival report4.
Colorectal cancer represents the commonest cancer in Saudi males and the second in the whole population3. The 5-year observed survival was remarkably similar to western data despite the latter representing cancer-specific survival. SEER data reported 54.8 and 57.7% 5-year cancer specific survival for colorectal cancer between 1990–1994 for males and females, respectively. This figure improved with a hazard ratio for improvement of 0.70 (95% confidence internal 0.68–0.72) for the years 2004–2009 in white Americans15. Evidently, a major factor affecting our survival figures in colorectal cancer is the late presentation in Saudi population with 30% of our patients presenting in metastatic stage. In fact, data on colorectal screening rates in a sample of the Saudi population showed 5.6% screening rate with less than 1% utilizing colonoscopy16.
Prostate cancer incidence is surprisingly low in Saudi Arabia with age-standardized rate (ASR) of 6.3/100,000 in 20162. This in contrast to a much higher reported incidence in USA and UK with ASR of 109 and 170 per 100,000 respectively17,18. The reason for the low incidence may relate to it being secondary to the lack of PSA screening19. This might also be the reason for a higher incidence of advanced stage at presentation with 32% being metastatic at presentation and the lower 5-year observed survival of 49%.
Liver cancer typically develops in patients with liver cirrhosis. The prevalence of hepatitis B infection in Saudi patients diagnosed with hepatocellular carcinoma (HCC) was reported to be 67% (95% CI: 57.7–75.3), with a much lower incidence of 11.9 for Hepatitis C virus20. Screening plays an important role in the detection of early stage HCC, which might make it more amenable for curative surgery21. Despite the implementation of a national vaccination program for hepatitis B virus in 1989 in Saudi Arabia, the effect on HCC incidence has been modest22. Additionally, unfortunately no systematic screening for HCC is present in patients with cirrhosis, and hence the low 5-year observed survival rate of 19%.
The hematological malignancies in Saudi Arabia have encouraging survival rates compared to western data4. Reasons behind this could be a usual early diagnosis in hematological malignancies and the available tertiary care centers that accept such cases promptly.
The survival difference by age has public health implications that need attention. However, caution should be taken as our study reports observed survival rather than net survival which adjust for the competing causes of death which increase in older population. In our study, younger patients did better in terms of survival similar to other countries. The exception was breast and prostate cancer, and both were not statistically significant4,15,23,24. Only 5 patients were younger than 40 years of age with prostate cancer which is expected due to higher median age at diagnosis. Older patients tend to have lower survival that may be explained by other comorbidities competing for death and are less likely to get aggressive therapy23.
In our study, sex has displayed a prognostic role with females having better survival across all reported cancer sites except in urinary bladder cancer where the difference was not statistically significant. It is important to note that urinary bladder cancer occurs predominantly in males in our region2,3. The survival superiority for females in cancer has been previously described in many populations in the literature4,23,25. Many hypotheses were proposed, of which that sex hormone patterns in female could play a role in providing a superior survival in females compared to males4.
Cancer stage at diagnosis serves as one of the most important prognostic factors in generally all cancer sites. Patients with localized disease have an advantage in survival compared with locally advanced and metastatic disease in view of the possible surgical intervention. The staging system used in our study represents the one used by the CanReg-4 registry program supplied by IARC. We interpret our survival data with caution in view of the high number of unknown cancer stage in some sites. The lower survival seen in some cancers like stomach, lung and liver represent the usually advanced stage in which they present. In general, cancers which are known to have higher sensitivity to systemic therapies in advanced stages had markedly improved 5-year observed survival such as thyroid, Hodgkin’s and non-Hodgkin’s lymphoma.
Survival trends observed in our study confirmed the steady improvement in the 5-year observed survival over time. Lung and uterine cancer survival rates did plateau over the 15-year period studied. Hodgkin’s lymphoma had an excellent survival rate of 86% in the period 1994–1999 and this was maintained in the years 2005–2009. These survival trends need to be interpreted with caution as many factors might have played a role like health care accessibility, care quality, staff expertise, treatment availability and statistical artifacts23. One important factor is the continued improvement in anticancer therapy. Additionally, the health care system has advanced with time. This might be behind the improvement in the 5-year observed survival over time.
Survival results from the Northern province underperformed other provinces in the Kingdom of Saudi Arabia. This could be explained by lack of oncology centers and patient education in that province. According to the Saudi Ministry of Health achievements report 2013, the Northern province had six specialized medical center (tertiary hospitals) while Riyadh region has 22, and Makkah region has 3626.Acknowledging these defects helps to tackle these issues leading to improvement in survival.
Population-based survival may give an insight into the effectiveness of the health care system in managing cancer patients23. Achieving better cancer control is a global health challenge that is used as a tool to assess the health care system efficacy and helps as guide if improvement is required by comparing population survival rates with others. The CONCORD-3 study is one of the biggest global comparative studies with 322 separate registries in 71 countries covering approximately 1 billion people of the global population. It investigated patients diagnosed with cancer between 2000 and 2014 and has shown that survival trends were in general on an upwards trend. However, it was clear that high-income countries enjoy better survival than low-middle income countries27.
As the population in Saudi Arabia continues to grow, the incidence of cancer has increased from 1990 to 201628. The SCR is the first national registry in Saudi Arabia established in 1992 by a resolution of the Minister of Health. It is one of first registries founded in the region. However, clearly efforts are needed to improve the registration process to get a more comprehensive survival and mortality data in the future.
Comparative survival results between populations and countries help health care officials to identify issues with the current health care system and possibly formulate national cancer strategies to improve cancer control27,29. The need for a national cancer screening programs in Saudi Arabia should be carefully studied. This is because the incidence of cancer in general in Saudi Arabia is much below western countries levels and the benefit of mass screening is not known.
Our study has several limitations. First, only 54% of cancer cases submitted were analyzed as the required data was not available for the others. An additional limitation was our inability to produce relative survival rates in view of the lack of the denominator data.
In summary, the relatively lower observed survival in some solid tumors in our study may represent the advanced stage at presentation. Hematological malignancies in Saudi Arabia have 5-year observed survival comparable to the developed countries. A positive trend in cancer survival over time was seen in most studied cancer sites. The Saudi cancer registry needs to develop a systematic method for capturing mortality and survival data with time. This study highlights the need for future studies assessing the role of screening programs for early diagnosis which could lead to improving the overall survival of cancer in the Kingdom of Saudi Arabia.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee at King Abdulaziz University Hospital (Date 21 April 2020/No. 215-20).
Consent to participate
Since the study involve retrospective national registry data, we were exempted from obtaining informed consent from patients.
Data availability
All data and documents needed will be provided upon request through email: bazarbashi@kfshrc.edu.sa.
Code availability
Not applicable.
References
Cancer Incidence in Five Continents, ed. F.B. D. Forman, D.H. Brewster, C. Gombe Mbalawa, B. Kohler, M. Piñeros, E. Steliarova-Foucher, R. Swaminathan and J. Ferlay Vol. Volume X. 2014, Lyon, France: The International Agency for Reseach on Cancer. 1365.
National Health Information Center. Cancer Incidence Report, Saudi Arabia, 2009 [cited 2021 31 January 2021]; Available from: https://nhic.gov.sa/en/eServices/Pages/TumorRegistration.aspx.
Bazarbashi, S., Al Eid, H. & Minguet, J. Cancer Incidence in Saudi Arabia: 2012 Data from the Saudi Cancer Registry. Asian Pac. J. Cancer Prev. 18(9), 2437–2444 (2017).
Chirlaque, M. D. et al. Cancer survival in adult patients in Spain. Results from nine population-based cancer registries. Clin. Transl. Oncol. 20(2), 201–211 (2018).
Allemani, C. et al. Global surveillance of cancer survival 1995–2009: Analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet 385(9972), 977–1010 (2015).
El Bcheraoui, C. et al. Breast cancer screening in Saudi Arabia: free but almost no takers. PLoS ONE 10(3), e0119051 (2015).
Al Mulhim, F. A. et al. Breast cancer screening programme: experience from Eastern province, Saudi Arabia. East Mediterr. Health J. 21(2), 111–119 (2015).
Abulkhair, O. A. et al. The first national public breast cancer screening program in Saudi Arabia. Ann. Saudi Med. 30(5), 350–357 (2010).
Akhtar, S. S. et al. First organized screening mammography programme in Saudi Arabia: preliminary analysis of pilot round. East Mediterr. Health J. 16(10), 1025–1031 (2010).
Gosadi, I. M. National screening programs in Saudi Arabia: Overview, outcomes, and effectiveness. J. Infect. Public Health 12(5), 608–614 (2019).
Gleicher, N. Why are reproductive cancers more common in nulliparous women?. Reprod. Biomed. Online 26(5), 416–419 (2013).
American Cancer Society. Endometrial cancer 2021 26 January 2021 [cited 2021 9 july 2021]; Available from: https://www.cancer.org/cancer/endometrial-cancer/detection-diagnosis-staging/survival-rates.html.
Cancer Research UK Cancer Statistics 2021 [cited 2021 9 july 2021]; Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/uterine-cancer/survival#heading-One.
Cancer Stat Facts: Bladder Cancer. 2021 [cited 2021 31 January 2021]; Available from: https://seer.cancer.gov/statfacts/html/urinb.html.
Zeng, C. et al. Disparities by Race, Age, and Sex in the Improvement of Survival for Major Cancers: Results From the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program in the United States, 1990 to 2010. JAMA Oncol. 1(1), 88–96 (2015).
Khoja, A. et al. Utilization of Colorectal Cancer Screening among Saudi Elderly Population: A Study from the Saudi National Survey for Elderly Health. Asian Pac. J. Cancer Prev. 19(12), 3401–3407 (2018).
Cancer Reaserch UK. Prostate Cancer Incidence Statistics 2021 [cited 2021 31 January 2021]; Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer/incidence#heading-Zero.
Cancer Stat Facts: Prostate Cancer. 2020 [cited 2021 31 January 2021]; Available from: https://seer.cancer.gov/statfacts/html/prost.html.
Arafa, M. A. & Rabah, D. M. With increasing trends of prostate cancer in the Saudi Arabia and Arab World: Should we start screening programs?. World J. Clin. Oncol. 8(6), 447–449 (2017).
Ayoola, E. A. & Gadour, M. O. Hepatocellular carcinoma in Saudi Arabia: Role of hepatitis B and C infection. J. Gastroenterol. Hepatol. 19(6), 665–669 (2004).
Wong, L. L. et al. Improved survival with screening for hepatocellular carcinoma. Liver Transpl. 6(3), 320–325 (2000).
National Health Information Center. Cancer Incidence Report, Saudi Arabia, 2012 [cited 2021 9 July 2021]; Available from: https://nhic.gov.sa/en/eServices/Pages/TumorRegistration.aspx.
Zeng, H. et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob. Health 6(5), e555–e567 (2018).
Arnold, M. et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995–2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol. 20(11), 1493–1505 (2019).
Bossard, N. et al. Survival of cancer patients in France: a population-based study from The Association of the French Cancer Registries (FRANCIM). Eur. J. Cancer 43(1), 149–160 (2007).
Ministry of Health acheivments 2013 [cited 2021 5 July 2021]; Ministry of Health acheivments report 2013]. Available from: https://www.moh.gov.sa/en/Documents/Facts.
Allemani, C. et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391(10125), 1023–1075 (2018).
Althubiti, M. A. & Nour Eldein, M. M. Trends in the incidence and mortality of cancer in Saudi Arabia. Saudi Med. J. 39(12), 1259–1262 (2018).
Rossi, S. et al. The EUROCARE-5 study on cancer survival in Europe 1999–2007: Database, quality checks and statistical analysis methods. Eur. J. Cancer 51(15), 2104–2119 (2015).
Acknowledgements
We gratefully acknowledge the cooperation of Saudi Cancer Registry in providing cancer records, data collection, sorting, verification, and database creation.
Author information
Authors and Affiliations
Contributions
R.S., M.A.A., H.A.E., and S.B. drafted the study design. E.D. and R.S. did the statistical analysis of the data. M.A. and S.B. prepared the tables. M.A., M.A.A., and S.B. analyzed the data. M.A. and S.B. drafted the report. S.B. did the overall supervision of the study. All authors contributed to data interpretation and reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aseafan, M., Devol, E., AlAhwal, M. et al. Population-based survival for cancer patients in Saudi Arabia for the years 2005–2009. Sci Rep 12, 235 (2022). https://doi.org/10.1038/s41598-021-04374-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-04374-6
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.